Abstract
BACKGROUND
Functional dyspepsia (FD) is a common digestive disease with limited therapeutic options. According to evidence-based clinical practice, acupuncture or electroacupuncture (EA) seems to be a promising therapy for patients with FD. However, there is still a lack of systematic reviews that have analyzed current clinical trials for a better understanding of mechanisms involved in the ameliorating effect of acupuncture and EA on FD.
AIM
To evaluate the results and qualities of existing clinical evidence for researching the underlying mechanisms of acupuncture/EA in treating FD.
METHODS
A systematic search of the literature was performed to identify randomized controlled trials in which research on the mechanism of acupuncture or EA was conducted in FD patients. Databases searched included PubMed, EMBASE, Cochrane Library, and Web of Science. Data extraction and quality assessment were completed by two investigators independently and the results of quality evaluation were exported through Review Manager V5.3.
RESULTS
Eight studies were included in this review with a total of 17 items for detecting techniques for mechanistic research. Positive effects of acupuncture and EA were observed in regulating gastric motility, gastric accommodation, mental status, gastrointestinal hormones, and central and autonomic functions while improving dyspeptic symptoms and quality of life.
CONCLUSION
The key findings of this systematic review support the potential of acupuncture and EA in altering the heterogeneous pathophysiology in patients with FD. However, high-quality studies with well-planned designs are necessary to provide more credible evidence.
Keywords: Acupuncture, Electroacupuncture, Functional dyspepsia, Gastrointestinal motility, Systematic review
Core tip: In this systematic review, we pooled randomized controlled trials with mechanistic investigations of acupuncture or electroacupuncture in improving dyspeptic symptoms, and illustrated the existing results that may provide potential explanations for the therapeutic effects. The findings of included studies in this review suggest that acupuncture and electroacupuncture can improve gastric motility and accommodation, regulate gastrointestinal hormones and mental status, and alter certain central and autonomic functions in patients with functional dyspepsia. However, due to limitations in the included articles, high-quality studies with well-planned designs and multiregional investigations are necessary to provide more convincing and credible evidence.
INTRODUCTION
Functional dyspepsia (FD) is one of the major functional gastrointestinal disorders (FGIDs)[1,2]. Defined by Rome IV criteria, FD patients suffer from several upper gastrointestinal (GI) symptoms including postprandial fullness, early satiety and epigastric pain or discomfort but without organic causes, and can be divided into two subtypes: Postprandial distress syndrome and epigastric pain syndrome (see Table 1)[3]. In a 100 population-based meta-analysis containing more than 312000 subjects, the overall pooled prevalence of uninvestigated dyspepsia was 20.8% (95% confidence interval: 17.8% to 23.9%)[4]. Unfortunately, the complexity of pathophysiological mechanisms of FD has led to insufficient efficacy of the limited available treatment options[5]. The persistent symptoms of FD are associated with negative impacts on psychological status and quality of life (QOL) for individuals[6] as well as a huge financial burden to the society, which totaled $18.4 billion in 2009 in the United States[7].
Table 1.
Rome IV criteria for functional dyspepsia
| Functional dyspepsia diagnostic criteria12 |
| One or more of the following: |
| Bothersome postprandial fullness |
| Bothersome early satiation |
| Bothersome epigastric pain |
| Bothersome epigastric burning |
| AND |
| No evidence of structural disease (including at upper endoscopy) that is likely to explain the symptoms |
| Postprandial distress syndrome diagnostic criteria2 |
| Must include one or both of the following at least 3 d per wk: |
| Bothersome postprandial fullness (i.e. severe enough to impact on usual activities) |
| Bothersome early satiation (i.e. severe enough to prevent finishing a regular-size meal) |
| No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms on routine investigations (including at upper endoscopy) |
| Supportive remarks: |
| Postprandial epigastric pain or burning, epigastric bloating, excessive belching, and nausea can also be present |
| Vomiting warrants consideration of another disorder |
| Heartburn is not a dyspeptic symptom but may often coexist |
| Symptoms that are relieved by evacuation of feces or gas should generally not be considered as part of dyspepsia |
| Other individual digestive symptoms or groups of symptoms, e.g., from gastroesophageal reflux disease and the irritable bowel syndrome may coexist with PDS |
| Epigastric pain syndrome diagnostic criteria2 |
| Must include at least 1 of the following symptoms at least 1 d a week: |
| Bothersome epigastric pain (i.e. severe enough to impact on usual activities) |
| AND/OR |
| Bothersome epigastric burning (i.e. severe enough to impact on usual activities) |
| No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms on routine investigations (including at upper endoscopy) |
| Supportive remarks: |
| Pain may be induced by ingestion of a meal, relieved by ingestion of a meal, or may occur while fasting |
| Postprandial epigastric bloating, belching, and nausea can also be present |
| Persistent vomiting likely suggests another disorder |
| Heartburn is not a dyspeptic symptom but may often coexist |
| The pain does not fulfill biliary pain criteria |
| Symptoms that are relieved by evacuation of feces or gas generally should not be considered as part of dyspepsia |
| Other digestive symptoms (such as from gastroesophageal reflux disease and the irritable bowel syndrome) may coexist with EPS |
Must fulfill criteria for B1a. Postprandial distress syndrome and/or epigastric pain syndrome.
Criteria fulfilled for the last 3 mo with symptom onset at least 6 mo before diagnosis. EPS: Epigastric pain syndrome; PDS: Postprandial distress syndrome.
Despite the increasing demand of clinical efficacy, there are no approved treatments for FD in Western societies[8]. Several current approaches are able to reduce discomfort to some extent but also with certain concerns. For example, Helicobacter pylori eradication is currently considered first-line therapy for FD patients with H. pylori infection[9]. However, increased antibiotic resistance and treatment-related side effects are the main drawbacks of this treatment[10,11]. Moreover, acid-suppressing drugs including proton pump inhibitors, prokinetic medications and tricyclic antidepressants are suggested in clinical practice to treat FD patients, but there is still an unmet need for treatment because of their limited efficacies and side effects[8].
The heterogeneous pathophysiology of FD is believed to have a close connection with the unsatisfactory clinical approaches[5]. Gastric dysmotility, impaired gastric accommodation, visceral hypersensitivity, and mucosal alterations have been highly recognized as the basic pathophysiological factors of FD[12]. Abnormal gastric motility is represented by delayed gastric emptying, antral hypomotility, and gastric dysrhythmia. It is reported that up to 60% of FD patients have delayed gastric emptying and abnormal gastric myoelectrical activity[13]. Currently, scintigraphy is considered the gold standard for testing gastric emptying while non-radioactive carbon 13 or carbon-14 breath test serves as a substitute for repeated testing[14]. Noninvasive electrogastrography (EGG) has been used to assess gastric pace-making activity in FD studies[13,15,16]. Using barostat testing, approximate one-third of FD patients are believed to suffer from visceral hypersensitivity and impaired gastric accommodation[17]. Low-grade duodenal inflammation along with impaired mucosal integrity have been recently discovered as an underlying pathophysiological mechanism in FD, which has characteristics of increased eosinophil and mast cell infiltration[18,19].
As a well-known alternative therapy, acupuncture has been applied for the treatment of various diseases[20]. Based on the different methods of stimulation, acupuncture can be classified as manual acupuncture (MA), electroacupuncture (EA), and transcutaneous electrical acustimulation (TEA)[21]. All of these methods have been used to treat FGIDs with seemingly promising therapeutic effects in clinical practice[21]. Based on the meta-analysis of randomized controlled trials (RCTs), acupuncture treatment reportedly has a significant positive effect on FD patients compared with sham acupuncture (pooled risk ratio = 2.66, 95% confidence interval: 1.85 to 3.82)[22]. Meanwhile, several clinical studies have been performed to investigate the possible underlying mechanisms of FD, including gastric dysrhythmias, delayed gastric emptying, and deactivated primary somatosensory areas and the cerebella[21,23]. However, there is still a lack of bibliometric analyses that have evaluated the results and qualities of existing clinical trials for a better understanding of the underlying mechanisms involved in the ameliorating effects of acupuncture and EA on FD.
A better understanding of the therapeutic mechanisms of acupuncture and EA will help to improve the clinical efficacy of acupuncture and EA in treating FD and even provide new insights into the medical practice for treating different subtypes of FD. Accordingly, the aim of this systematic review was to evaluate the pathophysiological mechanisms involved in the therapeutic effects of acupuncture and EA in patients with FD.
MATERIALS AND METHODS
Protocol and registration
The protocol of this systematic review was registered in the PROSPERO (International Prospective Register of Systematic Reviews) database (Registration No. CRD42019143193) with open access at https://www.crd.york.ac.uk/PROSPERO.
Selection criteria
Types of participants: Individuals, who were diagnosed with FD under the definitions of Rome criteria, including Rome I, II, III and IV criteria, were included. There were no restrictions on gender or race.
Types of interventions: Studies with applications of acupuncture or EA in patients with FD were included. Specifically, these interventions contain MA, EA, auricular acupuncture, acupressure and transcutaneous acupoint electrical stimulation using skin electrodes. Clinical trials, however, involving laser acupuncture, acupoint injection, acupoint embedding or acupoint moxibustion, were excluded. There were no limitations on the number of acupoints and the duration of treatment.
Types of comparators: Studies comparing sham acupuncture, medication, or no intervention were included in this review. On the other hand, studies with comparisons between different acupoints were excluded.
Types of outcome measures: Studies assessed the underlying mechanisms of acupuncture or EA by the usages of certain techniques, such as brain imaging, EGG, gastric emptying and questionnaires for mental status, were included.
Types of study designs: RCTs published in peer-reviewed journals in English were included.
Search strategy
A comprehensive literature search was conducted in four English online databases: PubMed, EMBASE, Cochrane Library, and Web of Science from their inception through July 9, 2019. The following search terms were combined for selected indications when appropriate: “functional dyspepsia (functional dyspepsia; non-ulcer dyspepsia; FD) and acupuncture therapy (acupuncture; electroacupuncture; acupressure; acupoint; acupuncture point).” The search strategy for PubMed was as follows: (1) search “acupuncture [Title/Abstract] OR electroacupuncture [Title/Abstract] OR acupressure [Title/Abstract] OR acupoint [Title/Abstract]”; (2) Search “functional dyspepsia [Title/Abstract] OR non-ulcer dyspepsia [Title/Abstract] OR FD [Title/Abstract]”; and (3) Search “English [Language]”.
Study selection and data extraction
Two independent reviewers evaluated the eligibility of all studies by screening the titles, abstracts, and full texts sequentially with the selection criteria mentioned above. One reviewer completed the data extraction from the included studies while the second reviewer checked the accuracy of the extracted data. Detailed information, including study design of RCT, participants’ demographics (e.g., number, gender, age, groups and diagnostic criteria with subtype information), details of interventions (according to standards for reporting interventions in clinical trials of acupuncture guidelines[24]), main results and research techniques in mechanisms, were extracted to form a conclusive table (see Table 2). Any disagreements were resolved by discussion and consensus with the corresponding author.
Table 2.
Characteristics of included studies of acupuncture vs sham, medication or no treatment in treating functional dyspepsia
| Ref. | Study design | Partial inclusion (details) | Participants | Interventions (acupoints) | Main results (scales) | Mechanism research |
| Liu et al[26], 2008 | Cross-over | Yes (chronic stage included) | n: 27 (F 18); Age (mean): 40.3 ± 4.5; groups (n): Verum A (27), Sham A (27); Diagnosis: Rome II | EXP: TEA (PC6, ST36); CONT: Sham TEA (2 non-acupoints); duration and frequency: 30 min, twice per day, for 2 wk | Decreased dyspepsia symptom scores by 55% in TEA group (dP < 0.01) (symptom scores without identified source) | Gastric motility (myoelectrical activity); neuroactivity (autonomic function); GI hormones |
| Zeng et al[27], 2012 | Parallel | No | n: 64 (F 39); Age (mean, 95%CI): Verum A (23.97, 22.90-25.04), sham A (23.83, 22.67-25.00); groups (n): Verum A (34), sham A (30); diagnosis (subtype): Rome III (PDS) | EXP: EA (ST34, ST36, ST40, ST42); CONT: Sham EA (4 non-acupoints); duration and frequency: 30 min, once per day, 20 sessions in 4 wk | Decreased symptom score in EA greater than sham EA (gP < 0.05) (SID); clinically improved QOL in EA not in sham EA (NDI for QOL) | Brain function |
| Ji et al[28], 2014 | Cross-over | No | n: 28; age (mean): 44.1 ± 9.4; Groups (n): Verum A (28), sham A (28); diagnosis (subtype): Rome III (PDS) | EXP: TEA (PC6, ST36); CONT: Sham TEA (2 non-acupoints); duration and frequency: 2 h, thrice per day, for 2 wk | Improved dyspeptic symptoms in TEA (cP < 0.05) not in sham TEA (GCSI); improved 4 domains of QOL in TEA (cP < 0.05) not in sham TEA (SF-36) | Gastric motility (myoelectrical activity and gastric emptying); gastric accommodation; mental status |
| Jin et al[29], 2015 | Parallel | Yes (serum gastrin concentration and gastric slow wave excluded) | n: 56 (F 35); age (mean): Verum A (49.29 ± 10.32), sham A (48.25 ± 11.40); groups (n): Verum A (28), sham A (28); diagnosis: Rome III | EXP: MA (ST36, KI3 ± GB4, PC6, HT7); CONT: Sham MA (non-acupoints); duration and frequency: 20-60 min in EXP/20 min in CONT, once every other d, for 4 wk | Improved dyspeptic symptoms in MA and better than sham MA (iP < 0.05) (NDI); improved QOL in MA and greater than sham MA (iP < 0.05) (SF-36) | Mental status |
| Xu et al[30], 2015 | Cross-over | Yes (TEA and sham TEA sessions included) | n: 8; age (mean): Not mentioned; groups (n): Verum A (8), sham A (8); diagnosis (subtype): Rome III (PDS) | EXP: TEA (PC6, ST36); CONT: Sham TEA (2 non-acupoints); Duration and frequency: 30 min, for 1 session | Improved dyspeptic symptoms in TEA and greater than sham TEA (cP < 0.05) (GCSI) | Gastric motility (myoelectrical activity); gastric accommodation; neuroactivity (autonomic function) |
| Zhang et al[31], 2015 | Parallel | Yes (EA and control groups included) | n: 319 (F 157); age (mean): EA (42.6 ± 11.9); CONT (41.8 ± 12.2); groups (n): EA (159), CONT (160); diagnosis: Rome III | EXP: EA (ST36, CV12, PC6, LR3, SP4); CONT: Oral pantoprazole, amitriptylines and mosapride; duration and frequency: 15 min, twice per day, 5-d per wk in EXP; pantoprazole 20 mg with amitriptylines 5 mg, twice per day, and mosapride 5 mg, thrice per day in CONT; for 4 wk | Decreased symptom scores in EA and greater than CONT (aP < 0.05) (symptom scores without identified source); increased QOL scores in EA and better than CONT (aP < 0.05) (SF-36) | GI hormones; gastric motility (myoelectrical activity and gastric emptying) |
| Ko et al[32], 2016 | Cross-over | Yes (from baseline to the first 4-wk included) | n: 76 (F 53); age (mean): MA (49.4 ± 12.1); CONT (49.1 ± 14.5); groups (n): MA (37), CONT (39); diagnosis: Rome III | EXP: MA (LI4, ST36, LR3, SP4, CV12 ± GB21, SI14, PC6, EX-HN5, ST34); CONT: No treatment; duration and frequency: 15 min, twice weekly, for 4 wk | Significantly higher PR in MA than CONT (eP < 0.001); lower symptom scores in MA than CONT (aP < 0.05) (NDI); improved QOL in MA (eP < 0.001) not in CONT (FD-QOL scale) | Mental status |
| Qiang et al[33], 2018 | Parallel | No | n: 64 (F 38); age (mean): EA (42.6 ± 11.9); CONT (41.8 ± 12.2); groups (n): EA (32), CONT (32); diagnosis: Rome III | EXP: EA (ST36, SP6, SP4, PC6); CONT: Oral mosapride; duration and frequency: 30 min, once per day in EXP; 5 mg, thrice per day in CONT; for 30 d | Decreased symptom score in EA and greater than CONT (aP < 0.05) (LDQ); increased QOL scores in EA and better than CONT (aP < 0.05) (FD-QOL scale) | GI hormones |
P < 0.05, bP < 0.01,
P < 0.001 vs control group;
P < 0.05,
P < 0.01, fP < 0.001 vs sham TEA;
P < 0.05 vs sham EA;
P < 0.05 vs sham MA. A: Acupuncture; CONT: Control group; EA: Electroacupuncture; EXP: Experimental group; F: Female; FD-QOL: Functional dyspepsia-related quality of life; GCSI: Gastroparesis cardinal symptom index; GI: Gastrointestinal; LDQ: Leeds dyspepsia questionnaire; MA: Manual acupuncture; NDI: Nepean dyspepsia index; PDS: Postprandial distress syndrome; PR: Proportion of responders; QOL: Quality of life; SF-36: Short form 36 health survey questionnaires; SID: Symptom index of dyspepsia; TEA: Transcutaneous electrical acustimulation; CI: Confidence interval.
Quality assessment
Based on the Cochrane Collaboration’s tool for assessing the risk of bias[25], all included trials were assessed for methodological quality by two independent investigators, with disagreements resolved by a third investigator. The following aspects were evaluated respectively for this assessment: generation of random sequence, concealment of allocation, blind method, incomplete outcome data, selective reporting and other bias, and the results were exported through Review Manager V 5.3 (Cochrane Collaboration, Oxford, United Kingdom).
RESULTS
Study selection
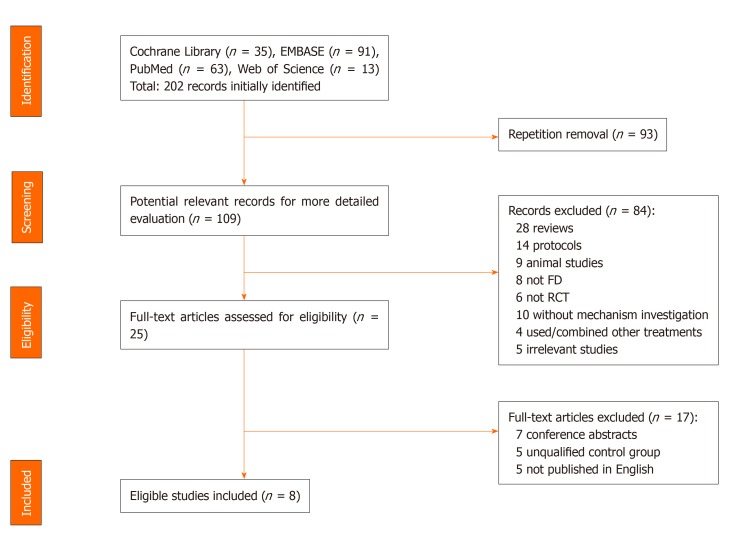
Based on the PRISMA flow diagram, the process of study selection is shown in Figure 1. A total of 202 potential records were retrieved through the four databases. After the removal of duplicates, 109 articles remained to be screened by the titles and abstracts. Of these 109 articles, 25 studies appeared to be relevant and were assessed in the full text. Upon agreement between the two reviewers, eight studies met the inclusion criteria and were included in this review[26-33].
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses flow diagram. FD: Functional dyspepsia; RCT: Randomized controlled trial.
In the study of Zhang et al[31], multiple groups were used; based on the requirements of inclusion criteria, only data from the EA group and control group were extracted for the analyses. Similarly, data came from the TEA and sham TEA sessions of the research of Xu et al[30] as well as the chronic stage of the study of Liu et al[26] were included in this review. Due to an ineligible control group, data on serum gastrin concentration and gastric slow waves were excluded in the study of Jin et al[29]. In the cross-over study from Ko et al[32], only data from the baseline to the end of the first 4 wk of the treatment (first arm of the treatment) were extracted for analysis and data from the second arm of the treatment were excluded due to lack of a wash-out period before the second-arm treatment (See Table 2).
Study characteristics
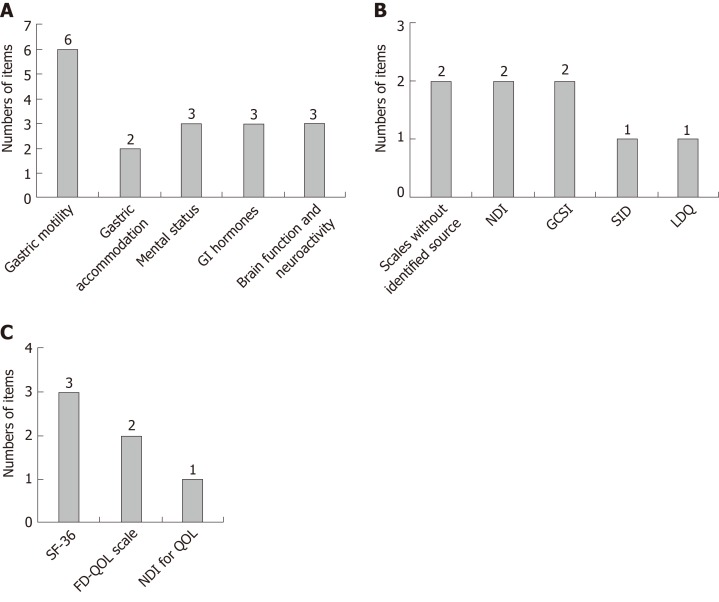
Results from eight studies published from 2012 to 2018 were included in this review with detailed information shown in Table 2. A total of 642 patients were involved in the eight trials and the number of participants varied from 8 to 319. The percentage of females was 49.2%-69.7% with two unknowns[28,30]. Therapeutic methods included MA, EA, and TEA. Five of the studies adopted the sham acupuncture as the control method[26-30], compared to two trials using medications[31,33] and one study without treatment[32] in the control group. All included studies applied certain dyspepsia symptom scales (see Table 2) to assess the efficacy of acupuncture, and six reported the effects of acupuncture on QOL[27-29,31-33]. In terms of mechanistic research, a total of 17 items were investigated in the studies and classified into the following categories: gastric motility, gastric accommodation, mental status, GI hormones, and central and autonomic functions (see Figure 2A).
Figure 2.
Numbers of detecting items for mechanism research, scales of dyspeptic symptoms, and scales of quality of life of acupuncture and electroacupuncture in treating functional dyspepsia. A: Numbers of detecting items for mechanism research; B: Numbers of detecting items for scales of dyspeptic symptoms; C: Numbers of detecting items for scales of quality of life. FD-QOL: Functional dyspepsia-related quality of life; GCSI: Gastroparesis cardinal symptom index; GI hormones: Gastrointestinal hormones; LDQ: Leeds dyspepsia questionnaire; NDI: Nepean dyspepsia index; QOL: Quality of life; SF-36: Short form 36 health survey questionnaires; SID: Symptom index of dyspepsia.
Clinical effects
Dyspeptic symptoms and QOL: All eight studies reported decreased dyspeptic symptom scores after the MA, EA, or TEA treatment by using varied symptom scales (see Figure 2B). However, different methods of assessment and different scales used in reporting results made it difficult to compare the outcomes among the studies. Most of the included trials indicated an improvement in QOL in FD patients treated with acupuncture, and the short form 36 health survey questionnaire and FD-related QOL were the popular measurement tools among the studies (see Figure 2C).
Pathophysiology
Gastric motility: Among the eight studies, three reported the results of gastric motility, including gastric myoelectrical activity and gastric emptying (see Table 3). To study the mechanism of gastric myoelectrical activity, EGG was used consistently in the trials and the gastric slow wave frequency was a major and common parameter[26,28,30,31]. Two trials reported improvement in the percentage of normal gastric slow waves[28,30] and one study showed an increase in gastric slow wave frequency[31]. Two of the three studies reported the outcomes of gastric emptying but with different methods, including the radiogram and B-ultrasound; accelerated gastric emptying was observed in both studies[28,31].
Table 3.
Characteristics of included studies in mechanism research
| Ref. | Detecting items | Research techniques | Main results |
| Gastric motility | |||
| Liu et al[26], 2008 | Gastric myoelectrical activity | EGG | Gastric slow wave not altered by TEA |
| Ji et al[28], 2014 | Gastric myoelectrical activity; Gastric emptying | EGG; Radiogram | Increased percentage of normal slow wave in both fasting and postprandial stages in TEA (dP < 0.01) not in sham TEA; accelerated gastric emptying in TEA (fP < 0.001) not in sham TEA |
| Xu et al[30], 2015 | Gastric myoelectrical activity | EGG | Increased dominant power and percentage of normal slow wave in postprandial stage in TEA compared with sham TEA (cP < 0.05) |
| Zhang et al[31], 2015 | Gastric myoelectrical activity; gastric emptying | EGG; B-ultrasound | Improved basic frequency and slow wave frequency in EA compared with CONT (aP < 0.05); increased gastric half-emptying time and antrum movement index in EA compared with CONT (aP < 0.05) |
| Gastric accommodation | |||
| Ji et al[28], 2014 | Gastric accommodation | Nutrient drinking test | Improved threshold of satiety volume (dP < 0.01) and maximum tolerance volume (fP < 0.001) in TEA not in sham TEA |
| Xu et al[30], 2015 | Gastric accommodation | Satiety drinking test | Increased maximum tolerable volume in TEA compared with sham TEA (cP < 0.05) |
| GI hormones | |||
| Liu et al[26], 2008 | Plasma NPY and motilin levels | Radioimmunoassay | Increased plasma NPY but not motilin level in TEA (cP < 0.05) not in sham TEA |
| Zhang et al[31], 2015 | Plasma motilin level | Radioimmunoassay | Increased plasma motilin level in EA compared with CONT (aP < 0.05) |
| Qiang et al[33], 2018 | Serum ghrelin, CGRP and GLP-1 levels | ELISA | Increased serum ghrelin and GLP-1 levels and decreased CGRP level in EA compared with CONT (aP < 0.05) |
| Mental status | |||
| Ji et al[28], 2014 | Anxiety and depression | SAS/SDS | Decreased anxiety (dP < 0.01) and depression (cP < 0.05) scores in TEA not in sham TEA |
| Jin et al[29], 2015 | Anxiety and depression | SAS/SDS | Improved anxiety (kP < 0.0001) and depression (kP < 0.001) status in MA compared with sham MA |
| Ko et al[32], 2016 | Anxiety and depression | STAI/BDI | Decreased anxiety and depression scores in MA (bP < 0.01) not in CONT |
| Central and autonomic functions | |||
| Liu et al[26], 2008 | Autonomic function | HRV derived from ECG | In fasting stage, higher HF activity (cP < 0.05) and lower LF/HF ratio (cP < 0.05) in TEA than that before the treatment but not in sham TEA |
| Zeng et al[27], 2012 | Cerebral glycometabolism changes | PET-CT scans | Extensive deactivation in cerebral activities in EA compared with the sham EA(fP < 0.001) |
| Xu et al[30], 2015 | Autonomic function | HRV derived from ECG | Enhanced vagal activity in TEA compared with sham TEA (fP < 0.001) |
P < 0.05,
P < 0.01 vs control group;
P < 0.05,
P < 0.01,
P < 0.001 vs sham TEA;
P < 0.001 vs sham EA. BDI: Beck depression inventory; CGRP: Calcitonin gene-related peptide; CONT: Control group; EA: Electroacupuncture; ECG: Electrocardiogram; EGG: Electrogastrogram; GI: Gastrointestinal; GLP-1: Glucagon-like peptide-1; HRV: Heart rate variability; MA: Manual acupuncture; NPY: Neuropeptide Y; SAS: Zung’s self-rating anxiety scale; SDS: Zung’s self-rating depression scale; STAI: State-trait anxiety inventory; PET-CT: Fluorine-18 fluorodeoxy glucose positron emission tomography computed tomography; TEA: Transcutaneous electrical acustimulation; ELISA: Enzyme linked immunosorbent assay.
Gastric accommodation: Due to the intolerance of barostat, which is the gold standard for assessing gastric accommodation, two studies applied the nutrient drinking test or satiety drinking test as a surrogate for the assessment of gastric accommodation[28,30] (see Table 3). The maximum tolerable volume was used to reflect the capacity of gastric accommodation and was increased after TEA in both studies.
Mental status: Anxiety and depression were the two focuses for evaluating mental status. Three studies assessed the anxiety and depression degrees by different questionnaires and showed improvement in mental status after acupuncture treatment[28,29,32] (see Table 3).
Mechanisms
GI hormones: Five GI hormones were tested in three of the eight trials[26,31,33], including neuropeptide Y (NPY), motilin, ghrelin, calcitonin gene-related peptide (CGRP) and glucagon-like peptide-1 (GLP-1). Radioimmunoassay and enzyme-linked immunosorbent assay were adopted as the testing methods in the studies (see Table 2). EA was reported to increase motilin, ghrelin, and GLP-1 levels and decrease CGRP level. The study of Liu et al[26], however, showed an increase in plasma NPY but not motilin after TEA treatment.
Central and autonomic functions: By means of fluorine-18 fluorodeoxy glucose positron emission tomography computed tomography (PET-CT) scans, one study observed the cerebral glycometabolism changes in FD patients and found extensive deactivation in cerebral activities in EA group compared with the sham EA group[27]. In addition, two cross-over trials reported a TEA-induced increase in vagal activity assessed by the spectral analysis of heart rate variability (HRV) derived from electrocardiogram[26,30] (see Table 3).
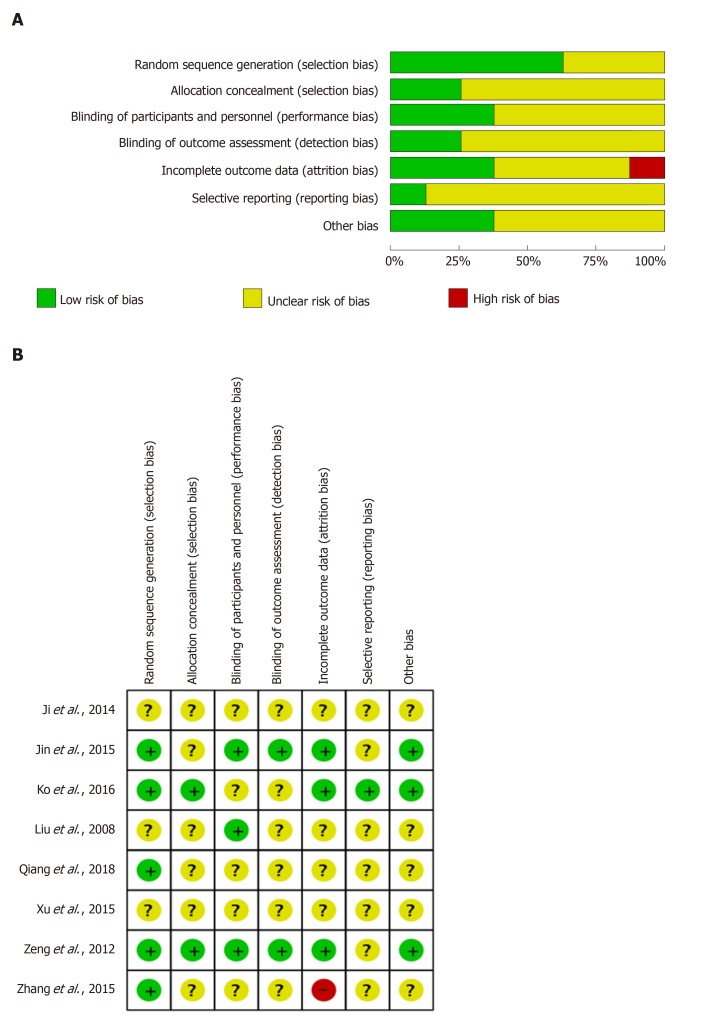
Methodological quality
Methodological assessment of the included studies was represented in the risk of bias graph (Figure 3A) and the risk of bias summary (Figure 3B). Most studies showed a low risk at the random sequence generation. However, the risk of selective reporting remained unclear in most trials due to the lack of research protocols published or registered previously. Meanwhile, most responses of allocation concealment, blinding of participants and personnel, and blinding of outcome assessment were unavailable in detail.
Figure 3.
Risk of bias graph and summary of included studies. A: Risk of bias graph of included studies; B: Risk of bias of included studies.
DISCUSSION
Due to the complex and multifactorial pathophysiology of FD, the effectiveness of current treatments remains unsatisfactory. Under this condition, nearly 50% of patients suffering from FGIDs showed the tendency to seek out complementary and alternative medicine[34]. A number of clinical studies have indicated the positive outcomes of acupuncture in treating FD[22]; however, there is a lack of mechanistic studies based on high-quality clinical trials. In this systematic review, using evidence-based evaluation methods, we pooled clinical trials with mechanism investigations of acupuncture in treating FD and presented the existing results that may provide potential explanations for the therapeutic effects.
Our findings demonstrated that the RCTs available in the literature placed emphasis on gastric motility and accommodation, psychopathological state, neuroendocrine functions, and central and autonomic functions to elucidate the underlying mechanisms of acupuncture in treating FD. All included articles demonstrated improvement of dyspeptic symptoms, and six trials reported the enhancement of QOL with acupuncture in FD patients, in agreement with a previous systematic and meta-analysis on the efficacy of acupuncture in treating FD[22].
Four studies showed enhanced gastric myoelectrical activity assessed by the EGG with both EA and TEA[26,28,30,31]. One trial tested the level of plasma motilin, one of GI hormones to simulate GI motility, and demonstrated that EA increased plasma motilin while ameliorating dyspeptic symptoms[31]. Two studies indicated that EA and TEA accelerated gastric emptying assessed by the radiogram or ultrasound[28,31]. Although the breath test and scintigraphy are more commonly used to assess gastric emptying[35], the positive results on gastric myoelectrical activity and gastric emptying in these studies have provided evidence that EA and TEA improve dyspeptic symptoms by enhancing gastric motility in patients with FD. Also, impaired gastric accommodation has been observed in FD patients[36]. Due to the intolerance of barostat, two studies applied a surrogate method, the nutrient drinking test, for the assessment of gastric accommodation, and reported enhanced gastric accommodation with TEA in comparison with sham treatment in patients with FD[28,30].
With the updates of Rome IV, FGIDs have been considered disorders of the gut-brain interaction[37]. Meanwhile, more and more research has garnered considerable interest in revealing the relative mechanisms and identifying potential therapeutic targets[38]. Brain-gut peptides, including GI hormones and neuropeptides, play an important role in communication between the GI system and the brain. It has been reported that NPY, motilin, ghrelin, and GLP-1 affect gastric emptying and appetite[39,40] and that CGRP participates in the development of visceral hypersensitivity[41]. All these peptides, including motilin, ghrelin, NPY, GLP-1 and CGRP, have been investigated in relevant research for studying potential managements of FD patients[42-45]. In this review, one study assessed the neuroendocrine function and observed that EA regulated the serum levels of ghrelin, GLP-1, and CGRP and concurrently improved dyspeptic symptoms and QOL[33]. A study by Liu et al[26] reported the enhanced release of NPY but not motilin with TEA in FD patients. On the contrary, another study showed an increased plasma motilin level in FD patients treated by EA in comparison with the control group[31]. It has been reported in rodent studies that EA with chronically implanted electrodes improve gastric dysmotility mediated via autonomic-cholinergic mechanisms[46] and suppress gastric hypersensitivity by restoring the sympathovagal balance[47]. According to a resting-state functional magnetic resonance imaging study, the functional connectivity of the brain was changed after MA in FD patients[48]. These possible modulations of acupuncture on both central and peripheral nervous systems may provide an underlying explanation for the regulatory effect of acupuncture on brain-gut peptides.
Epidemiological evidence has suggested a higher prevalence of anxiety and depression in FD patients than in healthy subjects, suggesting a role of psychiatric disorders in the onset of FD[49]. Three studies in our review reported a decrease in anxiety and depression scores after TEA or MA in FD patients[28,29,32]. To study the specific interactions between the gut and the brain, neuroimaging has been entered into the field of FGIDs and helped to partly elucidate the complexity of pathophysiological mechanisms[50]. With the use of PET-CT scans, one clinical trial investigated the cerebral glycometabolism changes in FD patients and detected extensive deactivation in cerebral activities with EA compared with sham[27]. The autonomic nerve system is an important interface of the gut-brain axis[51]; two studies showed TEA-induced increase in vagal activity assessed by the spectral analysis of HRV derived from the electrocardiogram[30].
Methods of MA, EA, and TEA
With substantial progress in clinical and mechanistic research, acupuncture has been increasingly accepted in Western societies[52] and has been applied in treating GI dysfunctions[53] such as irritable bowel syndrome[54], inflammatory bowel disease[55], and constipation[56]. According to the difference of implementation, the general terms of acupuncture include MA, EA, and TEA.
In clinical practice, MA is the classical and most commonly used method; it is performed by inserting needles into certain acupoints with or without special manual manipulations, such as twisting, lifting, thrusting, or other complex combinations, to achieve different sensations for specific therapeutic effects[57]. It has been indicated that different modes of MA have different effects on the same disease[58]. However, the main concern of MA is the difficulty in standardizing the treatment, especially in clinical research[21].
Compared to MA, EA is a modern approach that combines traditional acupuncture with modern concepts of neuromodulation[59]. Due to its advantages in great time saving and high reproducibility, EA has been widely applied in clinical and laboratory research[60,61]. Moreover, different clinical effects can be obtained through different stimulation parameters. For example, EA at a low frequency of 2-4 Hz can enhance the release of enkephalins in the central nervous system, whereas EA at a high frequency of 80-120 Hz can increase dynorphins in the spinal cord[62].
TEA is considered an alternative of EA. It is a noninvasive and needleless method of stimulating the acupoint via surface electrodes placed over the acupoints. Using a wearable stimulation device, TEA can be easily handled by the patient or family at home, which eliminates the hospital visit and reduce the treatment cost and increases the treatment frequency and thus therapeutic efficacy. Moreover, without the insertion of needles and tedious hospital visits, clinical compliance is greatly increase with TEA[21]. It has been shown that the efficacy of TEA in pain control is at least as effective as EA[63]. By increasing the frequency of administration from a few times per week to once or twice daily, TEA could be more effective than EA and acupuncture and therefore more attractive in treating FD.
Methods of the assessment of FD pathophysiology
According to the present understandings, different pathophysiological mechanisms are relevant to the occurrence of FD, including disturbed gastric motility and sensation, impaired gastric accommodation, low-grade gastroduodenal immune activation and dysregulation of gut-brain axis[18].
Gastric slow waves and emptying: Unlike the consistent usage of EGG in clinical studies of gastric slow waves for dysrhythmia[64-66], the methods of gastric emptying test are varied. Scintigraphy has been adopted as the current gold standard for measuring gastric emptying[14]. Meanwhile, corresponding consensus standards with the recommended protocol have been developed to overcome the shortness in reproducibility of different test meals and recording techniques[67,68]. Except the formal gastric emptying test, gastric food retention on endoscopy has been found having a correlation with delayed gastric emptying[69]. Also, several noninvasive approaches are available. For instance, 13C-octanoic acid breath test is a more commonly used reliable substitute for repeated testing with similar reproducibility of scintigraphy[70-72].
Gastric accommodation: Impaired gastric accommodation can be tested via an intragastric balloon connected to a barostat device, which is considered the gold standard. A few imagine techniques have also been used to assess gastric accommodation such as single-photon emission computed tomography, ultrasound, and magnetic resonance imaging[73-75]. However, none of these methods has been widely used in clinical diagnosis or clinical research[8,75]. On the other hand, the non-imaging nutrient drinking test has been employed as noninvasive and reproducible alternatives for the diagnosis of impaired accommodation as well as the assessment of therapeutic effectiveness[76-78]. It has been indicated that the distal instead of proximal stomach function may be more relevant to drinking capacity, but the persistent discomforts of FD patients are mostly associated with the proximal stomach volume[79]. More recently, one enhanced gastric emptying scintigraphy test showed the potential to obtain the results from gastric emptying and accommodation with antral contraction in one test[80]. However, further development is needed before it can be popularized.
Visceral hypersensitivity: Visceral sensations are conventionally classified into chemical and mechanical sensations. Gastric mechanosensitivity to distension can be measured by gastric barostat[81]. The prevalence of gastric hypersensitivity assessed by gastric barostat has been reported in 37% of FD patients[17] and a positive correlation between visceral hypersensitivity and GI symptom severity has been shown[82]. For visceral chemosensitivity, capsaicin, as an agonist at the transient receptor potential vanilloid 1 that plays an important role in converting noxious chemical and physical stimuli into nociceptive responses[83], has been used in related studies to uncover an increase in chemical hypersensitivity in FD patients[84,85]. Acid sensitivity has also been studied in FD patients. According to one study, the severity of dyspeptic symptoms caused by direct gastric acid infusion was greater in FD patients than in healthy volunteers[86].
Duodenal mucosal alterations: Recently, duodenal mucosal alterations represented by low-grade inflammation and impaired mucosal integrity have been considered one of the main pathological factors in FD[87]. Increased infiltration of mucosal eosinophils and mast cells have been identified in FD patients under immunohistochemical stain[19]. The Ussing chamber, a well-known technique for the evaluation of transmural resistance of epithelial tissue[88], has been applied to uncover the reduced transepithelial electrical resistance and enhanced paracellular permeability in patients with FD[19]. In addition, one study utilized an endoscopic catheterization method to measure the mucosal admittance and observed increased mucosal permeability in FD patients with a significant negative correlation between transepithelial electrical resistance and mucosal admittance in the duodenum[89]. Several studies have shown the systemic immune activation in FD[90]. For instance, in a previous study, the levels of tumor necrosis factor-α, interleukin-1β, and interleukin-10 as well as small bowel homing T cells were found to be elevated in FD patients compared with healthy controls or patients with irritable bowel syndrome, as assessed by flow cytometry and enzyme-linked immunosorbent assay[91].
Others: Neuroimaging studies, conducted mostly by PET-CT and magnetic resonance imaging, have manifested the dysfunctional brain-gut interactions in patients with FD[92-94]. By measuring HRV, altered autonomic function has been observed in FD in both adults and children[95,96]. Anxiety, depression, and somatoform disorders are the most common psychosocial factors in FD patients[97]. Therefore, various questionnaires, such as Spielberger State and Trait Anxiety Inventory, Centre of Epidemiological Studies Depression Scale, Symptom Checklist-90, Zung’s Self-Rating Anxiety Scale, Zung’s Self-Rating Depression Scale, 17-item Hamilton Depression Rating Scale, and the 14-item Hamilton Anxiety Rating Scale, have been adopted in clinical studies for psychosocial assessments and therapeutic evaluations[98-101].
Limitations and future directions
There were several limitations in this review. First, the included studies were highly heterogeneous in regard to study design, research aims, and targeted mechanisms. For instance, various scales were used to evaluate the efficacy of acupuncture, EA and TEA in improving dyspeptic symptoms, which led to non-mergeable data for further meta-analyses. To achieve consistent and comparable clinical outcomes, well-designed questionnaires, such as nepean dyspepsia index, or proportion of responders should be used as evaluation tools in future FD studies. Second, studies with a high methodological quality were relatively limited, based on the Cochrane Collaboration’s assessment tool. Critical information related to allocation concealment as well as blinding methods of participants, personnel and outcome assessment remains missing in most of the included trials. However, considering placebo effects in the acupuncture study, those unavailable details could bring along unreliable conclusions to medical practice. Hence, it is important to follow highly recognized guidelines, which is represented by standards for reporting interventions in clinical trials of acupuncture[24], to perform complete and transparent clinical trials in reporting acupuncture related interventions. Additionally, most included studies were conducted in China[27-31,33] with one published in South Korea[32], which may contribute to a potential reporting bias. To overcome this shortcoming, multi-regional studies are in a great demand to supply solid clinical outcomes and diverse mechanistic techniques. Moreover, several included studies focused on the stomach to reveal the potential mechanisms of MA, EA, and TEA in treating FD such as gastric myoelectrical activity, gastric emptying and accommodation. However, dysfunctions of other upper GI organs may also contribute to the onset of dyspeptic symptoms. For example, an increase of spontaneous duodenal acid exposure has been reported in FD patients with prominent nausea[102]. In the future, research involved with multifactorial dysfunction of upper GI organs should be considered in the clinical trials to serve a better understanding of the complexity of pathophysiology in FD.
In conclusion, this systematic review presented the results and qualities of existing RCTs performed to investigate underlying mechanisms of MA, EA and TEA in ameliorating FD. The findings of included studies in this review demonstrated that acupuncture reduced dyspeptic symptoms by improving pathophysiologic dysfunctions of FD such as enhancing gastric motility and accommodation, regulating GI hormones and mental status, and improving central and autonomic functions and in FD patients. However, in the view of limitations of included articles, high-quality studies with well-planned designs and multi-regional investigations are necessary to provide more convincing and credible evidence. For future research, mechanistic studies on EA in FGIDs should focus on revealing the interactions between the gut and brain to keep in pace with the latest pathophysiological understandings and clinical consensus.
ARTICLE HIGHLIGHTS
Research background
Functional dyspepsia (FD) is one of the most common functional gastrointestinal disorders in the clinic. Due to the multifactorial pathophysiology of this disease, however, current clinical approaches remain unsatisfactory with limited efficacy or side effects. Acupuncture along with electroacupuncture (EA) has been applied in treating FD with seemingly promising therapeutic effects.
Research motivation
Numerous clinical trials were performed to investigate the effects as well as the underlying mechanisms of acupuncture in treating FD. Still, there is a lack of a bibliometric analyses that evaluated the results and qualities of existing clinical evidence.
Research objectives
A better understanding of therapeutic mechanisms of acupuncture will help to improve the clinical efficacy of this treatment as well as provide new insights into the medical practice for treating FD. Hence, the aim of this systematic review was to evaluate pathophysiological mechanisms involved in the ameliorating effect of acupuncture/EA in patients with FD.
Research methods
According to the methodology of evidence-based medicine, a systematic search of the literature was performed to identify randomized controlled trials in which the mechanism researches of acupuncture or EA were applied in FD patients.
Research results
Eight studies were included in this review with a total of 17 items of detecting techniques for mechanistic research. Positive effects of acupuncture and EA were observed in regulating gastric motility, gastric accommodation, mental status, gastrointestinal hormones, and central and autonomic functions while improving dyspeptic symptoms and QOL.
Research conclusions
This is the first time that a systematic review focused on the underlying mechanisms of acupuncture including manual acupuncture, EA, and transcutaneous electrical acustimulation has been conducted to elaborate the current research status in the clinical trials of FD.
Research perspectives
Under the limitations of included articles, high-quality studies with well-planned designs and multi-regional investigations are necessary to provide more convincing and credible evidence. Also, mechanistic studies on acupuncture in FD should focus on revealing the interactions of gut-brain axis.
Footnotes
Conflict-of-interest statement: No potential conflicts of interest.
PRISMA 2009 Checklist statement: The authors have read the PRISMA 2009 checklist and the manuscript was prepared and revised according to the PRISMA 2009 checklist.
Manuscript source: Invited manuscript
Peer-review started: December 16, 2019
First decision: February 24, 2020
Article in press: April 22, 2020
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Farhat S, Ierardi E S-Editor: Tang JZ L-Editor: Filipodia E-Editor: Ma YJ
Contributor Information
Yu Guo, Department of Gastroenterology, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China; Division of Gastroenterology and Hepatology, Johns Hopkins University School of Medicine, Baltimore, MD 21224, United States.
Wei Wei, Department of Gastroenterology, Wangjing Hospital of China Academy of Chinese Medical Sciences, Beijing 100102, China.
Jiande DZ Chen, Division of Gastroenterology and Hepatology, Johns Hopkins University School of Medicine, Baltimore, MD 21224, United States; Division of Gastroenterology and Hepatology, University of Michigan School of Medicine, Ann Arbor, MI 48109, United States. jiandedzchen@gmail.com.
References
- 1.von Wulffen M, Talley NJ, Hammer J, McMaster J, Rich G, Shah A, Koloski N, Kendall BJ, Jones M, Holtmann G. Overlap of Irritable Bowel Syndrome and Functional Dyspepsia in the Clinical Setting: Prevalence and Risk Factors. Dig Dis Sci. 2019;64:480–486. doi: 10.1007/s10620-018-5343-6. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Li Z, Andruzzi E, Temple RD, Talley NJ, Thompson WG, Whitehead WE, Janssens J, Funch-Jensen P, Corazziari E. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 3.Stanghellini V, Chan FK, Hasler WL, Malagelada JR, Suzuki H, Tack J, Talley NJ. Gastroduodenal Disorders. Gastroenterology. 2016;150:1380–1392. doi: 10.1053/j.gastro.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 4.Ford AC, Marwaha A, Sood R, Moayyedi P. Global prevalence of, and risk factors for, uninvestigated dyspepsia: a meta-analysis. Gut. 2015;64:1049–1057. doi: 10.1136/gutjnl-2014-307843. [DOI] [PubMed] [Google Scholar]
- 5.Camilleri M, Stanghellini V. Current management strategies and emerging treatments for functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013;10:187–194. doi: 10.1038/nrgastro.2013.11. [DOI] [PubMed] [Google Scholar]
- 6.Aro P, Talley NJ, Agréus L, Johansson SE, Bolling-Sternevald E, Storskrubb T, Ronkainen J. Functional dyspepsia impairs quality of life in the adult population. Aliment Pharmacol Ther. 2011;33:1215–1224. doi: 10.1111/j.1365-2036.2011.04640.x. [DOI] [PubMed] [Google Scholar]
- 7.Lacy BE, Weiser KT, Kennedy AT, Crowell MD, Talley NJ. Functional dyspepsia: the economic impact to patients. Aliment Pharmacol Ther. 2013;38:170–177. doi: 10.1111/apt.12355. [DOI] [PubMed] [Google Scholar]
- 8.Vakil NB, Howden CW, Moayyedi P, Tack J. White Paper AGA: Functional Dyspepsia. Clin Gastroenterol Hepatol. 2017;15:1191–1194. doi: 10.1016/j.cgh.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 9.Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N. ACG and CAG Clinical Guideline: Management of Dyspepsia. Am J Gastroenterol. 2017;112:988–1013. doi: 10.1038/ajg.2017.154. [DOI] [PubMed] [Google Scholar]
- 10.Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010;59:1143–1153. doi: 10.1136/gut.2009.192757. [DOI] [PubMed] [Google Scholar]
- 11.Du LJ, Chen BR, Kim JJ, Kim S, Shen JH, Dai N. Helicobacter pylori eradication therapy for functional dyspepsia: Systematic review and meta-analysis. World J Gastroenterol. 2016;22:3486–3495. doi: 10.3748/wjg.v22.i12.3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tack J, Camilleri M. New developments in the treatment of gastroparesis and functional dyspepsia. Curr Opin Pharmacol. 2018;43:111–117. doi: 10.1016/j.coph.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 13.Lin Z, Eaker EY, Sarosiek I, McCallum RW. Gastric myoelectrical activity and gastric emptying in patients with functional dyspepsia. Am J Gastroenterol. 1999;94:2384–2389. doi: 10.1111/j.1572-0241.1999.01362.x. [DOI] [PubMed] [Google Scholar]
- 14.Stanghellini V, Tack J. Gastroparesis: separate entity or just a part of dyspepsia? Gut. 2014;63:1972–1978. doi: 10.1136/gutjnl-2013-306084. [DOI] [PubMed] [Google Scholar]
- 15.Pfaffenbach B, Adamek RJ, Bartholomäus C, Wegener M. Gastric dysrhythmias and delayed gastric emptying in patients with functional dyspepsia. Dig Dis Sci. 1997;42:2094–2099. doi: 10.1023/a:1018826719628. [DOI] [PubMed] [Google Scholar]
- 16.Lin X, Chen JZ. Abnormal gastric slow waves in patients with functional dyspepsia assessed by multichannel electrogastrography. Am J Physiol Gastrointest Liver Physiol. 2001;280:G1370–G1375. doi: 10.1152/ajpgi.2001.280.6.G1370. [DOI] [PubMed] [Google Scholar]
- 17.Vanheel H, Carbone F, Valvekens L, Simren M, Tornblom H, Vanuytsel T, Van Oudenhove L, Tack J. Pathophysiological Abnormalities in Functional Dyspepsia Subgroups According to the Rome III Criteria. Am J Gastroenterol. 2017;112:132–140. doi: 10.1038/ajg.2016.499. [DOI] [PubMed] [Google Scholar]
- 18.Enck P, Azpiroz F, Boeckxstaens G, Elsenbruch S, Feinle-Bisset C, Holtmann G, Lackner JM, Ronkainen J, Schemann M, Stengel A, Tack J, Zipfel S, Talley NJ. Functional dyspepsia. Nat Rev Dis Primers. 2017;3:17081. doi: 10.1038/nrdp.2017.81. [DOI] [PubMed] [Google Scholar]
- 19.Vanheel H, Vanuytsel T, Van Oudenhove L, Martinez C, Keita ÅV, Pardon N, Santos J, Söderholm JD, Tack J, Farré R. Impaired duodenal mucosal integrity and low-grade inflammation in functional dyspepsia. Gut. 2014;63:262–271. doi: 10.1136/gutjnl-2012-303857. [DOI] [PubMed] [Google Scholar]
- 20.Ma Y, Dong M, Zhou K, Mita C, Liu J, Wayne PM. Publication Trends in Acupuncture Research: A 20-Year Bibliometric Analysis Based on PubMed. PLoS One. 2016;11:e0168123. doi: 10.1371/journal.pone.0168123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen JDZ, Ni M, Yin J. Electroacupuncture treatments for gut motility disorders. Neurogastroenterol Motil. 2018;30:e13393. doi: 10.1111/nmo.13393. [DOI] [PubMed] [Google Scholar]
- 22.Kim KN, Chung SY, Cho SH. Efficacy of acupuncture treatment for functional dyspepsia: A systematic review and meta-analysis. Complement Ther Med. 2015;23:759–766. doi: 10.1016/j.ctim.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 23.Zeng F, Song WZ, Liu XG, Xie HJ, Tang Y, Shan BC, Liu ZH, Yu SG, Liang FR. Brain areas involved in acupuncture treatment on functional dyspepsia patients: a PET-CT study. Neurosci Lett. 2009;456:6–10. doi: 10.1016/j.neulet.2009.03.080. [DOI] [PubMed] [Google Scholar]
- 24.MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, Moher D STRICTA Revision Group. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): Extending the CONSORT statement. J Evid Based Med. 2010;3:140–155. doi: 10.1111/j.1756-5391.2010.01086.x. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu S, Peng S, Hou X, Ke M, Chen JD. Transcutaneous electroacupuncture improves dyspeptic symptoms and increases high frequency heart rate variability in patients with functional dyspepsia. Neurogastroenterol Motil. 2008;20:1204–1211. doi: 10.1111/j.1365-2982.2008.01164.x. [DOI] [PubMed] [Google Scholar]
- 27.Zeng F, Qin W, Ma T, Sun J, Tang Y, Yuan K, Li Y, Liu J, Liu X, Song W, Lan L, Liu M, Yu S, Gao X, Tian J, Liang F. Influence of acupuncture treatment on cerebral activity in functional dyspepsia patients and its relationship with efficacy. Am J Gastroenterol. 2012;107:1236–1247. doi: 10.1038/ajg.2012.53. [DOI] [PubMed] [Google Scholar]
- 28.Ji T, Li X, Lin L, Jiang L, Wang M, Zhou X, Zhang R, Chen JDz. An alternative to current therapies of functional dyspepsia: self-administrated transcutaneous electroacupuncture improves dyspeptic symptoms. Evid Based Complement Alternat Med. 2014;2014:832523. doi: 10.1155/2014/832523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jin Y, Zhao Q, Zhou K, Jing X, Yu X, Fang J, Liu Z, Zhu B. Acupuncture for Functional Dyspepsia: A Single Blinded, Randomized, Controlled Trial. Evid Based Complement Alternat Med. 2015;2015:904926. doi: 10.1155/2015/904926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu F, Tan Y, Huang Z, Zhang N, Xu Y, Yin J. Ameliorating Effect of Transcutaneous Electroacupuncture on Impaired Gastric Accommodation in Patients with Postprandial Distress Syndrome-Predominant Functional Dyspepsia: A Pilot Study. Evid Based Complement Alternat Med. 2015;2015:168252. doi: 10.1155/2015/168252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang CX, Guo LK. Dalitong granule combined with electroacupuncture in the treatment of functional dyspepsia: A randomized controlled trial. Chin J Integr Med. 2015;21:743–750. doi: 10.1007/s11655-015-2175-5. [DOI] [PubMed] [Google Scholar]
- 32.Ko SJ, Kuo B, Kim SK, Lee H, Kim J, Han G, Kim J, Kim SY, Jang S, Son J, Kim M, Lee H, Yeo I, Joo KR, Park JW. Individualized Acupuncture for Symptom Relief in Functional Dyspepsia: A Randomized Controlled Trial. J Altern Complement Med. 2016;22:997–1006. doi: 10.1089/acm.2016.0208. [DOI] [PubMed] [Google Scholar]
- 33.Qiang L, Jiang Y. Electroacupuncture for functional dyspepsia and the influence on serum Ghrelin, CGRP and GLP-1 levels. World J Acupunct-moxibustion. 2018;28:86–90. [Google Scholar]
- 34.Lahner E, Bellentani S, Bastiani RD, Tosetti C, Cicala M, Esposito G, Arullani P, Annibale B. A survey of pharmacological and nonpharmacological treatment of functional gastrointestinal disorders. United European Gastroenterol J. 2013;1:385–393. doi: 10.1177/2050640613499567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vijayvargiya P, Jameie-Oskooei S, Camilleri M, Chedid V, Erwin PJ, Murad MH. Association between delayed gastric emptying and upper gastrointestinal symptoms: a systematic review and meta-analysis. Gut. 2019;68:804–813. doi: 10.1136/gutjnl-2018-316405. [DOI] [PubMed] [Google Scholar]
- 36.Kindt S, Tack J. Impaired gastric accommodation and its role in dyspepsia. Gut. 2006;55:1685–1691. doi: 10.1136/gut.2005.085365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016 doi: 10.1053/j.gastro.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 38.Mukhtar K, Nawaz H, Abid S. Functional gastrointestinal disorders and gut-brain axis: What does the future hold? World J Gastroenterol. 2019;25:552–566. doi: 10.3748/wjg.v25.i5.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kalra SP, Dube MG, Sahu A, Phelps CP, Kalra PS. Neuropeptide Y secretion increases in the paraventricular nucleus in association with increased appetite for food. Proc Natl Acad Sci USA. 1991;88:10931–10935. doi: 10.1073/pnas.88.23.10931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khoo J, Rayner CK, Feinle-Bisset C, Jones KL, Horowitz M. Gastrointestinal hormonal dysfunction in gastroparesis and functional dyspepsia. Neurogastroenterol Motil. 2010;22:1270–1278. doi: 10.1111/j.1365-2982.2010.01609.x. [DOI] [PubMed] [Google Scholar]
- 41.Bueno L, Fioramonti J. Visceral perception: inflammatory and non-inflammatory mediators. Gut. 2002;51 Suppl 1:i19–i23. doi: 10.1136/gut.51.suppl_1.i19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanger GJ. Motilin, ghrelin and related neuropeptides as targets for the treatment of GI diseases. Drug Discov Today. 2008;13:234–239. doi: 10.1016/j.drudis.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 43.Jonsson BH, Hellström PM. Motilin- and neuropeptide Y-like immunoreactivity in a psychophysiological stress experiment on patients with functional dyspepsia. Integr Physiol Behav Sci. 2000;35:256–265. doi: 10.1007/BF02688788. [DOI] [PubMed] [Google Scholar]
- 44.Hu ML, Rayner CK, Wu KL, Chuah SK, Tai WC, Chou YP, Chiu YC, Chiu KW, Hu TH. Effect of ginger on gastric motility and symptoms of functional dyspepsia. World J Gastroenterol. 2011;17:105–110. doi: 10.3748/wjg.v17.i1.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mönnikes H, van der Voort IR, Wollenberg B, Heymann-Monnikes I, Tebbe JJ, Alt W, Arnold R, Klapp BF, Wiedenmann B, McGregor GP. Gastric perception thresholds are low and sensory neuropeptide levels high in helicobacter pylori-positive functional dyspepsia. Digestion. 2005;71:111–123. doi: 10.1159/000084625. [DOI] [PubMed] [Google Scholar]
- 46.Zhang S, Li S, Liu Y, Ye F, Yin J, Foreman RD, Wang D, Chen JDZ. Electroacupuncture via chronically implanted electrodes improves gastric dysmotility mediated by autonomic-cholinergic mechanisms in a rodent model of functional dyspepsia. Neurogastroenterol Motil. 2018;30:e13381. doi: 10.1111/nmo.13381. [DOI] [PubMed] [Google Scholar]
- 47.Zhou J, Li S, Wang Y, Foreman RD, Yin J, Zhang S, Chen JDZ. Inhibitory Effects and Mechanisms of Electroacupuncture via Chronically Implanted Electrodes on Stress-Induced Gastric Hypersensitivity in Rats With Neonatal Treatment of Iodoacetamide. Neuromodulation. 2017;20:767–773. doi: 10.1111/ner.12602. [DOI] [PubMed] [Google Scholar]
- 48.Fang J, Wang D, Zhao Q, Hong Y, Jin Y, Liu Z, Zhou K, Jing X, Yu X, Pan R, Chang A, Liu H, Zhu B. Brain-Gut Axis Modulation of Acupuncture in Functional Dyspepsia: A Preliminary Resting-State fcMRI Study. Evid Based Complement Alternat Med. 2015;2015:860463. doi: 10.1155/2015/860463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Van Oudenhove L, Aziz Q. The role of psychosocial factors and psychiatric disorders in functional dyspepsia. Nat Rev Gastroenterol Hepatol. 2013;10:158–167. doi: 10.1038/nrgastro.2013.10. [DOI] [PubMed] [Google Scholar]
- 50.Kano M, Dupont P, Aziz Q, Fukudo S. Understanding Neurogastroenterology From Neuroimaging Perspective: A Comprehensive Review of Functional and Structural Brain Imaging in Functional Gastrointestinal Disorders. J Neurogastroenterol Motil. 2018;24:512–527. doi: 10.5056/jnm18072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Front Neurosci. 2018;12:49. doi: 10.3389/fnins.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 53.Li H, He T, Xu Q, Li Z, Liu Y, Li F, Yang BF, Liu CZ. Acupuncture and regulation of gastrointestinal function. World J Gastroenterol. 2015;21:8304–8313. doi: 10.3748/wjg.v21.i27.8304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.MacPherson H, Tilbrook H, Agbedjro D, Buckley H, Hewitt C, Frost C. Acupuncture for irritable bowel syndrome: 2-year follow-up of a randomised controlled trial. Acupunct Med. 2017;35:17–23. doi: 10.1136/acupmed-2015-010854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bao C, Liu P, Liu H, Jin X, Calhoun VD, Wu L, Shi Y, Zhang J, Zeng X, Ma L, Qin W, Zhang J, Liu X, Tian J, Wu H. Different brain responses to electro-acupuncture and moxibustion treatment in patients with Crohn's disease. Sci Rep. 2016;6:36636. doi: 10.1038/srep36636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Liu Z, Yan S, Wu J, He L, Li N, Dong G, Fang J, Fu W, Fu L, Sun J, Wang L, Wang S, Yang J, Zhang H, Zhang J, Zhao J, Zhou W, Zhou Z, Ai Y, Zhou K, Liu J, Xu H, Cai Y, Liu B. Acupuncture for Chronic Severe Functional Constipation: A Randomized Trial. Ann Intern Med. 2016;165:761–769. doi: 10.7326/M15-3118. [DOI] [PubMed] [Google Scholar]
- 57.Ouyang H, Chen JD. Review article: therapeutic roles of acupuncture in functional gastrointestinal disorders. Aliment Pharmacol Ther. 2004;20:831–841. doi: 10.1111/j.1365-2036.2004.02196.x. [DOI] [PubMed] [Google Scholar]
- 58.Wang J, Sun L, Fei X, Zhu B. Chaos analysis of the electrical signal time series evoked by acupuncture. Chaos Solitons Fractals. 2007;33:901–907. [Google Scholar]
- 59.White A, Editorial Board of Acupuncture in Medicine. Western medical acupuncture: a definition. Acupunct Med. 2009;27:33–35. doi: 10.1136/aim.2008.000372. [DOI] [PubMed] [Google Scholar]
- 60.Ulett GA, Han S, Han J. Electroacupuncture: mechanisms and clinical application. Biol Psychiatry. 1998;44:129–138. doi: 10.1016/s0006-3223(97)00394-6. [DOI] [PubMed] [Google Scholar]
- 61.Mayor D. An exploratory review of the electroacupuncture literature: clinical applications and endorphin mechanisms. Acupunct Med. 2013;31:409–415. doi: 10.1136/acupmed-2013-010324. [DOI] [PubMed] [Google Scholar]
- 62.Han JS. Acupuncture: neuropeptide release produced by electrical stimulation of different frequencies. Trends Neurosci. 2003;26:17–22. doi: 10.1016/s0166-2236(02)00006-1. [DOI] [PubMed] [Google Scholar]
- 63.Wang JQ, Mao L, Han JS. Comparison of the antinociceptive effects induced by electroacupuncture and transcutaneous electrical nerve stimulation in the rat. Int J Neurosci. 1992;65:117–129. doi: 10.3109/00207459209003283. [DOI] [PubMed] [Google Scholar]
- 64.Lin X, Levanon D, Chen JD. Impaired postprandial gastric slow waves in patients with functional dyspepsia. Dig Dis Sci. 1998;43:1678–1684. doi: 10.1023/a:1018806913907. [DOI] [PubMed] [Google Scholar]
- 65.Friesen CA, Lin Z, Hyman PE, Andre L, Welchert E, Schurman JV, Cocjin JT, Burchell N, Pulliam S, Moore A, Lavenbarg T, McCallum RW. Electrogastrography in pediatric functional dyspepsia: relationship to gastric emptying and symptom severity. J Pediatr Gastroenterol Nutr. 2006;42:265–269. doi: 10.1097/01.mpg.0000189367.99416.5e. [DOI] [PubMed] [Google Scholar]
- 66.Sha W, Pasricha PJ, Chen JD. Rhythmic and spatial abnormalities of gastric slow waves in patients with functional dyspepsia. J Clin Gastroenterol. 2009;43:123–129. doi: 10.1097/MCG.0b013e318157187a. [DOI] [PubMed] [Google Scholar]
- 67.Tougas G, Eaker EY, Abell TL, Abrahamsson H, Boivin M, Chen J, Hocking MP, Quigley EM, Koch KL, Tokayer AZ, Stanghellini V, Chen Y, Huizinga JD, Rydén J, Bourgeois I, McCallum RW. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462. doi: 10.1111/j.1572-0241.2000.02076.x. [DOI] [PubMed] [Google Scholar]
- 68.Abell TL, Camilleri M, Donohoe K, Hasler WL, Lin HC, Maurer AH, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP, Shreve P, Szarka LA, Snape WJ, Jr, Ziessman HA American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–763. doi: 10.1111/j.1572-0241.2007.01636.x. [DOI] [PubMed] [Google Scholar]
- 69.Coleski R, Baker JR, Hasler WL. Endoscopic Gastric Food Retention in Relation to Scintigraphic Gastric Emptying Delays and Clinical Factors. Dig Dis Sci. 2016;61:2593–2601. doi: 10.1007/s10620-016-4173-7. [DOI] [PubMed] [Google Scholar]
- 70.Ghoos YF, Maes BD, Geypens BJ, Mys G, Hiele MI, Rutgeerts PJ, Vantrappen G. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1993;104:1640–1647. doi: 10.1016/0016-5085(93)90640-x. [DOI] [PubMed] [Google Scholar]
- 71.Choi MG, Camilleri M, Burton DD, Zinsmeister AR, Forstrom LA, Nair KS. Reproducibility and simplification of 13C-octanoic acid breath test for gastric emptying of solids. Am J Gastroenterol. 1998;93:92–98. doi: 10.1111/j.1572-0241.1998.092_c.x. [DOI] [PubMed] [Google Scholar]
- 72.Perri F, Bellini M, Portincasa P, Parodi A, Bonazzi P, Marzio L, Galeazzi F, Usai P, Citrino A, Usai-Satta P. (13)C-octanoic acid breath test (OBT) with a new test meal (EXPIROGer): Toward standardization for testing gastric emptying of solids. Dig Liver Dis. 2010;42:549–553. doi: 10.1016/j.dld.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 73.Tutuian R, Vos R, Karamanolis G, Tack J. An audit of technical pitfalls of gastric barostat testing in dyspepsia. Neurogastroenterol Motil. 2008;20:113–118. doi: 10.1111/j.1365-2982.2007.01005.x. [DOI] [PubMed] [Google Scholar]
- 74.Piessevaux H, Tack J, Walrand S, Pauwels S, Geubel A. Intragastric distribution of a standardized meal in health and functional dyspepsia: correlation with specific symptoms. Neurogastroenterol Motil. 2003;15:447–455. doi: 10.1046/j.1365-2982.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 75.Maurer AH, Parkman HP. Towards a Fuller Assessment of Gastric Motility in Patients With Upper GI Dyspepsia: Time to Accommodate! Am J Gastroenterol. 2019;114:16–18. doi: 10.1038/s41395-018-0404-1. [DOI] [PubMed] [Google Scholar]
- 76.Tack J, Caenepeel P, Piessevaux H, Cuomo R, Janssens J. Assessment of meal induced gastric accommodation by a satiety drinking test in health and in severe functional dyspepsia. Gut. 2003;52:1271–1277. doi: 10.1136/gut.52.9.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kindt S, Coulie B, Wajs E, Janssens J, Tack J. Reproducibility and symptomatic predictors of a slow nutrient drinking test in health and in functional dyspepsia. Neurogastroenterol Motil. 2008;20:320–329. doi: 10.1111/j.1365-2982.2008.01092.x. [DOI] [PubMed] [Google Scholar]
- 78.Tack J, Ly HG, Carbone F, Vanheel H, Vanuytsel T, Holvoet L, Boeckxstaens G, Caenepeel P, Arts J, Van Oudenhove L. Efficacy of Mirtazapine in Patients With Functional Dyspepsia and Weight Loss. Clin Gastroenterol Hepatol. 2016;14:385–392.e4. doi: 10.1016/j.cgh.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 79.van den Elzen BD, Bennink RJ, Holman R, Tytgat GN, Boeckxstaens GE. Impaired drinking capacity in patients with functional dyspepsia: intragastric distribution and distal stomach volume. Neurogastroenterol Motil. 2007;19:968–976. doi: 10.1111/j.1365-2982.2007.00971.x. [DOI] [PubMed] [Google Scholar]
- 80.Orthey P, Dadparvar S, Parkman HP, Maurer AH. Enhanced Gastric Emptying Scintigraphy to Assess Fundic Accommodation Using Intragastric Meal Distribution and Antral Contractility. J Nucl Med Technol. 2019;47:138–143. doi: 10.2967/jnmt.118.215566. [DOI] [PubMed] [Google Scholar]
- 81.Carbone F, Tack J. Gastroduodenal mechanisms underlying functional gastric disorders. Dig Dis. 2014;32:222–229. doi: 10.1159/000357854. [DOI] [PubMed] [Google Scholar]
- 82.Simrén M, Törnblom H, Palsson OS, van Tilburg MAL, Van Oudenhove L, Tack J, Whitehead WE. Visceral hypersensitivity is associated with GI symptom severity in functional GI disorders: consistent findings from five different patient cohorts. Gut. 2018;67:255–262. doi: 10.1136/gutjnl-2016-312361. [DOI] [PubMed] [Google Scholar]
- 83.Immke DC, Gavva NR. The TRPV1 receptor and nociception. Semin Cell Dev Biol. 2006;17:582–591. doi: 10.1016/j.semcdb.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 84.Hammer J, Führer M, Pipal L, Matiasek J. Hypersensitivity for capsaicin in patients with functional dyspepsia. Neurogastroenterol Motil. 2008;20:125–133. doi: 10.1111/j.1365-2982.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- 85.Führer M, Vogelsang H, Hammer J. A placebo-controlled trial of an oral capsaicin load in patients with functional dyspepsia. Neurogastroenterol Motil. 2011;23:918–e397. doi: 10.1111/j.1365-2982.2011.01766.x. [DOI] [PubMed] [Google Scholar]
- 86.Oshima T, Okugawa T, Tomita T, Sakurai J, Toyoshima F, Watari J, Yamaguchi K, Fujimoto K, Adachi K, Kinoshita Y, Kusunoki H, Haruma K, Miwa H. Generation of dyspeptic symptoms by direct acid and water infusion into the stomachs of functional dyspepsia patients and healthy subjects. Aliment Pharmacol Ther. 2012;35:175–182. doi: 10.1111/j.1365-2036.2011.04918.x. [DOI] [PubMed] [Google Scholar]
- 87.Jung HK, Talley NJ. Role of the Duodenum in the Pathogenesis of Functional Dyspepsia: A Paradigm Shift. J Neurogastroenterol Motil. 2018;24:345–354. doi: 10.5056/jnm18060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Gitter AH, Schulzke JD, Sorgenfrei D, Fromm M. Ussing chamber for high-frequency transmural impedance analysis of epithelial tissues. J Biochem Biophys Methods. 1997;35:81–88. doi: 10.1016/s0165-022x(97)00028-6. [DOI] [PubMed] [Google Scholar]
- 89.Ishigami H, Matsumura T, Kasamatsu S, Hamanaka S, Taida T, Okimoto K, Saito K, Minemura S, Maruoka D, Nakagawa T, Katsuno T, Fujie M, Arai M. Endoscopy-Guided Evaluation of Duodenal Mucosal Permeability in Functional Dyspepsia. Clin Transl Gastroenterol. 2017;8:e83. doi: 10.1038/ctg.2017.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Burns G, Carroll G, Mathe A, Horvat J, Foster P, Walker MM, Talley NJ, Keely S. Evidence for Local and Systemic Immune Activation in Functional Dyspepsia and the Irritable Bowel Syndrome: A Systematic Review. Am J Gastroenterol. 2019;114:429–436. doi: 10.1038/s41395-018-0377-0. [DOI] [PubMed] [Google Scholar]
- 91.Liebregts T, Adam B, Bredack C, Gururatsakul M, Pilkington KR, Brierley SM, Blackshaw LA, Gerken G, Talley NJ, Holtmann G. Small bowel homing T cells are associated with symptoms and delayed gastric emptying in functional dyspepsia. Am J Gastroenterol. 2011;106:1089–1098. doi: 10.1038/ajg.2010.512. [DOI] [PubMed] [Google Scholar]
- 92.Vandenberghe J, Dupont P, Van Oudenhove L, Bormans G, Demyttenaere K, Fischler B, Geeraerts B, Janssens J, Tack J. Regional cerebral blood flow during gastric balloon distention in functional dyspepsia. Gastroenterology. 2007;132:1684–1693. doi: 10.1053/j.gastro.2007.03.037. [DOI] [PubMed] [Google Scholar]
- 93.Zhou G, Liu P, Wang J, Wen H, Zhu M, Zhao R, von Deneen KM, Zeng F, Liang F, Gong Q, Qin W, Tian J. Fractional amplitude of low-frequency fluctuation changes in functional dyspepsia: a resting-state fMRI study. Magn Reson Imaging. 2013;31:996–1000. doi: 10.1016/j.mri.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 94.Liu P, Wang G, Zeng F, Liu Y, Fan Y, Wei Y, Qin W, Calhoun VD. Abnormal brain structure implicated in patients with functional dyspepsia. Brain Imaging Behav. 2018;12:459–466. doi: 10.1007/s11682-017-9705-z. [DOI] [PubMed] [Google Scholar]
- 95.Lorena SL, Figueiredo MJ, Almeida JR, Mesquita MA. Autonomic function in patients with functional dyspepsia assessed by 24-hour heart rate variability. Dig Dis Sci. 2002;47:27–31. doi: 10.1023/a:1013246900041. [DOI] [PubMed] [Google Scholar]
- 96.Friesen CA, Lin Z, Schurman JV, Andre L, McCallum RW. The effect of a meal and water loading on heart rate variability in children with functional dyspepsia. Dig Dis Sci. 2010;55:2283–2287. doi: 10.1007/s10620-009-1027-6. [DOI] [PubMed] [Google Scholar]
- 97.Barry S, Dinan TG. Functional dyspepsia: are psychosocial factors of relevance? World J Gastroenterol. 2006;12:2701–2707. doi: 10.3748/wjg.v12.i17.2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bennett EJ, Piesse C, Palmer K, Badcock CA, Tennant CC, Kellow JE. Functional gastrointestinal disorders: psychological, social, and somatic features. Gut. 1998;42:414–420. doi: 10.1136/gut.42.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hamilton J, Guthrie E, Creed F, Thompson D, Tomenson B, Bennett R, Moriarty K, Stephens W, Liston R. A randomized controlled trial of psychotherapy in patients with chronic functional dyspepsia. Gastroenterology. 2000;119:661–669. doi: 10.1053/gast.2000.16493. [DOI] [PubMed] [Google Scholar]
- 100.Huang ZP, Yang XF, Lan LS, Liu T, Liu CL, Li JL, Liang ZH. Correlation between social factors and anxiety-depression in function dyspepsia: do relationships exist? Prz Gastroenterol. 2014;9:348–353. doi: 10.5114/pg.2014.47897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Jiang SM, Jia L, Lei XG, Xu M, Wang SB, Liu J, Song M, Li WD. Incidence and psychological-behavioral characteristics of refractory functional dyspepsia: a large, multi-center, prospective investigation from China. World J Gastroenterol. 2015;21:1932–1937. doi: 10.3748/wjg.v21.i6.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lee KJ, Demarchi B, Demedts I, Sifrim D, Raeymaekers P, Tack J. A pilot study on duodenal acid exposure and its relationship to symptoms in functional dyspepsia with prominent nausea. Am J Gastroenterol. 2004;99:1765–1773. doi: 10.1111/j.1572-0241.2004.30822.x. [DOI] [PubMed] [Google Scholar]