Like severe acute respiratory syndrome coronavirus (SARS-CoV), the new coronavirus SARS-CoV-2, which is causing the epidemic coronavirus disease 2019 (COVID-19), enters human cells by binding to angiotensin-converting enzyme-2 (ACE2) although with a higher affinity.1 Once attached to ACE2, the viral spike protein is primed by the host serine protease TMPRSS2, which ultimately allows fusion of viral and cellular membranes.
ACE2 is a key protein of the protective branch of the renin-angiotensin system, which converts angiotensin (Ang) II, the main biologically active peptide of the RAS, into its physiological antagonist Ang-(1-7). ACE2 also metabolizes Ang I into Ang-(1-9), which is then converted into Ang-(1-7) by angiotensin-converting enzyme. Ang-(1-7) opposes the vasoconstrictor, proinflammatory, prooxidant, proproliferative, or profibrotic actions exerted by Ang II via AT1 receptors (Figure).
Figure.
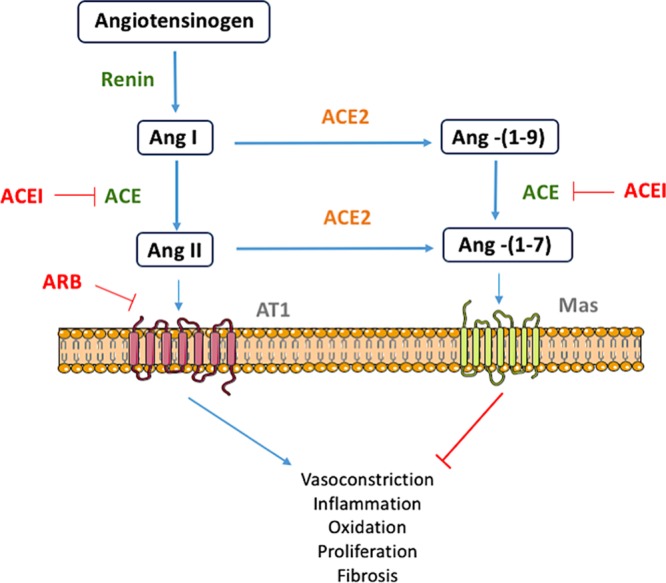
Diagram representing the main metabolic pathways driven by angiotensin-converting enzyme (ACE) and angiotensin-converting enzyme-2 (ACE2) in the renin-angiotensin system. The pharmacological targets for ACE inhibitors (ACEI) and angiotensin AT1 receptors blockers (ARB) are also shown. Ang indicates angiotensin.
The binding of SARS-CoV to ACE2 downregulates its expression, leading to increases in Ang II.1 ACE2 is expressed in many organs, but is particularly abundant in alveolar epithelial cells and vascular endothelial cells.2 This would explain why the lung is especially vulnerable to the new coronavirus. Indeed, the lethality of SARS-CoV has been shown to be dependent on the loss of key regulatory factors in the lung related to the downregulation of ACE2.3
Ang-(1-7) seems to be critical in protecting against lung inflammation and fibrosis. This heptapeptide inhibits alveolar cell apoptosis, attenuates endothelial cell activation and the loss of barrier function and edema, and limits the synthesis of proinflammatory and profibrotic cytokines. This is particularly relevant because both acute lung injury and acute respiratory distress syndrome are accompanied by a cytokine storm and an overwhelming inflammatory response.2 Indeed, activated endothelial cells are increasingly recognized as main orchestrators of the inflammatory response in acute respiratory distress syndrome.
Hypertension is a comorbidity that may exacerbate the severity of the new coronavirus infection.4 The underlying mechanisms are not clear, but the antihypertensive drugs such as AT1 receptor blockers or angiotensin-converting enzyme inhibitors increase ACE2 expression in animal models and humans. Because ACE2 is the receptor for the new coronavirus, it has been suggested that in patients treated with those drugs, the increase in the receptor may result in increased infection and therefore exacerbation of disease. Whether these treatments should be abandoned in favor of drugs neutral to ACE2, such as calcium channel blockers, is under discussion.5 However, there is at present no definitive evidence in humans in favor of this suggestion.
On the other hand, the protective effect of ACE2 overexpression is better understood and has led to the contrasting hypothesis that using AT1 receptor blockers might protect against viral-induced lung injury. In a model of SARS-CoV infection, the blockade of AT1 receptors revealed itself effective in attenuating pulmonary edema and severe lung injury.3 In addition to attenuating the binding of Ang II to its AT1 receptors, the beneficial actions of AT1 receptor blockers may be explained by 2 possible mechanisms: (1) the restored ACE2, normally decreased during the viral infection, helps reducing the concentrations of Ang II,3 and (2) there is an increased generation of the protective Ang-(1-7).
More clinical and experimental evidence is required to resolve this controversy. Meanwhile, we suggest that during viral infection, increasing the Ang-(1-7) concentration might be vital for protecting from endothelial cell activation and lung damage. The use of Ang-(1-7) or one of its mimetics should be considered among other strategies to prevent damage in high risk patients.
Sources of Funding
Dr Peiró is supported by a grant from Plan Nacional de I+D (SAF2017-84776-R).
Disclosures
None.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santos RAS, Sampaio WO, Alzamora AC, Motta-Santos D, Alenina N, Bader M, Campagnole-Santos MJ. The ACE2/angiotensin-(1-7)/MAS axis of the renin-angiotensin system: focus on angiotensin-(1-7). Physiol Rev. 2018;98:505–553. doi: 10.1152/physrev.00023.2016. doi: 10.1152/physrev.00023.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2005;11:875–879. doi: 10.1038/nm1267. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Liu L, Shan H, Lei C, Hui DSC, et al. Clinical characteristics of coronavirus disease 2019 in China [published online February 28, 2020]. N Engl J Med. doi: 10.1056/NEJMoa2002032. doi:10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? [published online March 11, 2020]. Lancet Respir Med. doi: 10.1016/S2213-2600(20)30116-8. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


