Abstract
American Indian/Alaska Native and First Nations communities suffer from health disparities associated with multiple forms of trauma exposure. Culturally appropriate interventions are needed to heal current and historical trauma wounds. Although there are evidence-based trauma interventions for other populations, few have been implemented or evaluated with Native communities. Understanding the extant research on trauma interventions in Native communities is crucial for advancing science and filling gaps in the evidence base, and for meeting the needs of underserved people. In this systematic review of the literature on trauma interventions in Native communities in the United States, Canada, Australia, and New Zealand, we identified 15 studies representing 10 interventions for historical and/or current trauma. These studies involved the community to some extent in developing or culturally adapting the interventions and suggested positive outcomes with regard to historical and interpersonal trauma symptoms. However, notable limitations in study design and research methods limit both internal validity and external validity of these conclusions. Only one study attempted (but did not achieve) a quasi-experimental design, and small sample sizes were persistent limitations across studies. Recommendations for researchers include working in partnership with Native communities to overcome barriers to trauma intervention research and to increase the rigor of the studies so that ongoing efforts to treat trauma can yield publishable data and communities can secure funding for intervention research.
Keywords: Native communities, American Indian/Alaska Native, Interpersonal trauma, Historical trauma, Interventions, Systematic review
Introduction
Native communities throughout the world, including American Indian and Alaska Natives (AI/ANs) and First Nations peoples, share two risk pathways associated with trauma exposure at both historical (e.g., boarding schools and forced removal from traditional lands) and current (e.g., adult interpersonal trauma and early childhood trauma) levels (Brave Heart, Chase, Elkins, & Altschul, 2011; Evans-Campbell, 2008). Generations of Native families have suffered from systemic policies of discrimination and violence that have greatly affected not only the individuals who experienced the trauma firsthand but also their descendants (Brave Heart & DeBruyn, 1998; Brave Heart-Jordan & DeBruyn, 1995). It has been theorized that historical trauma facilitates experiences of current interpersonal victimization (Brave Heart, 2003; Walls & Whitbeck, 2012), as AI/ANs have the highest rates of violence against women, child abuse and neglect, and traumatic injuries among all ethnic groups in the United States (Rosay, 2016; Yuan, Koss, Polacca, & Goldman, 2006). Native people are at significant risk of experiencing trauma in their lifetimes, and effective, culturally appropriate trauma interventions are needed. In this review, we report findings from our examination of the research literature regarding trauma interventions studied in Native communities and make recommendations for future research. Our review included interventions for historical trauma and current trauma, as described below.
Historical Trauma
Historical trauma is defined as the cumulative and generational emotional, physical, and psychological harm stemming from mass trauma exposure (Brave Heart & DeBruyn, 1998; Evans-Campbell, 2008). Historical trauma encompasses not only trauma exposure, but also the psychological and social responses to the traumatic event exhibited by the victimized group (Brave Heart & DeBruyn, 1998; Evans-Campbell, 2008). Historical trauma is rooted in experiences of discrimination, systemic abuse, and forced assimilation by the dominant society through law, education, and religion (Brave Heart, 1998; Evans-Campbell, 2008; Morrisette, McKenzie, & Morrisette, 1993). In the United States and Canada, Native communities’ experiences with historical trauma and loss stem from colonization practices, including forced removal of people from traditional lands, genocidal polices, and removal of children from families to government-operated boarding schools (Brave Heart, 2003; Brave Heart-Jordan & DeBruyn, 1995; Evans-Campbell, 2008; Whitbeck, Chen, Hoyt, & Adams, 2004), which has resulted in lasting negative effects for Native people, families, and communities.
One specific occurrence of historical trauma contributing to high rates of child abuse and neglect as well as disruptions in family functioning among Native people was government-run boarding schools, which lasted in the United States from 1860s to 1970s and from 1870s to 1990s in Canada (Royal Commission on Aboriginal Peoples, 1996; U.S. Department of Health and Human Services, 2001). In boarding schools, children were punished for speaking their traditional languages and engaging in their cultural and spiritual traditions as an attempt to forcibly assimilate the children into dominant Western culture —in other words, to “kill the Indian and save the man” (Brave Heart & DeBruyn, 1998; Jacobs, 2006; Whitbeck, Chen, et al., 2004). Children who attended boarding schools experienced high rates of physical and sexual abuse, starvation, and prolonged separation from families, starting as early as five years old and lasting for years (Brave Heart & DeBruyn, 1998; Brave Heart-Jordan & DeBruyn, 1995; Jacobs, 2006). Many children perished in these schools and were not returned to their families. Upon returning home, boarding school survivors suffered post-traumatic stress symptoms and negative emotions related to their experiences. Trauma from boarding schools affected the children, their families left behind, and their offspring, and became part of a cycle of intergenerational trauma that continues to affect Native communities today (Bombay, Matheson, & Anisman, 2011, 2014).
Following historically traumatic events, people who experience the trauma and their descendants may exhibit historical trauma responses (Brave Heart, 2003; Brave Heart & DeBruyn, 1998; Brave Heart et al., 2011; Evans-Campbell, Walters, Pearson, & Campbell, 2012). A historical trauma response includes rumination over past events, survivor’s guilt, unresolved grief, anger, depression, anxiety, and psychic numbing (Duran, Duran, Brave Heart, & Yellow Horse-Davis, 1998; Kestenberg, 1982). The historical trauma response is well documented in children of Holocaust survivors (Fogelman, 1988; Rowland-Klein & Dunlop, 1998), Japanese internment camp survivors (Nagata & Cheng, 2003; Nagata, Trierweiler, & Talbot, 1999), and Native people in North America and throughout the world (Brave Heart, 1998; Brave Heart & DeBruyn, 1998; Duran et al., 1998). The historical trauma response, if not addressed, may be passed down from generation to generation through the intergenerational transmission of trauma.
Intergenerational transference of trauma is suggested to occur when trauma symptoms are left untreated and later manifest in descendants of the victimized group (Brave Heart, 1998; Evans-Campbell, 2008; Walls & Whitbeck, 2012). Research suggests that trauma memories are passed down through generations via biological, cultural, social, and psychological mechanisms and contribute to the health disparities prevalent in Native communities today (Wesley-Esquimaux & Smolewski, 2004). Intergenerational trauma is associated with greater mental illness symptoms, substance use problems, and physical health problems among descendants of trauma survivors (Brave Heart, 2003; Brave Heart & DeBruyn, 1998; Evans-Campbell et al., 2012). Additionally, descendants of historically traumatized groups are more likely to develop post-traumatic stress disorder (PTSD) after experiencing a traumatic event in their own lives compared with members of groups with no historical trauma (Beals et al., 2005).
Historical trauma is also associated with a breakdown in healthy family connections and functioning, which contributes to the mental and physical health consequences observed in offspring of boarding school attendants (Bombay et al., 2014; Brave Heart & DeBruyn, 1998; Jacobs, 2006). Researchers found that people raised in government boarding schools were more likely to report feeling overwhelmed or inadequate when parenting, as they lacked proper parenting role models while growing up (Brave Heart & DeBruyn, 1998; Horejsi, Craig, & Pablo, 1992; Jacobs, 2006). Children of boarding school attendees further reflect this breakdown in parenting with greater reported childhood neglect and abuse and fewer experiences of parental warmth (Walls & Whitbeck, 2012). In this way, historical trauma gives rise to personal abuse and neglect, which in turn has been shown to contribute to negative outcomes across a broad spectrum of health behaviors and problems (Felitti et al., 1998; Oral et al., 2016).
Historical trauma also contributes to negative health outcomes by impeding the development of healthy coping behaviors that have served Native communities for millennia. Research suggests that children of families with unresolved historical trauma are more likely to internalize distressing thoughts and emotions to avoid upsetting or traumatizing their caregivers further (Evans-Campbell, 2008; Walters, Evans-Campbell, Simoni, Ronquillo, & Bhuyan, 2006). Children who are not able to express negative feelings may have difficulty learning coping skills from parents or guardians, and this inhibits their ability to cope with trauma and life stress in adulthood (Evans-Campbell, 2008; Walls & Whitbeck, 2012; Walters et al., 2006). This generational breakdown in learning healthy coping skills may contribute to the current health disparities experienced by Native communities. Specifically, individuals who do not learn healthy ways of coping may rely on harmful strategies, such as using substances, to manage negative emotions instead (Cooper, Russell, & George, 1988; Wolsko, Lardon, Mohatt, & Orr, 2007).
Current Trauma
Interpersonal Trauma
Scholars have suggested that unresolved historical trauma contributes to and exacerbates current experiences of interpersonal trauma, with dire consequences for affected individuals and communities (Brave Heart, 2003; Walls & Whitbeck, 2012). The connection between historical and interpersonal trauma is reflected in high rates of reported community violence, interpersonal violence, and child abuse in Native communities (Beals et al., 2013; Brockie, Dana-Sacco, Wallen, Wilcox, & Campbell, 2015; Deters, Novins, Novins, Fickenscher, & Beals, 2006; Gone & Trimble, 2011; Oetzel & Duran, 2004; Rosay, 2016). In the United States, both male and female AI/AN adults experience higher rates of domestic violence, sexual violence, homicide, and other violent crimes compared to non-Hispanic White populations (Rosay, 2016; Yuan et al.,2006). These experiences of interpersonal trauma are associated with higher rates of suicide, substance use disorders, mental health problems, and legal problems for AI/ANs (Beals et al., 2005; Brockie et al., 2015; Deters et al., 2006; Substance Abuse and Mental Health Services Administration [SAMHSA], 2017), and have been shown to contribute to ongoing health disparities (Boyd-Ball, Manson, Noonan, & Beals, 2006; Evans-Campbell, Lindhorst, Huang, & Walters, 2006).
Early Childhood Trauma
Native children are at greater risk for experiencing and witnessing violence in the family compared to other ethnic/racial groups (Brockie et al., 2015; Rosay, 2016; Yuan et al., 2006) and report high rates of adverse childhood experiences (ACEs) before age 18. The term ACEs was developed by Felitti et al. (1998) in a large-scale health survey conducted with Kaiser Permanente healthcare recipients. The ACE questionnaire developed in this study measures emotional and physical neglect as well as verbal, physical, and sexual abuse experienced in childhood. Aside from personal experiences of abuse in childhood, ACEs also include disruptions in healthy family functioning, such as parental mental illness, family violence, and loss of a parent through divorce or incarceration (Felitti et al., 1998).
One study conducted in the United States found that AI/AN youth are more likely than their non-Native counterparts to report experiencing five or more ACEs before age 18 (Kenney & Singh, 2016). This finding is troubling, particularly when contextualized in relation to research indicating that ACE scores greater than four are associated with significantly increased risk of developing mental and physical health problems later in life and early mortality (Brockie et al., 2015; Felitti et al., 1998). Trauma exposure in childhood is linked with greater likelihood of developing PTSD in adulthood, and AI/ANs have higher rates of PTSD than non-Native populations (Beals et al., 2013; Deters et al., 2006). Research suggests that trauma is a pervasive problem throughout the lifespan of many Native people and that treating childhood trauma could have wide-reaching positive effects on a wide range of health behaviors and outcomes (Weissbecker & Clark, 2007).
Barriers to Mental Health Services in Native Communities
Native communities are underserved when it comes to mental health services and programming, with the majority of children and adults who need mental health services going untreated (Beals et al., 2005; Ringel & Sturm, 2001). Children who do receive treatment primarily receive it from school-based programs (Langley, Nadeem, Kataoka, Stein, & Jaycox, 2010), but the effectiveness of treatment remains unknown; furthermore, Native adults do not have access to school-based supportive programs and have few options for treatment. Many Native people who want help and are referred to treatment never receive it because they are not supported by the existing services available in their community (Beals et al., 2005; Johnson & Cameron, 2001; LaFromboise, Albright, & Harris, 2010; Manson, 2000; Oetzel et al., 2006; Wexler, Silveira, & Bertone-Johnson, 2012).
Research on barriers to implementing mental health programs with Native communities suggests that low attendance and retention rates may be attributed to two factors: the lack of local treatment providers in often rural and isolated communities, and distrust toward formal mental health services (Duran et al., 2005; Johnson & Cameron, 2001; Manson, 2000). People from rural communities may have to travel far distances to see a provider, requiring them to take time away from work and family obligations. Community-based mental health service providers are often overextended and unable to keep up with the community’s needs (Duran et al., 2005; Johnson & Cameron, 2001; Manson, 2000). Additionally, many mental health service providers, while trained to treat PTSD symptoms, are not equipped to address symptoms of historical trauma (Gone, 2010). Apart from these system-level barriers to successful trauma interventions, the avoidant symptoms of trauma-based mental illness can prevent people from attending or completing trauma interventions (Trusz, Wagner, Russo, Love, & Zatzick, 2011). Therefore, trauma intervention research must focus on addressing system-level, logistical, and psychological barriers to mental health services for AI/ANs.
Evidence-Based Trauma Interventions
Research with non-Native populations has yielded six evidence-based treatments (EBTs) for treating trauma and its associated symptoms. These EBTs include trauma-focused cognitive behavioral therapy (TF-CBT; Cohen, Deblinger, Mannarino, & Steer, 2004; Deblinger, Mannarino, Cohen, & Steer, 2006), Seeking Safety (Najavits, 2004), prolonged exposure therapy (PE; Foa & Kozak, 1986), cognitive processing therapy (CPT; Monson et al., 2006), eye-movement desensitization and reprocessing (EMDR; Shapiro, 2001), and child-parent psychotherapy (CPP; Lieberman, Ippen, & Van Horn, 2006; Lieberman, Van Horn, & Ippen, 2005). The efficacy of EBTs for trauma is well-documented in other populations (Chorpita & Southam-Gerow, 2006; Keane, Marshall, & Taft, 2006; Silverman et al., 2008), and research suggests that treatment is associated with improvements in both physical health and psychological health (Weissbecker & Clark, 2007). These findings suggest that Native communities could benefit from trauma interventions. However, few interventions with this population have been evaluated and published in peer-reviewed sources, and it is unknown whether existing treatments would be culturally appropriate or effective for Native communities.
Of the EBTs for trauma, only TF-CBT and Seeking Safety have been culturally adapted for use in Native communities. Trauma-focused CBT was originally designed for sexually abused children and has been adapted for other types of interpersonal trauma (Bigfoot & Schmidt, 2010; Cohen et al., 2004; Deblinger et al., 2006). The intervention includes 8–24 psychoeducation sessions that teach cognitive restructuring skills and use exposure to trauma triggers to help recognize and shift maladaptive thoughts and behaviors (Cohen et al., 2004; Deblinger et al., 2006). Trauma-focused CBT also involves a narrative component that allows people to tell their trauma stories and explore the negative feelings related to these experiences (Cohen et al., 2004; Deblinger et al., 2006). This intervention has been used with African American and Hispanic populations, and was adapted for use with Native communities (Bigfoot & Schmidt, 2010).
Seeking Safety (Najavits, 2004) is an EBT designed to address substance use problems in addition to trauma, and addresses cognitive, behavioral, and interpersonal problems related to trauma and substance abuse concurrently. Seeking Safety also includes a case management component that helps participants make a plan for the future and obtain referrals to housing, job support, medical care, and other services they might need (Najavits, 2004). This intervention has been implemented successfully with adolescents and adults, and has been used with ethnic minorities in the United States, including African Americans, Hispanics, and Asian Americans (Najavits et al., 2009). Seeking Safety was adapted for use with a First Nations community in Canada (Marsh, Cote-Meek, Young, Najavits, & Toulouse, 2016).
Culturally Relevant Interventions
Culturally relevant interventions include those that are developed from the ground up for a particular cultural group (i.e., culturally grounded interventions) and those that are adapted for use in a cultural group other than the one in which the interventions were originally developed. Cultural adaptation is defined as the systematic modification of an existing EBT to include aspects of language, culture, and context for a specific minority group (Bernal, Jim enez-Chafey, & Domenech Rodr ıguez, 2009). The limited research on culturally adapted interventions with Native communities is concerning, as researchers have argued that mental healthcare providers have a moral and ethical responsibility to provide effective interventions for minority groups that reflect cultural values and contexts relevant to health and well-being (Sue & Sue, 2003; Trimble & Fisher, 2006). Additionally, it appears that culturally adapting EBTs can be helpful—a meta-analytic review of culturally adapted mental health interventions found an overall positive effect of cultural adaptation (d = 0.45 across 76 studies; Grinner & Smith, 2006), suggesting a moderate effect in favor of culturally adapted EBTs for minority groups. Despite support for the effectiveness of culturally adapted interventions (e.g., Grinner & Smith, 2006), some researchers have questioned the necessity of changing interventions to fit a given culture (Elliott & Mihalic, 2004; O’Donohue & Benuto, 2010) and recommend implementing standard EBTs first.
Researchers who support using unmodified EBTs across cultural groups argue that culturally adapting EBTs may dilute the active components of the intervention or otherwise impair their efficacy (Elliott & Mihalic, 2004; O’Donohue & Benuto, 2010). That is, when interventions are culturally adapted, important aspects of the original EBT may be lost, resulting in a less effective intervention. On the other hand, not adapting interventions may impair their uptake in a community, and the effective strategies are then unable to reach the people who need them. Mejia, Leijten, Lachman, and Parra-Cardona (2017) argue that intervention researchers should not debate about the effectiveness of non-adapted EBT versus culturally adapted interventions, but instead use both approaches (Mejia et al., 2017). This encourages researchers to be flexible and responsive to community needs and use aspects of non-adapted EBTs, culturally adapted, and culturally grounded interventions when appropriate (Mejia et al., 2017). Despite concerns that cultural adaptation may impair the efficacy of the original EBTs (Elliott & Mihalic, 2004; O’Donohue & Benuto, 2010), culturally relevant interventions are needed to enlist and retain participants (Sue & Sue, 2003; Trimble & Fisher, 2006).
While there are no agreed-upon guidelines for culturally adapting interventions, one cultural adaptation framework proposes using surface-level or deep-level structure changes to adapt existing EBTs depending on the needs of the population (Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1999; Resnicow, Soler, Braithwaite, Ahluwalia, & Butler, 2000). Surface structure adaptations (e.g., adding culturally relevant imagery or music) and deep structure adaptations (e.g., using culturally relevant program content) aim to make interventions more appealing to communities and more relevant to specific cultural values and ways of knowing (Resnicow et al., 1999, 2000). Cultural adaptations are intended to promote participant engagement by making interventions more responsive to communities’ unique needs and perspectives. However, while culturally adapting EBTs allows interventions to reflect cultural values and preferences, cultural adaptation is not always enough to serve a community’s needs. This is especially the case when existing EBTs are not designed to address specific culture-bound systems like the historical trauma response. In these instances, and when the community desires an intervention that does not yet exist, it is necessary to develop new interventions from the ground-up.
In culturally grounded interventions, communities design and implement new treatments from the ground up based on knowledge of the needs and strengths of their people (Okamoto, Kulis, Marsiglia, Steiker, & Dustman, 2014). Culturally grounded interventions emphasize the unique cultural and social context of a population as the focus of intervention (Marsiglia & Kulis, 2009; Okamoto, Kuli, et al., 2014; Okamoto, Helm, et al., 2014). A culturally grounded approach is especially useful when existing EBTs do not address symptoms or problems specific to the culture. For example, symptoms associated with historical trauma in Native communities are not addressed by existing EBTs, so culturally grounded interventions are necessary for treating these culture-bound symptoms. Grounded interventions are also necessary when the symptoms result from trauma caused by the dominant cultural group, and using non-adapted EBTs is associated with this dominance. In these cases, non-adapted EBTs may make trauma symptoms worse instead of treating them. Both culturally grounded and culturally adapted interventions are potentially useful approaches used to address the unique needs of underserved groups.
There are many options for implementing trauma interventions with Native communities: non-adapted EBTs, culturally adapted EBTs (with either surface or deep adaptations), and developing new, culturally grounded interventions. We reviewed the literature on trauma interventions implemented in Native communities in the United States, Canada, Australia, and New Zealand to identify non-adapted and culturally relevant (e.g., culturally adapted or culturally grounded) treatments for trauma and to make recommendations for future research.
Current Study
Native communities are disproportionally affected by traumatic experiences and their associated negative consequences (Beals et al., 2013; Deters et al., 2006) and are underserved with regard to mental health services and trauma interventions (Beals et al., 2005; Ringel & Sturm, 2001; Wexler et al., 2012). Given the notable health disparities associated with trauma, we aimed to examine current intervention strategies that have been used to treat historical trauma, interpersonal trauma, and/or early childhood trauma in Native communities in the United States, Canada, Australia, and New Zealand. Specifically, we examined (a) trauma interventions used with Native populations, (b) characteristics of participants, (c) intervention outcomes, (d) how the intervention incorporated culture, and (e) intervention implementation, evaluation methods, and study design, including community involvement and study limitations.
Method
Inclusion and Exclusion Criteria
This systematic review included English language, peer-reviewed, empirical articles on non-adapted, culturally adapted, and culturally grounded trauma interventions implemented with Native communities in the United States, Canada, Australia, and New Zealand. Trauma interventions were defined as any interventions that aimed to treat symptoms stemming from historical, interpersonal, or early childhood trauma. Qualitative empirical studies were included if they assessed some form of an intervention outcome. Mental health and substance use interventions were considered for inclusion only if they included assessments of trauma. Published empirical studies that did not report data from Native people separately from non-Native samples were excluded, and interventions not reporting outcome data were excluded.
Search Strategy
We searched the PubMed/MEDLINE, PsycINFO, PsycArticles, EMBASE, and ERIC databases. Search terms for “Native communities” included the following: “American Indian OR Native American OR Alaska Native OR Indigenous OR Aboriginal OR Native Communities OR Inuit OR Maori OR First Nations OR Native Hawaiian OR Samoan OR Tongas OR Taino OR Chamorro.” Search terms for “trauma” included the following: “PTSD OR historical trauma OR emotional trauma OR sexual abuse OR child abuse OR child neglect OR intergenerational trauma OR interpersonal trauma OR interpersonal violence OR childhood trauma OR sexual assault OR domestic violence OR victimization OR adverse childhood experiences.” Finally, search terms for “treatment” included the following: “prevention OR intervention OR therapy OR treatment” (Fig. 1).
Fig. 1.
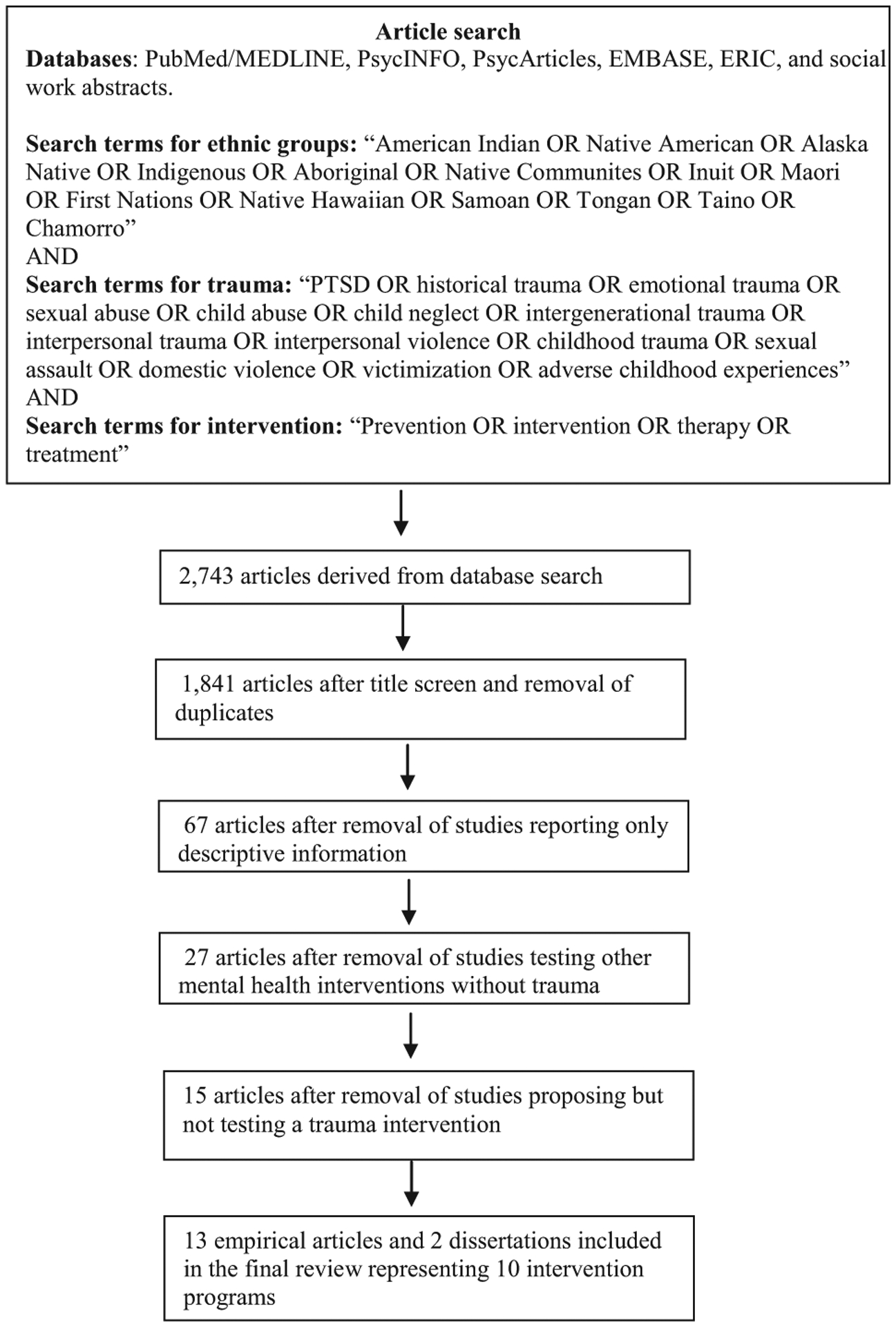
Flowchart of article selection process for the review selection
The search screening process was conducted in June 2019 and generated 13 unduplicated empirical reports and two dissertations on trauma interventions with Native communities. The dissertations were included because they presented data congruent with the peer-reviewed empirical reports. Among the 15 studies in this review, 10 used unique data sets and five included data sets in which the sample sizes changed over continued data collection. Specifically, Morsette et al. (2009), Morsette, van den Pol, Schuldberg, Swaney, and Stolle (2012), and Hepler (2013) reported on the same data set collected from 2003 to 2011 for the Cognitive Behavioral Intervention for Treating Trauma in School (CBITS) intervention. Additionally, Brave Heart (1999a) reported on gender differences not reported in Brave Heart’s (1998) primary Return to the Sacred Path intervention.
After an initial screening process, duplicate studies, studies with content outside the inclusion criteria, and studies reporting only epidemiological data on historical, interpersonal, and childhood trauma were excluded from the review. Next, studies proposing new trauma interventions without assessment information or outcome data were removed. Finally, interventions tested with Native people targeting other psychological disorders were removed if their assessments did not include trauma symptoms. The full-review research strategy and selection process are summarized in Figure 1.
Findings
The screening process yielded 13 peer-reviewed studies and two dissertations eligible for inclusion in this review. These studies investigated 10 different trauma-related interventions, with three targeting historical trauma, three targeting interpersonal trauma, three targeting early childhood trauma, and one targeting both historical trauma and early childhood trauma. Interventions included culturally adapted EBTs and culturally grounded programs; no studies examining standard (non-adapted) EBTs were reported in the literature (Table 1).
Table 1.
Summary of trauma interventions in native communities (N = 10)
| Intervention | Study | Trauma type | Sample/Location | Trauma measure | Intervention content | Treatment design | Assessment method | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Return to the Sacred Path | Brave Heart (1998)a | Historical | SD, United States
|
Lakota Grief experience questionnaire | Psychoeducational | 4-day group sessions | Quantitative & Qualitative |
|
| Return to the Sacred Path | Brave Heart (1999a)a | Men
|
||||||
| Oyate Ptayela | Brave Heart (1999b) | Historical (parenting) | SD, United States
|
Self-report of historical trauma | Psychoeducational | 7 group sessions | Qualitative |
|
| Cultural approach to the Incredible Years Parenting Program | Dionne et al. (2009) | Historical (parenting) | CA, United States
|
Interview about historical trauma | Culturally adapted motivational interviewing and Incredible Years Parenting Program | 14 sessions Control group
|
Quantitative & Qualitative |
|
| Our Life | Goodkind et al. (2012b)b | Historical (parenting) | NM, United States
|
|
Psychoeducational | 27 group sessions
|
Quantitative & Qualitative |
|
| Our Life | Goodkind et al. (2012a)b | Early childhood | NM, United States
|
|
Psychoeducational | 27 group sessions
|
Quantitative & Qualitative |
|
| Traditional Healing | Heilbron and Guttman (2000) | Interpersonal | Canada
|
Self-report of interpersonal violence | Healing circle with CBT elements | 10 group sessions | Qualitative |
|
| Cross Cultural Mental Health Program | Thomas and Bellefeuille (2006) | Interpersonal/Historical | Canada
|
Self-report attendance at a boarding school | Healing circle with focusing elements | 8 group sessions | Qualitative |
|
| Indigenous Healing and Seeking Safety | Marsh et al. (2016)/Marsh (2016) (dissertation) | Interpersonal/Historical | Canada
|
|
Seeking Safety | 13 group sessions (separated by gender) | Quantitative & Qualitative |
|
| Group Treatment for Sexually Abused American Indian Adolescents | Ashby et al. (1988) | Early childhood | WA, United States
|
Reported sexual abuse | Healing circles, art therapy, and didactic exercises | 10 group sessions
|
Quantitative & Qualitative |
|
| Culturally Adapted CBITS | Morsette et al. (2009)a | Early childhood | MT, United States
|
|
CBITS | 10 group sessions (in school)
|
Quantitative |
|
| Culturally Adapted CBITS | Morsette et al. (2012)a | Early childhood | MT, United States
|
Quantitative & Qualitative |
|
|||
| Culturally Adapted CBITS | Hepler (2013)a (dissertation) | Early childhood | MT, United States
|
Quantitative & Qualitative |
|
|||
| THRIVE | Goodkind et al. (2010) | Early childhood | NM, United States
|
|
CBITS | 10 group sessions (in school)
|
Quantitative |
|
CBITS, Cognitive Behavioral Intervention for Treating Trauma in Schools; CBT, Cognitive Behavioral Therapy; CPSS, Child PTSD Symptoms Scale; HLASS, Historical Loss and Associated Symptom Scale; HLS, Historical Loss Scale; LES, Life Events Scale; REVS, Recent Exposure to Violence Scale; THRIVE, Teen Health Resiliency Intervention for Violence Exposure; TSC-40, Trauma Symptoms Checklist- 40.
Same sample.
Same intervention, different sample.
Trauma Interventions
Historical Trauma
Return to the Sacred Path, the first intervention for historical trauma, was developed with the Lakota tribe and was a psychoeducation program with human service providers and community members (Brave Heart, 1998, 1999a). The aim of this intervention was to raise awareness about the negative impact of historical trauma on Native communities and to teach participants traditional bereavement practices to cope with historical loss. This intervention was influential in the development of historical trauma-informed parenting programs utilized in the Oyate Ptayela and Our Life interventions that followed (e.g., Brave Heart, 1998, 1999b; Goodkind, LaNoue, Lee, Freeland, & Freund, 2012b).
Three of the four historical trauma interventions focused on parenting and working to halt the intergenerational transmission of trauma. The Oyate Ptayela and Our Life parenting programs used a similar structure of raising awareness about historical trauma and teaching traditional coping skills as well as traditional parenting practices, communication skills, and alternative punishment strategies (Brave Heart, 1999b; Goodkind, LaNoue, Lee, Freeland, & Freund, 2012a; Goodkind et al., 2012b). This content was designed to facilitate intergenerational healing by improving parent–child relationships through teaching healthier, traditional parenting skills lost to Native communities through colonization.
In addition, a culturally adapted version of the Incredible Years Parenting Program (IYPP; Webster-Stratton, 2007), an intervention to promote healthy parenting and family relationships, was implemented in two Native communities in California (Dionne, Davis, Sheeber, & Madrigal, 2009). The first phase of this intervention included a culturally adapted motivational interviewing session to encourage parents to talk through their historical and interpersonal trauma experiences. In one-on-one sessions with trained interviewers, participants discussed their parental and family functioning, exploring the perceived strengths and weaknesses of their families. In the second phase of this intervention, parents worked on healing trauma, learning traditional parenting strategies, and improving parent–child communication skills within the IYPP framework during in-home visits. Of the parenting programs, only the Our Life intervention (Goodkind et al., 2012a, 2012b) included both parents and children in the assessment and intervention process.
Interpersonal Trauma
Interventions targeting trauma from adult interpersonal violence (n = 3) overlapped with interventions targeting elements of historical trauma (n = 2). One of these interventions, Indigenous Healing and Seeking Safety, targeted historical trauma, interpersonal trauma, and substance abuse (Marsh, 2016; Marsh et al., 2016); the Cross Culture Mental Health Program focused on boarding school attendants affected by interpersonal violence (Thomas & Bellefeuille, 2006); and the Traditional Healing intervention focused on Indigenous women with histories of domestic or sexual violence (Heilbron & Guttman, 2000). The Indigenous Healing and Seeking Safety intervention was adapted to include sessions targeted at historical trauma and historical loss symptoms. The adapted intervention emphasized elements of the medicine wheel and taught traditional activities to foster sobriety and heal trauma. The Cross-Cultural Mental Health Program (Thomas & Bellefeuille, 2006) and Traditional Healing (Heilbron & Guttman, 2000) interventions used traditional healing circles integrated with elements of Western psychotherapy. The healing circles were used to create a safe place in which to hold discussions about trauma, and they incorporated traditional spiritual and healing practices with cognitive behavioral therapy (CBT) (Heilbron & Guttman, 2000) and focusing (Thomas & Bellefeuille, 2006). Focusing is self-awareness technique used to change self-critical thoughts and manage negative thoughts related to trauma (Gendlin, 1996). These interventions were used to teach coping skills, increase social support, and teach healthy ways to handle stress and trauma in the future, with an emphasis on Native tradition and culture.
Early Childhood Trauma
Childhood trauma interventions for Native youth have been implemented in schools (n = 2) (Goodkind, LaNoue, & Milford, 2010; Hepler, 2013; Morsette et al., 2009, 2012), with mental health service providers (n = 1) (Ashby, Gilchrist, & Miramontez, 1988), and with families in community settings (n = 2) (Goodkind et al., 2012a, 2012b). The CBITS (Jaycox, 2004) program was culturally adapted for reservation youth with PTSD and depression and was implemented in schools. This intervention used CBT strategies and also incorporated traditional beliefs and narrative practices in the Teen Health Resiliency Intervention for Violence Exposure (THRIVE) and Culturally Adapted CBITS interventions (Goodkind et al., 2010; Hepler, 2013; Morsette et al., 2009, 2012). In addition to school-based programs, the Group Treatment for Sexually Abused American Indian Adolescents program was implemented with sexually abused Native females who were referred to the program by a social service provider. In this program, adolescents took part in traditional practices, such as beading and ceremonial talking circles, that were paired with elements of art therapy and didactic exercises (Ashby et al., 1988). The final intervention included in this review was the child portion of the Our Life (Goodkind et al., 2012a, 2012b) family trauma intervention. The aim of this program was to disrupt intergenerational trauma by addressing both parental historical trauma-related symptoms and childhood trauma symptoms in children. This was accomplished through the use of psychoeducation and skills training to address parental historical trauma, teach parenting skills, and help children cope with current trauma-related symptoms.
Study Samples
Although the inclusion criteria for this review allowed for trauma interventions tested in Native communities in the United States, Canada, Australia, and New Zealand, all studies included in this review were conducted in North America (seven in the United States and three in Canada). No trauma interventions conducted outside of North America met inclusion criteria for the current review. The adults in the historical and interpersonal trauma interventions were primarily female and ranged in age from 19 to 68. The Native youth in the early childhood trauma interventions ranged in age from 7 to 17 and included females and males. Overall sample sizes were small and ranged from 3 to 59 participants, with seven interventions reporting sample sizes of fewer than 20 participants. Larger samples included participants completing the interventions at multiple time points that were later grouped together. In addition to small sample sizes, there also was participant attrition between pre- and post-intervention assessments, thus reducing already small intervention samples to even smaller numbers.
Intervention Outcomes
Intervention outcomes were reported using both qualitative and quantitative data. Interventions appeared to be helpful, with outcomes ranging from reduced trauma symptoms to increased confidence in parenting and improved family communication. Specifically, quantitative outcomes for the historical and interpersonal trauma interventions revealed decreased anger, sadness, and grief (Brave Heart, 1998, 1999a); decreased historical loss and associated symptoms (Goodkind et al., 2012b; Marsh, 2016); decreased trauma symptoms (Marsh, 2016); and improved parent–child relationship ratings among adult participants (Dionne et al., 2009; Goodkind et al., 2012a, 2012b). The results for youth followed the same trend, suggesting reduced PTSD symptoms (Goodkind et al., 2010; Hepler, 2013; Morsette et al., 2009, 2012), increased positive coping skills, and better overall quality of life (Goodkind et al., 2012a), and increased self-esteem (Ashby et al., 1988; Goodkind et al., 2012a). However, the study that examined posttest self-esteem scores among youths who completed the Group Treatment for Sexually Abused American Indian Adolescents Program found that, while improved from baseline, self-esteem scores remained lower than those of youth who had never been victimized (M = 56 vs. M = 64; Ashby et al., 1988).
The qualitative outcome data supported the quantitative outcomes in that the participants reported greater connection with their communities and better understanding of historical trauma. Additionally, the participants reported enjoying the traditional components of the interventions and reflected that they experienced greater connection to their culture. However, some participants reported that the traditional spiritual aspects of the interventions conflicted with their Christian beliefs. This conflict prompted some people to leave the interventions or not participate in all of the intervention sessions (Goodkind et al., 2012a, 2012b; Thomas & Bellefeuille, 2006), suggesting that some culturally relevant interventions may only be appropriate for people with connection to or interest in traditional spiritual practices. While the findings as a whole pointed to positive post-intervention outcomes, the THRIVE intervention found that PTSD symptoms that had decreased post-intervention had returned to pre-intervention levels when assessed six months later (Goodkind et al., 2010). This finding calls into question the long-term effectiveness of trauma interventions.
Culturally Relevant Interventions
This review included both culturally adapted (n = 7) and culturally grounded (n = 3) trauma interventions. Three of the adapted interventions used talking or healing circles in tandem with non-adapted psychotherapeutic practices. Both the Traditional Healing and Cross-Cultural Mental Health interventions used this approach to treat adult interpersonal trauma (Heilbron & Guttman, 2000; Thomas & Bellefeuille, 2006). In the Cross-Cultural Mental Health intervention, researchers taught elements of CBT in the context of a talking circle. The content of the CBT program used in this study was not culturally adapted, but the method of delivery was changed to reflect the ceremonial practices of the talking circle (Thomas & Bellefeuille, 2006). Similarly, the Traditional Healing intervention utilized a healing circle, but with focusing instead of CBT as the non-adapted therapeutic element (Heilbron & Guttman, 2000). Additionally, the Group Treatment for Sexually Abused American Indian Adolescents program used talking circles with elements of art therapy and didactic exercise in a treatment program with Native girls with a history of sexual abuse (Ashby et al., 1988).
The remaining four adapted interventions included culturally adapted versions of CBITS (Goodkind et al., 2010; Hepler, 2013; Morsette et al., 2009, 2012), Seeking Safety (Marsh, 2016; Marsh et al., 2016), and the Incredible Years Parenting Program with motivational interviewing (Dionne et al., 2009). These interventions were selected for cultural adaptation because they were evidence-based and had been successfully adapted for other racial/ethnic minority and high-risk communities in previous studies (Boden et al., 2012; Lynch, Heath, Mathews, & Cepeda, 2012; Ngo et al., 2008). In these interventions, researchers worked with communities to adapt program lessons, measurement tools, and delivery methods to better reflect Native values and beliefs.
The final three trauma interventions in this review resulted from a culturally grounded approach to developing new trauma interventions from the ground up. The Return to the Sacred Path (Brave Heart, 1998, 1999a) and Oyate Ptayela (Brave Heart, 1999b) interventions used a ground-up approach to develop historical trauma interventions rooted in traditional Lakota practices. In these interventions, participants were taught about the impact of historical trauma on the Lakota people, traditional ways to cope with and express grief, and in one study, traditional parenting skills (Brave Heart, 1999a, 1999b). Furthermore, the Our Life intervention (Goodkind et al., 2012a, 2012b) was a new child-parent intervention developed to address historical trauma and teach parenting skills in addition to treating trauma-related symptoms in children.
Design, Evaluation, and Research Methods
Intervention Design
All of the trauma interventions were delivered through group sessions, with some sessions separated by participant gender or age. This approach sought to ensure that individuals were comfortable discussing their traumas and that the intervention topics were age- and gender-appropriate. Only the culturally adapted IYPP intervention attempted to use a quasi-experimental design with random assignment to intervention and waitlist control groups (Dionne et al., 2009). However, due to funding problems, the researchers were unable to collect data from the waitlist participants, prohibiting any between-group comparisons. In the Group Treatment of Sexually Abused American Indian Adolescents program, a group of sexually victimized girls who completed the intervention was compared to a group of non-victimized girls of the same age who did not receive the intervention (Ashby et al., 1988). Finally, the Our Life (Goodkind et al., 2012a, 2012b) family trauma intervention compared outcomes among three groups: families who had completed a screening process but did not complete the intervention, families who had attended fewer than half of the intervention sessions, and families who had completed more than half of the sessions.
Most interventions (n = 6) used both qualitative and quantitative outcome assessments, while the remaining used solely qualitative (n = 3) or quantitative (n = 1) assessments. Assessments mostly consisted of participant self-report measures (n = 8), with only two studies using data collected from other informants. Specifically, the Culturally Adapted CBITS intervention included qualitative assessments from intervention facilitators and teachers (Hepler, 2013; Morsette et al., 2012), and Our Life (Goodkind et al., 2012a, 2012b) included both parent and child assessments throughout the family trauma intervention. Finally, only three studies assessed participants after the original post-intervention assessment. The Return to the Sacred Path study reported an additional assessment at six-week follow-up (Brave Heart, 1998, 1999a), and the THRIVE and Our Life interventions reported both three-and six-month follow-up assessments (Goodkind et al., 2010, 2012a, 2012b).
Trauma Measures
Studies assessed trauma (historical, interpersonal, or early childhood) through qualitative self-report approaches (n = 5), quantitative questionnaires (n = 4), and, for one study, a newly developed quantitative measure. The Historical Loss Scale and the Historical Loss and Associated Symptoms Scale (HLS/HLASS; Whitbeck, Adams, Hoyt, & Chen, 2004) were used to assess thoughts of historical losses and symptoms of historical trauma. Current traumatic experiences were assessed using the Trauma Symptom Checklist-40 (TSC-40; Elliott & Briere, 1992), the Life Events Scale (LES; Stein, 2004), the Recent Exposure to Violence Scale (REVS; Singer, Anglin, Yu Song, & Lunghofer, 1995), and the Child PTSD Symptoms Scale (CPSS; Foa, Johnson, Feeny, & Treadwell, 2001).
Community Involvement
All studies reported collaboration with Native communities in some capacity to either develop or implement the trauma interventions. Most often, the communities engaged actively in the cultural adaptation of existing interventions or in the development of culturally grounded interventions, generally through having elders, key informants, or community advisory boards review intervention materials and give feedback on their cultural appropriateness. Communities were less involved in the implementation of the interventions, however. Interventions were primarily delivered by trained mental health professionals, and community members were trained to help facilitate group sessions in only six studies.
Study Limitations
The overarching limitations of the intervention research studies in the current review were small sample sizes and non-standardized assessment methods. Other study limitations included lack of meaningful comparison groups and lack of repeated, long-term follow-up assessments.
Discussion
The purpose of this review was to examine current intervention studies targeting historical, interpersonal, and early childhood trauma in Native communities. We identified 15 studies representing 10 interventions used to treat historical (n = 3), interpersonal (n = 3), and early childhood (n = 4) trauma in the United States and Canada. The historical trauma interventions in this review addressed grief associated with historical losses and healing intergenerational trauma through improved parent– child relationships and focused primarily on Native women and children. Of these studies, only the Oyate Ptayela intervention included fathers (Brave Heart, 1999b), while the other historical trauma-informed parenting interventions included mothers as the primary respondents. Similarly, current trauma interventions designed to treat adult interpersonal trauma reported more female than male participants. This finding reflects research conducted with non-Native populations, indicating a systemic issue of trauma interventions including more females than males (Mackenzie, Gekoski, & Knox, 2006).
Interventions conducted with children primarily took place in school systems, which allowed for easier access to youth participants. While those studies utilized a school setting to implement the trauma interventions, they still encountered difficulties in keeping children and parents involved in the treatment process. Without family involvement in early childhood trauma interventions, Native youth reported only short-term abatement of trauma symptoms (Goodkind et al., 2010). This suggests that, without change in the family or home environment, new experiences of victimization could counteract progress made in youth treatment programs. Further evidence for including both parents and children in trauma intervention comes from the THRIVE longitudinal CBITS study conducted with children (Goodkind et al., 2010). While this study reported a reduction of trauma-related symptoms, symptoms returned to pre-intervention levels at later assessment periods. Addressing children’s trauma-related symptoms alone is not likely to be effective if the home environments or parent relationships do not change.
The historical, interpersonal, and early childhood trauma interventions included in this review used both qualitative and quantitative outcome data. Studies reported a general improvement in historical trauma and PTSD-related symptoms, improvements in child-parent relationships, and increased positive coping skills. While the intervention participants reported a general improvement in symptoms related to historical and current trauma, limitations of small sample sizes, lack of meaningful comparison groups, and long-term follow-ups limit the generalizability and internal validity of these findings. It is possible that reported improvements may be better attributed to other factors (e.g., the passage of time, other therapeutic activities that occurred concurrently) than the interventions themselves.
Finally, the interventions in this review used culturally relevant approaches to addressing trauma, with studies reporting both culturally adapted (n = 7) and culturally grounded (n = 3) intervention strategies. Consistent with literature on culturally informed care, most participants reported enjoying the incorporation of traditional elements into trauma treatment. However, some reported that the traditional elements conflicted with their religious beliefs. This conflict was cited as a reason for people leaving intervention programs and not participating in certain intervention components (e.g., Goodkind et al., 2012a, 2012b; Thomas & Bellefeuille, 2006). People with religious-based concerns about culturally relevant interventions may benefit from non-adapted interventions instead, or from those whose adaptations focus on cultural aspects not deemed contradictory to Christian beliefs.
Limitations
This review had several limitations. The small number of trauma intervention studies identified in this review allowed for a discussion of the approaches to trauma intervention research but not an exploration of the efficacy or effectiveness of these interventions. There also were limitations to the search strategy used. While efforts were made to find all published empirical studies of trauma interventions in Native communities, some studies may have been missed in the review process due to the search term limitations. All interventions with Native communities in the United States, Canada, Australia, and New Zealand were eligible for inclusion in this review, but only studies conducted in the United States and Canada were found. This is possibly due to the English language inclusion criterion, and including studies published in non-English languages may have resulted in the identification of additional studies. Also, while we attempted to include an exhaustive list of all Native communities in the United States, Canada, Australia, and New Zealand as search terms, some groups may have been missed in the screening process. A more exhaustive list of Native communities could yield more studies missed in this screening process. Finally, the inclusion criteria of “peer-reviewed empirical articles” could overlook work from Native communities implementing their own trauma intervention research but not publishing the findings in peer-reviewed sources. Expanding the search to find non-published, community-implemented trauma interventions could offer insight into how Native communities may be conducting their own research and shed light on other strategies being used to treat trauma-related symptoms.
Implications and Recommendations
The high rates of trauma in Native communities combined with the small number of intervention programs available presents a serious public health concern. There is an urgent need to expand access to effective trauma interventions and to develop the evidence base surrounding useful ways to treat various sources of trauma. Additionally, communities are calling for mental health interventions that work, and desire the means to collect their own data on interventions that may help their people so they can effect change that facilitates healing (Brave Heart et al., 2011; Gone, 2013; Wendt & Gone, 2012). In this section, we offer recommendations for both intervention content and intervention research strategies.
Intervention Recommendations
While it is essential to address historical loss and its associated symptoms in Native communities, future research should focus on addressing current and historical trauma in tandem. More research is needed to examine how historical loss and associated symptoms impact current trauma experiences and trauma-related outcomes in Native populations. In the United States, AI/AN people have the highest early mortality rates of all ethnic groups (Deters et al., 2006; Whitesell, Beals, Crow, Mitchell, & Novins, 2012), suggesting that, while people are affected by historical loss, they also experience significant loss in their daily lives. This often constant cycle of grief and loss can change people’s support systems and disrupt coping skills learned in trauma interventions. Studies addressing current childhood bereavement and traumatic loss found promising results for improving self-esteem, teaching coping skills, and improving relationships and cohesion with other family members (Haine, Ayers, Sandler, & Wolchik, 2008). Therefore, EBTs that target experiences of current traumatic loss and grief could help bridge the gap between losses experienced in the present and historically.
Of the interpersonal trauma interventions, the Indigenous Healing and Seeking Safety program shows especially promising results. The Indigenous Healing and Seeking Safety intervention was adapted to address historical trauma, interpersonal trauma, and substance abuse concurrently (Marsh, 2016; Marsh et al., 2016). Interventions targeting adult trauma and substance use simultaneously could help target two of the major health disparities in this population. Indigenous Healing and Seeking Safety’s focus on substance use may attract more males who may be willing to seek help for substance use problems but may avoid interventions for interpersonal trauma. Admittedly, women have higher reported rates of victimization in their lifetimes (Rosay, 2016), suggesting that they may have a greater need for interpersonal trauma treatment than their male counterparts. Still, there are many men in Native communities who may benefit from trauma interventions but may not feel free to participate in them if they appear to be primarily for women.
Interventions also are needed to rehabilitate perpetrators in addition to helping victims. One way to decrease health disparities associated with trauma is to identify and develop evidence-based ways to stop the intergenerational transmission of trauma and prevent violence. Targeted interpersonal trauma interventions for both perpetrators and victims could help reduce instances of domestic and child abuse and benefit the family unit as a whole. Additionally, family-based interventions conducted with caregivers and children could help to heal intergenerational trauma and disrupt the cycle of violence in Native communities. Thus, the combination of aspects of historical trauma interventions, parenting programs, and early childhood trauma programs could increase the longevity of symptom reduction with children and improve parent–child relationships.
Research Recommendations
This review included both culturally adapted (n = 7) and culturally grounded (n = 3) trauma interventions with Native communities. Moving forward, researchers should follow the suggestions of Mejia et al. (2017) and use aspects of non-adapted EBTs, culturally adapted EBTs, and culturally grounded interventions to remain flexible and responsive to community needs. Non-adapted EBTs and surface-level adapations can offer a faster approach to addressing the urgent need for trauma treatment in Native communities. Surface-level adaptations, while not as reflective of cultural context, still reflect some cultural values by including aspects of traditional culture such as music and imagery (Resnicow et al., 1999, 2000). These smaller, surface-level changes could be enough to improve the cultural relevance of existing EBTs and increase the acceptability and palatability of an intervention without the time and expense required for deeper adaptations. However, interventions with surface-level adaptations are not as reflective of cultural values and may not be useful for addressing specific culture-bound symptoms such as historical trauma. They also risk strengthening power imbalances inherent in transporting EBTs to Native communities.
Culturally adapted interventions with deep-level changes and culturally grounded interventions are better situated in cultural contexts and are invaluable in creating intervention content to address culture-bound symptoms (e.g., historical trauma) missing from EBTs or symptoms related to cultural trauma that could be worsened by EBTs developed for the dominant culture (Marsiglia & Kulis, 2009; Okamoto, Kuli, et al., 2014; Okamoto, Helm, et al., 2014). Despite the positive aspects of deep-level adaptations and culturally grounded interventions, these interventions may suffer from hardships in securing grant funding and yielding the peer-reviewed publications that are required for grant funding in the current health research environment. Current funding and publication structures emphasize the importance EBTs and randomized control trials (RCTs) in intervention research, meaning interventions more situated in cultural contexts can be overlooked. Researchers should advocate for changes in the funding and peer-review structures to include more representation and acceptance of Indigenous research strategies and ways of knowing. These changes could provide more support for Native and community-based researchers outside of academia implementing their own trauma-informed interventions. Native people understand trauma and healing in their communities, and greater access to funding for Native communities can benefit future trauma intervention development. Culturally grounded interventions are essential for building the evidence base and ensuring that Native communities are receiving effective, culturally relevant care. Outside of these broader changes, researchers can advocate on broadening established approaches to intervention research design and assessment.
The RCT design is considered the “gold standard” for establishing internal validity in intervention research, but we found no RCTs of trauma interventions in this review. This lack of experimental design of intervention studies is considered a major limitation and suggests a need for more rigorous research and program evaluation. However, research suggests that RCTs in Native communities can be viewed as impractical or culturally unacceptable by community participants (Henry, Tolan, Gorman-Smith, & Schoeny, 2017). In these instances, RCTs can be more of a hindrance to testing interventions than a “gold standard.” Henry et al. (2017) suggest that researchers consider using alternatives to RCTs such as regression discontinuity designs, interrupted time series designs, and roll-out designs which are viewed more favorably by Native communities. Additionally, researchers should take steps to explore ways Native communities are currently designing interventions to better understand what is viewed as a culturally acceptable and ethnical research design.
Aside from the concerns over the design methods used to test the interventions, there are also concerns about the representation of Indigenous ways of knowing in the intervention assessment tools. Specifically, the Western scientific approach to evaluating the outcomes of the trauma interventions may overlook culturally specific signs of healing from trauma. One study conducted with a group of African women recovering from sexual assault found that women identified weight gain as a positive sign of recovering from trauma (Duma, Mekwa, & Denny, 2007a, 2007b). This idea of weight gain as a metric of healing may be missed by traditional Western assessment tools and suggests that more work is needed to identify culturally specific metrics of healing from trauma for Indigenous groups. This is especially important for culture-bound symptoms related to historical trauma, but could also prove beneficial for identifying other measurable trauma-related outcomes for use in future intervention research.
Finally, one strategy for making the tools and resources of Western science available to communities and building community trust in research is to use a community-based participatory research (CBPR) framework. The CBPR approach emphasizes equitable partnerships between researchers and communities in which community members are involved in all aspects of the research process (Israel et al., 2005). Additionally, CBPR seeks to build upon existing strengths within the community and effect social change (Castleden, 2008). All interventions in this review involved community participation in some way or another. In the future, interventions designed by Native researchers and using Native facilitators could enhance participation among people who distrust existing EBTs or mental health care services. Efforts to work in partnership with and support Native communities will help create sustainable programs controlled by the community and therefore build trust between community and academic partners. Although communities can and do conduct their own trauma interventions without academic research partners, they may benefit from CBPR partnerships to help them measure outcomes, systematically assess whether the interventions are working as intended, apply for grant funding, and other specialized expertise.
Conclusion
Native communities are at significant risk of experiencing multiple forms of trauma and suffer from health disparities associated with traumatic experiences. However, interventions that address historical, interpersonal, and early childhood trauma with Indigenous people are limited. In this review, 15 published studies were discovered that addressed trauma in Native communities. An increase in trauma intervention research in Native communities over the past 15 years illustrates a growing focus on treating trauma, and, significantly, utilizing community participation. Treating trauma in Native communities will not be accomplished by outside researchers alone; rather, it must honor Native communities’ values and knowledge. Intervention researchers working in partnership with communities to incorporate cultural values and knowledge in the design and assessment of trauma interventions, in conjunction with culturally relevant intervention content and study designs, could help improve the fit, acceptability, and effectiveness of trauma treatment for Native peoples. Changes to trauma intervention research are needed to expand access to effective trauma-informed care and reduce the burden of trauma and related symptoms in Native communities.
Highlights.
Native communities suffer from interpersonal, childhood, and historical trauma experiences.
Although there are effective trauma interventions, few have been tested in Native communities.
A systematic review of the literature yielded only 15 studies representing 10 interventions.
Research studies were limited by small sample sizes and lack of control groups.
Culturally appropriate, evidence-based interventions are needed in Native communities.
Acknowledgments
Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5P20GM104417-02. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors wish to thank Neha John-Henderson, Ben Oosterhoff, and Brandon Scott for their feedback on earlier drafts of this paper.
Footnotes
Conflict of Interest
We have no financial interests in this project, and we have no conflict of interest to declare.
References
References marked with an asterisk indicate studies included in the review.
- *.Ashby MR, Gilchrist LD, & Miramontez A (1988). Group treatment for sexually abused American Indian adolescents. Social Work with Groups, 10, 21–32. [Google Scholar]
- Beals J, Belcourt-Dittloff A, Garroutte EM, Croy C, Jervis LL, Whitesell NR, … & The AI-SUPERPFP Team (2013). Trauma and conditional risk of posttraumatic stress disorder in two American Indian reservation communities. Social Psychiatry and Psychiatric Epidemiology, 48, 895–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Mitchell CM, Novins DK, Simpson S, & Spicer P (2005). Prevalence of major depressive episode in two American Indian reservation populations: Unexpected findings with a structured interview. American Journal of Psychiatry, 162, 1713–1722. [DOI] [PubMed] [Google Scholar]
- Bernal G, Jim enez-Chafey MI, & Domenech Rodr ıguez MM (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40, 361–368. [Google Scholar]
- Bigfoot DS, & Schmidt SR (2010). Honoring children, mending the circle: Cultural adaptation of trauma-focused cognitive-behavioral therapy for American Indian and Alaska Native children. Journal of Clinical Psychology, 66, 847–856. [DOI] [PubMed] [Google Scholar]
- Boden MT, Kimerling R, Jacobs-Lentz J, Bowman D, Weaver C, Carney D, … & Trafton JA (2012). Seeking Safety treatment for male veterans with a substance use disorder and post-traumatic stress disorder symptomatology. Addiction, 107, 578–586. [DOI] [PubMed] [Google Scholar]
- Bombay A, Matheson K, & Anisman H (2011). The impact of stressors on second generation Indian residential school survivors. Transcultural Psychiatry, 48, 367–391. [DOI] [PubMed] [Google Scholar]
- Bombay A, Matheson K, & Anisman H (2014). The intergenerational effects of Indian Residential Schools: Implications for the concept of historical trauma. Transcultural Psychiatry, 51, 320–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd-Ball AJ, Manson SM, Noonan C, & Beals J (2006). Traumatic events and alcohol use disorders among American Indian adolescents and young adults. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 19, 937–947. [DOI] [PubMed] [Google Scholar]
- *.Brave Heart MYH (1998). The return to the sacred path: Healing the historical trauma and historical unresolved grief response among the Lakota through a psychoeducational group intervention. Smith College Studies in Social Work, 68, 287–305. [Google Scholar]
- *.Brave Heart MYHB (1999a). Gender differences in the historical trauma response among the Lakota. Journal of Health and Social Policy, 10, 1–21. [DOI] [PubMed] [Google Scholar]
- *.Brave Heart MYHB (1999b). Oyate Ptayela: Rebuilding the Lakota Nation through addressing historical trauma among Lakota parents. Journal of Human Behavior in the Social Environment, 2, 109–126. [Google Scholar]
- Brave Heart MYH (2003). The historical trauma response among natives and its relationship with substance abuse: A lakota illustration. Journal of Psychoactive Drugs, 35, 7–13. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, Chase J, Elkins J, & Altschul DB (2011). Historical trauma among Indigenous peoples of the Americas: Concepts, research, and clinical considerations. Journal of Psychoactive Drugs, 43, 282–290. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, & DeBruyn LM (1998). The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research, 8, 60–82. [PubMed] [Google Scholar]
- Brave Heart-Jordan M, & DeBruyn L (1995). So she may walk in back. Integrating the impact of historical trauma in the treatment of Native American Women. Racism in Therapy of Women: Testimony, Theory, and Guides to Antiracist Practice, 345–362. [Google Scholar]
- Brockie TN, Dana-Sacco G, Wallen GR, Wilcox HC, & Campbell JC (2015). The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based native American adolescents and young adults. American Journal of Community Psychology, 55, 411–421. [DOI] [PubMed] [Google Scholar]
- Castleden HE (2008). As sacred as cedar and salmon: A collaborative study with Huu-ay-aht First Nation, British Columbia into understanding the meaning of ‘resources’ from an indigenous worldview. ProQuest. [Google Scholar]
- Chorpita BF, & Southam-Gerow MA (2006). Fears and anxieties. Treatment of Childhood Disorders, 3, 271–335. [Google Scholar]
- Cohen JA, Deblinger E, Mannarino AP, & Steer RA (2004). A multisite, randomized controlled trial for children with sexual abuse–related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 393–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ML, Russell M, & George WH (1988). Coping, expectancies, and alcohol abuse: A test of social learning formulations. Journal of Abnormal Psychology, 97, 218–230. [DOI] [PubMed] [Google Scholar]
- Deblinger E, Mannarino AP, Cohen JA, & Steer RA (2006). A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 1474–1484. [DOI] [PubMed] [Google Scholar]
- Deters PB, Novins DK, Novins DK, Fickenscher A, & Beals J (2006). Trauma and posttraumatic stress disorder symptomology: Patterns among American Indian adolescents in substance abuse treatment. American Journal of Orthopsychiatry, 76, 335–345. [DOI] [PubMed] [Google Scholar]
- *.Dionne R, Davis B, Sheeber L, & Madrigal L (2009). Initial evaluation of a cultural approach to implementation of evidence-based parenting interventions in American Indian communities. Journal of Community Psychology, 37, 911–921. [Google Scholar]
- Duma SE, Mekwa JN, & Denny LD (2007a). Women’s journey of recovery from sexual assault trauma: A grounded theory-Part 1. Curationis, 30, 4–11. [PubMed] [Google Scholar]
- Duma SE, Mekwa JN, & Denny LD (2007b). Women’s journey of recovery from sexual assault trauma: A grounded theory-Part 2. Curationis, 30, 12–20. [PubMed] [Google Scholar]
- Duran E, Duran B, Brave Heart MYH, & Yellow Horse-Davis S (1998). Healing the American Indian soul wound In International handbook of multigenerational legacies of trauma (pp (pp. 341–354). Boston: Springer. [Google Scholar]
- Duran B, Oetzel J, Lucero J, Jiang Y, Novins DK, Manson S, & Beals J (2005). Obstacles for rural American Indians seeking alcohol, drug, or mental health treatment. Journal of Consulting and Clinical Psychology, 73, 819–829. [DOI] [PubMed] [Google Scholar]
- Elliott DM, & Briere J (1992). Sexual abuse trauma among professional women: Validating the Trauma Symptom Checklist-40 (TSC-40). Child Abuse and Neglect, 16, 391–398. [DOI] [PubMed] [Google Scholar]
- Elliott DS, & Mihalic S (2004). Issues in disseminating and replicating effective prevention programs. Prevention Science, 5, 47–53. [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T (2008). Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence, 23, 316–338. [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T, Lindhorst T, Huang B, & Walters KL (2006). Interpersonal violence in the lives of urban American Indian and Alaska Native women: Implications for health, mental health, and help-seeking. American Journal of Public Health, 96, 1416–1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Campbell T, Walters KL, Pearson CR, & Campbell CD (2012). Indian boarding school experience, substance use, and mental health among urban two-spirit American Indian/Alaska natives. American Journal of Drug and Alcohol Abuse, 38, 421–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14, 245–258. [DOI] [PubMed] [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, & Treadwell KR (2001). The Child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology, 30, 376–384. [DOI] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. [PubMed] [Google Scholar]
- Fogelman E (1988). Intergenerational group therapy: Child survivors of the holocaust and offspring of survivors. The Psychoanalytic Review, 75, 619–640. [PubMed] [Google Scholar]
- Gendlin E (1996). Focusing-oriented psychotherapy: A manual of the experiential method.
- Gone JP (2010). Psychotherapy and traditional healing for American Indians: Exploring the prospects for therapeutic integration. The Counseling Psychologist, 38, 166–235. [Google Scholar]
- Gone JP (2013). Redressing First Nations historical trauma: Theorizing mechanisms for indigenous culture as mental health treatment. Transcultural Psychiatry, 50, 683–706. [DOI] [PubMed] [Google Scholar]
- Gone JP, & Trimble JE (2011). American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology, 8, 131–160. [DOI] [PubMed] [Google Scholar]
- *.Goodkind J, LaNoue M, Lee C, Freeland L, & Freund R (2012a). Feasibility, acceptability, and initial findings from a community-based cultural mental health intervention for American Indian youth and their families. Journal of Community Psychology, 40, 381–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Goodkind J, LaNoue M, Lee C, Freeland L, & Freund R (2012b). Involving parents in a community-based, culturally grounded mental health intervention for American Indian youth: Parent perspectives, challenges, and results. Journal of Community Psychology, 40, 468–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Goodkind JR, LaNoue MD, & Milford J (2010). Adaptation and implementation of cognitive behavioral intervention for trauma in schools with American Indian youth. Journal of Clinical Child and Adolescent Psychology, 39, 858–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinner D, & Smith TB (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, training, 43, 531–548. [DOI] [PubMed] [Google Scholar]
- Haine RA, Ayers TS, Sandler IN, & Wolchik SA (2008). Evidence-based practices for parentally bereaved children and their families. Professional Psychology: Research and Practice, 39, 113–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Heilbron CL, & Guttman MAJ (2000). Traditional healing methods with first nations women in group counselling. Canadian Journal of Counselling, 34, 3–13. [Google Scholar]
- Henry D, Tolan P, Gorman-Smith D, & Schoeny M (2017). Alternatives to randomized control trial designs for community-based prevention evaluation. Prevention Science, 18, 671–680. [DOI] [PubMed] [Google Scholar]
- *.Hepler KIB (2013). A longitudinal exploration of factors impacting outcomes for Native American students participating in CBITS: looking beyond quantitative analysis (Doctoral dissertation, University of Montana; ). [Google Scholar]
- Horejsi C, Craig BHR, & Pablo J (1992). Reactions by Native American parents to child protection agencies: Cultural and community factors. Child Welfare League of America. [PubMed] [Google Scholar]
- Israel BA, Parker EA, Rowe Z, Salvatore A, Minkler M, L opez J, … & Potito PA (2005). Community-based participatory research: Lessons learned from the Centers for Children’s Environmental Health and Disease Prevention Research. Environmental Health Perspectives, 113, 1463–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs MD (2006). Indian boarding schools in comparative perspective: The removal of Indigenous children in the United States and Australia, 1880–1940 In Trafzer CE, Keller JA & Sisquoc L (Eds.), Boarding school blues: Revisiting American Indian educational experiences. Lincoln, NE: University of Nebraska Press. [Google Scholar]
- Jaycox L (2004). Cognitive Behavioral Intervention for Trauma in Schools (CBITS). Longmont, CO: SoprisWest. [Google Scholar]
- Johnson JL, & Cameron MC (2001). Barriers to providing effective mental health services to American Indians. Mental Health Services Research, 3, 215–223. [DOI] [PubMed] [Google Scholar]
- Keane TM, Marshall AD, & Taft CT (2006). Posttraumatic stress disorder: Etiology, epidemiology, and treatment outcome. Annual Review of Clinical Psychology, 2, 161–197. [DOI] [PubMed] [Google Scholar]
- Kenney MK, & Singh GK (2016). Adverse childhood experiences among American Indian/Alaska Native children: The 2011–2012 national survey of children’s health. Scientifica, 2016, 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestenberg JS (1982). A metapsychological assessment based on an analysis of a survivor’s child In Bergmann MS & Jucovy ME (Eds.), Generations of the Holocaust (pp. 137–158). New York: Columbia University Press. [Google Scholar]
- LaFromboise TD, Albright K, & Harris A (2010). Patterns of hopelessness among American Indian adolescents: Relationships by levels of acculturation and residence. Cultural Diversity and Ethnic Minority Psychology, 16, 68–76. [DOI] [PubMed] [Google Scholar]
- Langley AK, Nadeem E, Kataoka SH, Stein BD, & Jaycox LH (2010). Evidence-based mental health programs in schools: Barriers and facilitators of successful implementation. School Mental Health, 2, 105–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman AF, Ippen CG, & Van Horn P (2006). Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 913–918. [DOI] [PubMed] [Google Scholar]
- Lieberman AF, Van Horn P, & Ippen CG (2005). Toward evidence-based treatment: Child-parent psychotherapy with preschoolers exposed to marital violence. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 1241–1248. [DOI] [PubMed] [Google Scholar]
- Lynch SM, Heath NM, Mathews KC, & Cepeda GJ (2012). Seeking safety: An intervention for trauma-exposed incarcerated women? Journal of Trauma and Dissociation, 13, 88–101. [DOI] [PubMed] [Google Scholar]
- Mackenzie CS, Gekoski WL, & Knox VJ (2006). Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging and Mental Health, 10, 574–582. [DOI] [PubMed] [Google Scholar]
- Manson SM (2000). Mental health services for American Indians and Alaska Natives: Need, use, and barriers to effective care. The Canadian Journal of Psychiatry, 45, 617–626. [DOI] [PubMed] [Google Scholar]
- *.Marsh TN (2016). Exploring how Indigenous healing practices and a western treatment model “seeking safety” can co-exist in assisting Indigenous peoples to heal from trauma and addiction (Doctoral dissertation).
- *.Marsh TN, Cote-Meek S, Young NL, Najavits LM, & Toulouse P (2016). Indigenous Healing and Seeking Safety: A blended implementation project for intergenerational trauma and substance use disorders. International Indigenous Policy Journal, 7, 1–35. [Google Scholar]
- Marsiglia FF, & Kulis S (2009). Diversity, oppression, and change: Culturally grounded social work. Chicago: Lyceum Books. [Google Scholar]
- Mejia A, Leijten P, Lachman JM, & Parra-Cardona JR (2017). Different strokes for different folks? Contrasting approaches to cultural adaptation of parenting interventions. Prevention Science, 18, 630–639. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, & Stevens SP (2006). Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 898–907. [DOI] [PubMed] [Google Scholar]
- Morrisette V, McKenzie B, & Morrisette L (1993). Towards an Aboriginal model of social work practice: Cultural knowledge and traditional practices. Canadian Social Work Review, 10, 91–108. [Google Scholar]
- *.Morsette A, Swaney G, Stolle D, Schuldberg D, van den Pol R, & Young M (2009). Cognitive behavioral intervention for trauma in schools (CBITS): School-based treatment on a rural American Indian reservation. Journal of Behavior Therapy and Experimental Psychiatry, 40, 169–178. [DOI] [PubMed] [Google Scholar]
- *.Morsette A, van den Pol R, Schuldberg D, Swaney G, & Stolle D (2012). Cognitive behavioral treatment for trauma symptoms in American Indian youth: Preliminary findings and issues in evidence-based practice and reservation culture. Advances in School Mental Health Promotion, 5, 51–62. [Google Scholar]
- Nagata DK, & Cheng WJ (2003). Intergenerational Communication of Race-Related Trauma by Japanese American Former Internees. American Journal of Orthopsychiatry, 73, 266–278. [DOI] [PubMed] [Google Scholar]
- Nagata DK, Trierweiler SJ, & Talbot R (1999). Long-term effects of internment during early childhood on third-generation Japanese Americans. American Journal of Orthopsychiatry, 69, 19–29. [DOI] [PubMed] [Google Scholar]
- Najavits LM (2004). Treatment of posttraumatic stress disorder and substance abuse: Clinical guidelines for implementing Seeking Safety therapy. Alcoholism Treatment Quarterly, 22, 43–62. [Google Scholar]
- Najavits LM, Ryngala D, Back SE, Bolton E, Mueser KT, & Brady KT (2009). Treatment of PTSD and comorbid disorders In Foa EB, Keane TM, Friedman MJ & Cohen JA (Eds.), Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies (pp. 508–535). New York: Guilford Press. [Google Scholar]
- Ngo V, Langley A, Kataoka SH, Nadeem E, Escudero P, & Stein BD (2008). Providing evidence-based practice to ethnically diverse youths: Examples from the Cognitive Behavioral Intervention for Trauma in Schools (CBITS) program. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 858–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donohue W, & Benuto L (2010). The many problems of cultural sensitivity. Scientific Review of Mental Health Practice, 7, 34–37. [Google Scholar]
- Oetzel J, & Duran B (2004). Intimate partner violence in American Indian and/or Alaska Native communities: A social ecological framework of determinants and interventions. American Indian and Alaska Native Mental Health Research, 11, 49–69. [DOI] [PubMed] [Google Scholar]
- Oetzel J, Duran B, Lucero J, Jiang Y, Novins DK, Manson S, & Beals J (2006). Rural American Indians’ perspectives of obstacles in the mental health treatment process in three treatment sectors. Psychological Services, 3, 819–829. [Google Scholar]
- Okamoto SK, Helm S, Pel S, McClain LL, Hill AP, & Hayashida JK (2014). Developing empirically based, culturally grounded drug prevention interventions for indigenous youth populations. The journal of Behavioral Health Services and Research, 41, 8–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto SK, Kulis S, Marsiglia FF, Steiker LKH, & Dustman P (2014). A continuum of approaches toward developing culturally focused prevention interventions: From adaptation to grounding. The Journal of Primary Prevention, 35, 103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oral R, Ramirez M, Coohey C, Nakada S, Walz A, Kuntz A, … & Peek-Asa C (2016). Adverse childhood experiences and trauma informed care: The future of health care. Pediatric Research, 79, 227–234. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, & Braithwaite RL (1999). Cultural sensitivity in public health: Defined and demystified. Ethnicity and Disease, 9, 10–21. [PubMed] [Google Scholar]
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, & Butler J (2000). Cultural sensitivity in substance use prevention. Journal of Community Psychology, 28, 271–290. [Google Scholar]
- Ringel JS, & Sturm R (2001). National estimates of mental health utilization and expenditures for children in 1998. The Journal of Behavioral Health Services and Research, 28, 319–333. [DOI] [PubMed] [Google Scholar]
- Rosay AB (2016). Violence against American Indian and Alaska native women and men. National Institute of Justice, 277. Available from: https://nij.gov/journals/277/Pages/violence-against-american-indians-alaska-natives.aspx [last accessed September 19 2018].
- Rowland-Klein D, & Dunlop R (1998). The transmission of trauma across generations: Identification with parental trauma in children of Holocaust survivors. Australian and New Zealand Journal of Psychiatry, 32, 358–369. [DOI] [PubMed] [Google Scholar]
- Royal Commission on Aboriginal Peoples (RCAP) (1996). Looking forward, looking back: Report of the Royal Commission on Aboriginal Peoples, vol 1. Ottawa, ON: Communication Group. [Google Scholar]
- Shapiro F (2001). Eye movement desensitization and reprocessing (EMDR): Basic principles, protocols, and procedures. Guilford Press. [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, & Amaya-Jackson L (2008). Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 37, 156–183. [DOI] [PubMed] [Google Scholar]
- Singer MI, Anglin TM, Yu Song L, & Lunghofer L (1995). Adolescents’ exposure to violence and associated symptoms of psychological trauma. JAMA, 273, 477–482. [PubMed] [Google Scholar]
- Stein B (2004). Revised child screening instruments. Unpublished report.
- Substance Abuse and Mental Health Services Administration (2017). Results from the 2016 national survey on drug use and health: Detailed tables. Available from: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.pdf [last accessed January 12 2019].
- Sue DW, & Sue D (2003). Counseling the culturally different (4th edn). New York: Wiley. [Google Scholar]
- *.Thomas W, & Bellefeuille G (2006). An evidence-based formative evaluation of a cross cultural Aboriginal mental health program in Canada. Australian e-journal for the Advancement of Mental Health, 5, 202–215. [Google Scholar]
- Trimble JE, & Fisher CB (Eds.) (2006). The handbook of ethical research with ethnocultural populations and communities. California: Sage. [Google Scholar]
- Trusz SG, Wagner AW, Russo J, Love J, & Zatzick DF (2011). Assessing barriers to care and readiness for cognitive behavioral therapy in early acute care PTSD interventions. Psychiatry: Interpersonal and Biological Processes, 74, 207–223. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2001). Administration on Children, Youth and Families. Child Maltreatment: 1999 Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Walls ML, & Whitbeck LB (2012). The intergenerational effects of relocation policies on Indigenous families. Journal of Family Issues, 33, 1272–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Evans-Campbell T, Simoni JM, Ronquillo T, & Bhuyan R (2006). “My Spirit in My Heart” identity experiences and challenges among American Indian two-spirit women. Journal of Lesbian Studies, 10, 125–149. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C (2007). The Incredible Years parent training manual: BASIC program. Seattle, WA: Umbrella. [Google Scholar]
- Weissbecker I, & Clark C (2007). The impact of violence and abuse on women’s physical health: Can trauma-informed treatment make a difference? Journal of Community Psychology, 35, 909–923. [Google Scholar]
- Wendt DC, & Gone JP (2012). Rethinking cultural competence: Insights from indigenous community treatment settings. Transcultural Psychiatry, 49, 206–222. [DOI] [PubMed] [Google Scholar]
- Wesley-Esquimaux CC, & Smolewski M (2004). Historic trauma and Aboriginal healing (p. 3). Ottawa, ON: Aboriginal Healing Foundation. [Google Scholar]
- Wexler L, Silveira ML, & Bertone-Johnson E (2012). Factors associated with Alaska Native fatal and nonfatal suicidal behaviors 2001–2009: trends and implications for prevention. Archives of Suicide Research, 16, 273–286. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Adams GW, Hoyt DR, & Chen X (2004). Conceptualizing and measuring historical trauma among American Indian people. American Journal of Community Psychology, 33, 119–130. [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Chen X, Hoyt DR, & Adams GW (2004). Discrimination, historical loss and enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American Indians. Journal of Studies on Alcohol, 65, 409–418. [DOI] [PubMed] [Google Scholar]
- Whitesell NR, Beals J, Crow CB, Mitchell CM, & Novins DK (2012). Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38, 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolsko C, Lardon C, Mohatt GV, & Orr E (2007). Stress, coping, and well-being among the Yupik of the Yukon-Kuskokwim Delta: The role of enculturation and acculturation. International Journal of Circumpolar Health, 66, 51–61. [DOI] [PubMed] [Google Scholar]
- Yuan NP, Koss MP, Polacca M, & Goldman D (2006). Risk factors for physical assault and rape among six Native American tribes. Journal of Interpersonal Violence, 21, 1566–1591. [DOI] [PubMed] [Google Scholar]


