1. Introduction
Physical activity (PA) has strong relevance for limiting the harms to human health and well-being due to the coronavirus disease-2019 (COVID-19) pandemic.1 Active muscles produce chemicals that improve immune functioning, which in turn reduces the extent of infections, and decreases inflammation, and these are the main causes of the lung damage from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. PA is a powerful preventive and therapeutic intervention for the most common pre-existing chronic conditions that increase risk of severe COVID-19 infections and mortality.2,3 PA's effectiveness in preventing and treating anxiety and depression could have worldwide benefits during this stressful global crisis.2 PA enhances the efficacy of vaccines,4 so active lifestyles will continue to be relevant through every phase of the pandemic. Worldwide, about 23% of men and 32% of women are at risk for the underlying conditions of COVID-19, severe COVID-19 infections, and stress-related psychological symptoms, because they do not meet PA guidelines, based on self-report measures.5,6
It is likely that prolonged shelter-at-home measures will lead to reduced PA and increased sedentary behaviors that adversely affect immune function and enhance risk for chronic health conditions.7,8 Many people, especially with low incomes, do not have equipment, Internet access, or indoor space to make at-home PA realistic. Thus, the current pandemic is almost certain to exacerbate socioeconomic inequities in PA.9, 10, 11
The pandemic is changing the places where people can be physically active because many jurisdictions closed or restricted access to common indoor and outdoor places for PA.12, 13, 14 Though some jurisdictions allowed people to exercise outdoors on the streets, others did not, so for millions of people, being active at home was the only option. As limitations are eased, policies related to indoor and outdoor PA places vary across jurisdictions.15,16 If spikes occur in COVID-19 cases and deaths, movement restrictions may be put back in place. It is unknown how long this dynamic ebb and flow of limits on people's ability to be physically active will last and what the impact will be on PA. There are many unanswered questions about how pandemic-related policies in each jurisdiction are affecting PA. Therefore, it is important to identify the most pressing scientific questions that could be translated to policy and practice aimed at favorably impacting population health outcomes.
There is ample evidence to justify making PA promotion a global public health priority during the coronavirus pandemic.1,17 One pathway to increasing the prominence of PA as a solution is to set a public health research agenda for promoting scientific studies to document any health and societal benefits during the COVID-19 pandemic, and to evaluate public health strategies for effectively promoting PA under crisis conditions.
We consider research on PA and COVID-19 to be an urgent global public health need. Within this context, relevant PA research can span a broad range from basic science covering in vitro laboratory studies and human studies, to clinical studies with diagnosed patients, to public health studies focusing on prevention. Among the many research needs, the present paper focuses on studies with the potential to guide public health policy and practice, with a secondary focus on studies that could guide clinical practice. Our international author team has proposed priority areas for PA and public health research relevant to the COVID-19 pandemic. Although the current literature provides strong scientific premise for the public health relevance of PA for COVID-19,1,4,8 no research has specifically examined the impact of PA on SARS-CoV-2 infections or produced data directly related to the evaluation of infection control strategies that might impact PA. Evidence on these and other emergent topics is needed in a timely manner to inform PA policy and practice locally and internationally.
The author team includes a senior researcher who has studied PA for decades (JFS) and 3 early-career investigators who bring research skills related to PA, the creativity of youth, and diverse geographic and cultural experience, having grown up in India (DA), Nigeria (AO), and Mexico (DS). We have interdisciplinary expertise in behavioral science, spatial epidemiology, urban health, physiotherapy, and health promotion. Our goal is to stimulate research studies that should be started now in multiple countries, especially among those countries most affected by the SARS-CoV-2 virus, to inform effective PA promotion strategies to be applied during the current pandemic, as well as to improve preparedness for future pandemics. Each author nominated study ideas, and consensus was reached on the highest priorities based on the need to conduct the study during the pandemic, direct relevance to practice or policy, and feasibility.
The 7 research topics selected for inclusion in the present paper are just a few of those initially nominated by the authors. We encourage investigators to plan studies on the topics suggested here and identify additional questions related to PA and COVID-19 that deserve to be investigated. For each research topic below, we briefly explain the purpose of the study, though few methodological details are provided, on the assumption investigators will bring their own skills and creativity to each study. We provide a rationale for the importance of each topic and summarize the significance for policy or practice. We also highlight a few challenges likely to be encountered in conducting each type of study.
2. Using the behavioral epidemiology framework to guide PA and COVID-19 research
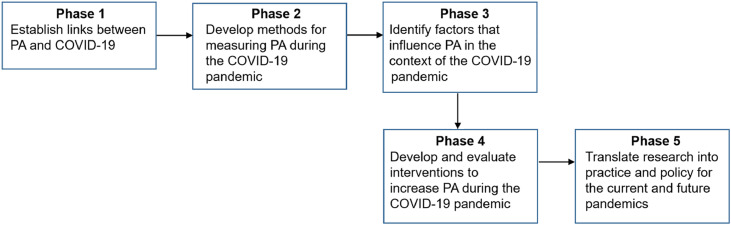
The proposed study topics are organized according to a behavioral epidemiology framework that specifies a systematic sequence of studies on health-related behaviors designed to lead to evidence-based interventions directed at populations.18 Fig. 1 lists the 5 phases of research, adapted to apply specifically to PA and COVID-19 studies. The subheadings are the phases of the behavioral epidemiology framework, used to organize presentation of the proposed research topics.
Fig. 1.
The behavioral epidemiology framework applied to studying physical activity and coronavirus disease-2019 (COVID-19). PA = physical activity.
2.1. Establish links between PA and COVID-19
2.1.1. Research Proposal 1: examine the potential of PA as a mitigation strategy in moderating the impact of the novel coronavirus
As part of COVID-19 testing for both clinical and surveillance purposes, administer a brief lifestyle survey that includes questions about PA frequency, intensity, duration, and type, as well as sedentary behaviors, prior to the onset of any current illness. If the patient is too ill to complete the survey, it could be completed by someone who knows the patient's PA habits. When available, PA data from the medical record could be used. Then, follow patients for their outcomes related to COVID-19, including severity of symptoms, time to recovery, hospitalization, health care utilization and costs, and mortality. A valuable add-on would be to monitor expected mediators (e.g., lung function, immune indicators, inflammatory markers, psychological health, and mental status) so mechanisms of action underlying PA and COVID-19 outcomes can be elucidated.
2.1.1.1. Rationale
Because of PA's documented effects on immunity, inflammation, and infection,19,20 we hypothesize that people who engage in regular moderate-intensity PA prior to being infected will have less severe infections compared to those who do not. The proposed study would quantify the association, if any, of PA with COVID-19 outcomes.
2.1.1.2. Policy implications
If regular, moderate-intensity PA is found to have beneficial effects on COVID-19 outcomes, such results would justify increased public health efforts to educate the public and provide a scientific foundation for implementing evidence-based PA promotion strategies as part of the pandemic response.21 The findings would allow PA promotion consistent with global and national guidelines to be included in predictive models and public policy statements.6,21, 22, 23
2.1.1.3. Challenges
Studies like this will require a team with expertise in PA measurement, sampling methods, clinical outcomes, health care financing, and physiology of immune systems and inflammation. The logistics of integrating the research project in clinical care settings and obtaining access to clinical and health care cost outcomes will have to be arranged.
2.2. Develop methods for measuring PA during the COVID-19 pandemic
No specific studies for this phase are proposed because widely used methods to measure PA and sedentary behavior should be used if possible. Currently, there are many validated measures, using diverse modes of assessment, available for all ages and tailored for many population subgroups.24, 25, 26, 27, 28, 29, 30, 31, 32
Although device-based measures may be preferred due to their better accuracy than self-reports, the use of device-based measures could be challenging in large studies due to cost constraints, especially in low- and middle-income countries (LMICs).33 Device-based measures also do not capture domain- and context-specific PA behaviors. Researchers planning to conduct studies pertaining to other phases of the behavioral epidemiology framework are encouraged to consider the trade-off in their choice of measurement tool vis-à-vis the need for precision vs. feasibility, and any necessary adaptations for collecting PA data during the pandemic (e.g., adapt existing instruments for online administration).
2.3. Identify factors that influence PA in the context of the COVID-19 pandemic
2.3.1. Research Proposal 2: use big data to understand changes in PA during the pandemic
Use big data analytics to conduct longitudinal built environment, active transportation, and PA assessments to identify changes in patterns of human movement, hotspots of pedestrian and bicyclist movement, and crowding during the pandemic.34 These studies should harness the power of technologies (e.g., web cameras, drones, smartphone apps), artificial intelligence, and machine learning to collect data before, during, and after the COVID-19 pandemic.35 The extensive, objective nature of these data has the potential for real-time tracking of PA across large geographic areas and over longer time spans, enabling longitudinal studies. For example, recent data from Garmin wearable devices was used to estimate percent change in PA across many locations during the pandemic.36
2.3.1.1. Rationale
A prevailing notion prompting several governmental responses to the pandemic is that residential density promotes the spread of infections. However, density can also be beneficial as it supports many local amenities like larger hospitals, rapid emergency responses, walkable shops and services, public transit, parks and playgrounds, and other facilities that aid health and wellness.37, 38, 39 The problem in dense cities is crowding at a given time and place that could enhance the spread of infection. Big data from mobile technologies can provide an unprecedented amount of behavioral and environmental data, at both individual and aggregated levels, to help understand and improve human movement, including in dense urban spaces, during the pandemic.
2.3.1.2. Policy implications
Unobtrusive, real-time monitoring of trends in pedestrian and bicyclist behaviors could inform local government policies for urban design and transport planning that integrate density and diversity of land uses in ways that support PA. Such data could simultaneously detect and help to regulate hotspots of overcrowding.
2.3.1.3. Challenges
The adoption of new technologies is known to vary by socioeconomic status, gender, age, ethnicity, and other demographic factors. Thus, it may be difficult to monitor and quantify the changes in high-risk, vulnerable populations. It would be ideal for international groups to develop standardized procedures for cross-country studies using big data analytics by overlaying PA and health data with factors like weather, transportation infrastructure, and neighborhood conditions. Studies will also need to consider privacy and data protection challenges.
2.3.2. Research Proposal 3: learn how to reduce disparities in PA opportunities during crises
Conduct mixed-methods, longitudinal studies of individuals at high-risk for (a) becoming infected with SARS-CoV-2 (e.g., low-wage “essential workers”), (b) developing a severe case of COVID-19 (e.g., older people, smokers, and those with obesity, hypertension, and diabetes), and (c) being significantly economically impacted by the pandemic (e.g., laid off or furloughed individuals, and immigrants/refugees without access to government services). A combination of quantitative and qualitative methods for identifying the multilevel barriers and facilitators for maintaining PA during the pandemic are encouraged across the various phases of the pandemic, including (a) the period of exponential growth and peak of the epidemic in the study site, (b) the “back to normal” transition period, and (c) the post-pandemic period.
2.3.2.1. Rationale
In contrast to anecdotal reports from high-income settings of increases in outdoor PA (e.g., more use of trails and parks),40, 41, 42 the most disadvantaged members of society (e.g., low-income settings, LMICs) likely do not have these opportunities. It is critical to identify the barriers and opportunities for maintaining active lifestyles during the pandemic among multiple high-risk populations.
2.3.2.2. Policy implications
These studies will provide evidence to tailor programs and policies that can help high-risk groups to stay active, healthy, and resilient during and after the COVID-19 pandemic and future crises.
2.3.2.3. Challenges
Many parts of the world have either already reached the peak of SARS-CoV-2 transmission, or are about to, at the time of this writing (early May 2020). An alternative is to rely on valid recall methods to retrospectively assess PA (and barriers and facilitators) among high-risk groups during the shelter-at-home phase of the COVID-19 pandemic. Creative use of mail-, telephone-, and online-based recruitment strategies should be harnessed during stay-at-home orders. However, some subgroups targeted in these studies (e.g., low-income groups) are less responsive to these types of recruitment approaches, compared to in-person recruitment.43 Social media ads, snowball sampling, and partnerships with local institutions,43 are potential strategies to overcome this challenge.
2.4. Develop and evaluate interventions to increase PA during the COVID-19 pandemic
2.4.1. Research Proposal 4: improving clinical care of people with coronavirus infections through PA
Conduct randomized controlled trials of newly diagnosed COVID-19 cases to evaluate the effects of daily PA on COVID-19 outcomes, compared to usual care. Patients with mild cases could be supported to do moderate-intensity activity through online or telephone support while they are at home. Patients hospitalized with moderate cases could be supported by physiotherapists to do light-intensity activity in the hospital. Patients with severe cases would not be eligible. PA would continue as long as the patient could tolerate it, even during hospitalization.
2.4.1.1. Rationale
Moderate-intensity PA has acute beneficial effects on immune functioning and inflammation that should help reduce the severity of COVID-19 outcomes,19,20 and/or be protective for populations with underlying medical conditions. These benefits may continue if people are physically active after infection and during hospitalization. Current practices that do not promote PA may be equivalent to overly conservative practices in earlier decades when heart attack patients were prescribed bed rest and told to avoid PA. We argue the current approach fails to take advantage of the powerful pro-immunity and anti-inflammatory properties of each session of PA. The goal of the proposed studies is to determine how long patients with confirmed COVID-19 can remain physically active after diagnosis, and whether remaining or becoming active has net benefits on the severity of symptoms, quality of life, time to recovery, health care utilization and costs, and mortality.
2.4.1.2. Policy implications
Demonstration that PA interventions improve outcomes for patients with COVID-19 would provide evidence on which to base new clinical guidelines.
2.4.1.3. Challenges
Prescribed moderate-intensity PA with COVID-19 patients is certain to raise ethical questions about the safety of the intervention. Thus, investigators will need to thoroughly document the expected benefits for patients, clearly define the risk status of patients to be included in studies, provide protocols for stopping PA, and monitor continuously for adverse events. Though in-person data collection could be used within hospitals, it would require a strong collaboration between researchers and clinicians and administrators. Out-of-hospital data collection and intervention would need to be delivered virtually. Especially in low-income areas, this would likely require the provision of electronic devices and Internet access to some patients.
2.4.2. Research Proposal 5: evaluate methods for managing safe use of PA locations
Conduct population surveys before and after indoor and outdoor PA facilities are closed to determine the impact on people's PA practices. Alternatively, conduct retrospective studies in areas where places for PA have been closed, to document reported changes on amounts of, and locations for, PA. These studies should include measures of government efforts to mitigate effects of closures on PA, such as opening streets or other locations so people can be active while maintaining safe distances,42 or allowing access to PA locations only to those being active while monitoring to ensure safe distances. These studies could also investigate how people reacted to restrictions, such as by finding ways to be active in the home, use of online exercise resources, seeking out e-health behavior change programs, seeking social support from friends or family, reducing overall PA, or purposively violating restrictions. Such studies should be conducted with all age groups.
2.4.2.1. Rationale
PA locations like trails, parks, and boardwalks became more popular after shelter-in-place orders.40, 41, 42 Because of observed crowding, many localities closed these places for PA.44 Closing the most popular places may have a net negative impact on COVID-19 infections, unless mitigation measures are implemented or individuals seek out alternative places for PA. The many variations of closure orders and mitigation efforts around the world create a massive natural experiment that should be evaluated. Outcomes could include PA, psychological health, infection rates, hospitalizations, and mortality.
2.4.2.2. Policy implications
The proposed studies would provide information about which types of policies about access to PA places and which management/mitigation practices can have the most positive net effect on the pandemic, minimizing the risk of infection spread while maximizing the benefits of physically active populations.
2.4.2.3. Challenges
Assessing the impact of policy changes on PA will be challenging because policies that close, restrict, manage, and reopen places for PA are frequently shifting. Another challenge is the number and diversity of parks, playgrounds, trails, and indoor gyms and studios in each jurisdiction. Though the impact of policy changes on park use and PA could be observed, the impact on PA of the community might require a population survey or use of electronic monitors or smartphones.
2.4.3. Research Proposal 6: evaluate local mapping of safe places to be active during the pandemic
Use geographic information systems mapping to identify safe community walking and cycling routes or develop access protocols for PA in hyperlocal outdoor environments.20 Evaluate the impact of publicizing maps of PA locations on PA of community residents, evidence of crowding, and infection rates.
2.4.3.1. Rationale
Outdoor spaces such as parks, green spaces, and trails have been closed due to crowding.44,45 Restricting access to popular places is likely to have negative implications for PA, mental health, and perhaps COVID-19 infections.46 Maps that highlight parks, green spaces, and safe, convenient walking or cycling routes with marked distances can help people to discover opportunities for local PA that could result in greater dispersion of people being active outdoors.
2.4.3.2. Policy implications
The outcomes of these proposed studies could inform the development of policies and guidelines that aim at promoting PA and access to neighborhood outdoor environments during future infectious disease pandemics.
2.4.3.3. Challenges
The processes of gathering, integrating, processing, and visualizing large-scale geographic and social spatial information for decision making requires a unified geographical framework, which creates data limitations and financial implications in resource-constrained settings. A longer term solution would be for researchers to develop a global monitoring system of outdoor PA locations and establish a data integration and analysis platform, which would provide accurate and timely information for emergency policymaking before, during, and after future pandemics.
2.4.4. Research Proposal 7: cultural tailoring of PA promotion during crises
Develop and evaluate culturally tailored PA promotion strategies for community members sheltering in place during the COVID-19 pandemic. These studies should include evaluation of PA programs and messaging primarily using e-health modes of delivery (e.g., online, mobile apps, and printed pdf) on PA.
2.4.4.1. Rationale
There is a need for safe, effective, and accessible PA programs to help maintain immune system function while sheltering in place.8 Populations differ on many dimensions between and within countries, such as age, sex, culture, language use, socioeconomic status, physical abilities, prior PA, built environment conditions, and PA preferences. Thus, PA interventions likely need to be tailored for a variety of subgroups within each country. Although e-health modes of delivery seem most applicable when physical distancing is required, access to and cultural acceptability of Internet-based technologies is far from universal, so other delivery modes such as print or telephone may be needed, depending on the target group. A participatory co-creation approach is recommended, involving PA researchers, behavioral scientists, and community members who are on restriction, to design culturally appropriate and evidence-informed PA programs that could be delivered through e-health, print, or telephone media. Programs should include social interaction elements, as socialization is a key driver of PA for some individuals and cultures.47 These co-created PA interventions should be implemented on a broad basis and evaluated with outcomes including participation in programs, program satisfaction, and PA.
2.4.4.2. Policy implications
These studies would create culturally tailored, low-cost, high-reach programs to promote PA for isolated individuals and communities that could be used during future crises.
2.4.4.3. Challenges
Challenges include the logistics of co-creation of interventions by a diverse team including community residents sheltering-in-place when physical distancing is required. In LMICs, penetration of technology is not as high as in high-income countries, and the receptiveness to use technology for receiving health intervention is lower than in high-income countries. Access to online-based virtual interventions in LMICs may be limited by cost of cell phones, data plans, and Internet coverage, when it is available. A practical solution may be to incorporate more conventional and feasible ways of delivering tailored interventions, such as through print media, radio, and network television.
2.5. Translate research into practice and policy for the current and future pandemics
There are many evidence-based PA interventions for people of all ages,21,48, 49, 50 but virtually none of them have been scaled up for wide implementation.51 Though PA benefits continue to be relevant during the current pandemic,1,17,20 there are additional challenges to applying previously evaluated interventions when physical distancing is mandated. In-person classes are not possible. Although online PA classes have proliferated,52 their use and effectiveness need to be evaluated before they can be considered evidence based. Online PA behavior change programs have evidence of effectiveness.21,50 Therefore, there is a tremendous opportunity to evaluate diverse interventions in the context of the pandemic. We encourage researchers in each region to identify existing PA interventions that are well suited to local populations and determine whether adaptations are needed for specific target populations. Then, researchers could implement “hybrid” studies that simultaneously evaluate the efficacy of the interventions during the pandemic and collect data on feasibility, user satisfaction, and cost 53 that can be used to plan scaling-up the intervention if efficacy results are promising.
3. Conclusion
PA has multiple well-documented benefits directly related to reducing impact of the COVID-19 infection itself, as well as helping the global population cope with the isolation and stress caused by the pandemic.1 Yet PA is not being strategically nor systematically promoted to reduce harms from the current pandemic. Thus, there is an urgent need for research that can inform more effective PA policies and practices in the short term and prepare global public health for better responses to future crises. The studies prioritized in this article represent several phases of the behavioral epidemiology framework,18 that, if implemented, would document the impact of moderate-intensity PA on severity of SARS-CoV-2 infections and possibly lead to specific public health recommendations for populations to be active as well as inclusion of PA effects in statistical models used to guide policy. Most of the proposed studies would evaluate interventions of various types during the context of the current pandemic, and those results could be directly applicable to improving responses to the current and future crises.
We encourage investigators from around the world to conduct studies like those recommended here and to initiate them as soon as possible. Ideally, investigators could coordinate their study methods, measures, and analyses so results across countries will be as comparable as possible. This is scientifically important so country-context similarities and differences can be documented and distinguished from methodological differences. To facilitate coordination of studies across sites, we created a repository of PA and COVID-19 research studies that supports researchers with similar interests to connect (access to repository of all studies: https://docs.google.com/spreadsheets/d/1Dt9rIiJe0_-z3Qm9x0yxpSuD0cWQgoPg68i-PMZ7PbY/edit#gid=434161713; access to form to enter study information: https://forms.gle/rZ9k4TNruSVnpKiv9). We invite PA researchers, scientific organizations, and global scientific networks to disseminate and contribute to this repository.
Acknowledgments
Authors’ contributions
JFS conceptualized the paper, assembled the writing team, drafted proposed research studies, and drafted the introduction and conclusion sections; DA, AO, and DS drafted proposed research studies. All authors voted on priority research studies to include in the paper from a longer list and critically edited the full manuscript draft. All authors have read and approved the final version of the manuscript, and agree with the order of the presentation of the authors (which is alphabetical for the last 3 authors).
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Sallis JF, Pratt M. A call to action: physical activity and COVID-19. Available at: https://www.exerciseismedicine.org/support_page.php/stories/?b=896. [accessed 06.05.2020].
- 2.Powell K.E., King A.C., Buchner D.M., Campbell W.W., DiPietro L., Erickson K.I. The scientific foundation for the physical activity guidelines for Americans, 2nd edition. J Phys Act Health. 2018;17:1–11. doi: 10.1123/jpah.2018-0618. [DOI] [PubMed] [Google Scholar]
- 3.Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 4.Pascoe A.R., Fiatarone Singh M.A., Edwards K.M. The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans. Brain Behav Immun. 2014;39:33–41. doi: 10.1016/j.bbi.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Guthold R., Stevens G.A., Riley L.M., Bull F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob Health. 2018;6:e1077–e1086. doi: 10.1016/S2214-109X(18)30357-7. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Global recommendations on physical activity for health. Available at: https://www.who.int/dietphysicalactivity/factsheet_recommendations/en/. [accessed 23.04.2020]. [PubMed]
- 7.Fitbit Staff. The impact of coronavirus on global activity. Available at: https://blog.fitbit.com/covid-19-global-activity/. [accessed 23.04.2020].
- 8.Chen P., Mao L., Nassis G.P., Harmer P., Ainsworth B.E., Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: a social crisis in the making. Lancet Public Health. 2020;5:e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Douglas M., Katikireddi S.V., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020;369:m1557. doi: 10.1136/bmj.m1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cockerham W.C., Hamby B.W., Oates G.R. The social determinants of chronic disease. Am J Prev Med. 2017;52:S5–12. doi: 10.1016/j.amepre.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan P, McIntyre N, Cutler S. Coronavirus park closures hit BAME and poor Londoners most. Available at: https://www.theguardian.com/uk-news/2020/apr/10/coronavirus-park-closures-hit-bame-and-poor-londoners-most. [accessed 06.05.2020].
- 13.Gagliano L. Malta: COVID-19 update: closure of public places. Available at: https://www.mondaq.com/coronavirus-covid-19/909400/covid-19-update-closure-of-public-places. [accessed 06.05.2020].
- 14.Government of the Netherlands. Closing public and private spaces. Available at: https://www.government.nl/topics/coronavirus-covid-19/tackling-new-coronavirus-in-the-netherlands/faqs-about-approach-to-tackling-coronavirus/closing-public-and-private-spaces. [accessed 06.05.2020].
- 15.Tupekci Z. Keep the parks open. Available at: https://www.theatlantic.com/health/archive/2020/04/closing-parks-ineffective-pandemic-theater/609580/. [accessed 06.05.2020].
- 16.Freeman S, Eykelbosh A. COVID-19 and outdoor safety: considerations for use of outdoor recreational spaces. Available at: https://ncceh.ca/documents/guide/covid-19-and-outdoor-safety-considerations-use-outdoor-recreational-spaces. [accessed 06.05.2020].
- 17.World Health Organization. Be active during COVID-19. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/be-active-during-covid-19. [accessed 06.05.2020].
- 18.Sallis J.F., Owen N., Fotheringham M.J. Behavioral epidemiology: a systematic framework to classify phases of research on health promotion and disease prevention. Ann Behav Med. 2000;22:294–298. doi: 10.1007/BF02895665. [DOI] [PubMed] [Google Scholar]
- 19.Hojman P. Exercise protects from cancer through regulation of immune function and inflammation. Biochem Soc Trans. 2017;45:905–911. doi: 10.1042/BST20160466. [DOI] [PubMed] [Google Scholar]
- 20.Nieman D.C., Wentz L.M. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019;8:201–217. doi: 10.1016/j.jshs.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.King A.C., Whitt-Glover M.C., Marquez D.X., Buman M.P., Napolitano M.A., Jakicic J. Physical activity promotion: highlights from the 2018 Physical Activity Guidelines Advisory Committee systematic review. Med Sci Sports Exerc. 2019;51:1340–1353. doi: 10.1249/MSS.0000000000001945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Piercy K.L., Troiano R.P., Ballard R.M., Carlson S.A., Fulton J.E., Galuska D.A. The physical activity guidelines for Americans. JAMA. 2018;320:2020–2028. doi: 10.1001/jama.2018.14854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies S, Atherton F, McBride M, Calderwood C. UK chief medical officers’ physical activity guidelines. Available at:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/832868/uk-chief-medical-officers-physical-activity-guidelines.pdf. [accessed 18.05.2020].
- 24.Warren J.M., Ekelund U., Besson H., Mezzani A., Geladas N., Vanhees L. Assessment of physical activity—a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17:127–139. doi: 10.1097/HJR.0b013e32832ed875. [DOI] [PubMed] [Google Scholar]
- 25.Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Connor Gorber S., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prince S.A., Elliott C.G., Scott K., Visintini S., Reed J.L. Device-measured physical activity, sedentary behaviour and cardiometabolic health and fitness across occupational groups: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2019;16:30. doi: 10.1186/s12966-019-0790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenberger M.E., Buman M.P., Haskell W.L., McConnell M.V., Carstensen L.L. Twenty-four hours of sleep, sedentary behavior, and physical activity with nine wearable devices. Med Sci Sports Exerc. 2016;48:457–465. doi: 10.1249/MSS.0000000000000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murphy J., Uttamlal T., Schmidtke K.A., Vlaev I., Taylor D., Ahmad M. Tracking physical activity using smart phone apps: assessing the ability of a current app and systematically collecting patient recommendations for future development. BMC Med Inform Decision Making. 2020;20:1–11. doi: 10.1186/s12911-020-1025-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Voicu R.A., Dobre C., Bajenaru L., Ciobanu R.I. Human physical activity recognition using smartphone sensors. Sensors. 2019;19:458. doi: 10.3390/s19030458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neff L.J., Ainsworth B.E., Wheeler F.C., Krumwiede S.E., Trepal A.J. Assessment of trail use in a community park. Fam Community Health. 2000;23:76–84. [Google Scholar]
- 31.Craig C.L., Marshall A.L., Sjöström M., Bauman A.E., Booth M.L., Ainsworth B.E. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 32.Bull F.C., Maslin T.S., Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health. 2009;6:790–804. doi: 10.1123/jpah.6.6.790. [DOI] [PubMed] [Google Scholar]
- 33.Hallal PC, Matsudo S, Farias Jr JC. Measurement of physical activity by self-report in low- and middle-income countries: more of the same is not enough. J Phys Act Health 2012;9(Suppl. 1):S88–90. [DOI] [PubMed]
- 34.Adlakha D. Quantifying the modern city: emerging technologies and big data for active living research. Front Public Health. 2017;5:105. doi: 10.3389/fpubh.2017.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hipp J.A., Adlakha D., Eyler A.A., Chang B., Pless R. Emerging technologies: webcams and crowd-sourcing to identify active transportation. Am J Prev Med. 2013;44:96–97. doi: 10.1016/j.amepre.2012.09.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garmin. The effect of the global pandemic on active lifestyles. Available at: https://www.garmin.com/en-US/blog/general/the-effect-of-the-global-pandemic-on-active-lifestyles/. [accessed 06.05.2020].
- 37.Badger E. Density is normally good for us. That will be true after coronavirus, too. Available at: https://www.nytimes.com/2020/03/24/upshot/coronavirus-urban-density-risks.html. [accessed 18.05.2020].
- 38.Chandrabose M., Owen N., Giles-Corti B., Turrell G., Carver A., Sugiyama T. Urban densification and 12-year changes in cardiovascular risk markers. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.013199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kärmeniemi M., Lankila T., Ikäheimo T., Koivumaa-Honkanen H., Korpelainen R. The built environment as a determinant of physical activity: a systematic review of longitudinal studies and natural experiments. Ann Behav Med. 2018;52:239–251. doi: 10.1093/abm/kax043. [DOI] [PubMed] [Google Scholar]
- 40.Caruso AC. Indiana state parks see more people, officials encourage social distancing while using trails. Available at: https://www.wfyi.org/news/articles/indiana-state-parks-see-more-people-officials-encourage-social-distancing-while-using-trails. [accessed 23.04.2020].
- 41.Cross B. Austin park and trail usage up despite warnings about coronavirus. Available at: https://cbsaustin.com/news/local/austin-park-usage-up-despite-warnings-about-coronavirus. [accessed 23.04.2020].
- 42.Horton B. Closing streets to create space for walking and biking. Available at:https://www.railstotrails.org/trailblog/2020/march/27/closing-streets-to-create-space-for-walking-and-biking/. [accessed 23.04.2020].
- 43.Salvo D., Reis R.S., Sarmiento O.L., Pratt M. Overcoming the challenges of conducting physical activity and built environment research in Latin America: IPEN Latin America. Prev Med. 2014;69(Suppl. 1):S86–S92. doi: 10.1016/j.ypmed.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Babwin D, Foody K. Lack of social distancing leads to closure of parks, trails. Available at: https://apnews.com/a4c5c49410ec59f65792f280f6ff53a6. [accessed 23.04.2020].
- 45.Honey-Roses J, Anguelovski I, Bohigas J, Chireh V, Daher C, Konijnendijk C, et al. The impact of COVID-19 on public space: a review of the emerging questions.Available at: 10.31219/osf.io/rf7xa [accessed 18.05.2020]. [DOI]
- 46.McNeill L.H., Emmons K. GIS walking maps to promote physical activity in low-income public housing communities: a qualitative examination. Prev Chronic Dis. 2012;9:E17. doi: 10.5888/pcd9.110086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salvo D., Sarmiento O.L., Reis R.S., Hino A.A.F., Bolivar M.A., Lemoine P.D. Where Latin Americans are physically active, and why does it matter? Findings from the IPEN-adult study in Bogota, Colombia; Cuernavaca, Mexico; and Curitiba, Brazil. Prev Med. 2017;(Suppl. 103):S27–S33. doi: 10.1016/j.ypmed.2016.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lavizzo-Mourey R., Dorn J.M., Fulton J.E., Janz K.F., Lee S.M., McKinnon R. Department of Health and Human Services; Washington, DC: 2012. Physical activity guidelines for Americans mid-course report: strategies to increase physical activity among youth. [Google Scholar]
- 49.Sallis J.F., Bull F., Guthold R., Heath G.W., Inoue S., Kelly P. Progress in physical activity over the Olympic quadrennium. The Lancet. 2016;388:1325–1336. doi: 10.1016/S0140-6736(16)30581-5. [DOI] [PubMed] [Google Scholar]
- 50.Heath G.W., Parra D.C., Sarmiento O.L., Andersen L.B., Owen N., Goenka S. Evidence-based intervention in physical activity: lessons from around the world. The Lancet. 2012;380:272–281. doi: 10.1016/S0140-6736(12)60816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reis R.S., Salvo D., Ogilvie D., Lambert E.V., Goenka S., Brownson R.C. Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. The Lancet. 2016;388:1337–1348. doi: 10.1016/S0140-6736(16)30728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koren M. The healthiest way to sweat out a pandemic. Available at: https://www.theatlantic.com/health/archive/2020/03/coronavirus-gyms-exercise-social-distancing/608278/. [accessed 06.05.2020].
- 53.Brownson R.C., Colditz G.A., Proctor E.K. Oxford University Press; London: 2017. Dissemination and implementation research in health: translating science to practice. [Google Scholar]