Abstract
Standards targeting children’s healthy eating and physical activity (HEPA) in after-school programs call for staff to display or refrain from HEPA-promoting or -discouraging behaviors that are linked to children’s HEPA. This study evaluated strategies to align staff behaviors with HEPA Standards. Staff at four afterschool programs serving approximately 500 children participated in professional development training from January 2012 to May 2013. Site leaders also attended workshops and received technical support during the same time frame. Changes in staff behaviors were evaluated using the System for Observing Staff Promotion of Activity and Nutrition in a pre- (fall 2011) multiple-post (spring 2012, fall 2012, and spring 2013), no–control group study design. A total of 8,949 scans were completed across the four measurement periods. Of the 19 behaviors measured, 14 changed in the appropriate direction. For example, staff engaging in physical activity with children increased from 27% to 40% of scans and staff eating unhealthy foods decreased from 56% to 14% of days. Ongoing training and technical assistance can have a measureable impact on staff behaviors linked to child-level HEPA outcomes. Future research should explore the feasibility of disseminating ongoing trainings to after-school program staff on a large scale.
Keywords: intervention, obesity, out-of-school time, children
INTRODUCTION
National and state organizations have developed Healthy Eating and Physical Activity (HEPA) standards for after-school programs (Beets, Tilley, Kim, & Webster, 2011; Beets, Wallner, & Beighle, 2010) because of their potential to promote the HEPA of children in their care (Beets, Huberty, & Beighle, 2012; Beighle et al., 2010). These standards are designed to increase the nutritional quality of snacks served and the amount of physical activity children accumulate while attending (Beets, 2012b; Beets et al., 2011; Beets, Wallner, et al., 2010; Missouri Afterschool Network, 2006; Wiecha, Gannett, Hall, & Roth, 2011).
In November 2011, the YMCA of the USA, one of the largest after-school program providers in the country, adopted HEPA Standards for all of their after-school programs (Wiecha et al., 2011). These Standards call on frontline staff (i.e., those individuals interacting with children daily—hereafter referred to as “staff”) to create HEPA-friendly after-school program environments by exhibiting key behaviors that are empirically, theoretically, and intuitively linked to increasing children’s HEPA. Staff behaviors outlined in the Standards include staff verbal promotion of HEPA, staff modeling HEPA behaviors (e.g., eating with children, playing with children), and staff refraining from prescribing or withholding physical activity as punishment. What these standards lack are strategies for increasing the staff behaviors targeted in HEPA Standards, leaving program leaders with no guidance on how to bridge the gap between recommended best practice and routine practice in their programs.
Recognizing this gap, one YMCA organization in Columbia, South Carolina, entered into a 2-year partnership with the University of South Carolina to identify strategies for meeting the YMCA of the USA HEPA Standards in their after-school programs. First-year findings from this partnership were promising. Of the 20 staff behaviors targeted, 17 increased or decreased in the appropriate direction. Furthermore, these impacts on staff behaviors occurred in as little as 3 months (Weaver, Beets, Saunders, Beighle, & Webster, 2014). However, there is little evidence for what intervention strategies align staff behaviors with HEPA Standards in the afterschool program setting. Only one other study has examined a professional development training’s impact on staff behaviors related to HEPA Standards (Weaver, Beets, Saunders, & Beighle, 2014). Furthermore, it is unknown if these changes will be sustainable over time.
Developing strategies that successfully align staff behaviors with HEPA Standards is a crucial first step to addressing the gap between policy and practice in after-school programs (Beets, 2012a; Beets, Webster, Saunders, & Huberty, 2013; Weaver, Beets, Webster, Beighle, & Huberty, 2012). The purpose of this pilot study is to describe changes in after-school program staff’s HEPA-promoting and -discouraging behaviors after a 2-year competency-based professional development training program.
METHOD
Design
This article presents the evaluation of a 2-year intervention using a single-group repeated cross-sectional design (i.e., pretest—fall 2011, and three follow-up measures—spring 2012, fall 2012, and spring 2013). A time line of the intervention and key events is presented in Table 1.
TABLE 1.
Timeline of Key Intervention Events and Site Leader Turnover
| Time/Date | Key Event | Site Leader Turnover |
|---|---|---|
| Fall 2011 (Baseline) | • Collaborative group meetings | Site 1: A |
| • Baseline measurement | Site 2: A | |
| Site 3: A | ||
| Site 4: A | ||
| Spring 2012 (Measurement 1) | • Delivery of HEPA strategies training (January 2012) | Site 1: A |
| • Implementation of HEPA strategies | Site 2: A | |
| Site 3: A, B, C | ||
| Site 4: A | ||
| Fall 2012 (Measurement 2) | • Delivery of HEPA strategies training (August 2012) | Site 1: A, B |
| • Implementation of HEPA strategies | Site 2: A, B | |
| Site 3: A, B, C | ||
| Site 4: A, B | ||
| Spring 2013 (Measurement 3) | • Delivery of HEPA strategies training (January 2013) | Site 1: A, B |
| • Implementation of HEPA strategies | Site 2: A, B, C | |
| Site 3: A, B, C, D, E, F | ||
| Site 4: A, B, C, D, E |
NOTE: HEPA = Healthy Eating and Physical Activity. Each letter, A-F, represents an individual site leader. For instance, at Measurement 1, Site 3 was on their third site leader as indicated by Site 3: A, B, C. At Measurement 3, Site 3 was on their sixth site leader as indicated by Site 3: A, B, C, D, E, F.
First-year findings have been reported elsewhere (Weaver, Beets, Saunders, Beighle, & Webster, 2014) and can be found in Figures 1 and 2. The methods reported herein closely reflect the methods of the firstyear outcomes paper given the continuation from Year 1 of the study and are provided in brief below. All protocols were approved by the university’s institutional review board prior to the start of the study.
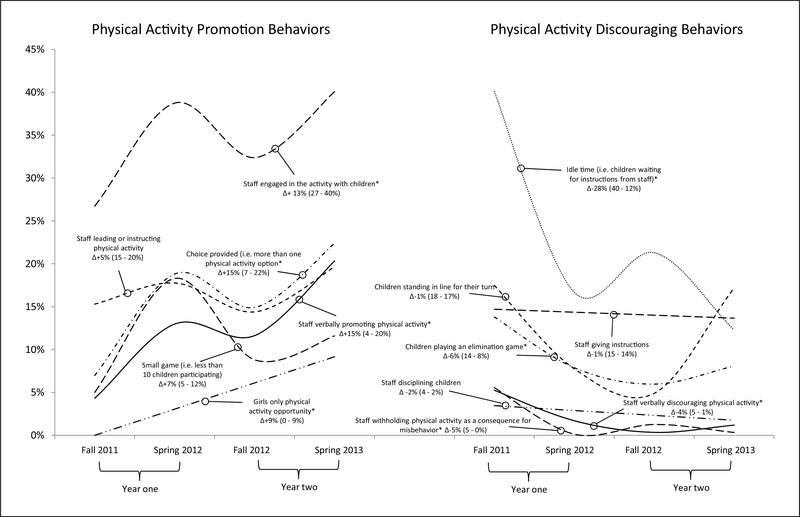
FIgure 1. Change in Staff Physical Activity Promotion Behaviors From Baseline to Postassessment.
NOTE: Based on 4842 SOSPAN (System for Observing Staff Promotion of Activity and Nutrition) scans over 87 program days. Percentages are based on the regression models and represent the percentage of scans a behavior was observed during scheduled physical activity time.
*Indicates statistically significant changes at p < .05.
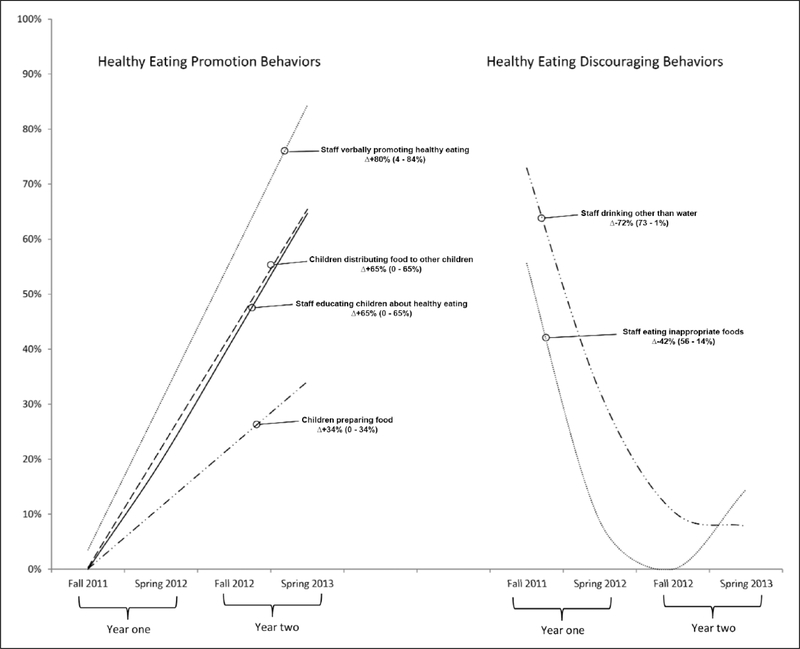
FIgure 2. Change in Staff Healthy Eating Promotion Behaviors From Baseline to Postassessment.
NOTE: Based on 87 program days. Percentages are based on the regression models and represent the percentage of days a behavior was observed. All estimates represent statistically significant changes at p < .05.
Sample
Participant after-school programs were preexisting programs located at a local YMCA, were available daily throughout the academic year (Monday through Friday), took place immediately following the regular school day between 3 and 6 p.m., and provided a combination of scheduled activities, including snacks, homework assistance/tutoring, enrichment activities (e.g., arts and crafts, music), and opportunities for children to be physically active. Approximately 500 children attended the four sites daily across the 2-year study.
Sites were structured to include a site leader and staff. Site leaders were responsible for staffing the program, planning daily activities, budgeting, and so on. Staff were responsible for delivering the program to children. All site leaders and staff at the after-school programs participated in the intervention. There were four site leaders (i.e., one per site) and approximately 50 staff across the four after-school program sites at each measurement period.
Intervention
Identification of Strategies to Meet HEPA Standards
The conceptual framework of the intervention has been described in detail elsewhere (Beets et al., 2014; Beets, Webster, et al., 2013) and is based on the principles of community-based participatory research (Israel et al., 2010), complex systems change (FosterFishman, Nowell, & Yang, 2007), and social ecological models of health promotion (Sallis & Owen, 2002). Using these frameworks, university and after-school program staff created a collaborative work group to review the YMCA of the USA’s HEPA Standards (Beets et al., 2011; Beets, Wallner, et al., 2010) and identify strategies flexible enough to achieve HEPA Standards while still meeting the unique challenges of each afterschool program site.
Using the social ecological model as a frame, the collaborative workgroup identified four levels of influence on children’s HEPA (i.e., staff, site leader, parent, and environment of the after-school program) targeted by the Standards. Strategies created by the collaborative workgroup targeted all levels. This article presents the strategies that target the staff level of the social ecological model exclusively. Consistent with a systems framework (Foster-Fishman et al., 2007) and the social ecological model (Sallis & Owen, 2002) approach, it was theorized that the most modifiable lever for change in after-school programs was staff skills and competencies. The collaborative work group believed that staff could be trained to create a HEPA-friendly environment, and this would, in turn, affect children’s HEPA while in the program. Specifically, strategies selected by the collaborative work group to align staff behaviors with HEPA Standards targeted appropriate and inappropriate behaviors of staff (e.g., staff prepare an activity plan and model HEPA). These strategies were chosen because they were low- to no-cost, since the association was already delivering professional development training to staff into which HEPA trainings could be incorporated.
Professional Development Training
The primary strategy for increasing staff HEPA-promoting behaviors was professional development training consisting of a 2-hour healthy eating training and a 3-hour physical activity training. Trainings were integrated into existing professional development trainings delivered twice yearly at the YMCA (beginning of school year— August; and mid-school year—January). All staff were required to attend along with their site leaders. The professional development training was founded on the 5Ms—Mission, Manage, Motivate, Monitor, and Maximize (Weaver et al., 2012)—training model and was designed to develop after-school program staff competencies related to increasing child engagement in HEPA. Competencies included in the trainings are consistent with policy documents (Beets et al., 2011; Beets, Rooney, Tilley, Beighle, & Webster, 2010; Wiecha et al., 2011; Zarrett, Skiles, Wilson, & McClintock, 2012), “best practices” position statements from physical education (American Academy of Pediatrics, 2012; National Association of Sport and Physical Education, 2009), literature on competencies for schoolwide and after-school physical activity promotion (Beighle et al., 2010; Kelder et al., 2005; Missouri Afterschool Network, 2006; North Carolina Afterschool Professional Development Work Group, 2010), and theory on physical activity promotion (Deci & Ryan, 1987; Stuntz & Weiss, 2010).
All trainings were led by university personnel with expertise in HEPA promotion. During trainings, staff participated in and led healthy eating exercises and physical activities in the five domains of the training program. Competencies included in the healthy eating training were role modeling healthy eating, promoting healthy eating, and promoting safe food handling. The physical activity component of the professional development training used the LET US Play (i.e., lines, elimination, team size, uninvolved staff/kids, and space, equipment, and rules) principles. The LET US Play principles were introduced to staff in order to provide a reflective tool for the identification of barriers that limit children’s activity during free-play and organized-activity opportunities. Staff also practiced competencies related to managing children in physical activity environments (e.g., using countdowns to transition between activities quickly, actively supervising children, and keeping all children in view) in order to reduce instruction, maintain discipline, and reduce idle time.
Booster Training Sessions
A total of nine booster sessions (three each in spring 2012, fall 2012, spring 2013) in each after-school program site were conducted. Booster sessions consisted of a walk-through observation with the site leader over one complete program day (i.e., ~3–6 p.m.). During these observations, staff and site leaders received real-time feedback and modeling of HEPA promotion strategies from an expert in HEPA promotion. Observation notes were compiled, along with suggestions for program enhancement, and were e-mailed to site leaders and branch directors for dissemination to staff. Observations and suggestions were aligned with competencies presented to staff in the 5Ms professional development training and focused on modifying games to enhance child physical activity levels based on the LET US Play principles, managing physical activity environments effectively, as well as modeling and encouraging child HEPA.
Technical Support and Feedback
Weekly contact with site leaders was provided by a HEPA expert via phone or face-to-face conversations. These contacts were designed to provide ongoing technical support regarding each after-school program site’s progress toward meeting the HEPA Standards. Conversations centered on barriers to implementation of strategies to meet HEPA Standards and solutions for overcoming identified barriers.
Measures
Staff incorporation of HEPA promotion behaviors into routine practice was measured via direct observation using the System for Observing Staff Promotion of Activity and Nutrition (SOSPAN). The instrument was designed to measure staff behaviors related to HEPA promotion using momentary time sampling (Weaver, Beets, Webster, & Huberty, 2014). Behaviors included in SOSPAN and reported in this study are described in Table 2. As described in detail elsewhere (Weaver, Beets, Webster, et al., 2014), SOSPAN captures 19 staff behaviors (13 physical activity behaviors and 6 healthy eating behaviors) that either promote (e.g., verbal promotion, modeling HEPA) or discourage (e.g., verbal discouragement of physical activity, staff eating inappropriate foods) HEPA. The instrument is divided into three subsections, including staff management behaviors, staff promotion behaviors, and context of the after-school program. Staff management behaviors (n = 9) consist of contextual factors of the activity (e.g., children eliminated from physical activity opportunities, children stand and wait in line for turn, children preparing food) occurring, over which staff have direct control. Staff promotion behaviors (n = 9) include actions that staff perform (e.g., staff engaging in physical activity with children, verbally promoting HEPA, educating children about healthy eating). The context of the after-school program (i.e., scheduled physical activity, snack, enrichment, and academics) in which staff behaviors occur is also recorded by the SOSPAN instrument. SOSPAN has been found reliable and valid (Weaver, Beets, Webster, et al., 2014).
TABLE 2.
SOSPAN Instrument Sequence of Scans and Variables collected
| Scan | Variable |
|---|---|
| SOSPAN physical activity promotion scana | |
| Activity context | Scheduled activity |
| Grade level of children | |
| Location of activity | |
| Equipment available | |
| Staff promotion behaviors | Staff leading or instructing physical activity |
| Staff verbally promoting physical activity | |
| Staff engaged in physical activity with children (i.e., playing the games) | |
| Choice provided (i.e., more than one activity opportunity provided) | |
| Small game (i.e., games with less than 10 children participating) | |
| Girls-only physical activity opportunity | |
| Staff discouraging behaviors | Staff giving instructions |
| Staff disciplining children | |
| Idle time (i.e., children waiting for direction from staff with no specific task) | |
| Children standing in line and waiting for turn | |
| Playing elimination game (i.e., children eliminated from physical activity opportunities) | |
| Staff verbally discouraging physical activity | |
| Withholding physical activity as a consequence of misbehavior | |
| SOSPAN nutrition promotion scanb | |
| Staff promotion behaviors | Staff verbally promoting healthy eating |
| Staff verbally educating children about healthy eating | |
| Children preparing food | |
| Children distributing food to other children | |
| Staff discouraging behaviors | Staff eating inappropriate foods |
| Staff drinking other than water |
NOTE: SOSPAN = System for Observing Staff Promotion of Activity and Nutrition.
Scans completed during all scheduled activities.
Scans completed during scheduled snack or lunch only.
Observation occurred on four unannounced nonconsecutive weekdays (Monday-Thursday) during each measurement period. Observing after-school programs over multiple unannounced nonconsecutive days provides a representative sample of a typical program day (Beets et al., 2014; Coleman, Geller, Rosenkranz, & Dzewaltowski, 2008). A schedule of the daily activities was collected at the beginning of each observation day. SOSPAN scans were completed continuously one after another from the beginning to the end of the program (~3–6 p.m.). Prior to observation, each site was visited to determine available spaces in which program activities could occur. These spaces are referred to as “target areas” (Weaver, Beets, Webster, et al., 2014).
Observer Training and SOSPAN Reliability
Observer training was conducted prior to each assessment. Observers completed classroom training and field practice. Interrater agreement criteria were set at >80% using interval-by-interval agreement for each category (McKenzie, Marshall, Sallis, & Conway, 2000; Ridgers, Stratton, & McKenzie, 2010). Consistent with published reliability protocols (Brown et al., 2006; Ridgers et al., 2010), reliability was collected on at least 30% of measurement days. Reliability for SOSPAN was collected over 58 of the 87 measurement days (i.e., 66.7%). Estimates are based on 1,313 reliability scans across the four measurement periods. Percentage agreement between observers for staff behaviors ranged from 84.5% to 99.8%.
Data Analysis
All statistical analyses were conducted using Stata (Version12.0., College Station, TX). Changes in staff behaviors over time were estimated using multilevel random effects models accounting for the clustering of observer scans within days within sites. Staff physical activity promotion behaviors were expressed as a percentage of scans observed during scheduled physical activity since that is when Standards call for staff to display these behaviors. All staff healthy eating promotion behaviors were converted into the percentage of days the behavior was observed since HEPA Standards call for these behaviors to be displayed each day (i.e., children should prepare and distribute food at the beginning of snack) or call for a staff behavior to be displayed weekly (i.e., staff should deliver nutrition education weekly). Where appropriate, both linear and nonlinear terms (e.g., square) were included in the models to account for the nonlinear change in staff behaviors over time.
RESULTS
A total of 8,949 SOSPAN scans were completed across the four measurement periods, with 4,842 scans occurring during scheduled physical activity. Model estimates of the changes in staff behaviors over time are presented in Figures 1 and 2. All of the 19 behaviors recorded in this study moved in the desired direction, with 14 behaviors demonstrating statistically significant changes from baseline (i.e., fall 2011) to final assessment (i.e., spring 2013). Eight of the 13 changes in staff physical activity–promoting and –discouraging behaviors reached statistical significance. Changes in staff physical activity promotion behaviors ranged from a 7% increase in staff organizing small games (5% vs. 12%) to a 16% increase in staff verbally promoting physical activity (4% vs. 20%). Changes in staff physical activity discouraging behaviors ranged from a 1% decrease in both children standing in line for their turn (18% vs.17%) and staff giving instructions (15% vs. 14%) to a 28% decrease in idle time (40% vs.12%).
All changes in the percentage of days a healthy eating behavior was observed over time reached statistical significance. Changes in healthy eating promotion behaviors ranged from a 34% increase in the percentage of days children prepared food (0% vs. 34%) to an 80% increase in the percentage of days staff verbally promoted healthy eating (4% vs. 84%). Reductions in the percentage of days staff modeled unhealthy eating and drinking were 42% and 72%, respectively.
DISCUSSION
This study is among the first to evaluate strategies to align staff behaviors with those called for in HEPA Standards. By the end of the 2-year intervention, 14 of the 19 targeted staff behaviors had changed in the desired direction. The findings in this study indicate that competency-based professional development training, feedback, and technical assistance can align staff behaviors with those called for in HEPA Standards.
The study described herein focused on the staff’s role in creating an after-school program environment to promote HEPA by displaying certain behaviors called for in HEPA Standards. Staff were provided training targeting these behaviors to enable them to create this environment. This is an important distinction between this study and previous studies that relied on prepackaged curricula for increasing children’s HEPA (Dzewaltowski et al., 2010; Iversen, Nigg, & Titchenal, 2011; Nigg, Battista, Chang, Yamashita, & Chung, 2004; Sharpe, Forrester, & Mandigo, 2011). As HEPA Standards are calling for staff to create a HEPA-friendly environment, it is important to develop effective strategies for providing staff with the skills to do so.
We are aware of one other study that has intervened on staff behaviors and evaluated subsequent changes (Weaver, Beets, Saunders, & Beighle, 2014). This study and the study reported herein provide initial evidence that routine practice can be amended to create a HEPA-friendly environment for children through professional development training coupled with feedback and technical support. Since HEPA Standards call for staff to display or refrain from certain HEPA-promoting or -discouraging behaviors, and staff behaviors are linked to children’s HEPA (Huberty, Beets, Beighle, & McKenzie, 2012; Weaver, Beets, Webster, et al., 2014), identifying effective strategies for modifying staff behaviors is an essential first step to creating the desired changes in children’s HEPA in after-school programs.
An important finding of this study is that staff demonstration of the behaviors called for in HEPA Standards fluctuated over time. One possible explanation is the substantial turnover at the frontline staff (50% to 70% retention) and site leader levels (16 site leaders in 2 years; see Table 1). However, staff implementation of HEPA-promoting behaviors was consistently higher than baseline levels, while staff demonstration of HEPA-discouraging behaviors was consistently lower than at baseline. These findings indicate that in the face of substantial turnover at multiple levels, the strategies adopted herein can enhance the HEPA environment of after-school programs. These findings also highlight the need for ongoing professional development training, feedback, and technical support. Site leaders and university personnel should seek collaborative partnerships like the one described in this study to deliver these strategies to staff. Furthermore, HEPA trainings should be incorporated into preexisting frontline staff trainings when possible to mitigate the cost of trainings.
This study’s strengths include the use of a valid and reliable systematic observation instrument (i.e., SOSPAN), the quantity of SOSPAN scans collected (i.e., 8,949) over multiple evaluation periods, and the collaborative partnership between the YMCA afterschool programs and university personnel. The SOSPAN instrument and the quantity of scans over multiple time periods provide an accurate representation of the staff behaviors occurring within these afterschool programs. The collaborative partnership between the YMCA after-school programs and university personnel led to the use of strategies that were practical, making them more easily adopted by the participant sites (Beets, Webster, et al., 2013). Limitations of this study include lack of a control group and the limited number of after-school program sites (n = 4). The small number of program sites limits the generalizability of the findings presented herein. Additional large-scale studies employing a more rigorous research design (i.e., randomized controlled trials) to determine the scalability of these strategies to multiple sites in multiple different settings are needed. The lack of a control group makes it impossible to determine if the observed changes would have occurred without the presence of the strategies presented herein. These changes could have occurred due to history, selection bias, the “Hawthorne effect,” or regression to the mean. Finally, 19 different models were estimated to test the changes in staff behaviors over time. When many statistical tests are run, the possibility of finding a statistically significant result by chance increases (Zaykin, Zhivotovsky, Westfall, & Weir, 2002). However, it is unlikely that 14 of the 19 targeted behaviors would have changed due to chance, suggesting that changes were due to the intervention (i.e., training, feedback, and technical support). Further changes in staff behaviors were accompanied by increases in children’s HEPA, suggesting that these changes were real and meaningful (Beets et al., 2014; Beets, Tilley, et al., 2013).
In conclusion, this study demonstrates that ongoing professional development training, feedback, and technical support can produce substantial changes in staff incorporation of HEPA-promoting and in elimination of HEPA-discouraging behaviors, despite turnover at the site leader and frontline staff levels. Future studies should evaluate the effectiveness and feasibility of these strategies on a larger scale with a more rigorous research design.
Acknowledgments
Authors’ Note: The project described was supported by Award No. R21HL106020 from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The authors have no potential conflicts of interest to disclose.
REFERENCES
- American Academy of Pediatrics. (2012). Preventing childhood obesity in early care and education (2nd ed.) Selected standards from caring for our children: National Health and Safety Performance Standards; Guidelines for Early Care and Education Programs, 3rd edition. Retrieved from http://cfoc.nrckids.org/WebFiles/PreventingChildhoodObesity2nd.pdf [Google Scholar]
- Beets MW (2012a). Enhancing the translation of physical activity interventions in afterschool programs. American Journal of Lifestyle Medicine, 6, 328–341. doi: 10.1177/1559827611433547 [DOI] [Google Scholar]
- Beets MW (2012b). Policies and standards for promoting physical activity in after-school programs (Research Brief). Retrieved from http://activelivingresearch.org/policies-andstandards-promoting-physical-activity-after-school-programs
- Beets MW, Huberty J, & Beighle A (2012). Physical activity of children attending afterschool programs: Research- and practicebased implications. American Journal of Preventive Medicine, 42, 180–184. [DOI] [PubMed] [Google Scholar]
- Beets MW, Rooney L, Tilley F, Beighle A, & Webster C (2010). Evaluation of policies to promote physical activity in afterschool programs: Are we meeting current benchmarks? Preventive Medicine, 51, 299–301. doi: 10.1016/j.ypmed.2010.07.006 [DOI] [PubMed] [Google Scholar]
- Beets MW, Tilley F, Kim Y, & Webster C (2011). Nutritional policies and standards for snacks served in afterschool programmes: A review. Public Health Nutrition, 14, 1882–1890. [DOI] [PubMed] [Google Scholar]
- Beets MW, Tilley F, Weaver RG, Turner-McGrievy G, Moore JB, & Webster C (2013). From policy to practice: Addressing snack quality, consumption, and price in after-school programs. Journal of Nutrition Education and Behavior, 46, 384–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Wallner M, & Beighle A (2010). Defining standards and policies for promoting physical activity in afterschool programs. Journal of School Health, 80, 411–417. doi: 10.1111/j.1746-1561.2010.00521.x [DOI] [PubMed] [Google Scholar]
- Beets MW, Weaver RG, Moore JB, Turner-McGrievy G, Pate RR, Webster C, & Beighle A (2014). From policy to practice: Strategies to meet physical activity standards in YMCA afterschool programs. American Journal of Preventive Medicine, 46, 281–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beets MW, Webster C, Saunders R, & Huberty JL (2013). Translating policies into practice: A framework for addressing childhood obesity in afterschool programs. Health Promotion Practice, 14, 228–237. doi: 10.1177/1524839912446320 [DOI] [PubMed] [Google Scholar]
- Beighle A, Beets MW, Erwin HE, Huberty J, Moore JB, & Stellino M (2010). Promoting physical activity in afterschool programs. Afterschool Matters, 11, 24–32. [Google Scholar]
- Brown WH, Pfeiffer KA, McIver KL, Dowda M, Almeida MJ, & Pate RR (2006). Assessing preschool children’s physical activity: The observational system for recording physical activity in children-preschool version. Research Quarterly for Exercise and Sport, 77, 167–176. [DOI] [PubMed] [Google Scholar]
- Coleman KJ, Geller KS, Rosenkranz RR, & Dzewaltowski DA (2008). Physical activity and healthy eating in the afterschool environment. Journal of School Health, 78, 633–640. doi: 10.1111/j.1746-1561.2008.00359.x [DOI] [PubMed] [Google Scholar]
- Deci EL, & Ryan RM (1987). The support of autonomy and the control of behavior. Journal of Personality and Social Psychology, 53, 1024–1037. [DOI] [PubMed] [Google Scholar]
- Dzewaltowski DA, Rosenkranz RR, Geller KS, Coleman KJ, Welk GJ, Hastmann TJ, & Milliken GA (2010). HOP’N after-school project: An obesity prevention randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 7(1), 90. doi: 10.1186/1479-5868-7-90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster-Fishman PG, Nowell B, & Yang H (2007). Putting the system back into systems change: A framework for understanding and changing organizational and community systems. American Journal of Community Psychology, 39, 197–215. doi: 10.1007/s10464-007-9109-0 [DOI] [PubMed] [Google Scholar]
- Huberty JL, Beets MW, Beighle A, & McKenzie T (2012). Association of staff behaviors and afterschool program features to physical activity: Findings from movin’ afterschool. Journal of Physical Activity & Health, 10, 423–429. [DOI] [PubMed] [Google Scholar]
- Israel BA, Coombe CM, Cheezum RR, Schulz AJ, McGranaghan RJ, Lichtenstein R, … Burris A (2010). Community-based participatory research: A capacity-building approach for policy advocacy aimed at eliminating health disparities. American Journal of Public Health, 100, 2094–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iversen CSS, Nigg C, & Titchenal CA (2011). The impact of an elementary after-school nutrition and physical activity program on children’s fruit and vegetable intake, physical activity, and body mass index: Fun 5. Hawaii Medical Journal, 70(7 Suppl. 1), 37–41. [PMC free article] [PubMed] [Google Scholar]
- Kelder S, Hoelscher DM, Barroso CS, Walker JL, Cribb P, & Hu S (2005). The CATCH Kids Club: A pilot after-school study for improving elementary students’ nutrition and physical activity. Public Health Nutrition, 8, 133–140. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Marshall SJ, Sallis JF, & Conway TL (2000). Leisure-time physical activity in school environments: An observational study using SOPLAY. Preventive Medicine, 30, 70–77. doi: 10.1006/pmed.1999.0591 [DOI] [PubMed] [Google Scholar]
- Missouri Afterschool Network. (2006). Core competencies for youth development professionals, Kansas and Missouri (1st ed.). Retrieved from https://www.openinitiative.org/Resources/Core%20Competencies/CoreComp2011.pdf
- National Association of Sport and Physical Education. (2009). Physical activity used as punishment and/or behavior management. Retrieved from http://www.shapeamerica.org/advocacy/positionstatements/pa/loader.cfm?csModule=security/getfile&pageid=4737
- Nigg CR, Battista J, Chang JA, Yamashita M, & Chung RS (2004). Physical activity outcomes of a pilot intervention using SPARK active recreation in elementary after-school programs. Journal of Sport & Exercise Psychology, 26, S144–S145. [Google Scholar]
- North Carolina Afterschool Professional Development Work Group. (2010). North Carolina afterschool professional core competencies. Retrieved from http://www.nccap.net/media/pages/A)_FINAL-_CORE_COMPETENCIES.pdf
- Ridgers ND, Stratton G, & McKenzie TL (2010). Reliability and validity of the system for observing children’s activity and relationships during play (SOCARP). Journal of Physical Activity & Health, 7, 17–25. [DOI] [PubMed] [Google Scholar]
- Sallis JE, & Owen N (2002). Ecological models of health behaviour In Glanz K, Rimer B, & Lewis F (Eds.), Health behavior and health education: Theory, research and practice (Vol. 3, pp. 462484). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Sharpe EK, Forrester S, & Mandigo J (2011). Engaging community providers to create more active after-school environments: Results from the Ontario CATCH Kids Club implementation project. Journal of Physical Activity & Health, 8(Suppl. 1), S26S31. [DOI] [PubMed] [Google Scholar]
- Stuntz CP, & Weiss MR (2010). Motivating children and adolescents to sustain a physically active lifestyle. American Journal of Lifestyle Medicine, 4(5), 433–444. doi: 10.1177/1559827610368779 [DOI] [Google Scholar]
- Weaver RG, Beets MW, Saunders RP, & Beighle A (2014). A coordinated comprehensive professional development training’s effect on summer day camp staff healthy eating and physical activity promoting behaviors. Journal of Physical Activity & Health, 11, 1170–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Saunders RP, Beighle A, & Webster C (2014). A comprehensive professional development training’s effect on afterschool program staff behaviors to promote healthy eating and physical activity. Journal of Public Health Management & Practice, 20(4), E6–E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Webster C, Beighle A, & Huberty J (2012). A conceptual model for training after-school program staffers to promote physical activity and nutrition. Journal of School Health, 82, 186–195. doi: 10.1111/j.1746-1561.2011.00685.x [DOI] [PubMed] [Google Scholar]
- Weaver RG, Beets MW, Webster C, & Huberty J (2014). System for Observing Staff Promotion of Activity and Nutrition (SOSPAN). Journal of Physical Activity & Health, 11, 173–185. [DOI] [PubMed] [Google Scholar]
- Wiecha J, Gannett E, Hall G, & Roth B (2011). National afterschool association standards for healthy eating and physical activity in out-of-school time programs. Retrieved from http://www.niost.org/pdf/host/Healthy_Eating_and_Physical_Activity_Standards.pdf [DOI] [PubMed]
- Zarrett N, Skiles B, Wilson DK, & McClintock L (2012). A qualitative study of staff’s perspectives on implementing an after school program promoting youth physical activity. Evaluation and Program Planning, 35, 417–426. doi: 10.1016/j.evalprogplan.2011.12.003 [DOI] [PubMed] [Google Scholar]
- Zaykin DV, Zhivotovsky LA, Westfall PH, & Weir BS (2002). Truncated product method for combining P-values. Genetic Epidemiology, 22, 170–185. [DOI] [PubMed] [Google Scholar]