Abstract
Background:
Social media can effectively mediate digital health interventions and thus, overcome barriers associated with face-to-face interaction.
Objective:
To assess the impact of patient-centered diabetes education program administered through WhatsApp on glycosylated hemoglobin (HbA1c) values, assess the correlation, if any, between health literacy and numeracy on intervention outcomes
Methods:
During an ‘intervention phase’ spread over six months, target diabetic patients (N=109) received structured education through WhatsApp as per the American Association of Diabetes Educators Self-Care Behaviors recommendations. The control group with an equal number of participants received ‘usual care’ provided by health professionals void of the social media intervention. Changes in HbA1c levels were recorded thrice (at baseline, 3 and 6 months) for the test group and twice (baseline and 6 months) for the control group. Change in HbA1c values were compared and statistical significance was defined at p<0.05. Baseline health literacy and diabetes numeracy were assessed for both groups (N=218) using the Literacy Assessment for Diabetes (LAD), and the Diabetes Numeracy Test (DNT), respectively, and values were correlated with HbA1c change p<0.05. Participants’ satisfaction with the intervention was also assessed.
Results:
The average age of respondents was 41.98 (SD 15.05) years, with a diabetes history of 10.2 (SD 8.5) years. At baseline, the average HbA1c in the control and test groups were 8.4 (SD 1.06) and 8.5 (SD 1.29), respectively. After six months, a significant drop in HbA1c value was noticed in intervention group (7.7; SD 1.35; p= 0.001); with no significance in the control group (8.4; SD 1.32; p=0.032, paired t-test). Moreover, the reduction in HbA1c was more in the test group (0.7%) than the control group (0.1%) with a difference of 0.6% which is considered clinically significant. There was no significant correlation between LAD score and HbA1c at baseline (r=-0.203, p=0.064), 3 months (r=-0.123, p=0.266) and 6 months (r=-0.106, p= 0.337) Pearson correlation. A similar result was observed with DNT, where DNT score and HbA1c at baseline, 3 months and 6 months showed no correlation (r=0.112, 0.959 and 0.886; respectively) with HbA1c levels. Eighty percent of the respondents found the social media intervention ‘beneficial’ and suggested it be used long term.
Conclusions:
Diabetes education via WhatsApp showed promising outcomes regardless of the level of patients’ health literacy or numeracy.
Keywords: Social Media, Patient Education as Topic, Self Care, Health Literacy, Patient-Centered Care, Personal Satisfaction, Diabetes Mellitus, Glycated Hemoglobin A, Non-Randomized Controlled Trials as Topic, United Arab Emirates
INTRODUCTION
Diabetes mellitus is a chronic disease affecting millions of individuals worldwide and impacting on patients’ quality of life, often leading to morbidity and mortality.1 The incidence of diabetes rapidly increased worldwide in the last few decades as documented in the International Diabetes Federation Atlas (IDF). There is a high prevalence of diabetes mellitus in the United Arab Emirates (UAE), reaching around 21.4% in 2030 according to IDF 2017 report.2 This pattern is expected due to rapid economic growth and associated lifestyle changes such as reduced physical activity and increased caloric intake.3 Diabetes self-management education reinforces lifestyle modification as part of diabetes management.
Diet and physical activity are aspects of lifestyle modification which lead to improved glycemic control and a decrease in morbidity.3-7 Worldwide, previous studies reported that diabetes self-management education improves glycosylated hemoglobin (HbA1c) levels and reduces the risk of life-threatening complications.1,8 However, patients with diabetes face many obstacles adhering to traditional self-management education protocols such as lack of knowledge about potential benefits of education, absence of personalized education, diabetes education costs, and time limitations.1,5,9,10
There have been growing efforts to implement new approaches for self-management interventions that improve diabetes control.1 Recently, information technology use has increased dramatically resulting in improved communication.11 Social Media is defined as the Internet-based tools that allow individuals to communicate, gather and share information, ideas and images, and to team up with other users in real-time.12 Social media channels such as Facebook, Instagram, WhatsApp, Snapchat, Twitter may mediate digital health interventions, which provide continuous support and effective communications, and overcome barriers associated with face to face modalities.4,5 Patients consider social media as a source to get disease-specific information, interact quickly and efficiently with others and share medical information with a community of patients having similar problems.3,11
Social media has become a valuable resource for people with diabetes to enhance self-management skills. Patients who have similar conditions and similar experiences connect very easily through Social media, providing a suitable environment to share knowledge and peer support.7 However, there is little evidence to support the role of social media in improving self-management behavior and health outcomes in patients with diabetes.4 Lifestyle changes such as diet adjustment and physical activity involvement, blood glucose monitoring, online education, peer support and real-time interaction between patients and healthcare professionals, are all facilitated through social media.1,6,7 Hence, healthcare professionals have recommended using social media to improve diabetes self-management skills and consequently improve glycemic control.6,13
Patient health literacy levels have a crucial role in patient response to diabetes education efforts.14 Patients with low health literacy often face obstacles in understanding instructions on prescribed drug labels, comprehending medical education leaflets, consuming healthy diet, and achieving better control of their diabetes.15,16 Similarly, diabetic patients with low numeracy skills face difficulties in interpreting glucose readings, determining serving portions, applying medications dose changes, and performing daily self-management tasks.17 Many tools have been used to assess diabetic patients health literacy and numeracy levels, this will help in developing effective educational strategies that are designed to fit patient health literacy and numeracy levels.18,19 The Literacy Assessment of Diabetes (LAD) is a test of patients’ ability to pronounce diabetes-related terms commonly used during clinic visits or when reading food menu and self-care instructions.20 It is word recognition test, which is considered an indirect measurement of the level of patient comprehension.21 Diabetes Numeracy Test (DNT) is designed to assess diabetes - related numeracy skills that are required in performing daily diabetes self-management. DNT covers general mathematical skills and concepts such as addition, subtraction, multiplication, division, fractions, and multi-step calculations.22
The UAE population is considered one of the world’s highest users of mobile phones and social networking avenues which makes social media-related interventions to improve diabetes control possibly successful.23 Studies evaluating the use of social media to enhance diabetes management in the Middle East are sparse.3,11 Additionally, a recent literature review showed no previous studies that explored social media interventions in improving diabetes control in the UAE.3 Therefore, the aim of this research was to assess the impact of a structured patient education coordinated through WhatsApp on diabetes control, and to assess any effect of health literacy and/or numeracy levels of patients undergoing through this education on diabetic control.
METHODS
Study design
This study was approved by Ajman University Research Ethics Committee (approval number: P-F-H-18-11-16), dated 19th January, 2019.
This research was a randomized, two-arm parallel interventional study with a 6 months patient follow-up conducted among diabetic patients. The intervention group received diabetes self-management education through social media network application (i.e., WhatsApp) while the control group received usual care.
Participants
Recruitment: Participants from seven emirates (Abu Dhabi, Dubai, Ajman, Fujairah, Ras al Khaimah, Sharjah and Umm al Quwain) were conveniently recruited from private medical centers.
Sample size: This was part of a larger study to translate and culturally adapt the LAD and DNT into the Arabic context.21 Four hundred patients participated in the original study but only 218 agreed to continue with the six months social media intervention and were hence included.
Inclusion and exclusion criteria: Those whose age is between 18 to 80 years, diabetes mellitus type 1 or 2, could speak Arabic or English, with an HbA1c>7.5%, and were regular users of WhatsApp were included in the study. Those who had severe hearing or visual impairment, or did not know how to use WhatsApp were excluded. Those with gestational diabetes were excluded because their condition required different clinical management procedures (Figure 1).
Figure 1. Participant enrollment and follow-up.
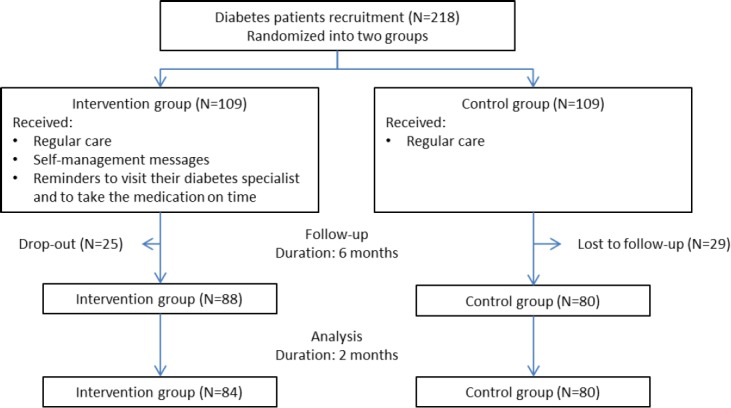
Randomization: All agreeing participants were randomized into one of two groups using simple randomization method: the interventional group (n=109) and the control group (n=109).
Participant enrollment and consent: Prior to starting the study, participants were asked to sign a consent form and fill out background information including participant demographic and clinical information such as diabetes duration, treatment regimen and if the participants had received diabetes education previously.
Health literacy assessment: Participant’s health literacy and numeracy levels were assessed using LAD and DNT before starting the intervention. LAD test was administrated by requesting participants to loudly read and pronounce 60 words. Five seconds were given to read each word, if a particular participant needed more than 5 seconds, he/she was asked to pass to the next word.20 Participants were then asked to complete the DNT. Here, participants were asked to answer 43 questions related to diabetes numeracy skills required to perform daily diabetes self-management such as nutrition, exercise, managing symptoms of uncontrolled diabetes such as hypoglycemia, oral medications and insulin dosing adjustments.22
Structured intervention
During a six months follow-up period, participants in the intervention group received daily educational information through WhatsApp. The educational material related to diabetes self-management behaviors (AADE7 Self-Care Behaviors®) recommended by the American Association of Diabetes Educators (AADE) and the American Diabetes Association (ADA) (
).24 The AADE7 Self-Care Behaviors® guidelines are suitable for both Type 1 and Type 2 diabetes mellitus. The messages contained information about healthy eating, food portion management, physical activity, self-monitoring of blood glucose, reminders for medication intake, insulin use and coping with and adjusting to living with diabetes.24
Each day, participants received WhatsApp messaging about self-management behaviors. Messages were sent at a particular time of the day; though they were opened at the participant’s convenient time. WhatsApp broadcast provided private bidirectional communication between the participants and the investigators, which allowed participants to seek advice and get free-of-charge feedback.
Intervention procedure
Step 1: A WhatsApp group was initiated involving participants from the intervention group. This intervention was moderated by the researchers (licensed pharmacists) who were responsible for all communications (
).
Step 2: The original English messages were translated by the research team to Arabic; they were adapted and refined to suit the local cultural context. Before starting the study, participants were asked about their language preference in which messages were to be communicated. All questions sent by participants to the research team through WhatsApp broadcast were treated confidentially.
Step 3: Three months into the study, participants were contacted via WhatsApp to obtain their most recent HbA1c value. HbA1c values were collected via phone calls from those who did not respond to WhatsApp.
Step 4: Six months into the study, participants were contacted again to obtain their HbA1c value and to determine participants’ satisfaction level concerning the social media intervention.
Meanwhile, participants in the control group were offered usual diabetes care without the WhatsApp intervention; they only received phone calls 6 months into the study to obtain their most recent HbA1c value. The control group subjects were followed twice versus thrice for the test group. Since the main purpose of the control group was to compare the test group outcome with a similar control in order to quantify the impact of the intervention, the research proposal included only twice measurement for the control group subjects against three for the test group.
The main outcome of the study was the mean change in HbA1c level by comparing the control group and intervention group values at different time intervals. Self-reported HbA1c value was obtained from participants in the intervention group at baseline, 3 months, and 6 months post study initiation, while for the control group, baseline and 6 months HbA1c values were collected.
On the LAD test, scores were totaled and converted to a reading grade level. Scores between 0 and 20 were considered of fourth grade level and below; participants who achieved scores between 21 and 40 were considered of fifth to ninth grade levels, while those achieving scores between 41 and 60 were considered above ninth grade level.20 DNT scores, however, were reported as a percentage of the total correct answers.22
Participant satisfaction level with the social media intervention was assessed online through WhatsApp using a self-developed satisfaction tool at the end of the study. Participants responded on a three-point Likert-type scale (ranging from agree to disagree) to items regarding how much the intervention was beneficial, convenient, and if they agreed to continue using social media to help in monitoring their disease.
Prior to starting the main study, a small pilot test was conducted over 3 months on 10 diabetic patients. The pilot study aimed to assess the feasibility and acceptability of the social media intervention procedures. Results obtained were used to refine the main study protocol. The pilot study revealed that patients’ desired to continue diabetes follow up through social media for more than 3 months. Participants gave positive feedback about the medical information received through WhatsApp.
Data analysis
The IBM SPSS version 26 was used for data analysis. Descriptive statistical parameters of mean, standard deviations (SD), frequencies and percentages were used to analyze the demographic information and clinical characteristics of the participants. The data was normally distributed as determined by histograms and normality plots. Paired t-test was used to compare HbA1c change in the intervention group at different time intervals (baseline, after 3- and 6-months period) and for the control groups at the baseline and at 6 months. Pearson Correlation was used to assess the association between participants’ health literacy level (LAD, DNT scores) and HbA1c change during the social media intervention. Independent sample t-test was used for one variable comparison between two groups. One-way ANOVA was used in multiple group comparisons. Study findings were considered statistically significant if p-value <0.05.
RESULTS
Two hundred and eighteen participants were randomized into two groups: 109 in the interventional group and 109 as the control group. However, 84 participants from the intervention group and 80 participants from the control group completed the study through the 6-month follow-up (Figure 1). The reason for drop outs were participants refuse to continue the program due to social obligations (not interested anymore and not having time, traveling overseas and disconnections in WhatsApp due to change in their telephone number and subsequently the WhatsApp number.
The mean (SD) age of the participants was 41.98 (15.05) years; they had diabetes duration of 10.2 (8.5) years, the earliest 40 years ago, and the most recent was 1 month before the start of the study. Most (57.9%) of the participants were women; (71.9%) were college graduates. More than 60% of the participants had type 2 diabetes mellitus and visited their diabetes specialist only as needed. There was no significant difference of patients’ characteristics between the intervention and the control group at baseline (Table 1).
Table 1. Participants’ demographic and other information.
| Intervention group (N= 84) | Control group (N= 80) | p-value* | |
|---|---|---|---|
| Age mean (SD) | 43.9 (15.4) | 40.06 (14.7) | 0.51 |
| Duration of diagnosis of diabetes mean (SD) | 9.4 (8.9) | 11.2 (8.1) | 0.86 |
| N (%) | N (%) | ||
| Gender | |||
| Women | 52 (61.9%) | 43 (53.8%) | |
| Men | 32 (38.1%) | 37 (46.3%) | |
| Marital status | |||
| single | 15 (17.9%) | 26 (32.5%) | |
| married | 66 (78.6%) | 50 (62.5%) | |
| divorced | 1 (1.2%) | 3 (3.8%) | |
| widowed | 2 (2.4%) | 1 (1.3%) | |
| Educational Level | |||
| Never attended school | 1 (1.2%) | 1 (1.3%) | |
| Elementary (grade 1-6) | 4 (4.8%) | 2 (2.5%) | |
| Intermediate (grade 7-9) | 2 (2.4%) | 3 (3.8%) | |
| High school (grade 10-12) | 16 (19.0%) | 17 (21.3%) | |
| Collage Graduate | 61 (72.6%) | 57 (71.3%) | |
| Medical Insurance | |||
| Yes | 38 (45.2%) | 36 (45%) | |
| No | 46 (54.8%) | 44 (55%) | |
| Diabetes Type | |||
| Type 1 | 27 (32.1%) | 38 (47.5%) | |
| Type 2 | 57 (67.9%) | 42 (52.5%) | |
| Diabetes specialist Visit | |||
| never | 1 (1.2%) | 0 (0%) | |
| every month | 13 (15.5%) | 17 (21.3%) | |
| every 3 months | 20 (23.8%) | 23 (28.7%) | |
| more than 3 months | 1 (1.2%) | 1 (1.3%) | |
| as needed | 49 (58.3%) | 39 (48.8%) | |
| Diabetes Education | |||
| Yes | 34 (59.5%) | 50 (62.5%) | |
| No | 50 (40.5%) | 30 (37.5%) |
(*) independent sample t-test.
HbA1c decreased significantly in the intervention group from 8.4% (SD=1.06) to 7.7% (SD=1.35) after 6 months (p=0.001) (Table 2).
Table 2. HbA1c change in the intervention and the control groups.
| HbA1c | Intervention group (N= 84) | Control group (N= 80) | ||
|---|---|---|---|---|
| Mean (SD) | p-Value | Mean (SD) | p-Value* | |
| Baseline | 8.4 (1.06) | 8.5 (1.29) | ||
| 3 months | 7.9 (1.26) | 0.001† | ** | ** |
| 6 months | 7.7 (1.35) | 0.001†† | 8.4 (1.32) | 0.032††† |
| mean change (SD) | -0.7 (0.84) | -0.1 (0.58) | ||
Paired t-test at alpha less than 0.05
no HbA1c value obtained from the control group at 3 months
statistically significant while comparing baseline with 3 months
statistically significant while comparing baseline with 6 months
statistically significant while comparing baseline with 6 months
In addition, in both diabetes type 1 and 2 significant differences in HbA1c values between the baseline and after 6 month follow up in the intervention group were seen, see Figure 2.
Figure 2. HbA1c change in type 1 and type 2 diabetes mellitus.

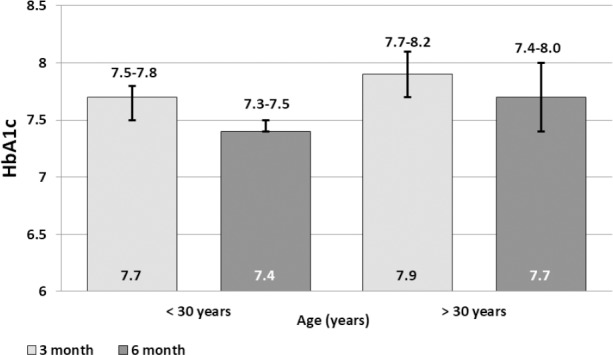
There were also significant differences in the intervention group between baseline and after 6 months HbA1c values for those younger than 30 years versus those older than 30 years (Figure 3).
Figure 3. HbA1c change comparison between <30 and >30 years old Diabetes patients in the intervention group.
However, no significant differences were seen in HbA1c values at different time intervals based on gender, diagnosis duration, obtainment of diabetes education, and availability of medical insurance. Statistical assessments showed no significant differences among different nationalities after the intervention (ANOVA p=0.44).
The results showed that there was no correlation between LAD score and HbA1c value at baseline, 3 months and 6 months (p=0.064, 0.266 and 0.337 respectively). In addition, there was no correlation between DNT score and HbA1c value at baseline, 3 months and 6 months (bivariate Pearson correlation p=0.112, 0.959 and 0.886, respectively).
Only 30 (35.7%) participants responded to the patient satisfaction assessment. Twenty-seven (90%) participants’ answers showed preference to continue long-term social media intervention, 24 (80%) said that social media intervention was beneficial, and 20 (67%) classified the WhatsApp intervention as convenient.
DISCUSSION
This study evaluated the usefulness of WhatsApp as a tool to improve communication and achieve better glycemic control among diabetes patients. This study gains importance as there is an increase use of social media in pharmacy practice.25-29 It is imperative for pharmacy practitioners to explore social media as a potential tool to educate, monitor and assess clinical outcomes. The present research approach involved a direct communication with diabetic patients using social media overcoming the barriers associated with direct personal contact. The intervention provided diabetic patients with readily available, easily accessible, quality information at no cost.
Acute and chronic complications associated with diabetes have been shown to be delayed or prevented by offering patients self-management education.30 Use of social media in healthcare has widely been encouraged to enable quick, direct and effective communication between patients and health professionals.4,31,32 This is especially true since smartphone use is now a common trend among most people, adding to their exceptional ability to share data in a simple, effective, and timely manner.33 Moreover, patients benefit more with self-management plans if interventions were conducted in a familiar and more convenient environment such as their homes.34 Hence, it is crucial to design interventions which could be delivered at recipients’ convenience regarding time, place and direct human interference.
As a measure of diabetes glycemic control, lowering HbA1c is an important outcome for diabetes interventions.33 In the current research, after six months of intervention, a significant change in HbA1c value was shown. This reduction was attributed to adherence to medications, timely follow-ups and other tips provided by the pharmacist (
). Moreover, the intervention group had a lower HbA1c values after six months compared to the control group with a difference of 0.6 percent. As per the American diabetes association, a half percentage difference in HbA1c is considered clinically significant change to reduce risk of comorbidities.8,35 Other studies reported that a one percentage reduction in HbA1c was linked to twenty one percentage risk reduction in diabetes mortality and thirty seven percentage reduction in microvascular complications.36 These research findings were consistent with previous studies which showed that social media was an innovative and feasible method of improving glycemic control in people with diabetes.6,8,11 In addition, previous studies proved that traditional or unconventional interventional methods of patient education and reminders were both associated with improvements in patient adherence to guidelines and improvements in patient outcomes.33,37 However, one study reported that using social media for one year yielded HbA1c reduction similar to that of applying other interventions for three years.38 It is better to provide long-term diabetes self-management education to avail more effective and efficient patient care services.39 However, the duration of our intervention was only six months. Interestingly, a previous meta-analysis investigated the effect of antidiabetic medications like thiazolidinedione and sulfonylureas on reduction in HbA1c levels which were reported at 0.5 to 1.25 percentage, respectively.36 Our findings, thus, showed an effect from the social media intervention on HbA1c level reduction as that reported from using pharmacological approaches.
This study also revealed that participants’ health literacy and numeracy levels had no effect on HbA1c change after the social media intervention. This was a positive outcome that was worth noting - the social media intervention seemed effective in all patients including those with low health literacy and numeracy skills. In this regard, our findings agreed with those of previous studies which also used social media-based interventions to manage patients with diabetes regardless of their health literacy levels.40 This outcome may be related to the simple language used in the intervention program, in addition to the use of visual aids such as videos and pictures that suited all patients including those with low health literacy.40,41
Our results also indicated a greater reduction in HbA1c value among type 2 diabetic patients with a mean change of 0.8 percent compared to 0.4 percent for type 1 patients in a six month intervention period. A possible explanation for this difference in response is that social media intervention through WhatsApp messages targeted factors such as sedentary lifestyle and unhealthy diet whose modification would affect type 2 diabetes control to a larger extent.
The reduction in mean HbA1c value in participants younger than 30 years in our study was significantly higher than that of participants who were older. Results close to the desired HbA1c value were reported to reflect higher social media engagement from younger participants.8 Similar findings were reported by previous studies which considered age as a barrier to achieving glycemic control related to social media interventions in older patients.34
The suitability and sustainability of interventions could be ensured only if the recipients were satisfied with the interventions. A high satisfaction level was reported among participants about using the social media intervention. The findings suggested this approach could potentially encourage participants to adopt a healthy lifestyle and enhance their diabetes self-management behaviors with minimal cost and effort.
in this study, the results revealed the potential of investing in social media programs to improve healthcare outcomes. Several previous studies showed that the use of social media in clinical practice enabled healthcare providers to implement effective patient support, and improve patient engagement and satisfaction.42
Strengths and limitations
The strength of this study lies in the use of a larger sample size compared to other studies.3,35 The treatment regimen with which each participant started was maintained throughout the intervention period; participants whose treatment regimen was changed were removed from the study. Although message content relied on standard guidelines that suited all participants, the content was tailored and customized depending on each participant’s needs. This adaptation included different strategies such as message frequency and timing as well as providing options for the participants to select messages from specific self-management domains.35
In the WhatsApp application, messages are marked with two blue checkmarks that appeared near to the message after being opened by the recipient. However, the investigators could not be sure that each message sent was actually opened and read. Confidentiality is an issue in using social media especially in the cases of other persons accessing WhatsApp massages. Also, since the effective sample size was decreased to 84 in intervention group and 80 in control group the power of the study could have been compromised.
CONCLUSIONS
Using social media (i.e., WhatsApp) to improve self-management education had a positive influence on glycemic control of patients with diabetes. On average, the social media intervention produced a 0.7% change in HbA1c compared to routine care. The effect of social media on HbA1c change was not influenced by patients’ health literacy and numeracy skill levels; this attests to the simplicity of the messages and the efficacy of the intervention. Patients were satisfied with the intervention and agreed to continue to use it if it were to continue in the future. Future research could focus on other outcomes of social media interactions such as the level of patients’ engagement, patient behavior and attitudes, and the efficacy of patient-healthcare provider communication levels.
Footnotes
CONFLICT OF INTEREST
The Authors declare no potential conflicts of interest with respect to research, authorship, or publication of this article.
FUNDING
This research was funded by Research grant from the Deanship of Graduate Studies and Research at Ajman University (Ref: CRG-A-2018-PH-01).
Contributor Information
Muaed AL Omar, PhD. Associate Professor. Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University. Ajman (United Arab Emirates). m.alomar@ajman.ac.ae.
Sanah Hasan, PhD. Associate Professor. Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University. Ajman (United Arab Emirates). s.hasan@ajman.ac.ae.
Subish Palaian, PhD. Associate Professor. Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University. Ajman (United Arab Emirates). s.palaian@ajman.ac.ae.
Shrouq Mahameed, MSc. Research Assistant. Department of Clinical Sciences, College of Pharmacy and Health Sciences, Ajman University. Ajman (United Arab Emirates). s.mahameed@ajman.ac.ae.
References
- 1.Kitsiou S, Pare G, Jaana M, Gerber B. Effectiveness of mHealth interventions for patients with diabetes:an overview of systematic reviews. PLoS One. 2017;12(3):e0173160. doi: 10.1371/journal.pone.0173160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation. IDF Diabetes Atlas. 8th edn. Brussels: International Diabetes Federation; 2017. [(accessed Feb 1, 2019)]. Available at https://diabetesatlas.org/IDF_Diabetes_Atlas_8e_interactive_EN/ [Google Scholar]
- 3.Alanzi T. Role of social media in diabetes management in the Middle East region:systematic Review. J Med Internet Res. 2018;13(20(2)):e58–e58. doi: 10.2196/jmir.9190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gabarron E, Arsand E, Wynn R. Social media use in interventions for diabetes:rapid evidence-based review. J Med Internet Res. 2018;20(8):e10303. doi: 10.2196/10303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pal K, Dack C, Ross J, Michie S, May C, Stevenson F, Farmer A, Yardley L, Barnard M, Murray E. Digital health interventions for adults with type 2 diabetes:qualitative study of patient perspectives on diabetes self-management education and support. J Med Internet Res. 2018;20(2):e40. doi: 10.2196/jmir.8439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toma T, Athanasiou T, Harling L, Darzi A, Ashrafian H. Online social networking services in the management of patients with diabetes mellitus:systematic review and meta-analysis of randomised controlled trials. Diabetes Res Clin Pract. 2014;106(2):200–211. doi: 10.1016/j.diabres.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Cooper A. New dawn:the role of social media in diabetes education. J Diabetes Nurs. 2014;18(2):68–71. [Google Scholar]
- 8.Quinn CC, Butler EC, Swasey KK, Shardell MD, Terrin MD, Barr EA, Gruber-Baldini AL. Mobile diabetes intervention study of patient engagement and impact on blood glucose:mixed methods analysis. JMIR Mhealth Uhealth. 2018;6(2):e31. doi: 10.2196/mhealth.9265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whitley HP, Fermo JD, Ragucci KR, Chumney EC. Assessment of patient knowledge of diabetic goals, self-reported medication adherence, and goal attainment. Pharm Pract (Granada) 2006;4(4):183. doi: 10.4321/s1885-642x2006000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adisa R, Alutundu MB, Fakeye TO. Factors contributing to nonadherence to oral hypoglycemic medications among ambulatory type 2 diabetes patients in Southwestern Nigeria. Pharm Pract (Granada) 2009;7(3):163–169. doi: 10.4321/s1886-36552009000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Petrovski G, Zivkovic M, Stratrova SS. Social media and diabetes:can facebook and skype improve glucose control in patients with type 1 diabetes on pump therapy?One-year experience. Diabetes Care. 2015;38(4):e51–e52. doi: 10.2337/dc14-2487. [DOI] [PubMed] [Google Scholar]
- 12.Ventola CL. Social media and health care professionals:benefits, risks, and best practices. P T. 2014;39(7):491–520. [PMC free article] [PubMed] [Google Scholar]
- 13.Veazie S, Winchell K, Gilbert J, Paynter R, Ivlev I, Eden K, Nussbaum K, Weiskopf N, Guise J-M, Helfand M. Technical Brief No. 31. Rockville, MD: Agency for Healthcare Research and Quality; 2018. Mobile applications for self-management of diabetes. [PubMed] [Google Scholar]
- 14.Qin L, Xu H. A cross-sectional study of the effect of health literacy on diabetes prevention and control among elderly individuals with prediabetes in rural China. BMJ Open. 2016;6(5):e011077. doi: 10.1136/bmjopen-2016-011077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moss TR. The impact of health literacy on clinical outcomes for adults with type 2 Diabetes Mellitus. Adv Diabetes Metab. 2014;2(1):10–19. doi: 10.13189/adm.2014.020103. [DOI] [Google Scholar]
- 16.Hussein SH, Almajran A, Albatineh AN. Prevalence of health literacy and its correlates among patients with type II diabetes in Kuwait:A population-based study. Diabetes Res Clin Pract. 2018;141:118–125. doi: 10.1016/j.diabres.2018.04.033. [DOI] [PubMed] [Google Scholar]
- 17.White RO, Wolff K, Cavanaugh KL, Rothman R. Addressing health literacy and numeracy to improve diabetes education and care. Diabetes Spectr. 2010;23(4):238–243. doi: 10.2337/diaspect.23.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haun JN, Valerio MA, McCormack LA, Sorensen K, Paasche-Orlow MK. Health literacy measurement:an inventory and descriptive summary of 51 instruments. J Health Commun. 2014;19(Suppl 2):302–333. doi: 10.1080/10810730.2014.936571. [DOI] [PubMed] [Google Scholar]
- 19.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51(3):267–275. doi: 10.1016/s07383991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 20.Nath CR, Sylvester ST, Yasek V, Gunel E. Development and validation of a literacy assessment tool for persons with diabetes. Diabetes Educ. 2001;27(6):857–864. doi: 10.1177/014572170102700611. [DOI] [PubMed] [Google Scholar]
- 21.Hasan S, Mahameed S, AlHariri Y. Translation and culture adaptation of the simplified diabetes knowledge test, the literacy assessment for diabetes and the diabetes numeracy test. Res Soc Adm Pharm. 2019 doi: 10.1016/j.sapharm.2019.11.003. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, Fuchs LS, Malone R, Cherrington A, Dewalt DA, Buse J, Pignone M, Rothman RL. Development and validation of the diabetes numeracy test (DNT) BMC Health Serv Res. 2008;8:96. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alanzi T, Istepanian R, Philip N. Design and usability evaluation of social mobile diabetes management system in the gulf region. JMIR Res Protoc. 2016 26 Sep;5(3):e93–e93. doi: 10.2196/resprot.4348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Association of Diabetes Educators. [(accessed Sep 22, 2019)];AADE7 Self-Care Behaviors. 2019 Available from: https://www.diabeteseducator.org/living-with-diabetes/aade7-self-care-behaviors#.XagszI1hKJU.mendeley .
- 25.Benetoli A, Chen TF, Aslani P. The use of social media in pharmacy practice and education. Res Social Adm Pharm. 2015;11(1):1–46. doi: 10.1016/j.sapharm.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Alkhateeb FM, Clauson KA, Latif DA. Pharmacist use of social media. Int J Pharm Pract. 2011;19(2):140–142. doi: 10.1111/j.2042-7174.2010.00087.x. [DOI] [PubMed] [Google Scholar]
- 27.Grindrod K, Forgione A, Tsuyuki RT, Gavura S, Giustini D. Pharmacy 2.0:a scoping review of social media use in pharmacy. Res Social Adm Pharm. 2014;10(1):256–270. doi: 10.1016/j.sapharm.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 28.Benetoli A, Chen TF, Schaefer M, Chaar B, Aslani P. Do pharmacists use social media for patient care? Int J Clin Pharm. 2017;39(2):364–372. doi: 10.1007/s11096-017-0444-4. [DOI] [PubMed] [Google Scholar]
- 29.O'Hara B, Fox BI, Donahue B. Social media in pharmacy:heeding its call, leveraging its power. J Am Pharm Assoc (2003) 2013;53(6):565. doi: 10.1331/JAPhA.2013.13536. [DOI] [PubMed] [Google Scholar]
- 30.Standards of medical care in diabetes. American Diabetes Association, 2014. Diabetes Care. 2014;37(Suppl 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 31.Williams G, Hamm MP, Shulhan J, Vandermeer B, Hartling L. Social media interventions for diet and exercise behaviours:a systematic review and meta-analysis of randomized controlled trials. BMJ Open. 2014;4(2):e003926. doi: 10.1136/bmjopen-2013-003926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Döğer E, Bozbulut R, Soysal Acar AŞ, Ercan Ş, KılınçUğurlu A, Akbaş ED, Bideci A, Çamurdan O, Cinaz P. Effect of telehealth system on glycemic control in children and adolescents with type 1 diabetes. J Clin Res Pediatr Endocrinol. 2019;11(1):70–75. doi: 10.4274/jcrpe.galenos.2018.2018.0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Quinn CC, Gruber-Baldini AL, Shardell M, Weed K, Clough SS, Peeples M, Terrin M, Bronich-Hall L, Barr E, Lender D. Mobile diabetes intervention study:testing a personalized treatment/behavioral communication intervention for blood glucose control. Contemp Clin Trials. 2009;30(4):334–346. doi: 10.1016/j.cct.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 34.Tao D, Or CK. Effects of self-management health information technology on glycaemic control for patients with diabetes:a meta-analysis of randomized controlled trials. J Telemed Telecare. 2013 Apr;19(3):133–143. doi: 10.1177/1357633X13479701. [DOI] [PubMed] [Google Scholar]
- 35.Sahin C, Courtney KL, Naylor PJ, E Rhodes R. Tailored mobile text messaging interventions targeting type 2 diabetes self-management:A systematic review and a meta-analysis. Digit Heal. 2019;5 doi: 10.1177/2055207619845279. 2055207619845279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yoshida Y, Boren SA, Soares J, Popescu M, Nielson SD, Simoes EJ. Effect of health information technologies on glycemic control among patients with type 2 diabetes. Curr Diab Rep. 2018;18(12):130. doi: 10.1007/s11892-018-1105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weingarten SR, Henning JM, Badamgarav E, Knight K, Hasselblad V, Gano AJ, Ofman JJ. Interventions used in disease management programmes for patients with chronic illness-which ones work?Meta-analysis of published reports. BMJ. 2002;325(7370):925. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrovski G, Zivkovic M. Impact of facebook on glucose control in type 1 diabetes:a three-year cohort study. JMIR diabetes. 2017;2(1):e9. doi: 10.2196/diabetes.7693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Association of Diabetes Educators (AADE) [(accessed Nov 22, 2019)];AADE7TM self-care behaviors american association of diabetes educators (aade) position statement. 2014 Available at: https://www.diabeteseducator.org/docs/default-source/practice/practice-resources/position-statements/aadne7-self-care-behaviors-position-statement.pdf?sfvrsn=6 .
- 40.Kim SH, Utz S. Effectiveness of a social media –based, health literacy –sensitive diabetes self-management intervention:A Randomized Controlled Trial. J Nurs Scholarsh. 2019;51(6):661–669. doi: 10.1111/jnu.12521. [DOI] [PubMed] [Google Scholar]
- 41.Davis T. [(accessed Nov 2, 2019)];Health literacy:hidden barriers and practical strategies. 2015 Available at: https://www.ahrq.gov/healthliteracy/qualityresources/tools/literacytoolkit/tool3a/index.html .
- 42.Dhar VK, Kim Y, Graff JT, Jung AD, Garrett J, Dick LE, Harris J. Shan S, Benefit of social media on patient engagement and satisfaction:results of a 9-month, qualitative pilot study using Facebook. Surgery. 2018;163(3):565–570. doi: 10.1016/j.surg.2017.09.056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


