Abstract
The Latinx population in the United States is disproportionately affected by HIV. Our community-based participatory research partnership developed, implemented and evaluated a Spanish-language peer navigation intervention designed to increase HIV testing and condom use among social networks of immigrant Spanish-speaking Latinx gay, bisexual and other men who have sex with men (GBMSM) and transgender women (TW). We randomized 21 social networks of Latinx GBMSM and TW, ages 18–55 years, to the intervention, known as HOLA, or a waitlist control group. Social network participants (n = 166) completed structured assessments at baseline and 12-month follow-up (24 months after baseline). Follow-up retention was 95%. Individual in-depth interviews with a sample of participants documented their intervention-related experiences, needs, and priorities to inform future research. At follow-up, HOLA participants reported increased HIV testing (adjusted odds ratio = 8.3; 95% CI = 3.0–23.0; P < 0.0001). All study participants reported increased condom use; there was no significant difference between HOLA and waitlist control participants. In-depth interviews identified critical intervention elements and impacts and community needs and priorities. The HOLA intervention is effective for increasing HIV testing among Latinx GBMSM and TW, an initial step within the HIV prevention and care continua, and may be adaptable to promote pre-exposure prophylaxis uptake.
Introduction
The United States has a large and rapidly growing Latinx population. Over the past decade, the Latinx (Latinx is a gender-neutral term used in lieu of Latina and Latino.) population grew by 43% and became the largest racial/ethnic minority in the United States, having reached more than 59.9 million in 2018 [1]. The southern region of the United States has the fastest growth of the Latinx population compared with any other US region [2, 3], increasing by nearly 700% between 1990 and 2015 [4]. The burden of HIV is particularly heavy in the southern United States, which accounted for more than half of new HIV diagnoses in the country during 2018. That same year, HIV diagnosis rates per 100 000 population were 15.7 in the southern United States, compared with 10.0 in the northeastern, 9.3 in the western, and 7.2 in the midwestern regions [5].
The Latinx population is disproportionately affected by HIV and has the second highest rate of AIDS diagnoses of all racial/ethnic groups. Latinx persons accounted for about 18% of the US population but 27% of the total number of HIV diagnoses in 2018 [5]. HIV incidence among Latinx GBMSM increased by 30% from 2010 to 2017, while it remained relatively stable among non-Latinx Black GBMSM and decreased by 16% among non-Latinx White GBMSM [5]. More than one-third of Latinx persons diagnosed with HIV in the United States during 2017 were living in the southern United States, and the proportion of total HIV diagnoses in this region represented by Latinx gay, bisexual and other men who have sex with men (GBMSM) and transgender women (TW) is increasing [6, 7].
Current estimates suggest that about 14% of TW and 3% of transgender men in the United States are living with HIV [8], and Latinx TW are particularly affected [9–12]. Many TW have high rates of not being screened [9, 13], and less than half of all TW with HIV know their status [14].
Despite the disproportionate burden of HIV among the US Latinx population, few strategies have been found to reduce the disproportionate burden of HIV among Latinx GBMSM and TW [15–17]. Thus, our community-based participatory research (CBPR) partnership developed HOLA, a community-level, Spanish-language peer navigation intervention for Latinx GBMSM and TW that grew out of our successful HoMBReS [18, 19] and HoMBReS por un Cambio [19] interventions. These interventions increased HIV testing and condom use among predominately heterosexual, social networks of Spanish-speaking Latinx men through peer navigation.
HOLA was developed to promote HIV testing and condom use among Latinx GBMSM and TW by harnessing natural helping through the deliberate selection, careful training, and ongoing support of Latinx GBMSM and TW to serve as community peer navigators. These navigators, known as Navegantes (Navigators), are informal, lay community leaders, who share similar backgrounds and demographic characteristics of the target community. Navegantes work within their existing social networks of Latinx GBMSM and TW to increase awareness and provide information, promote behavior change, bolster positive and reframe negative perceptions and attitudes and advocate on behalf of communities. Our objective was to test whether participants of social networks randomized to the HOLA intervention group increased HIV testing and condom use compared with participants of social networks randomized to the waitlist control group. We also sought to better understand the intervention-related experiences and the needs and priorities of Latinx GBMSM and TW through in-depth interviews with a sample of Navegantes and their social network participants.
Materials and methods
Community-based participatory research
This study was conducted by a multi-sectoral and long-standing CBPR partnership in North Carolina, United States, whose members strive to reduce health disparities from positive, ecological perspectives; equalize power among partners; harness the strengths and resources each partner; promote co-learning; and integrate knowledge acquisition and intervention [20–24]. The development, implementation and evaluation of the HOLA intervention was guided by our partnership, comprised of local Latinx community members; representatives from AIDS service organizations, public health departments and other community organizations; and academic researchers. Blending the lived experiences of community members, expertise of public health practitioners and other service providers, and sound science has the potential to develop deeper and more informed understandings of health and produce interventions that are more relevant, culturally congruent, and more likely to be successful [21, 24, 25].
The HOLA intervention
Briefly, the implementation phase of HOLA included 21 Latinx GBMSM and TW who were recruited to serve as Navegantes. Because the reputation of each Navegante as a leader within existing social networks is critical to the success of interventions implemented within social networks [18, 19, 26–28], we recruited Navegantes primarily through word-of-mouth.
Selection of Navegantes focussed on primary characteristics that the CBPR partnership identified as essential to Navegante success. Personal characteristics included attributes such as being a natural leader, dedicated and respectful and having a sense of humor. The potential Navegante had to be (or have the potential to be trained to be) comfortable talking and offering sound advice about sensitive issues (e.g. sexual health) and remaining discreet. Performance characteristics included the ability to read low-literacy study materials, complete low-literacy process evaluation data collection forms (i.e. Activity Logs), communicate orally, participate in meetings and work with members of their social networks. Situational characteristics included time availability and access to transportation.
Additionally, each Navegante was required to recruit eight non-overlapping members of their social networks who were GBMSM or TW and reported sex with men to participate in the study. After Navegantes were consented, they were taught how to explain details of the study to their friends.
Navegantes were trained by two Latinx gay men during four sessions of four hours each in private rooms within conveniently located Mexican restaurants. HOLA is based on social cognitive theory [29], empowerment education [30] and social support [28, 31]. The training included, the impact of HIV and sexually transmitted infections (STIs) on Latinx populations and sexual and gender minorities; HIV and STI prevention strategies; the process for accessing health services and testing for HIV and STIs; the correct use of condoms (including internal condoms); factors that influence health, including cultural expectations, values and reciprocal determinism; what it is like to live with HIV; the roles and responsibilities of Navegantes; and effective communication and social support strategies.
Training sessions were interactive and included opportunities for Navegantes to role play and practice both informal and formal helping. Each Navegante received a satchel that contained supplies and materials for distribution, including all presentations used during the training, pocket-sized cards outlining the locations of HIV and STI testing sites and depicting how to correctly use a condom, condoms, individually packaged water-based lubricants, a penis model, brochures about HIV and other STIs, and a DVD with five different CBPR partnership-developed video segments that summarized key points related to HIV prevention that Navegantes could screen with their social network members individually or in groups. After completion of their training, Navegantes participated in a graduation ceremony and received a framed signed certificate of completion.
Navegantes then met monthly for 12 months as a group with the HOLA project coordinator to obtain additional project and peer support, restock satchels with supplies, and submit their Activity Logs to document their helping activities. During this period, Navegantes promoted sexual health, particularly HIV and STI testing and condom use, among their social network members by carrying out informal and formal helping, using the skills and materials gained through the training.
Study design
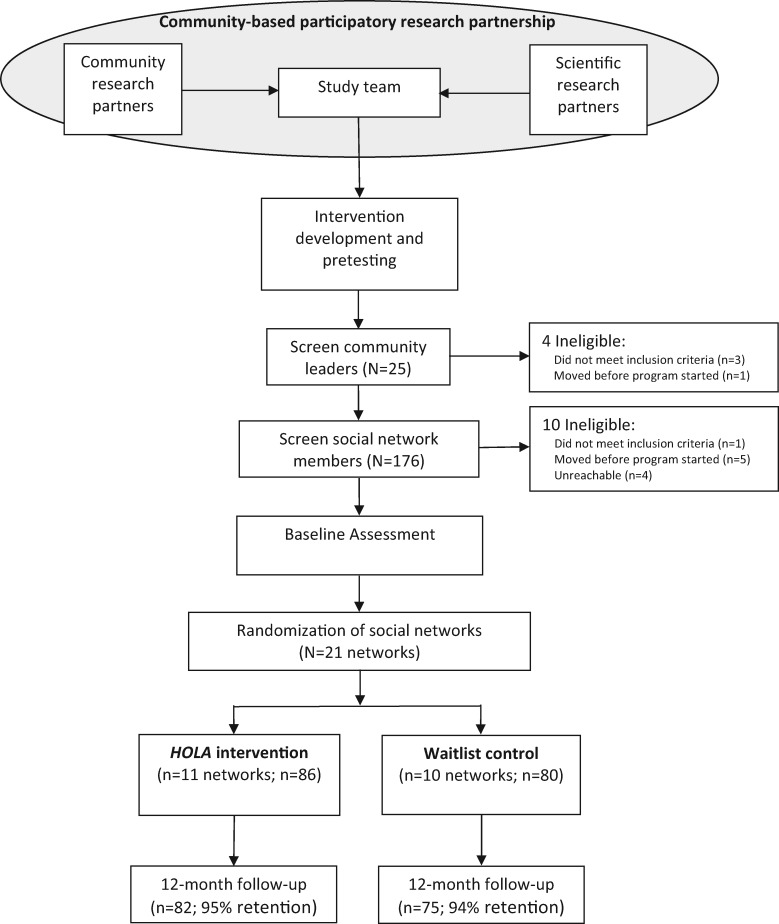
We used a two-group, randomized, intervention-waitlist control group design to evaluate the efficacy of HOLA. Twenty-one naturally existing social networks of Latinx GBMSM and TW were identified; each network had eight members plus one Navegante (Fig. 1). Baseline data were collected from each social network member, social networks were randomized into intervention (n = 11) and waitlist control (n = 10) groups using a standard numbers table [32].
Fig. 1.
Schematic of the research design to test the HOLA intervention among Latinx GBMSM and TW.
Navegantes were compensated $50 for each training session and each month for submitting their Activity Log. Navegantes also received a t-shirt, a baseball cap, a nametag identifying them as Navegantes, and satchel, all with the project logo on it (Fig. 2). Dinner was served at each training session. Social network participants were compensated for completing the baseline assessment ($30) and the 12-month follow-up assessment ($50). Each social network member also received a t-shirt, a baseball cap, a drawstring bag, and a rubber bracelet with the project name and telephone number printed on it to facilitate connectedness and retention [33].
Fig. 2.

The HOLA intervention logo.2
Measurement
Data were collected at baseline and 12-month post-intervention (i.e. 24 months after baseline data collection) from enrolled social network participants in both intervention and waitlist control groups. The assessment contained 112 items with predefined response categories. The assessment was read aloud by trained native Spanish-speaking staff members to assist with challenges associated with low-literacy rates and/or poor vision, was completed in 45–120 min, depending on the participant’s skip pattern. The follow-up window was 2 months; data were collected up to 1 month before and 1 month after the target follow-up date for each participant.
Demographics
Demographic data, including age in years, country of origin, educational attainment, employment, weekly income, sexual orientation, gender identity, acculturation and immigration status, were assessed at baseline using measures that have been validated among US Latinx populations [18, 34, 35].
Primary outcomes
We measured participants’ self-reports of HIV testing in the past 12 months and condom use during insertive or receptive anal sex with men and insertive vaginal or anal sex with women in the past 3 months in both the baseline and 12-month follow-up assessments.
Intervention-related targets
We assessed cognitive–psychosocial factors that HOLA was designed to influence, using Likert scales. We assessed HIV and STI knowledge—types of diseases, modes of transmission and prevention strategies—with 12 true–false items each [36] and condom use knowledge and skills with 18 correct–incorrect items [34].
We assessed participants’ condom use self-efficacy (α = 0.97) [37]; condom use expectancies (α = 0.93) [38], sexual communication skills and self-efficacy (α = 0.87) [34, 39], adherence to traditional notions of masculinity (α = 0.83) [40], homo-negativity (α = 0.83 [34, 41], fatalism (α = 0.92) [42], community attachment (α = 0.88) [40] and social support (α = 0.95) [43].
Higher scores indicated greater knowledge; condom use skills, self-efficacy and expectancies; sexual communication skills and self-efficacy; and higher adherence to traditional notions of masculinity, homo-negativity, fatalism, community attachment and social support.
Quantitative analysis
We used an intent-to-treat protocol to analyze participants’ outcomes relative to their assigned group (i.e. intervention or waitlist control [44]). At baseline, we used descriptive statistics to summarize the characteristics of intervention and waitlist participants. We assessed differences between the groups at baseline using the Student’s t-test for continuous variables and χ2 for categorical variables.
Our primary data analyses to evaluate the efficacy of the intervention compared rates of past 3-month condom use and past 12-month HIV testing reported by intervention and waitlist participants at post-intervention follow-up while adjusting for baseline rates. Statistical analysis used multivariable random effects logistic regression modeling that adjusted for potential clustering within social networks [45]. This adjustment accounted for the possibility that participants in the same network may exhibit more similar patterns of condom use and HIV testing at 12-month follow-up as participants in other social networks.
We adjusted models by baseline age, educational attainment and country of origin to obtain adjusted odds ratios (AORs) and computed the 95% CI and corresponding P values. We fit models using PROC GLIMMIX in SAS.
Qualitative analysis
Individual in-depth interviews were conducted with intervention Navegantes and a random sample of 11 intervention social network members (one from each social network) after 12-month follow-up. Standardized interview guides explored implementation experiences (e.g. overall satisfaction; challenges faced; preferred topics; and other lessons learned) and current issues affecting the health of Latinx GBMSM and TW (e.g. health needs and priorities; perceived barriers to care; and social media use) to inform future research and public health practice. Interviews were conducted in Spanish by native Spanish-speaking gay men. Interviews lasted 25–73 (mean = 43) min and were digitally recorded and transcribed; interview participants were compensated $40. Themes were identified through constant comparison, an approach to developing grounded theory, combining inductive coding with simultaneous comparison; initial observations were refined throughout data collection and analysis [46].
Human subjects protection oversight and approval were provided by the Wake Forest School of Medicine Institutional Review Board.
Results
The mean age of the 166 study’s network participants was 29.6 years old (SD = 6.7; range: 18–48); 48% had a high school diploma/GED; three-quarters were employed year-round; and 72% earned <$2000 per month. Most participants were foreign born: 75.3% in Mexico; 7.2% in Honduras; 4.2% in El Salvador; 3.0% in Guatemala; and 10.3% in other Central or South American or Caribbean countries or the United States. Nearly two-thirds (66.3%) reported speaking only/mostly Spanish. Foreign-born participants had been living in the United States for a mean of 10.1 years. In total, 73% reported being undocumented. Most of the sample identified as cisgender male and 11%, as male-to-female transgender. There were no significant differences between sociodemographic characteristics of intervention and waitlist control participants (Table I).
Table I.
Comparability of Latinx GBMSM and TW in the HOLA intervention and the waitlist control groups at baseline (n = 166)
| Characteristics | HOLA intervention group, n (%) or mean (SD; n = 86) | Waitlist group, n (%) or mean (SD; n = 80) | P-valuea |
|---|---|---|---|
| Age (years) | 28.7 (6.5) | 30.6 (6.7) | 0.2 |
| Age came to the United States | |||
| 16 or younger | 30 (36.1) | 17 (22.4) | 0.07 |
| 17 or older | 53 (63.9) | 59 (77.6) | |
| Country of origin | |||
| Mexico | 64 (75.3) | 63 (79.7) | 0.5 |
| Other | 21 (24.7) | 16 (20.3) | 0.6 |
| Educational attainment | |||
| Less than high school | 41 (50.0) | 40 (53.3) | 0.7 |
| High school (or GED) or more | 41 (50.0) | 35 (46.7) | |
| Employed year round | |||
| Yes | 64 (76.2) | 55 (74.3) | 0.8 |
| No | 20 (23.8) | 19 (25.7) | |
| Weekly income (US dollars) | |||
| $2000 or more | 22 (32.4) | 13 (22.8) | 0.4 |
| <$2000 | 46 (67.6) | 44 (77.2) | |
| Sexual identity | |||
| Heterosexual | 3 (3.5) | 0 (0.0) | |
| Gay | 68 (80.0) | 64 (84.2) | 0.1 |
| Bisexual | 14 (16.5) | 12 (15.8) | |
| Transgender identity | 6 (7.1) | 12 (15.8) | 0.1 |
| Time in the United States (years) | 10.5 (5.9) | 9.7 (4.8) | 0.2 |
| Acculturation | 24.5 (7.4) | 22.1 (7.5) | 0.1 |
P-value calculated by t-test statistics for mean and χ2 statistics for %.
Intervention effects
At 12-month follow-up, HOLA participants’ past 12-month HIV testing increased from 58.1% at baseline to 90.2% (P < 0.0001); waitlist control participants did not significantly change (55.0% versus 60.0%). HOLA participants’ past 3-month condom use significantly increased, from 34.9% at baseline to 63.4% at 12-month follow-up (P < 0.0001); waitlist control participants also significantly changed, from 25% at baseline to 50.7% at 12-month follow-up (P < 0.0001).
Adjusting for baseline testing and covariates, including age, educational attainment and country of origin, HOLA participants were 8.3 (95% CI = 3.0–23.0) times as likely as waitlist control participants to report past 12-month HIV testing (P < 0.0001; Table II) at follow-up. While condom use increased for participants in both the intervention and waitlist control groups, there was no significant difference in past 3-month condom use between groups.
Table II.
Latinx GBMSM and TW in the HOLA intervention and the waitlist control groups at baseline and 12-month follow-up
| Variable | Unadjusted rates/means |
||||||
|---|---|---|---|---|---|---|---|
| Baseline (%) |
Follow-up (%) |
||||||
| Intervention | Waitlist | P-value | Intervention | Waitlist | P-value | AOR or adjusted beta (95% CI), P-valuea | |
| HIV testing | 58.1 | 55.0 | 0.7 | 90.2 | 60.0 | <0.001 | 8.3 (3.0 to 23.0), <0.0001 |
| Past 3-month condom use | 34.9 | 25.0 | 0.2 | 63.4 | 50.7 | 0.2 | 1.6 (0.6 to 3.8), 0.3 |
| HIV knowledge | 8.5 | 8.2 | 0.5 | 11.1 | 8.8 | <0.001 | 2.2 (1.7 to 2.7), <0.0001 |
| STI knowledge | 4.9 | 5.6 | 0.1 | 9.4 | 6.2 | <0.001 | 3.3 (2.5 to 4.1), <0.001 |
| Condom skills | 14.3 | 14.5 | 0.5 | 17.2 | 15.0 | 0.0002 | 2.0 (1.2 to 2.7), <0.0001 |
| Condom efficacy | 4.4 | 4.3 | 0.7 | 4.7 | 4.4 | 0.1 | 6.7 (2.9 to 10.6), 0.0008 |
| Condom expectancy | 3.0 | 3.1 | 0.7 | 3.0 | 3.0 | 0.9 | 0.5 (−3.0 to 4.1), 0.8 |
| Sexual communication | 2.4 | 2.6 | 0.6 | 3.0 | 2.6 | 0.1 | 0.5 (−0.1 to 1.1), 0.09 |
| Masculinity | 52.5 | 52.5 | 0.9 | 52.2 | 54.0 | 0.3 | −1.1 (−3.8 to 1.5), 0.4 |
| Homo−negativity | 36.2 | 36.1 | 0.9 | 39.3 | 38.4 | 0.5 | 0.8 (−2.6 to 4.2), 0.7 |
| Fatalism | 43.6 | 44.5 | 0.7 | 42.9 | 46.8 | 0.1 | −3.6 (−7.6 to 0.5), 0.09 |
| Attachment | 4.1 | 3.7 | 0.2 | 4.2 | 4.1 | 0.8 | −0.6 (−1.8 to 0.5), 0.3 |
| Social support | 3.1 | 3.0 | 0.4 | 3.1 | 3.0 | 0.6 | 0.2 (−6.3 to 6.7), 0.95 |
AORs were based on multivariable random-effect logistic regression models accounting for social network clustering, baseline rates, educational attainment and country of origin.
Bold values are significant at P <0.05
We also observed significant differences in some intervention-related targets from baseline to 12-month follow-up (Table II). When compared with waitlist control participants at 12-month follow-up, HOLA participants had increases in HIV (P < 0.001), STI (P < 0.001) knowledge and condom use skills (P < 0.0002). There were no statistically significant differences in condom use efficacy and expectancies, sexual communication, adherence to traditional notions of masculinity, homo-negativity, fatalism, community attachment and social support.
Qualitative findings
Participant intervention experiences
We identified eight themes related to participant intervention experiences that we organized into three domains (Table III). First, participants noted the importance of the careful selection, training and support of Navegantes and reported that Navegantes must be individuals who are already viewed as community leaders, respected, and trusted within their social networks before they are selected. They also must be motivated to help others. Participants reported that the intervention reflected the lived experiences of participants and prepared Navegantes to promote sexual health within their social networks. Navegantes also indicated that the monthly group meetings with the project coordinator were critical for social support and problem solving.
Table III.
Participant experiences with HOLA intervention implementation: domains, themes and select quotations
| Navegante Selection, Training, and Support |
| 1. Navegantes must be viewed as leaders, respected, and trusted within their social networks, and they must be motivated to help others. |
| “She was very trustworthy all the time. She always knew how to listen and was well informed. Before she was a Navegante, she was already my friend, so I have a lot, a lot, of trust in her.” (Social network member #5) |
| “[Navegantes should be] people who are committed to providing support, so that they can become the right hand for all of us… So that we feel able to talk to them or approach them, because as a community we are always in need of somewhere to go to get support.” (Social network member #4) |
| 2. The HOLA intervention Navegante training and materials reflected the real-world, lived experiences of Latinx GBMSM and TW and prepared Navegantes to promote sexual health. |
| “After all the information that they gave us, I think that they prepared me very well. They give you a foundation, concrete and detailed information, and the elements to help other people and transmit the correct information.” (Navegante #1) |
| 3. Monthly group meetings with the HOLA project coordinator empowered Navegantes through social support and creative problem-solving. |
| “Meeting together was beneficial both for me, and for the other Navegantes, to be able to become more informed and follow-up on what we were doing, to see what was working or wasn’t, and share experiences that each of us had had with our friends.” (Navegante #1) |
| Interactions Between Navegantes and Social Network Members |
| 4. Navegantes overcame challenges discussing sexual health by continuing to build trust with social network members and making activities fun and engaging. |
| “It’s a little difficult at first. People, especially Hispanics, aren’t very comfortable about talking about sex. They don’t feel free to say what they feel, but people start to feel a little more confident talking about sexuality after they have more information.” (Navegante #1) |
| “Because they are very private things, I had to know how to ask questions and how to have a conversation where they [social network members] would feel comfortable.” (Navegante #2) |
| 5. Navegantes' personalized activities met social network members' diverse needs and priorities. |
| “Each person is different. I tried to see which person was more inclined to a group conversation and which person was more inclined to an individual conversation. Before [HOLA] our conversation topics were very different, about nightclubs or things like that. After [HOLA] and still up to today, we talk about sex and experiences that happen. On occasions, guys ask me to accompany them to the health department, and I go with them, and they get tested for HIV.” (Navegante #6) |
| Impact of the HOLA Intervention |
| 6. Participation increased Navegantes’ and social network members’ knowledge and leadership skills. |
| “It opened our minds to talk a little bit more. Now they [social network members] are more informed. Now they take care of themselves more, they know more, and they pass on information to others.” (Navegante #4) |
| “Well, I learned how to put on a condom, because I didn’t know. I thought it was put it on and that’s it. I learned about many sexually transmitted diseases that one can easily catch without knowing and little things that I didn’t have knowledge about.” (Social network member #5) |
| 7. Problem-solving and public-speaking skills were developed and strengthened. |
| “Well, I think that, in itself, it wasn’t so much the information as the concept of how to take care of ourselves, and how to react in the face of situations. For example, if you have a friend who is going through a phase, be it depression or some other disease or that they have caught something, I know how to react in that situation to help.” (Social network member #5) |
| 8. Community capacity for intervention sustainability and dissemination was built. |
| “A benefit was creating a network of leaders who know each other a little better on another level. It created networking among us. Many of us are still in touch. And it is good to note that they [social network members] have kept the habit of asking me for condoms, and now they don’t take 10 condoms but instead 100 condoms for their co-workers, for their neighbors. They turned in to little leaders themselves. It was because it wasn’t just one educational talk and that was it, but it was about sexual intimacy and about condoms. It was something that was taking place at the level of an entire community. If you went to a party people would say, ‘I’m part of HOLA.’ ‘Oh, I’m also part of HOLA.’” (Navegante #3) |
| “I think that I will never stop being a Navegante because I will continue giving people information that they need. I will continue giving out condoms to people that don’t have them, giving out brochures. I will never stop being a Navegante” (Navegante #8) |
The second domain involved the interactions between Navegantes and members of their social networks. Navegantes built trust and made activities fun and engaging. For example, Navegantes used condom distribution as a way to initiate sexual health discussions. Navegantes’ helping activities were personalized to the needs and priorities of their social network members. For example, if a social network member needed help with correctly using a condom, the Navegante would provide guidance about correct condom use to overcome the social network member’s specific challenges. This discussion, however, might lead to a discussion of whether the social network member needed support in discussing condom use with a partner, and if so, the Navegante probed to determine specifics about the situation and provide support personalized to that situation. Similarly, rather than merely educating members of their social networks about HIV testing and the rationale behind HIV testing, Navegantes worked to identify barriers to testing and problem-solve ways to overcome these barriers. Navegantes also tailored their communication styles based on social network members’ preferences and comfort levels for discussing sexual health.
The final domain related to the impact of the HOLA intervention. Navegantes and members of their social networks reported increased knowledge of HIV, STIs and prevention as well as increased leadership skills. For example, participants gained problem-solving and public-speaking skills experientially, and these skills were identified as leading to sustaining and supporting dissemination of the intervention. Community capacity was further built by Navegantes and social network members; participants noted that the HOLA intervention did not end when the project ended; rather, participants continued to share information and disseminate resources throughout their social networks.
Perceptions, needs and priorities
We identified 10 themes related to the perceptions, needs, and priorities of Latinx GBMSM and TW and organized them into three domains (Table IV). The first domain focused on discrimination. Participants reported high levels of discrimination based on sexual, gender and racial/ethnic identity. Based on personal experiences living in other parts of the United States or on general perceptions, participants considered the South to have particularly high levels of discrimination, with experiences of discrimination based on sexual orientation and gender identity being particularly common and impactful. Participants noted that often communities in the southern United States are known for not having the political, religious, social, ideological, economic or cultural diversity and support that some larger urban settings have, particularly those with more well-established Latinx populations and larger LGBTQ (lesbian, gay, bisexual, transgender and queer or questioning) communities. Participants also described how discrimination in the United States is often more subtle than in their countries of origin, where LGBTQ-related discrimination was reported as being more overt and perhaps more hostile with fewer legal protections for LGBTQ persons than in the United States.
Table IV.
Perceptions, needs, and priorities of Latinx GBMSM and TW domains, themes and select quotations
| Discrimination |
| 1. The U.S. South is considered particularly discriminatory and hostile to sexual, gender, and racial/ethnic minorities, with experiences of discrimination based on sexual orientation and gender identity being particularly common and impactful. |
| “In Mexico we think that people in the USA are very open minded, that there isn’t discrimination for being gay, but when I arrived here I realized that it’s very different.” (Social network member #6) |
| “It’s very difficult, especially in this area in the South. It’s a very conservative state. There aren’t many resources for the LGBT community. There are many barriers.” (Navegante #4) |
| 2. Discrimination in the United States is perceived as more subtle compared to discrimination in countries of origin where discrimination is perceived as more aggressive with fewer legal protections. |
| “There are more laws [in the U.S.] that don’t allow them to attack you. For example, they say that they aren’t giving you a job because you aren’t the person they are looking for. They don’t say that it is because you’re gay. On the other hand, in my country, they tell you directly that they aren’t giving you the job because you are gay. (Navegante #3) |
| 3. Discrimination in United States affects people in profound ways (e.g., employment options, healthcare access, and recreational opportunities). |
| “I think it makes life more difficult. You see more homophobia in these rural places than in big metropolises, and it’s also more difficult getting access to healthcare, work, and housing. It’s more complicated.” (Navegante #1) |
| “When you go to look for a job, even if you have experience and are one of the best workers, the fact that they see your appearance and that you look like I do, like a women, and on your application you put your name as it is [male]. For this simple fact, they look at you like you are the worst thing that exists, and that depresses you. It’s depressing.” (Social network member #6) |
| 4. Coping methods used to mitigate the effects of discrimination include normalizing the experiences of discrimination, seeking support from family and friends, and using alcohol. |
| “There is discrimination, teasing, and sarcasm. It used to make me mad. Now I feel sorry for people’s ignorance, that in spite of the fact that there is so much information, that there are so many of us, they still have such an ignorant mind that it really is sad. There is no gay, lesbian, or transgender person who has not been through this. (Social network member #5) |
| “Well, I think that discrimination happens everywhere, but sometimes you try to move forward and not pay much attention to those things.” (Social network member #8) |
| “Discrimination exists everywhere. Fifteen years ago I was very explosive because they would say something to me in the street, and I yelled at them what I needed to yell. Now, no, I just see it or hear it, and it doesn’t harm me at all because my family supports me, my mom is with me. What is around me doesn’t bother me.” (Social network member #10) |
| Sexual Health |
| 5. There is a profound need to focus on the health priorities of Latinx transgender women while building on that community’s existing assets. |
| “Because [my Navegante was transgender], I wanted to know more. I asked her for recommendations, and she talked to me about hormones. She oriented me and tried to help me to not be afraid and move forward.” (Social network member #8) |
| 6. Alcohol and drugs are used excessively by some Latinx GBMSM and transgender women, are perceived to be risk factors for HIV and STI infection, and are linked to mental health challenges. |
| “There is more risk because if you don’t have all your faculties there is more risk that you can have sex without a condom. In that moment, you don’t think in what can happen. I think that is common.” (Navegante #1) |
| “Often, the person doesn’t act the same. They think and behave differently and don’t really know what happened. Sometimes it is because of depression, lack of family here, lack of a job, or personal problems, so they resort to [drugs].” (Navegante #9) |
| “I think sometimes, self-esteem is very low, so people start to mix one thing with another to raise their self-esteem a little, and sometimes the consequences don’t matter to them, and I think that’s a little bad. It’s well known that when a person has very low self-esteem, with alcohol and drugs, they may not worry about consequences.” (Social network member #1) |
| 7. Use of social media (including Facebook and mobile applications [“apps”] designed for sexual and social networking) is common. |
| “I think that, since we are so bombarded with the internet, People use all of those pages to look for partners, more commonly than in the park or clubs.” (Navegante #10)“Apps are the fastest and easiest way to find a partner for sex.” (Social network member #4) |
| Health Care |
| 8. Very little awareness about PrEP exists, and more knowledge is needed to address confusion about what PrEP does; its effectiveness, related side effects, and cost; how to access it; and who can benefit from it. |
| “I am not taking PrEP. I don’t know anybody who is taking PrEP. Based on what I know, in this state it is very expensive, insurance doesn’t cover it, and health centers don’t give it to you because the cost is high.” (Navegante #4) |
| “Another barrier would be not knowing where to get [PrEP]. Also, if you don’t have a good job and you have to pay for it that is also a challenge. As an immigrant, you don’t have insurance, you don’t know where to get it, and you don’t know what to do about these types of things.” (Social network member #2) |
| “I have hesitations [about PrEP]. These are chemical products, and it scares me what reactions they might have, maybe not at that time but in the future, you never know. Well, to be honest, I don’t know if I would use it.” (Social network member #3) |
| 9. Barriers to accessing healthcare services were lack of the understanding of the U.S. healthcare system, the financial cost, and fears related to immigration enforcement are the greatest barriers to accessing health services. |
| “There are still people who, due to lack of information, think that they can’t get tested because of not having documents.” (Navegante #2) |
| 10. Some Latinx GBMSM and transgender women use low-cost clinics when sick, and most of those feel they can discuss sexual health with a health provider. |
| “I am not shy to talk about sexual topics, and even less so with a professional.” (Navegante #2) |
Participants noted that discrimination in the United States affects them in profound ways including limiting employment options, healthcare access and recreational opportunities. Coping methods that participants identified to mitigate the effects of discrimination included normalizing these experiences (e.g. expecting to be discriminated against as a member of a minority group and feeling they deserved being discriminated against). Participants reported that they sometimes sought support from family and friends; however, participants acknowledged that Latinx GBMSM and TW commonly face challenges with their families based on their orientation and/or gender identity.
Within the domain of sexual health, participants identified a profound need to focus on the sexual health-related needs, priorities and assets of Latinx TW. Latinx TW were identified as a particularly neglected and vulnerable group. Although some are connected to networks of other Latinx TW and GBMSM, there are many who remain isolated (especially in rural communities), and all could benefit from interventions and programs to meet their needs and priorities, in terms of access to gender-affirming supports including, education, mental health resources, hormone therapy, pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP). At the same time, participants reported that the social networks of Latinx TW and GBMSM overlap heavily, and they rely on one another.
Excessive use of alcohol and drugs were identified as a problem for some Latinx GBMSM and TW and was perceived by participants as contributing to increased HIV and STI infection within these populations. Participants reported that substance use is interwoven with mental health challenges including felt and enacted stigmas, social support, depression and anxiety and the ability to ‘make ends meet’. Social media use, including the use of Facebook and mobile applications (‘apps’) designed for social and sexual networking, was identified as common. Participants noted primarily using social media for social support and meeting new friends and sex partners yet suggested that social media could be harnessed to support other priorities (e.g. referrals to resources).
Finally, within the domain of health care, participants reported very little awareness of and confusion about PrEP, including what PrEP is and does; its effectiveness, side effects and cost; how to access it; and who can benefit from it. Participants also noted that they did not know how to access healthcare services, were unclear about their eligibility to receive services, perceived that they could not afford health care, and were fearful that their immigration status may place them at risk for detainment and deportation if they sought health care in the United States. Participants reported that some Latinx GBMSM and TW use low-cost clinics when sick, and most of those reported that they can discuss their sexual health with a health provider.
Discussion
Latinx GBMSM and TW in the United States are particularly vulnerable to HIV infection and comprise an increasing proportion of new HIV. However, there is a severe shortage of strategies designed to reach and support these populations, and fewer still for Spanish-speaking and immigrant subgroups. HOLA increased HIV testing among Spanish-speaking Latinx GBMSM and TW in our sample. At 12-month follow-up, HOLA participants were more than eight times as likely as waitlist control participants to report they had been tested for HIV during the past 12 months. We also observed favorable changes in cognitive and psychosocial factors, including increased HIV and STI knowledge and increased condom-use skills.
Our study had an extremely high retention rate; 95% of participants completed 12-month follow-up assessments. This may be attributable to the effects of substantial participation of Latinx GBMSM and TW at all stages of developing intervention content, recruitment and retention strategies, and measurement. HOLA reflected the lived experiences of these communities; each intervention training module and activity was conducted to meet the expressed needs and priorities of Latinx GBMSM and TW and built on community assets in an engaging manner. Furthermore, study team members who recruited participants, delivered the interventions, and contacted participants for follow-up assessments, reflected the population that was the focus of the intervention. Many study team members, including the principal investigator, self-identified as gay, were Latinx native Spanish speakers, or were proficient in Spanish, and had personal immigration-related experiences with which participants could identify. Finally, the high follow-up retention rates also resulted from the creativity of study staff to locate participants and complete follow-up assessments.
Given the recent development of biomedical prevention strategies such as PrEP and PEP, the intervention could be enhanced and tested to determine whether it can increase awareness of biomedical strategies and how to access them; address concerns regarding stigma, access, effectiveness, side effects and resources to defray costs; and increase uptake. Building on HOLA and in response to expressed needs for interventions specifically for Spanish-speaking Latinx TW, our CBPR partnership is currently testing ChiCAS (Chicas Creando Acceso a la Salud [Chicas: Girls Creating Access to Health]), a two-session Spanish-language small-group combination intervention designed to increase PrEP uptake by HIV seronegative Spanish-speaking Latinx TW who have sex with men.
HOLA could also be adapted for HIV-positive Latinx GBMSM and TW to promote engagement in HIV care and prevent HIV transmission to sexual partners. Information could also be incorporated about local care services, thereby facilitating contacts with providers.
Limitations
Our study relied on self-reported data; however, self-reported data can be reliable if collected carefully, including acknowledgments that some questions may cause discomfort and explanations concerning the importance of providing honest responses to ensure the usefulness of the research [47, 48]. The increase in condom use in both the intervention and waitlist control groups suggest contamination between these groups, which may be related to the community capacity built by the intervention and participants’ dissemination of knowledge and skills through natural helping activities with others. A study design that ensures that social networks are not geographically close in order to reduce contamination might be more successful in testing peer navigation within social networks. Our partnership has applied this type of design in the past successfully [18].
Conclusions
Critical gaps exist in the current intervention arsenal for reducing HIV and STI risks among Latinx GBMSM and TW and increasing PrEP uptake, PEP use, and care engagement. Given that HIV testing is the first step to ensuring that those who test negative remain negative and those who test positive get linked to care, HOLA is a potential invaluable resource for increasing testing among Latinx GBMSM and TW and thus linking them to biomedical prevention strategies (e.g. PrEP) or HIV care as appropriate.
Acknowledgments
We would like to acknowledge the National Institute of Health (grant R01MH087339) and the Program in Community Engagement of the Wake Forest Clinical and Translational Science Institute, which is supported by the National Center for Advancing Translational Sciences, National Institutes of Health (grant UL1TR001420).
Conflict of interest statement
None declared.
References
- 1.US Census Bureau. 2019. Available at: http://www.census.gov/. Accessed: February 28, 2020.
- 2. Martinez AD, Rhodes SD.. Introduction: disentangling language and the social determinants of Latinx health in the United States In: Martinez AD, Rhodes SD (eds). New and Emerging Issues in Latinx Health. Switzerland: Springer, 2020, 1–15. [Google Scholar]
- 3. Flores A, Lopez MH, Krogstad JM.. US Hispanic Population Reached New High in 2018, but Growth Has Slowed. Washington, DC: Pew Research Center, 2019. [Google Scholar]
- 4.U. S. Census Bureau. Hispanic or Latino origin 2015 American Community Survey 1-Year Estimates U.S. Census Bureau, 2015.
- 5.Centers for Disease Control and Prevention. HIV Surveillance Report, 2019. Available at: http://www.cdc.gov/hiv/library/reports/surveillance/. Accessed: February 28, 2020.
- 6. Reif S, Safley D, McAllaster C. et al. State of HIV in the US deep south. J Community Health 2017; 42: 844–53. [DOI] [PubMed] [Google Scholar]
- 7. Painter TM, Song EY, Mullins MM. et al. Social support and other factors associated with HIV testing by Hispanic/Latino gay, bisexual, and other men who have sex with men in the U.S. South. AIDS Behav 2019; 23: 251–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Becasen JS, Denard CL, Mullins MM. et al. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006-2017. Am J Public Health 2019; 109: e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Habarta N, Wang G, Mulatu MS. et al. HIV testing by transgender status at Centers for Disease Control and Prevention-funded sites in the United States, Puerto Rico, and US Virgin Islands, 2009-2011. Am J Public Health 2015; 105: 1917–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nuttbrock L, Hwahng S, Bockting W. et al. Lifetime risk factors for HIV/sexually transmitted infections among male-to-female transgender persons. J Acquir Immune Defic Syndr 2009; 52: 417–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kellogg TA, Clements-Nolle K, Dilley J. et al. Incidence of human immunodeficiency virus among male-to-female transgendered persons in San Francisco. J Acquir Immune Defic Syndr 2001; 28: 380–4. [DOI] [PubMed] [Google Scholar]
- 12. Rapues J, Wilson EC, Packer T. et al. Correlates of HIV infection among transfemales, San Francisco, 2010: results from a respondent-driven sampling study. Am J Public Health 2013; 103: 1485–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lippman SA, Moran L, Sevelius J. et al. Acceptability and feasibility of HIV self-testing among transgender women in San Francisco: a mixed methods pilot study. AIDS Behav 2016; 20: 928–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Herbst JH, Jacobs ED, Finlayson TJ. et al. ; for the HIV/AIDS Prevention Research Synthesis Team. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav 2008; 12: 1–17. [DOI] [PubMed] [Google Scholar]
- 15.The White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. U.S. Department of Health & Human Services, 2015.
- 16. Tanner AE, Philbin MM, Ma G.. HIV prevention interventions with adolescents: innovations and challenges in partnerships across the integrated transitions model In: Rhodes SD. (ed.). Innovations in HIV Prevention Research and Practice through Community Engagement. New York, NY: Springer, 2014, 77–104. [Google Scholar]
- 17. Rhodes SD, Mann-Jackson L, Alonzo J. et al. The health and well-being of Latinx sexual and gender minorities in the USA: a call to action In: Martinez AD, Rhodes SD (eds). New and Emerging Issues in Latinx Health. Switzerland: Springer, 2020, 217–36. [Google Scholar]
- 18. Rhodes SD, Hergenrather KC, Bloom FR. et al. Outcomes from a community-based, participatory lay health adviser HIV/STD prevention intervention for recently arrived immigrant Latino men in rural North Carolina. AIDS Educ Prev 2009; 21: 103–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rhodes SD, Leichliter JS, Sun CJ. et al. The HoMBReS and HoMBReS Por un Cambio interventions to reduce HIV disparities among immigrant Hispanic/Latino men. MMWR Morb Mortal Wkly Rep 2016; 65: 51–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Israel BA, Schulz AJ, Parker EA. et al. Critical issues in developing and following community based participatory research issues In: Minkler M, Wallerstein N (eds). Community-Based Participatory Research for Health. San Francisco, CA: Jossey-Bass, 2003, 53–76. [Google Scholar]
- 21. Rhodes SD, Tanner AE, Mann-Jackson L. et al. Promoting community and population health in public health and medicine: a stepwise guide to initiating and conducting community-engaged research. J Health Dispar Res Pract 2018; 11: 16–31. [PMC free article] [PubMed] [Google Scholar]
- 22. Rhodes SD. Authentic engagement and community-based participatory research for public health and medicine In: Rhodes SD. (ed.). Innovations in HIV Prevention Research and Practice through Community Engagement. New York, NY: Springer, 2014, 1–10. [Google Scholar]
- 23. Rhodes SD, Tanner AE, Mann-Jackson L. et al. Community-engaged research as an approach to expedite advances in HIV prevention, care, and treatment: a call to action. AIDS Educ Prev 2018; 30: 243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rhodes SD, Mann L, Alonzo J. et al. CBPR to prevent HIV within ethnic, sexual, and gender minority communities: successes with long-term sustainability In: Rhodes SD. (ed.). Innovations in HIV Prevention Research and Practice through Community Engagement. New York, NY: Springer, 2014, 135–60. [Google Scholar]
- 25. Israel BA, Schulz AJ, Parker EA, Becker AB.. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health 1998; 19: 173–202. [DOI] [PubMed] [Google Scholar]
- 26. Vissman AT, Eng E, Aronson RE. et al. What do men who serve as lay health advisors really do?: Immigrant Latino men share their experiences as Navegantes to prevent HIV. AIDS Educ Prev 2009; 21: 220–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sun CJ, Mann L, Eng E. et al. Once a Navegante, always a Navegante: Latino men sustain their roles as lay health advisors to promote general and sexual health to their social network. AIDS Educ Prev 2015; 27: 465–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Eng E, Rhodes SD, Parker EA.. Natural helper models to enhance a community’s health and competence In: DiClemente RJ, Crosby RA, Kegler MC (eds). Emerging Theories in Health Promotion Practice and Research. San Francisco, CA: Jossey-Bass, 2009, 303–30. [Google Scholar]
- 29. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs: Prentice-Hall, 1986. [Google Scholar]
- 30. Freire P. Education for Critical Consciousness. New York, NY: Seabury Press, 1973. [Google Scholar]
- 31. Wills TA. Supportive functions of interpersonal relationships In: Cohen S, Syme L (eds). Social Support and Health. Orlando, FL: Academic Press, 1985, 61–82. [Google Scholar]
- 32. Altman DG, Bland JM.. How to randomise. BMJ 1999; 319: 703–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rhodes SD, Alonzo J, Mann Jackson L. et al. Selling the product: strategies to increase recruitment and retention of Spanish-speaking Latinos in biomedical research. J Clin Transl Sci 2018; 2: 147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rhodes SD, Alonzo J, Mann L. et al. Small-group randomized controlled trial to increase condom use and HIV testing among Hispanic/Latino gay, bisexual, and other men who have sex with men. Am J Public Health 2017; 107: 969–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rhodes SD, McCoy TP, Hergenrather KC. et al. Prevalence estimates of health risk behaviors of immigrant Latino men who have sex with men. J Rural Health 2012; 28: 73–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rhodes SD, McCoy TP, Vissman AT. et al. A randomized controlled trial of a culturally congruent intervention to increase condom use and HIV testing among heterosexually active immigrant Latino men. AIDS Behav 2011; 15: 1764–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marin BV, Tschann JM, Gomez CA. et al. Self-efficacy to use condoms in unmarried Latino adults. Am J Community Psychol 1998; 26: 53–71. [DOI] [PubMed] [Google Scholar]
- 38. DiIorio C, Maibach E, O’Leary A. et al. Measurement of condom use self-efficacy and outcome expectancies in a geographically diverse group of STD patients. AIDS Educ Prev 1997; 9: 1–13. [PubMed] [Google Scholar]
- 39. van der Straten A, Catania JA, Pollack L.. Psychosocial correlates of health-protective sexual communication with new sexual partners: the National AIDS Behavioral Survey. AIDS Behav 1998; 2: 213–27. [Google Scholar]
- 40. Sun CJ, Ma A, Tanner AE. et al. Depressive symptoms among Latino sexual minority men and Latina transgender women in a new settlement state: the role of perceived discrimination. Depress Res Treat 2016; 2016: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Ross MW, Rosser BR.. Measurement and correlates of internalized homophobia: a factor analytic study. J Clin Psychol 1996; 52: 15–21. [DOI] [PubMed] [Google Scholar]
- 42. Shen L, Condit CM, Wright L.. The psychometric property and validation of a fatalism scale. Psychol Health 2009; 24: 597–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gilbert PA, Rhodes SD.. Psychometric performance of a novel measure of social support among Spanish-speaking immigrant Latino gay men. Hisp J Behav Sci 2012; 34: 491–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Friedman LM, Furberg CD, DeMets DL.. Fundamentals of Clinical Trials, 3rd edn.New York, NY: Springer-Verlag, 1998. [Google Scholar]
- 45. Wolfinger R, O’Connell M.. Generalized linear mixed models: a pseudo-likelihood approach. J Stat Comput Simul 1993; 48: 233–43. [Google Scholar]
- 46. Glaser BG, Strauss AL.. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine, 1967. [Google Scholar]
- 47. Pequegnat W, Fishbein M, Celentano D. et al. NIMH/APPC workgroup on behavioral and biological outcomes in HIV/STD prevention studies: a position statement. Sex Transm Dis 2000; 27: 127–32. [DOI] [PubMed] [Google Scholar]
- 48. Rhodes SD, Duck S, Alonzo J. et al. Intervention trials in community-based participatory research In: Blumenthal D, DiClemente RJ, Braithwaite RL. et al. (eds). Community-Based Participatory Research: Issues, Methods, and Translation to Practice. New York: Springer, 2013, 157–80. [Google Scholar]