Abstract
Objective
The study aimed to identify the prevalence of sarcopenia in patients with osteoporotic hip fractures, investigate the anthropometric differences between sarcopenic and non-sarcopenic patients, and evaluate and compare the surgical outcomes between the two groups.
Methods
The study included 135 patients (35 men and 100 women; mean age: 74.1 years (range; 25–96)) who received surgical treatment for hip fracture between March 2014 and October 2016 and underwent whole-body dual-energy X-ray absorptiometry (DEXA). The skeletal muscle mass index (SMI) for diagnosis of sarcopenia was measured using whole-body DEXA. The following data were collected to compare the preoperative details of the sarcopenic and non-sarcopenic groups: SMI, age, sex, type of fracture, type of operation, BMI, obesity, American society of Anesthesiologists (ASA) class, pre-injury mobility score, BMD, and follow-up period. We compared clinical outcomes, including Harris Hip Score (HSS) and the walking ability at the last follow-up visit and radiologic outcomes, including non-union and the time to union.
Results
The average HHS and Parker’s mobility score at the last follow-up were 81.7 and 6.9 in the sarcopenic group, and 77.6 and 6.3 in the non-sarcopenic group, respectively (p=0.149 and 0.122). Non-union was identified 0 (0%) in sarcopenic group and 4 (10%) in non-sarcopenic group (p=0.288). The mean union timer of the patients in the sarcopenia group was 4.0 months and that of patients in the non-sarcopenic group was 4.4 months (p=0.210). Multiple regression analysis did not show any significant association between sarcopenia and postoperative surgical outcomes, including HHS, mobility score at the last follow up, non-union, and time to union.
Conclusion
Although the present study showed that the prevalence of sarcopenia in hip fracture patients was 45.9% (62/135), there was no clinical association between sarcopenia and postoperative. Based on these results, the clinical impact of sarcopenia may be confined to increased risk of hip fracture occurrence and surgical outcomes of hip fracture may not be affected by sarcopenia.
Level of Evidence
Level III, Therapeutic Study
Keywords: Sarcopenia, Prevalence, Hip fracture
A recent study in Asia showed that there has been a rapid increase in the total number of hip fractures in the last 10 years (1). Hip fractures among the elderly are considered critical because they are related to high mortality, reduced quality of life, and high socioeconomic burden (2–4). Conventionally, aging, sex, osteoporosis, and medical comorbidities have been accepted as important risk factors associated with hip fractures. Recently, sarcopenia, which is associated with increased functional impairment and physical disability, and results in a risk of falling, has received much attention in elderly patients with hip fractures (5–8).
Sarcopenia is characterized by progressive reduction of skeletal muscle and impaired muscle function (9). Sarcopenia and osteoporosis are a hazardous combination related to fragility in elderly people. Recent studies have reported that muscle and bone play important roles in endocrine organs that are related to muscle and bone formation and function (10–12). Therefore, many orthopedic surgeons have been begun paying closer attention to this medical condition, and many studies on sarcopenia in various cohorts have been published (1, 5–7). Although a few studies have reported the prevalence of sarcopenia in patients with hip fracture, the clinical impact of sarcopenia on surgical outcomes has never been reported, to the best of our knowledge.
Thus, the aims of this study were to 1) identify the prevalence of sarcopenia in patients with osteoporotic hip fractures, 2) investigate the anthropometric differences between patients with sarcopenia and those without, 3) compare the surgical outcomes between the two groups, and 4) analyze the clinical impact of sarcopenia on hip fracture. We hypothesized that there is high prevalence of sarcopenia in patients with osteoporotic hip fractures and that sarcopenia affects surgical outcomes adversely.
Methods
Study population
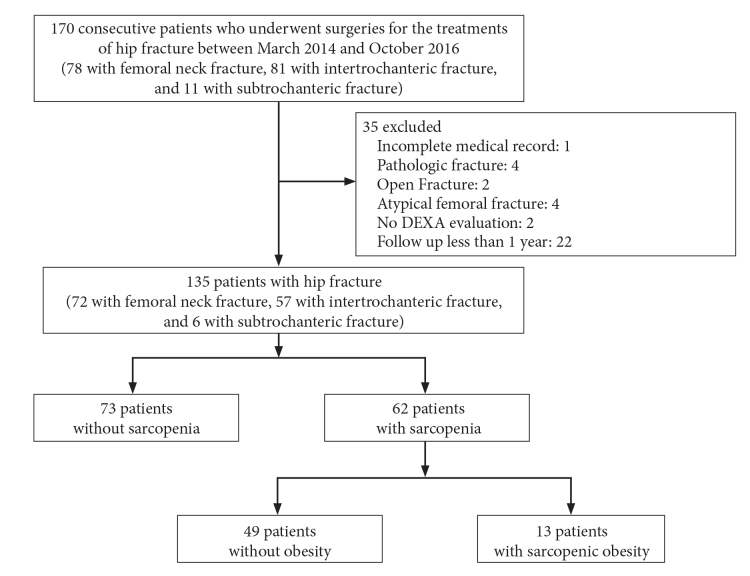
This study followed the guidelines of the Declaration of Helsinki and the Korean good clinical practice guidelines, and Pusan National University Hospital (PNUH) review board approval was obtained (H-11901-023-075). This retrospective cohort study was based on consecutively collected data in a tertiary university hospital. From March 2014 to October 2016, 170 patients (78 with femoral neck fractures, 81 with intertrochanteric fractures, and 11 with subtrochanteric fractures) underwent surgery for hip fractures. The inclusion criteria were as follows: 1) patients with osteoporotic hip fractures who received surgical treatment and 2) underwent whole-body dual-energy X-ray absorptiometry (DEXA). We excluded those patients who had any of the following: 1) a hip fracture due to a high-energy injury such as falling from a height or a vehicle accident; 2) incomplete medical records; 3) pathologic fracture; 4) open fracture; 5) atypical femoral fracture; 6) no whole-body DEXA; 7) follow up for less than 1 year (Figure 1). Osteoporotic hip fracture was defined as a fracture that occurs as a result of a minimal trauma, such as a fall from a standing height or less.
Figure 1.
Study flow chart
Measurement of body composition
Participants’ body compositions were measured using whole-body DEXA (Lumbar Prodigy Advance; GE Healthcare, Madison, WI, USA). The bone mineral content, fat mass, and lean soft tissue mass were measured separately for each part of the body, including the arms and legs. Since absolute muscle mass correlates with height, the skeletal muscle mass index (SMI) was calculated using the following formula: lean mass/height2 (kg/m2). The arm (or leg) SMI was defined as the arm (or leg) lean mass/height2 (kg/m2). Appendicular SMI was defined as the sum of arm and leg SMIs.
Sarcopenia was defined as an SMI below 5.4 kg/m2 in women and below 7.0 kg/m2 in men, according to the criteria of the Asia Working Group for Sarcopenia (AWGS) (3, 4). We simultaneously measured bone mineral density (BMD) using whole-body DEXA. Osteoporosis was defined as a BMD 2.5 standard deviations (SD) below the peak bone mass of a young, healthy, sex- and race-matched reference population according to the World Health Organization’s diagnostic classification (1, 3, 4). Obesity was defined as a BMI more than 25.0 kg/m2. Sarcobesity was defined as the co-existence of diminished muscle mass (sarcopenia) and increased fat mass (obesity) (1).
Assessment of outcome measures
The following data were collected to compare the preoperative details of the sarcopenic and non-sarcopenic groups: SMI, age, sex, type of fracture, type of operation, BMI, obesity, American society of Anesthesiologists (ASA) class, pre-injury mobility score, BMD, and follow-up period. We clinically evaluated hip function using Harris Hip Score (HHS) and walking ability at the last follow-up visit. The participant’s walking ability was graded from 0 to 9 using the mobility score of Parker and Palmer, which reflects the summed abilities to walk indoors and outdoors and to participate in social activities (1, 5). The assessment of radiologic outcomes evaluated non-union, union, and time to union in patients with peritrochanteric fractures that were treated with osteosynthesis using an intra-medullary nail, and in patients with femoral neck dislocation fractures that were treated with hip arthroplasty. Two orthopedic surgeons confirmed fracture union, which was defined as full, painless weight bearing with a bridging callus across at least three cortices on anteroposterior and lateral views of the femur (13). Non-union was defined as a definite fracture gap at a minimum of 9 months after injury with no visible, progressive signs of healing for three months.
Statistical Analysis
We compared the preoperative details and surgical outcomes of the groups using Pearson’s Chi-square test or Fisher’s exact test for categorical variables, and the independent Student’s test or Mann-Whitney U-test for continuous variables, as appropriate. Multiple regression analysis was used to identify the clinical impact of SMI on surgical outcomes. The regression parameters, including intercept (α), slope (β), and coefficient of determination (R2), were also calculated for the regression model. The Statistical Packages for the Social Science software version 21.0 (IBM Corp.; Armonk, NY, USA) was used for all statistical analyses. Statistical significance was set at p<0.05.
Results
One hundred thirty-five patients (35 men and 100 women) met the above criteria. Their mean age was 74.1 years (range: 25–96 years). The average SMI and overall prevalence of sarcopenia were 6.15 kg/m2 and 45.9% (62/135 patients), respectively. The prevalence of sarcopenia in women and men was 39% (39/100) and 65.7% (23/35), respectively. The prevalence of sarcopenia in men was significantly higher than in women (p=0.010).
The comparison of preoperative demographics and surgical outcomes between the sarcopenic and non-sarcopenic groups is presented in Table 1. The average SMI was 5.4 kg/m2±0.8 (range: 3.8–6.9) for the sarcopenic group, and 6.8 kg/m2±1.3 (5.4–10.0) for the non-sarcopenic group. The mean age of patients in the sarcopenic group was 71.6±12.9 years, while that of patients in the non-sarcopenic group was 75.8±9.3 years. Patients in the sarcopenic group were younger than those in the non-sarcopenia group (p=0.027). The mean BMI of patients in the non-sarcopenic group (21.9±3.1 kg/m2) was significantly (p=0.005) higher than that of patients in the sarcopenic group (23.5±3.5 kg/m2). The prevalence of obesity in the non-sarcopenic group was also higher than in the sarcopenic group. However, we could not identify any significant difference in postoperative surgical outcomes, including HHS, mobility score at the last follow up, dislocation of arthroplasty, union period, or non-union between the two groups.
Table 1.
Comparison of preoperative demographics and postoperative surgical outcomes between sarcopenic group and non-sarco-penic group
| Variables | Sarcopenic group | Non-sarcopenic group | p |
|---|---|---|---|
| Number (n, %) | 62 (45.9) | 73 (54.1) | - |
| SMI (kg/m2) | 5.4±0.8 (3.8–6.9) | 6.8±1.3 (5.4–10.0) | <0.001 |
| Age (years) | 71.6±12.9 (25–96) | 75.8±9.3 (51–94) | 0.027 |
| Female (n, %) | 39 (62.9) | 61 (83.6) | 0.010 |
| Type of fracture (n, %) | |||
| Femoral neck | 39 (62.9) | 33 (45.2) | 0.097 |
| Intertrochanteric | 20 (32.3) | 37 (50.7) | |
| Subtrochanteric | 3 (4.8) | 3 (4.1) | |
| Type of operation (n, %) | |||
| Bipolar hemiarthroplasty | 18 (29.0) | 20 (27.4) | 0.095 |
| Total hip arthroplasty | 20 (32.3) | 13 (17.8) | |
| Intramedullary nailing | 24 (38.7) | 40 (54.8) | |
| Body mass index (kg/m2) | 21.9±3.1 (12.9–30.1) | 23.5±3.5 (17.4–34.2) | 0.005 |
| Obesity (n, %) | 13 (21.0) | 36 (49.3) | 0.001 |
| ASA class (n, %) | |||
| ASA I, II | 28 (45.2) | 26 (35.6) | 0.293 |
| ASA III, IV | 34 (54.8) | 47 (64.4) | |
| Pre-injury mobility score | 7.5±1.6 (3–9) | 7.1±1.7 (3–9) | 0.270 |
| BMD (T-score) | |||
| L-spine | −2.3±1.8 (−5.6–2.8) | −2.1±1.7 (−5.8–1.5) | 0.579 |
| Femur | −2.6±1.2 (−6.1–0.9) | −2.5±1.3 (−4.9–0.6) | 0.727 |
| Follow up period | 17.2±5.4 (12–36) | 16.3±4.8 (12–33) | 0.316 |
| Harris hip score at the last follow up | 81.7±16.5 (50–100) | 77.6±16.7 (50–100) | 0.149 |
| Parker’s mobility score at the last follow up | 6.9±2.1 (3–9) | 6.3±2.3 (3–9) | 0.122 |
| Dislocation of arthroplasty | 2 (2.7) | 3 (9.1) | 0.658 |
| Union period in osteosynthesis | |||
| (month) | 4.0±1.0 (3–12) | 4.4±1.2 (3–9) | 0.210 |
| Non-union | 0 (0) | 4 (10) | 0.288 |
SMI: skeletal muscle mass index; BMD: bone mineral density; ASA: American society of Anesthesiologists
The age-specific prevalence of sarcopenia is shown in Figure 2. The prevalence of sarcopenia in patients in age groups of 60 or younger, 61–70, 71–80, 81–90, and 90 years or older were 70.6% (12/17), 47.4% (9/19), 46.2% (24/52), 34.2% (13/38), and 44.4% (4/9), respectively (Figure 2). The age-specific prevalence of sarcopenia showed a general decrease with increasing age, with a statistically significant correlation between them, as indicated by Spearman rank correlation analysis (p=0.037, rs=−0.900).
Figure 2.
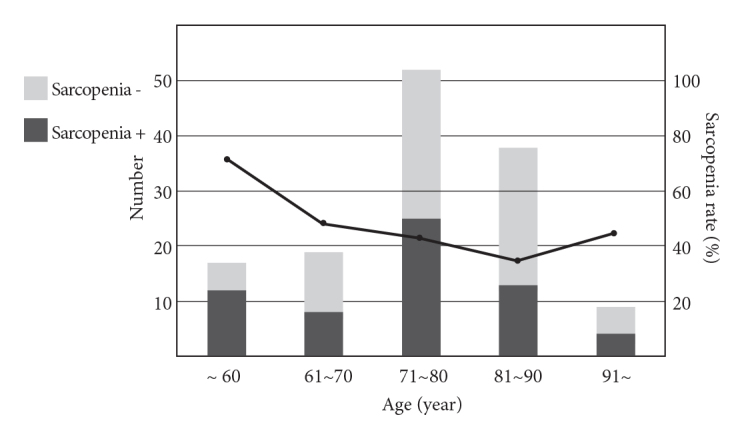
The number of cases and prevalence of sarcopenia according to age group
Multiple regression analysis showed that HHS at the last follow up was significantly associated with pre-injury mobility score and age. The mobility score at the last follow up also showed a significant association with pre-injury mobility score and age. SMI was significantly associated with L-spine BMD and BMI. However, SMI was not significantly associated with postoperative surgical outcomes, including Harris Hip Score and mobility score at the last follow up (Table 2).
Table 2.
Multiple regression analysis showing the factors associated with surgical outcomes, including Harris Hip Score and mobility score at the last follow up, and SMI
| Variables | Regression coefficient | R2 | p | |
|---|---|---|---|---|
|
| ||||
| α (intercept) | β (slope) | (coefficient of determination) | ||
| Harris Hip Score at the last follow up (dependent variable) | ||||
| Pre-injury mobility score | 31.587 | 8.358 | 0.152 | <0.001 |
| Age | −0.177 | |||
| Mobility score at the last follow up (dependent variable) | ||||
| Pre-injury mobility score | −0.455 | 1.156 | 0.833 | <0.001 |
| Age | −0.020 | |||
| Skeletal muscle mass index (dependent variable) | ||||
| L-spine BMD | 4.528 | 0.086 | 0.152 | 0.014 |
| BMI | 0.152 | |||
BMD: bone mineral density; BMI: bone mineral density
Discussion
Many recent studies have demonstrated that high prevalence of sarcopenia could be identified in patients with hip fracture (8, 14). These studies have suggested a clinical association between sarcopenia and hip fractures because sarcopenia may increase the risk of fall, which can be a leading cause of hip fracture among the elderly (15, 16). However, these studies are limited because they have only documented an anthropometric association between sarcopenia and hip fracture. In particular, few studies have evaluated the clinical impact of sarcopenia on hip fracture and the outcome of hip fracture surgery. Therefore, this study evaluated the surgical impact of sarcopenia on osteoporotic hip fractures based on pre- and postoperative values.
This study demonstrated that the prevalence of sarcopenia in women and men was 39% (39/100) and 65.7% (23/35), respectively. The prevalence of sarcopenia in patients with hip fractures reported here differed strongly from prevalence as reported in previous studies. Di Monaco et al. reported that the prevalence of sarcopenia in patients with hip fractures, based on the New Mexico Elder Health Survey (height-adjusted appendicular SMI <2 SD in a young reference group), was 64% in women and 95% in men (17). Gonzalez et al. reported that the prevalence of sarcopenia was 17.1% (18.3% in women and 12.4% in men), using the definition of the European Working Group on Sarcopenia in Older People (18). We believe that these differences in the prevalence of sarcopenia in patients with hip fractures are mainly attributable to the application of different criteria for sarcopenia. In the study by Yoo et al., which evaluated the prevalence of sarcopenia in 359 patients with hip fracture using the AWGS definition, the prevalence of sarcopenia in women and men was 44.3% and 68.2%, respectively (5). Since these findings are similar to our results, we believe that consistent outcomes can be achieved when the definition and criteria for sarcopenia are controlled.
We identified that there was a large difference in the prevalence of sarcopenia between men and women. This result may be related to the poorer medical condition or greater number of comorbidities for male patients with hip fractures than for female patients with hip fractures. However, Iannuzzi et al. showed that bioavailable testosterone could predict skeletal muscle mass in their cohort of men (19); many previous studies have shown that bioavailable testosterone is related to extremity strength and function, and testosterone treatment in older, hypogonadal men increased their hand grip strength and lower extremity muscle strength (19–23). Thus, we believe that a decrease in testosterone may be one of the multifactorial causes affecting the significant loss of skeletal muscle mass in male patients with hip fractures.
In this study, the age-specific prevalence of sarcopenia significantly decreased as age increased. Since sarcopenia is a degenerative change characterized by the progressive loss of skeletal muscle that accompanies aging, this result differed from our expectation. This finding could be due to selection bias in the present study, which can occasionally be found in retrospective cohort studies. However, in a study that evaluated the prevalence of sarcopenia in 239 Chinese geriatric patients in Hong Kong with hip fractures, Ho et al. reported that the mean relative SMI in women was lowest in patients aged 60–64 years (24). The authors mentioned that sarcopenia may be a risk factor in this group of relatively younger geriatric patients with hip fracture.
We could not identify any significant difference in postoperative surgical outcomes between sarcopenic and non-sarcopenic patients at the last follow up, including the Harris Hip Score, mobility score, dislocation of arthroplasty, union period, and non-union. Furthermore, multiple regression analysis showed that the SMI, the presence of sarcopenia, and sarcobesity were not significantly associated with clinical outcomes, including Harris Hip Score and mobility score at the last follow up. Based on these results, it is unlikely that the clinical impact of sarcopenia on surgical outcomes in patients with hip fractures is significant. However, because this finding may be related to the small sample size in the present study, further studies are needed to evaluate patient physical function and performance by measuring the short physical performance battery (using balance, gait speed, sit-to-stand), and grip strength. These studies would thus demonstrate the clinical impact of sarcopenia on surgical outcomes in patients with hip fractures.
Several limitations impacted the present study. First, this was a retrospective cohort study, and the sample size was relatively small, so this study may have suffered from selection bias. However, the comparison of preoperative details in this study between the two groups produced results that seem to be consistent with those of previous studies using the same criteria for sarcopenia (5). Second, we did not consider grip strength and gait speed for the diagnosis of sarcopenia preoperatively. However, it is impossible to measure gait speed preoperatively in patients with hip fractures. Although gait speed can be measured postoperatively, there is no standard guidance about when and how to measure postoperative gait speed. In addition, it is difficult to measure the impact of sarcopenia for postoperative gait speed quantitatively, since many factors may affect gait speed postoperatively. Third, we did not evaluate the rates of mortality at one year or 30 days after surgery, which may impact the relationship between sarcopenia and surgical outcomes of hip fracture due to relatively short follow up and small sample size. Finally, we could not find any significant differences in surgical outcomes between the sarcopenic and non-sarcopenic groups. Multiple regression analysis did not demonstrate that SMI, presence of sarcopenia, or sarcobesity was significantly associated with postoperative clinical outcomes, but instead showed that only two factors (preoperative mobility score and age) were significantly associated with surgical outcomes. However, to the best of our knowledge, this is the first study to evaluate the clinical association between sarcopenia and surgical outcomes in patients with hip fractures. Thus, although we did not verify our hypothesis that sarcopenia would negatively affect surgical outcomes, we believe that this evaluation is among the main strengths of our study.
There was no significant difference in surgical outcomes between sarcopenic and non-sarcopenic groups in the present study. However, we could identify unique patterns in the prevalence of sarcopenia according to age group. Based on these results, the clinical impact of sarcopenia may be confined to occurrence of hip fracture, and surgical outcomes of hip fracture may not be affected by sarcopenia. Moreover, further studies are needed to quantitatively evaluate the clinical impact of sarcopenia in patients with hip fracture and provide evidence for prevention and treatment of sarcopenia.
MAIN POINTS.
There has been a rapid increase in the total number of hip fractures in the last 10 years.
Sarcopenia, which is associated with increased functional impairment and physical disability, and results in a risk of falling, has received much attention in elderly patients with hip fractures.
Unique patterns in the prevalence of sarcopenia according to age group can be identified.
The clinical impact of sarcopenia may be confined to occurrence of hip fracture, and surgical outcomes of hip fracture may not be affected by sarcopenia.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Pusan National University Hospital.
Informed Consent: Written informed consent was obtained from patients and patients’ family members who participated in this study.
Author Contributions: Concept - N.H.M., W.C.S.; Design - N.H.M., W.C.S.; Supervision - K.T.S.; Resources - N.H.M.; Materials - N.H.M.; Data Collection and/or Processing - N.H.M., H.E.S.; Analysis and/or Interpretation - N.H.M., H.E.S.; Literature Search - N.H.M., W.C.S.; Writing Manuscript - N.H.M.; Critical Review - W.C.S., K.T.S.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Ha YC, Park YG, Nam KW, Kim SR. Trend in hip fracture incidence and mortality in Korea: A prospective cohort study from 2002 to 2011. J Korean Med Sci. 2015;30:483–8. doi: 10.3346/jkms.2015.30.4.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd BD, Williamson DA, Singh NA, et al. Recurrent and injurious falls in the year following hip fracture: A prospective study of incidence and risk factors from the Sarcopenia and Hip Fracture study. J Gerontol A Biol Sci Med Sci. 2009;64:599–609. doi: 10.1093/gerona/glp003. [DOI] [PubMed] [Google Scholar]
- 3.Chen LK, Lee WJ, Peng LN, Liu LK, Arai H, Akishita M. Recent advances in Sarcopenia research in Asia: 2016 update from the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2016;17:767. doi: 10.1016/j.jamda.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 4.Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: Consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- 5.Yoo JI, Ha YC, Kwon HB, Lee YK, Koo KH, Yoo MJ. High prevalence of Sarcopenia in Korean patients after hip fracture: A case-control study. J Korean Med Sci. 2016;31:1479–84. doi: 10.3346/jkms.2016.31.9.1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ji HM, Han J, Jin DS, Suh H, Chung YS, Won YY. Sarcopenia and sarcopenic obesity in patients undergoing orthopedic surgery. Clin Orthop Surg. 2016;8:194–202. doi: 10.4055/cios.2016.8.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hida T, Ishiguro N, Shimokata H, et al. High prevalence of sarcopenia and reduced leg muscle mass in Japanese patients immediately after a hip fracture. Geriatr Gerontol Int. 2013;13:413–20. doi: 10.1111/j.1447-0594.2012.00918.x. [DOI] [PubMed] [Google Scholar]
- 8.Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: A systematic review and meta-analysis. J Am Geriatr Soc. 2004;52:1121–9. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- 9.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age ageing. 2010;39:412–23. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fukumoto S, Martin TJ. Bone as an endocrine organ. Trends Endocrinol Metab. 2009;20:230–6. doi: 10.1016/j.tem.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Pratesi A, Tarantini F, Di Bari M. Skeletal muscle: An endocrine organ. Clin Cases Miner Bone Metab. 2013;10:11–4. doi: 10.11138/ccmbm/2013.10.1.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DiGirolamo DJ, Kiel DP, Esser KA. Bone and skeletal muscle: Neighbors with close ties. J Bone Miner Res. 2013;28:1509–18. doi: 10.1002/jbmr.1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Corrales LA, Morshed S, Bhandari M, Miclau T., 3rd Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–8. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Landi F, Liperoti R, Russo A, et al. Sarcopenia as a risk factor for falls in elderly individuals: Results from the ilSIRENTE study. Clin Nutr. 2010;31:652–8. doi: 10.1016/j.clnu.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Flicker L, MacInnis RJ, Stein MS, et al. Should older people in residential care receive vitamin D to prevent falls? Results of a randomized trial. J Am Geriatr Soc. 2005;53:1881–8. doi: 10.1111/j.1532-5415.2005.00468.x. [DOI] [PubMed] [Google Scholar]
- 16.Hida T, Ishiguro N, Shimokata H, et al. High prevalence of sarcopenia and reduced leg muscle mass in Japanese patients immediately after a hip fracture. Geriatr Gerontol Int. 2013;13:413–20. doi: 10.1111/j.1447-0594.2012.00918.x. [DOI] [PubMed] [Google Scholar]
- 17.Di Monaco M, Castiglioni C, Vallero F, Di Monaco R, Tappero R. Sarcopenia is more prevalent in men than in women after hip fracture: A cross-sectional study of 591 inpatients. Arch Gerontol Geriat. 2012;55:48–52. doi: 10.1016/j.archger.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Gonzalez-Montalvo JI, Alarcon T, Gotor P, et al. Prevalence of sarcopenia in acute hip fracture patients and its influence on short-term clinical outcome. Geriatr Gerontol Int. 2016;16:1021–7. doi: 10.1111/ggi.12590. [DOI] [PubMed] [Google Scholar]
- 19.Iannuzzi-Sucich M, Prestwood KM, Kenny AM. Prevalence of sarcopenia and predictors of skeletal muscle mass in healthy, older men and women. J Gerontol A Biol Sci Med Sci. 2002;57:772–7. doi: 10.1093/gerona/57.12.M772. [DOI] [PubMed] [Google Scholar]
- 20.van den Beld AW, de Jong FH, Grobbee DE, Pols HAP, Lamberts SWJ. Measures of bioavailable serum testosterone and estradiol and their relationships with muscle strength, bone density, and body composition in elderly men. J Clin Endocr Metab. 2000;85:3276–82. doi: 10.1210/jc.85.9.3276. [DOI] [PubMed] [Google Scholar]
- 21.Perry HM, Miller DK, Patrick P, Morley JE. Testosterone and leptin in older African-American men: Relationship to age, strength, function, and season. Metabolism. 2000;49:1085–91. doi: 10.1053/meta.2000.7710. [DOI] [PubMed] [Google Scholar]
- 22.Sih R, Morley JE, Kaiser FE, Perry HM, Patrick P, Ross C. Testosterone replacement in older hypogonadal men: A 12-month randomized controlled trial. J Clin Endocr Metab. 1997;82:1661–7. doi: 10.1210/jcem.82.6.3988. [DOI] [PubMed] [Google Scholar]
- 23.Morley JE, Perry HM, Kaiser FE, et al. Effects of Testosterone replacement therapy in old hypogonadal males - a preliminary-study. J Am Geriatr Soc. 1993;41:149–52. doi: 10.1111/j.1532-5415.1993.tb02049.x. [DOI] [PubMed] [Google Scholar]
- 24.Ho AWH, Lee MML, Chan EWC, et al. Prevalence of pre-sarcopenia and sarcopenia in Hong Kong Chinese geriatric patients with hip fracture and its correlation with different factors. Hong Kong Med J. 2016;22:23–9. doi: 10.12809/hkmj154570. [DOI] [PubMed] [Google Scholar]