Abstract
Objective
The aim of this study was to evaluate the long-term follow-up and functional and radiological outcomes of minimally invasive medial plate osteosynthesis in distal tibia fractures.
Methods
From January 2011 to November 2015, we reviewed the medical records of 60 patients with 62 tibia fractures (41 men and 19 women; mean age: 45.3±14.9 years) who were treated with open reduction and internal fixation for distal tibia pilon fractures. The mean follow-up time after surgery was 42.7±4.6 months. Union time, coronal plan deformity, complication rates and AOFAS and Olerud-Molander functional outcome scores were evaluated.
Results
According to the AO/OTA classification, there were thirty four (54.8%) type 43-A fracture, eight (12.9%) type 43-B fractures, twenty (32.3%) type 43-C fractures. The average time for fracture union was 16.1 weeks. The mean AOFAS score was 86.6±9.1. The mean Olerud-Molander score was 85.6±9.8. There were four patients (6.5%) with a varus of less than 5°, two patients (3.2%) with a valgus of less than 5°, 39 patients (62.9%) with recurvatum (34 of them less than 5°; five of them less than 10°), and 14 patients (22.6%) with procurvatum (12 of them less than 5°; two of them less than 10°). The AOFAS and Olerud-Molander scores in the smoker and diabetic patients were significantly lower than the non-smoker (p=0.002; p=0.005) and non-diabetic patients (p=0.022, p=0.002). The duration of union was significantly higher in both diabetic (p=0.025) and smoker patients (p=0.041). There was no association between the fracture type and the presence of varus, valgus, recurvatum and rotation deformity. The AOFAS score, Olerud-Molander score and plantar-flexion were significantly higher in type A fractures than in type C fractures (p=0.021; p=0.030, and p=0.033, respectively). AOFAS score, Olerud-Molander score, plantar-flexion value did not differ between type B and type C fractures. There was no significant difference among the dorsi-flexion (p=0.211), the follow-up time (p=0.531) and duration of union (p=0.908) of type A, type B and type C fractures. Three patients with open fracture had delayed wound healing. One patient developed skin necrosis. They were treated by local wound care.
Conclusion
Minimally invasive medial plate osteosynthesis is a reliable method of treatment for tibial pilon fractures. This technique provides a high fracture healing rate and satisfying functional outcome with minimal wound healing complications. Sagittal plan deformity remains a common complication with minimally invasive medial plate osteosynthesis.
Level of Evidence
Level IV, Therapeutic Study
Keywords: Pilon fracture, Radiological outcomes, Olerud-Molander score, AOFAS score, MIPO
A pilon fracture is a comminuted fracture of the distal tibia describing the anatomical region extending 5 cm from the joint line. When the tibiotalar articular cartilage is involved, it is called plafound fractures (1).
Fractures of the distal end of the tibia that contain a significant portion of the weight-bearing articular surface are extremely challenging to treat. The involvement of the articular surface with extension into the distal tibial metaphysis is a characteristic of a pilon fracture. Pilon fractures account for only 5% to 10% of all fractures of the tibia, and it may involve less than 1% of fractures of the lower extremity, which are most common in the fourth decade of life, and it is more common in men (2). Pilon fractures are related to the high-energy mechanism that accompanying articular and metaphyseal comminution, chondral injuries, open wounds, deep abrasion, fracture blister, and compartment syndrome. Approximately 10% to 30% are open fractures. The treatment of these complex fractures remains challenging for orthopedic surgeons.
The ideal treatment method for pilon fractures is a controversial subject. The common method for the treatment of tibial pilon fracture is open reduction and internal fixation (ORIF). It was applied for the restoration of the anatomic structures of the joint surface; however, widespread dissection of the soft tissue leads to increased rates of infection and soft tissue complications. In addition, open reduction and plate fixation have been discovered to alter the blood supply of the tibia, which may lead to delayed union or nonunion (3, 4).
The minimally invasive plate osteosynthesis (MIPO) technique enables indirect reduction and stable fixation with minimal soft tissue dissection by maintaining the fracture hematoma (5). Fracture is primarily reduced by ligamentotaxis in percutaneous plating via minimally invasive technique (6–8).
The aim of this study was to evaluate the long-term follow-up, as well as the functional and radiological outcomes of MIPO in distal tibia fractures.
Material and Methods
This study was approved by the institutional review board of İstanbul Trainig and Research Hospital (2016/891) and the consent the patients were obtained. From January 2011 to November 2015, we reviewed 60 patients (62 tibia) who were treated with open reduction and internal fixation for distal tibia pilon fractures who could be postoperatively followed for three years or more.
The exclusion criteria included multiple fractures, previous foot or ankle surgery, accompanying neural or vascular pathology, neuropathic foot, pathologic fractures of the tibia, patients younger than 18 years, and the loss in the follow-up.
To precisely asses of the intra-articular tibia fractures, preoperative conventional radiographs and computerized tomography with three-dimensional analysis were used (Figure 1). The comparison views were used under surgical guidance in restoring normal anatomy in the contralateral foot.
Figure 1. a–c.
Fractures of the distal tibia in a 47-year-old-man anterior-posterior (a), lateral (b) preoperative radiography and 3D computerize tomography (c)
Fractures were classified using the AO/OAT classification system. Metaphyseal fractures with partial articular involvement (AO/OAT type 43-A, 43-B1, and 43-B2) were categorized as simple fractures, and articular fractures (AO/OAT Type 43-B3 and 43- C) were categorized as complex fractures, respectively (9). In addition, open fractures were categorized according to the Gustilo Anderson classifications (10).
Open fractures were treated initially with extensive debridement. A 3-day management of a first-generation cephalosporin and an aminoglycoside, supplemented with ampicillin were given for the cases open fractures. Tetanus prophylaxis was also administered. We did not use external fixator during the soft tissue healing period. As soon as the soft tissues and swelling started, i.e. skin wrinkling, the articular surface was reconstructed and simply reduced if necessary via stab incisions, and subsequently, the articular block was fixed to the diaphysis using a medially placed, percutaneously introduced flat scallop plate. The anatomically-contoured locking compression plate (TST® locking compression plate) was fixed in the Minimal Invasive Plate Osteosynthesis (MIPO) technique. The operations were performed under spinal anesthesia with the patient in a supine position and a tourniquet was applied. Reconstruction of the correct length of the fibula; anatomical reconstruction of the articular surface of the tibia; stable internal fixation by a percutaneous plate placed on the medial aspect of the tibia was controlled using fluoroscopy. When required, we used cannulated screws through k wires. As a result of the limited tibia medial longitudinal incision, we reached the help of plaque proximal stab incisions. We paid attention and made sure that there was at least 6 cm between two incisions. The skin was closed using Ethilon 3.0. No wound drain was used. A pressure bandage was then applied for a few days. The patients received cefazolin for 24 hours due to preoperative prophylaxis.
Sutures were postoperatively removed in the 3rd week while the patients avoided motion exercises during that period to lessen the shear forces under the flap. Protection was supplied by the use of a short-leg, non-weight-bearing cast for 6 weeks before beginning range-of-motion activities. After the soft tissues healed, and postoperative swelling diminished, non-weight-bearing ambulation with crutches was allowed for the patients. Therefore, gradual weight-bearing was encouraged. Full weight-bearing was allowed after 12 to 16 weeks depending on the radiographic evidence of healing.
The patients were asked to complete a questionnaire consisting of two outcome scores: the disease specific American Orthopedic Foot & Ankle Society (AOFAS) hindfoot and Olerud and Molander score (11, 12). Based on the AOFAS hidfoot sore, the results were classified as ‘excellent’, ‘good’, ‘fair’ and ‘poor’ when the total score ranges from 90 to 100, 75 to 89, 50 to 74, and below 49 points, respectively (11).
Postoperative radiography was evaluated with the Kellgren and Lawrence score.
Statistical Analysis
In the descriptive statistics of the data, the mean, standard deviation, frequency, median, lowest and highest value, and ratio values were used. The normality of distribution was measured using the Kolmogorov Smirnov test. In the analysis of quantitative independent data, the Kruskal-Wallis and the Mann-Whitney u-test were used. The Chi-Square test was used for the analysis of qualitative independent data and Fischer’s test was used when the Chi-Square test conditions were not provided. The data were analyzed using the Statistical Package for Social Sciences version 22.0 (IBM Corp.; Armonk, NY, USA). Statistically significant level was taken as p<0.05.
Results
The demographic features of the patients are summarized in Table 1. There were 19 (31.7%) females and 41 (68.3%) males. The average age of the patients at the time of surgery was 45.3±14.9 (range, 18–75 years). The fractures were at the right side in 32 (51.6%) and at the left side in 28 (45.2%) patients. Two patients (3.2%) were injured bilaterally, and one of them was a female and the other was a male. The mean follow-up after surgery was 42.7±4.6 months (range, 36–66 months). The mean operative time was 65 min (range, 45–125 min). The mean time until surgery was 2 days (range, 1–7 days).
Table 1.
Demographic features of the patients
| Age (years ) | 45.3±14.9 (18–75) | ||
| Sex | Female | 19 | 31.70% |
| Male | 41 | 68.30% | |
| Side | Left | 28 | 45.20% |
| Right | 32 | 51.60% | |
| Bilaterally | 2 | 3.20% | |
| Fracture types | A | 34 | 54.80% |
| type 43 A1 | 1 | 1.60% | |
| type 43 A2 | 13 | 20.90% | |
| type 43 A3 | 20 | 32.30% | |
| B | 8 | 12.90% | |
| type 43 B1 | 2 | 3.20% | |
| type 43 B2 | 5 | 8.10% | |
| type 43 B3 | 1 | 1.60% | |
| C | 20 | 32.30% | |
| type 43 C1 | 5 | 8.10% | |
| type 43 C2 | 10 | 16.10% | |
| type 43 C3 | 5 | 8.10% | |
| Smoking | 32 | 51.60% | |
| Diabetes | 5 | 8.10% | |
| Gustilo Anderson classification | 0 | 52 | 83.90% |
| I | 2 | 3.20% | |
| II | 3 | 4.80% | |
| III | 5 | 8.10% | |
| Associated injury | 13 | 21.00% | |
| Fibula fracture | 33 | 53.20% | |
| Fibula fixation | 23 | 37.10% | |
| Infection | 13 | 21.00% | |
| Syndesmosis | 2 | 3.20% | |
| fixation | |||
| Varus | 4 | 6.50% | |
| Valgus | 2 | 3.20% | |
| Recurvatum | 39 | 62.90% | |
| Procurvatum | 14 | 22.60% | |
| Rotation | 2 | 3.20% | |
| AOFAS score | 86.6±9.1 (62–100) | ||
| Olerud-Molander score | 85.6±9.8 (70–100) | ||
| Follow-up (month) | 42.7±4.6 (36–66) | ||
| Healing time (week) | 16.1±4.7 (11–48) | ||
| Dorsiflexion | 13.6±3.3 (10–20) | ||
| Plantarflexion | 46.7±6.4 (30–55) |
Mean± standard deviation (minumum-maximum value) Percentage%
Associated injuries were present in 13 patients (21%): ipsilateral lower leg fracture in 4 patients (30.8%), vertebra fractures in 5 patients (38.5%) and upper extremity fractures in 4 patients (30.8%). 32 patients (51.6%) were smokers and 8 patients (8.1%) had diabetes.
Accompanying fibula fractures were found in 33 (53.2%) patients. 69.7% of the patients with fibula fracture (23 patients) received fibula osteosythesis.
The average time for fracture union was 16.1±4.7 (range, 11–48 weeks). The mean range of motion was 13.6 ± 3.3 of dorsiflexion (range, 10–20 degrees), and 46.7±6.4 of plantar-flexion (range, 30–55 degrees) during the last follow-up (Figure 1).
All radiographs demonstrated healing of the fractures at the last follow-up (Figure 2). There were four patients (6.5%) with varus of less than 5°, two patients (3.2%) with valgus of less than 5°, 39 patients (62.9%) with recurvatum (34 of them less than 5°; five of them less than 10°), and 14 patients (22.6%) with procurvatum (12 of them less than 5°; two of them less than 10°).
Figure 2. a, b.
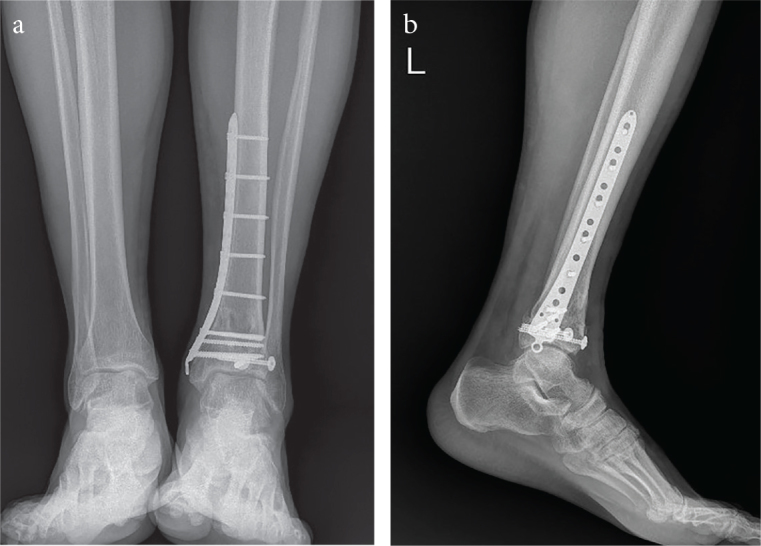
Patient treated with a MIPO anterior-posterior (a) and lateral (b) radiography
The mean AOFAS ankle hind food was 86.6±9.1 (range, 62–100 points). According to the AOFAS score, 27 patients (43.5%) had an excellent score, 26 patients (41.9%) a good result, and 9 patients (14.5%) a fair result. The mean Olerud-Molander score was 85.6±9.8 (range, 70–100 points) in the last follow-up.
The AOFAS score for the group of patients that are smokers (smoker group) was significantly lower (p=0.002) than the AOFAS score for the group of patients that are non-smokers (non-smoker group). The Olerud–Molander score was significantly lower for the smoker group (p=0.005) than for the non-smoker group. The duration of union was significantly higher for the smoker group (p=0.041) than for the non-smoker group. The open fracture (p=0.130), and classification of the fracture (p=0.280) were similar for the smoker and non-smoker groups (Table 2).
Table 2.
Functional scores and fracture healing time of the patients according to smoking habits
| Smoking (−) | Smoking (+) | p | ||||||
|---|---|---|---|---|---|---|---|---|
| AOFAS Score | 90.3 | ± | 6.9 | 83.1 | ± | 9.6 | 0.002 | m |
| Olerud-Molander Score | 89.2 | ± | 9.5 | 82.3 | ± | 9.0 | 0.005 | m |
| Fracture healing time (weeks) | 15.2 | ± | 2.3 | 17.1 | ± | 6.0 | 0.041 | m |
Mann-whitney U test
Mean±standard deviation
In the group of patients with diabetes (diabetic group), the AOFAS score was significantly lower (p=0.022) than for the group of patients that are non-diabetic (non-diabetic group). The Olerud-Molander score was significantly lower (p=0.002) for the diabetic group than in the non-diabetic group. The duration of union was significantly higher for diabetic group (p=0.025) than for the non-diabetic group. The open fracture (p=0.430) and classification of the fracture (p=0.080) were similar for the diabetic and non-diabetic groups (Table 3).
Table 3.
Functional scores and fracture healing time of the patients with regards to the presence of diabetes
| Diabetes mellitus (−) | Diabetes mellitus(+) | p | ||||||
|---|---|---|---|---|---|---|---|---|
| AOFAS Scor | 87.6 | ± | 8.4 | 75.6 | ± | 11.1 | 0.022 | m |
| Olerud-Molander Scor | 86.8 | ± | 9.2 | 72.0 | ± | 2.7 | 0.002 | m |
| Fracture healing time (weeks) | 15.5 | ± | 2.2 | 23.6 | ± | 13.7 | 0.025 | m |
Mann-whitney U test
Mean±standard deviation
The patients’ comprehensive results according to the fractures types are summarized in Table 4. The presence of varus, valgus, recurvatum and rotation was not significant compared to fracture type. The fracture Type A AOFAS score (p=0.021), Olerud-Molander score (p=0.030), and plantar-flexion (p=0.033) were significantly higher than the AOFAS score for fracture Type C. The difference in the AOFAS score, Olerud-Molander score, and plantar- flexion value was insignificant for fracture Type B and Type C fractures. Among fracture Type A, Type B, and Type C, the dorsiflexion (p=0.211), the follow-up time (p=0.531), and duration of union (p=0.908) were not significant (Table 4).
Table 4.
Patients comprehensive results according to the fractures types
| Fracture Type A | Fracture Type B | Fracture Type C | P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Varus | (−) | 33 | 97.1% | 8 | 100.0% | 17 | 85.0% | p>0.05 | |||
| (+) | 1 | 2.9% | 0 | 0.0% | 3 | 15.0% | |||||
| Valgus | (−) | 33 | 97.1% | 8 | 100.0% | 19 | 95.0% | p>0.05 | |||
| (+) | 1 | 2.9% | 0 | 0.0% | 1 | 5.0% | |||||
| Recurvatum | (−) | 13 | 38.2% | 3 | 37.5% | 7 | 35.0% | p>0.05 | |||
| (+) | 21 | 61.8% | 5 | 62.5% | 13 | 65.0% | |||||
| Procurvatum | (−) | 29 | 85.3% | 5 | 62.5% | 14 | 70.0% | p>0.05 | |||
| (+) | 5 | 14.7% | 3 | 37.5% | 6 | 30.0% | |||||
| Rotation | (−) | 34 | 100,0% | 8 | 100,0% | 18 | 90.0% | p>0.05 | |||
| (+) | 0 | 0,0% | 0 | 0,0% | 2 | 10.0% | |||||
| AOFAS Score | 89.4 | ± | 7.8 | 86.4 | ± | 7.1 | 81.9 | ± | 10.3 | 0.021 | |
| Olerud-Molander Score | 88.1 | ± | 8.8 | 87.5 | ± | 8.5 | 80.8 | ± | 10.4 | 0.030 | |
| Follow-up time (month) | 24.9 | ± | 4.0 | 23.5 | ± | 3.2 | 24.7 | ± | 5.9 | 0.531 | |
| Fracture healing time (week) | 15.6 | ± | 2.5 | 15.6 | ± | 2.1 | 17.4 | ± | 7.4 | 0.908 | |
| Dorsiflexion | 14.3 | ± | 3.5 | 13.1 | ± | 2.6 | 12.7 | ± | 3.0 | 0.211 | |
| Plantarflexion | 48.7 | ± | 5.8 | 45.0 | ± | 4.6 | 44.0 | ± | 7.0 | 0.033 | |
Kruskal-wallis (Mann-whitney U test ) /X2 Ki-kare test (Fischer test)
Mean±standard deviation/number%
Postoperative radiographic assessments showed no signs of post-traumatic arthrosis in 17 patients (27.4%), mild signs in 23 (37.1%), clear signs in 15 (24.2%), and severe signs in 7 (11.3%). This was in accordance with the Kellgren and Lawrence score (13).
Three patients with open fractures had delayed wound healing. One of these patients was diabetic; the other patient was a smoker and diabetic. They were treated by local wound care, debridement, daily change of dressing with povidone iodine, using intravenous antibiotics (first generation cephalosporin) for 2 weeks; this was according to the bacterial culture results. Methicillin-sensitive Staphylococcus aureus was present in the culture. One patient developed skin flap necrosis at the corner of the lateral L shaped incision. Debridement of the necrotic tissue yielded a good result.
Discussion
A number of different treatment strategies and fixation methods are presented for pilon fractures related to the development of novel treatment concepts. The aim of the surgical treatment of these fractures includes anatomical reduction of the articular surface, stabile fixation of the fracture, and restoration of the alignment. Closed reduction and application of percutaneous minimally invasive fixation methods have been recently recognized to allow indirect reduction and stable fixation preserved in fracture hematoma. Minimally invasive medial plate osteosynthesis may have a biological advantage over open reduction and internal fixations, especially when dealing with critical soft tissue conditions. Clinical studies using the minimally invasive technique showed good results with low rate of complications (14–17).
However, there are some challenges associated with the use of minimally invasive medial plate osteosynthesis in pilon fractures, including skin impingement, malunion, delayed union and intra-operative saphenous nerve, and vein injury (18, 19).
Although MIPO poses little or no damage to soft tissue. There are different criteria related to the acceptable level of malalignment.
According to Hasenboehler et al. when varus or valgus exceeds 5°, recurvatum or procurvatum exceeds 5°, when the rotation and shortening is beyond 5°, and shortening indicate significant malalignment (20). Helfet et al. showed that less than 5° varus, less than 10° valgus, and less than 10° recurvatum or procurvatum is acceptable (14). In this series, five patients had fracture union with recurvatum and two patients had union with procurvatum of less than 10°, without functional impairment. The alignment of these patients is regarded as normal according to Helfet et al. (14) while their alignment was regarded as abnormal according to Hasenboehler et al. (20). Angular deformities greater than 7 degrees, implant failure, and nonunion have been reported (21). In the long-term follow-up, we did not implant failure or nonunion of the cases. In addition, there was no loss of function in these patients. Therefore, the correction of the alignment was not planned.
The control of the reduction with scopy should be done on both the coronal and sagittal planes during the operation. Varus and valgus correction are provided in the coronal plane while recurvation and procurvation are corrected in the sagittal plane. It is important to take both side views with the scopy. In our cases, the correction of the deformation in the coronal plane was more precise. We had no coronal deformity of more than 5 degrees, but we had more than 5 degrees of sagittal deformity. The main problem of our patients is the sagittal instability. As similar results were obtained by Beytemur et al. (22). They retrospectively evaluated seventy-three simple intra- articular distal tibial fracture patients. They compared the midterm functional and radiographic results of minimally invasive plate osteosynthesis and intramedullary nailing of simple intra-articular distal tibial fractures. They concluded that recurvatum was more prevalent in the minimally invasive plate osteosynthesis group (22). We conclude that one minimally invasive plate applied at the medially may be insufficient to correct the deformity in the sagittal plane. More attention should be paid to the correction of the deformation in the sagittal plane in the minimally invasive medial plate osteosynthesis technique. Reduction and stability support can be provided with a cannulated screw.
The outcomes of these fractures mainly depend on the severity of the trauma, and the quality of surgical reduction and stability of the fixation (9). Locking screws fixed in the plate with the MIPO technique provides superior stability and minimizes the risk of loss of reduction. Fracture is primarily reduced by ligamentotaxis in percutaneous plating via minimally invasive technique. Subcutaneously applied plates have little or no effect on soft tissue and periosteal blood supply, and this leads to fewer soft tissue and healing complications (23). In this retrospective study, all fractures healed without bone healing problem.
The pilon fracture of the tibia is frequently seen due to high energy trauma, and nearly 25% of these fractures are open fractures (9). Ten of our patients (16.1%) had open fractures. In general, surgical treatment should be delayed until the soft tissues have healed and the swelling has begun to decrease. This usually requires a period of 7 to 14 days (range, 5 days to 7 weeks). Researchers have shown that delayed surgery for open tibial plafound fracture prevented postoperative soft tissue problems while it did not have influences on the postoperative functional results and the general health status (24). Minimal invasive methods of plating have been developed to decrease the wound problems accompanying with conventional open plating techniques (23). Zalavras et al. revealed that primary wound closure after a meticulous debridement did not increase the infection rate for open fractures (25). Parrett et al. noted that wounds should be closed within 7 days to decrease the risk of infection, osteomyelitis, nonunion, and tissue loss (26). Our patients underwent fracture stabilization and wound closure within a week after meticulous emergent debridement. Three patients had delayed wound healing. They were treated with local wound care and conservative method. Secondary contamination could be avoided when primary wound closure is applied; morbidity, as well as hospital stay and cost, is expected to decrease. We advise that open pilon fractures be closed primarily and stabilized percutaneously after thorough debridement.
The complex subgroup of AO/OAT Type C fractures are mainly due to high-energy trauma mechanisms which have been shown to have higher complication rates and poorer long-term results that relate to lower energy partial intra-articular Type B or extra-articular Type A fractures (27). Van den berg et al. revealed that complex fractures are associated with poor functional outcomes (28). Leonard et al. showed excellent AOFAS scores (83%) of patients with high energy pilon fractures following MIPO locking plating method. We achieved satisfactory results with our treatment method (29). We found that the mean AOFAS ankle was hindered by 86.6 points and the mean Olerud-Molander score was 85.6 points. In accordance with the findings from literature, MIPO of AO/OAT Type C distal tibia fractures were associated with poorer functional outcomes as compared to Type A and B fractures.
The amount of possible plantar flexion was greater than that of dorsiflexion. In this series, the level of plantar flexion was affected more in complex intra-articular fractures compare to simple fractures. In the postoperative rehabilitation process, consideration should be given to the evaluation of plantar flexion and dorsiflexion. The anatomical reduction of the fractures is effective in achieving the range of motion of the joint. In intra-articular fractures, care should be taken during surgery to ensure a perfect reduction of the fracture.
Tobacco abuse is known to be associated with an increased risk of bone healing complications (20). Despite that all fractures healed, we noticed that the time of fracture union was higher for patients that smoked compared to the patients that are non-smokers. In addition, functional outcomes were more favorable for patients that are non-smokers. The management of tibial pilon fractures in diabetic patients is difficult with a high rate of complications compared to non-diabetic patients (30). The duration of union was longer and the functional scores of the patients were worse for diabetic patients.
Minimally invasive medial plate osteosynthesis is a reliable method for the treatment of tibial pilon fractures. This technique provides a high fracture healing rate and satisfying functional outcome with minimal wound healing complications. Sagittal plan deformity remains a common complication with minimally invasive medial plate osteosynthesis.
MAIN POINTS.
Minimally invasive medial plate osteosynthesis is a reliable method of treatment for tibial pilon fractures.
This technique provides a high fracture healing rate and a satisfying functional outcome with minimal wound healing complications.
Sagittal plan deformity remains a common complication with minimally invasive medial plate osteosynthesis.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of İstanbul Training and Research Hospital (25/11/2016-891).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Author Contributions: Concept - A.B.; Design - A.B.,E.C.; Supervision - Y.0.; Resources - A.B.; Materials - A.B., Z.D.; Data Collection and/or Processing - Z.D.; Analysis and/or Interpretation - E.C.; Literature Search - E.C.; Writing Manuscript - E.C.; Critical Review - A.B., E.C.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Calori GM, Tagliabue L, Mazza E, de Bellis U, Pierannunzii L, Marelli BM, et al. Tibial pilon fractures: Which method of treatment? Injury. 2010;41:1183–90. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 2.Bourne RB. Pylon fractures of the distal tibia. Clin Orthop Relat Res. 1989:42–6. doi: 10.1097/00003086-198903000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Davidovitch RI, Elkhechen RJ, Romo S, Walsh M, Egol KA. Open reduction with internal fixation versus limited internal fixation and external fixation for high grade pilon fractures (OTA type 43C) Foot Ankle Int. 2011;32:955–61. doi: 10.3113/FAI.2011.0955. [DOI] [PubMed] [Google Scholar]
- 4.McCann PA, Jackson M, Mitchell ST, Atkins RM. Complications of definitive open reduction and internal fixation of pilon fractures of the distal tibia. Int Orthop. 2011;35:413–8. doi: 10.1007/s00264-010-1005-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ronga M, Shanmugam C, Longo UG, Oliva F, Maffulli N. Minimally invasive osteosynthesis of distal tibial fractures using locking plates. Orthop Clin North Am. 2009;40:499–504. doi: 10.1016/j.ocl.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Jha AK, Bhattacharyya A, Kumar S, Ghosh TK. Evaluation of results of minimally invasive plate osteosynthesis (MIPO) of distal tibial fractures in adults. J Indian Med Assoc. 2012;110:823–4. [PubMed] [Google Scholar]
- 7.Devkota P, Khan JA, Shrestha SK, Acharya BM, Pradhan NS, Mainali LP, et al. Minimally invasive plate osteosynthesis for distal tibial fractures. J Orthop Surg (Hong Kong) 2014;22:299–303. doi: 10.1177/230949901402200306. [DOI] [PubMed] [Google Scholar]
- 8.Vidovic D, Matejcic A, Ivica M, Jurisic D, Elabjer E, Bakota B. Minimally- invasive plate osteosynthesis in distal tibial fractures: Results and complications. Injury. 2015;46(Suppl 6):S96–99. doi: 10.1016/j.injury.2015.10.067. [DOI] [PubMed] [Google Scholar]
- 9.Korkmaz A, Ciftdemir M, Ozcan M, Copuroglu C, Saridogan K. The analysis of the variables, affecting outcome in surgically treated tibia pilon fractured patients. Injury. 2013;44:1270–4. doi: 10.1016/j.injury.2013.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. doi: 10.2106/00004623-197658040-00004. [DOI] [PubMed] [Google Scholar]
- 11.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–53. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 12.Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103:190–4. doi: 10.1007/BF00435553. [DOI] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Helfet DL, Shonnard PY, Levine D, Borrelli J. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(Suppl 1):A42–7. doi: 10.1016/S0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 15.Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28:159–62. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000;375:69–77. doi: 10.1097/00003086-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: Minimally invasive plate osteosynthesis. Injury. 2004;35:615–20. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 18.Cheng W, Li Y, Manyi W. Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Int Orthop. 2011;35:737–42. doi: 10.1007/s00264-010-1052-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int. 2002;23:818–24. doi: 10.1177/107110070202300908. [DOI] [PubMed] [Google Scholar]
- 20.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: A retrospective study of 32 patients. Injury. 2007;38:365–70. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 21.Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg. 2004;70:148–54. [PubMed] [Google Scholar]
- 22.Beytemur O, Baris A, Albay C, Yuksel S, Caglar S, Alagoz E. Comparison of intramedullary nailing and minimal invasive plate osteosynthesis in the treatment of simple intra-articular fractures of the distal tibia (AO-OTA type 43 C1-C2) Acta Orthop Traumatol Turc. 2017;51:12–6. doi: 10.1016/j.aott.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32:697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bacon S, Smith WR, Morgan SJ, Hasenboehler E, Philips G, Williams A, et al. A retrospective analysis of comminuted intra-articular fractures of the tibial plafond: Open reduction and internal fixation versus external Ilizarov fixation. Injury. 2008;39:196–202. doi: 10.1016/j.injury.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 25.Zalavras CG, Singh A, Patzakis MJ. Novel technique for medullary canal debridement in tibia and femur osteomyelitis. Clin Orthop Relat Res. 2007;461:31–4. doi: 10.1097/BLO.0b013e318098673f. [DOI] [PubMed] [Google Scholar]
- 26.Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg. 2006;117:1315–22. doi: 10.1097/01.prs.0000204959.18136.36. [DOI] [PubMed] [Google Scholar]
- 27.Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia--results in 20 patients. Injury. 2006;37:877–87. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 28.van den Berg J, Monteban P, Roobroeck M, Smeets B, Nijs S, Hoekstra H. Functional outcome and general health status after treatment of AO type 43 distal tibial fractures. Injury. 2016;47:1519–24. doi: 10.1016/j.injury.2016.04.009. [DOI] [PubMed] [Google Scholar]
- 29.Leonard M, Magill P, Khayyat G. Minimally-invasive treatment of high velocity intra-articular fractures of the distal tibia. Int Orthop. 2009;33:1149–53. doi: 10.1007/s00264-008-0629-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kline AJ, Gruen GS, Pape HC, Tarkin IS, Irrgang JJ, Wukich DK. Early complications following the operative treatment of pilon fractures with and without diabetes. Foot Ankle Int. 2009;30:1042–7. doi: 10.3113/FAI.2009.1042. [DOI] [PubMed] [Google Scholar]



