Abstract
Background:
There is no known safe level of alcohol use among patients with HIV and liver disease. We examined the effectiveness of integrated stepped alcohol treatment (ISAT) on alcohol use, HIV, and liver outcomes among patients with HIV and liver disease.
Methods:
In this multi-site, randomized trial conducted between January 28, 2013 through July 15, 2016, we enrolled 95 patients with HIV and liver disease [defined as having active hepatitis C infection or FIB-4 score>1.45]. ISAT (n=49) involved: Step 1- Brief Negotiated Interview with telephone booster, Step 2- Motivational Enhancement Therapy, and Step 3- Addiction Physician Management. Treatment as usual (TAU) (n=46) involved receipt of a health handout plus routine care. Analyses were conducted based on intention to treat.
Results:
Among ISAT participants, 55% advanced to Step 2, among whom 70% advanced to Step 3. Participants randomized to ISAT and TAU increased abstinence (primary outcome) over time. Abstinence rates were non-significantly higher by self-report (38% vs. 23%, adjusted odds ratio [AOR] [95% CI]= 2.6 [0.8, 9.0]) and phosphatidylethanol (43% vs. 32%, AOR [95% CI]= 1.8 [0.5, 6.3] among those randomized to ISAT vs. TAU at week 24. VACS Index scores (AMD [95% CI]= 1.1 [−3.2, 5.5]) and the proportion with an undetectable HIV viral load (AOR [95% CI]= 0.3 [0.1, 1.3]) did not differ by group at week 24 (p values >0.05). ISAT had non-significantly lower FIB-4 scores (adjusted mean difference [AMD] [95% CI]= −0.2 [−0.9, 0.5]), ALT (AMD [95% CI]= −7 [−20, 7]) and AST (AMD [95% CI]= −4 [−15, 7]) at week 24 compared to TAU.
Conclusion:
ISAT is feasible and potentially effective at enhancing delivery of evidence-based alcohol treatment to promote alcohol abstinence and improve liver biomarkers among patients with HIV and liver disease.
Keywords: HIV, hepatitis C, alcohol-related disorders, delivery of health care, integrated
1. INTRODUCTION
Globally, liver disease is a leading cause of morbidity and mortality among people with HIV (PWH) (Farahani, Mulinder, Farahani, & Marlink, 2017). In addition to HIV-related causes (e.g., antiretroviral therapy [ART] toxicities), this is driven by viral hepatitis, particularly hepatitis C virus (HCV), with an estimated 2.75 million people worldwide estimated to be co-infected with HCV and HIV (World Health Organization).
Alcohol use contributes to increased risk of liver fibrosis, hepatocellular carcinoma, and death (Lim et al., 2014; McGinnis et al., 2006). Alcohol synergistically interacts with viral infections to increase viral replication and undermines efforts along the care continuum to promote HIV viral suppression (Fuster & Samet, 2018; Marcus et al., 2018; Williams et al., 2018). Because of this, there is no known safe level of alcohol use among patients with HIV/HCV-coinfection or liver fibrosis regardless of etiology and guidelines recommend alcohol abstinence among patients with liver disease. The challenge of getting patients with such low levels of alcohol use to consider abstinence cannot be overstated. Most interventions to decrease alcohol consumption have focused on patients with established alcohol use disorder who are motivated by life events to achieve abstinence. Similarly, brief interventions have focused on “at-risk” drinking, as defined by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) (National Institute on Alcohol Abuse and Alcoholism). No studies have targeted drinking in individuals with moderate alcohol use (i.e., levels of use below at-risk levels and not consistent with alcohol use disorder) and liver disease with a goal of abstinence (Khan et al., 2016; Sims, Maynard, & Melton, 2016).
There are a number of evidence-based counseling and medication treatment options available to address alcohol use among patients with HIV and liver disease (Fuster & Samet, 2018). Yet, patients often fail to receive alcohol-related treatment (Fultz et al., 2003) and are frequently unaware of the health risks associated with their alcohol use (Elliott, Aharonovich, O’Leary, Johnston, & Hasin, 2014). To address this problem, models of care that result in integration of alcohol treatment into specialty settings (e.g., HIV or liver treatment settings) are recommended (Institute of Medicine, 2005; SAMHSA-HRSA Center for Integrated Health Solutions; Singal, Bataller, Ahn, Kamath, & Shah, 2018). However, given variability in patient response to alcohol treatment, models of care that are flexible and responsive for individual patients are needed. Such “stepped care models,” whereby the intensity of services increases for patients with suboptimal treatment responses, have been applied to multiple chronic health conditions (e.g., chronic pain, depression and hypertension) (Bair et al., 2015; van Straten, Hill, Richards, & Cuijpers, 2015) and offer a potential strategy to optimize alcohol treatment (M. B. Sobell & Sobell, 2000).
To date, there have been a paucity of studies focused on integrating alcohol treatment into specialty care settings to specifically reach patients with HIV and liver disease. A few prior efforts have focused on integrating alcohol treatment with HCV (Khan et al., 2016; Proeschold-Bell et al., 2018; Sims et al., 2016) and HIV (Edelman et al., 2018; Hasin et al., 2013; Kahler et al., 2018; Korthuis et al., 2017; Springer et al., 2017) care for patients with unhealthy alcohol use (i.e. the spectrum of alcohol use ranging from at-risk drinking to alcohol use disorder). To our knowledge, previous studies have not targeted patients with HIV and liver disease, focused on lower alcohol use risk levels, or included a stepped care model. Thus, the goals of the present study were to examine the effectiveness of a stepped care model to address alcohol use among patients with HIV and liver disease who report moderate alcohol use in a manner that is integrated into their ongoing healthcare within HIV treatment settings. We hypothesized that integrated stepped alcohol treatment (ISAT) would be associated with improved drinking and health outcomes compared to treatment as usual.
2. METHODS
2.1. Settings and Participants
The Starting Treatment for Ethanol in Primary Care (STEP) Moderate Alcohol Use with Liver Disease (MALD) Trial was conducted as part of three parallel trials addressing different levels of alcohol-related risk in patients with HIV; these two other trials separately enrolled patients who met criteria for at-risk drinking or alcohol use disorder (Edelman et al., 2019; Edelman et al., 2017). The trial was conducted according to standards in the field (Witkiewitz, Finney, Harris, Kivlahan, & Kranzler, 2015), and the protocol and implementation experiences have been reported (Edelman et al., 2016; Edelman et al., 2019; Edelman et al., 2017). From January 28, 2013 through July 15, 2016, we recruited participants across five Veterans Health Administration (VA) Infectious Disease (HIV) Clinics to participate in the STEP MALD Trial. Patients, the majority of whom were not seeking treatment for their alcohol use, were recruited into the study using a multi-pronged approach.
Patients were eligible if they met the following criteria: 1) were HIV positive; 2) received care at one of the five participating Veterans Health Administration (VA) HIV Clinics; 3) English speaking and were able to provide written informed consent; and 4) reported any alcohol consumption in the past 30 days AUDIT-C >0 (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998) and by Timeline Followback [TLFB] (L. C. Sobell & Sobell, 1996) and 5) were either hepatitis C virus co-infected (confirmed by HCV antibody and presence of detectable HCV RNA viral load) or had evidence of liver fibrosis (defined as FIB-4 score >1.45) (Lim et al., 2014; Sterling et al., 2006) (Figure 1).
Figure 1. Participant Flow.
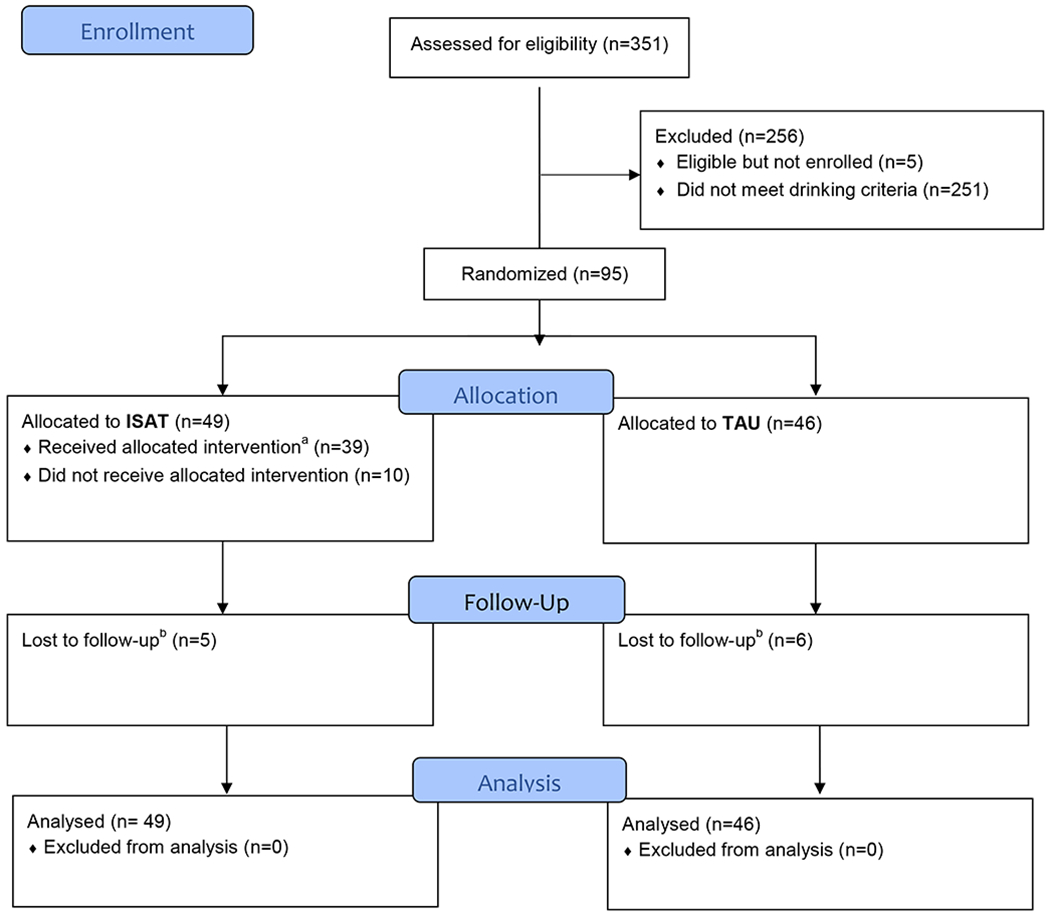
Notes: a. Received allocated intervention: defined as attending at least one intervention visit over the 24 week period. b. Lost to follow-up: defined as not having any assessment at week 24 and afterwards through week 52.
Patients were excluded if they met the following criteria: 1) met criteria for at-risk drinking (alcohol consumption defined for men less than or equal to 65 years old as drinking an average of 14 or more drinks per week or 4 or more drinks per occasion, or for women and men older than 65 years old as 7 or more drinks per week or three or more drinks per occasion during the past 30 days by TLFB) (National Institute on Alcohol Abuse and Alcoholism) or alcohol use disorder (by the mini-SCI D) (American Psychiatric Association, 2013); 2) were acutely suicidal or with a psychiatric condition that affected their ability to provide informed consent or participate in counseling interventions; 3) were currently enrolled in formal treatment for unhealthy alcohol use, excluding self or mutual-help groups (e.g., Alcoholics Anonymous); 4) had any medical condition(s) that would preclude completing the study or cause harm during the course of the study; and 5) were a pregnant or nursing woman, or woman of child-bearing potential who did not agree to use a reliable form of birth control. Since abstinence is recommended during pregnancy and specialty care might be required to achieve this goal, this final criterion was put in place to avoid randomizing pregnant women to treatment as usual.
Participants provided written and informed consent and were reimbursed $25 for baseline assessments and $50 for follow-up assessments. The study was approved by Institutional Review Boards at Yale, VA Connecticut Healthcare System, and each participating VA site. The study was Health Insurance Portability and Accountability Act (HIPAA) compliant, and a Certificate of Confidentiality was obtained from NIAAA. The study was registered at www.clinicaltrials.gov (ClinicalTrials.gov identifier: NCT01410123).
2.2. Treatment Conditions
Eligible and consented patients were randomized to ISAT versus treatment as usual (TAU). Regardless of treatment group, participants could receive any non-study services recommended by VA clinicians.
2.3. Integrated Stepped Alcohol Treatment
ISAT interventions were stepped up at pre-defined time points based on a priori criteria and delivered over the course of a 24-week period. Because this was an effectiveness trial, neither patients nor providers were specifically incentivized to attend or complete sessions as part of ISAT. ISAT was provided by VA clinicians and whenever possible occurred in the HIV clinics (i.e., co-located), where patients received their routine HIV care.
2.3.1. Step 1
Step 1 consisted of a brief psychosocial intervention, the Brief Negotiated Interview (BNI) delivered by an onsite social worker. This manual-guided brief intervention is based upon principles of motivational interviewing and the stages of change model of behavior change. The BNI has demonstrated efficacy in decreasing alcohol use in patients with at-risk drinking (D’Onofrio et al., 2012). For this trial, the content was modified to include HIV and HCV specific content.
The main goals of the session, designed to be 15 to 20 minutes long, were to: 1) decrease participant ambivalence to reduce alcohol use by reviewing the participant’s perceptions regarding pros and cons of alcohol use and providing tailored feedback regarding the impact of alcohol on the participant’s medical conditions using the STEP Trials Feedback Form and 2) negotiate strategies for change based on the participant’s readiness to change. Participants were also referred to web-based resources for help. Modeled after Project TREAT (Fleming, Barry, Manwell, Johnson, & London, 1997), a telephone booster designed to be 15 to 20 minutes in duration occurred 2 weeks after the BNI session. This was also conducted by the social worker and, following a similar structure as the BNI, was designed to review participant progress and challenges towards meeting their drinking goals.
2.3.2. Step 2
At the week 4 research assessment, those reporting any alcohol use in the prior 14 days by TLFB (L. C. Sobell & Sobell, 1996) were advanced to Step 2, which provided four sessions of psychologist-delivered Motivational Enhancement Therapy (MET). MET sessions, scheduled every other week over the course of six weeks, were manual-guided with content tailored to PWH (Maisto et al., 2001). Grounded in motivational interviewing and the stages of change model for behavior change, the psychologists employed reflective listening to help elicit participant-centered reasons to decrease their alcohol use; promoted skill-building as indicated; provided individual-level feedback regarding the potential impact of alcohol on the participant’s health (e.g., increased liver function tests); and offered web-based resources for self-help.
2.3.3. Step 3
At week 12, those who were advanced to Step 2 and who reported any alcohol use in the prior 14 days, were advanced to Step 3. Step 3 included Addiction Psychiatrist-delivered Addiction Physician Management (APM) with an emphasis on consideration of medications to decrease alcohol use with medical management, consistent with the approach used to provide buprenorphine for treatment of opioid use disorder in HIV treatment settings (Fiellin et al., 2006; Tetrault et al., 2012). Following an initial assessment visit, subsequent visits were scheduled weekly for two weeks, every other week for four weeks and then monthly for a total of five visits.
2.4. Treatment as Usual
As part of recommended care in the VA, for every patient followed in a primary care clinic, including HIV clinics, providers are prompted to be screened annually with an AUDIT-C via a clinical reminder. This reminder includes prompts to conduct brief interventions or referral to addiction treatment as indicated (U.S. Department of Veteran Affairs, 2011). In addition, participants received a health handout that includes advice about drinking in the context of general health advice (e.g., smoking cessation, exercise).
2.5. Assignment of Treatment
We used a web-based clinical trial management system (Nadkarni et al., 1998) to randomize patients in a 1:1 ratio to ISAT or TAU stratified by site. The randomization sequence was concealed. Blinding of patients, providers or research assistants following randomization was not possible.
2.6. Monitoring Intervention Fidelity and Adherence
After initial training of social workers, psychologists and psychiatrists, the study team offered ongoing supervision and monitoring by teleconferences held every 1 to 2 months; provided structured encounter forms to guide intervention sessions; and conducted two site visits per site. BNI and MET sessions were digitally recorded and a subset were reviewed with feedback provided by a study psychologist. We tracked the number of completed sessions and the session duration. VA-based pharmacy data were used to assess prescription of Food and Drug Administration (FDA) (i.e., disulfiram, acamprosate and naltrexone) (Jonas et al., 2014) and non-FDA (i.e. topiramate, baclofen and gabapentin) (Soyka & Lieb, 2015) approved medications used to treat alcohol use disorder in the six months prior to randomization and through week 52.
2.7. Outcomes
The primary effectiveness outcome was past 30-day alcohol abstinence at week 24 by TLFB. Additional drinking outcomes at week 24 and based on the past 30 days by TLFB included: drinks per week, percentage of participants with no heavy drinking days (where a heavy drinking day was defined for men as >5 drinks per day and for women as >4 drinks per day), drinks per drinking day, and percentage of days abstinent; and phosphatidylethanol (PEth) blood levels (an alcohol biomarker that reflects past 21 days of alcohol consumption, with higher levels associated with greater quantities of alcohol use and values of <8 ng/mL consistent with abstinence or near abstinence) (Wurst et al., 2015). We also assessed biomarkers impacted either directly and/or indirectly by alcohol use including: the VACS Index score (validated measure of morbidity and mortality, with higher scores associated with increasing mortality risk) (Justice et al., 2016); undetectable plasma HIV viral load (HIV RNA <50 copies/mL); and liver markers (FIB-4 [validated non-invasive measure of liver fibrosis](Sterling et al., 2006), alanine aminotransferase [ALT], and aspartate aminotransferase [AST]).
We additionally assessed durability of the intervention by examining outcomes at week 52 (except for PEth, which was only collected at baseline and week 24). PEth was not used to determine study eligibility nor did clinicians or the coordinating center monitor PEth values during the study. Receipt of VA-based outpatient and inpatient addiction treatment services as well as all-cause emergency department visits or hospitalizations were assessed by electronic medical record (EMR) data during the 180-day period prior to baseline, week 24 and week 52, respectively.
2.8. Sample Size Calculations and Statistical Analysis
To detect an absolute increase of 15% (from 10% to 25%) in self-reported abstinence, a sample size of 97 participants per group was needed to have 80% power at the two-sided 0.05 significance level. Given an anticipated 15% dropout rate, our target enrollment was 228. Due to slower than expected recruitment, we enrolled 95 participants and recruitment was halted after 3.5 years of enrollment given that it was unlikely that we would be able to meet recruitment targets. With a total of 95 participants, we had 80% power to detect a difference of 25% in self-reported abstinence (from 10% to 35%).
We used descriptive statistics to compare baseline characteristics of the treatment groups, report attendance at scheduled intervention visits, proportion receiving treatment medications, and session duration. Our primary analysis was based on intention to treat (ITT), including all participants in the group to which they were randomized. We used generalized linear mixed effects models to evaluate the proportion with self-reported abstinence and no heavy drinking days. We used linear mixed effects models to evaluate drinks per week, drinks per drinking day, percentage of days abstinent, VACS Index, FIB-4, ALT and AST with the assumption that missing data occurred at random. Analyses included fixed effects for intervention (ISAT vs. TAU), time (4, 12, 24, and 52 weeks), and the interaction of intervention with time. Additional fixed effects included baseline covariates: baseline outcome level, VACS Index and site. Random intercept and time effects were included for each participant with an unstructured covariance pattern for serial correlation. Linear contrasts were used to estimate intervention group differences and 95% confidence intervals (CI) at week 24 (primary) and week 52. Linear regression analyses were used to compare 24 week differences in PEth levels.
In post-hoc adherence adjusted analyses, we adjusted for intervention adherence to determine the effect of ISAT that would have been observed if all participants maintained an adequate level of adherence. We used the marginal structural model (MSM) approach (46) that employs inverse probability weights based on an individual’s propensity to adhere throughout the study. The inverse probability weighting employed in MSM creates a pseudo-population which removes the confounding effects of adherence. The adequate level of adherence of at least 30% of ISAT expected visits was chosen given this was the average level of adherence. Stabilized probability weights for less than 30% adherence to ISAT interventions were created using a logistic regression with baseline (age, drinks per week, race, site, HIV viral load, depressive symptoms by Patient Health Questionniare-9 scores, any drug use, education and employment) and time varying (drinks per week) covariates. The MSM was then implemented by weighted generalized estimating equations (GEE). Odds ratios and 95% CIs are presented demonstrating the impact of ISAT if an adequate level of adherence was maintained.
In sensitivity analyses, we excluded those with a baseline AUDIT-C = 8 and VACS Index score ≥ 99 (given that this is consistent with severe illness) to examine the impact of the intervention on self-reported abstinence. Additionally, we evaluated the impact of the intervention on PEth as a continuous outcome. Lastly, in analyses examining the impact of the intervention on PEth, we excluded those with a baseline PEth <8ng/mL.
All analyses involved 2-tailed tests of significance and were performed using SAS v9.4 (SAS Institute, Cary, NC). P values < 0.05 were considered statistically significant.
2.9. Role of the funding source
STEP Trial researchers had primary responsibility for study design, data collection, analysis, data interpretation, and writing of the manuscript. NIAAA staff (KJB) collaborated in the design of the study and provided comments for consideration in drafts of the manuscript. None of the study sponsors had a role in data collection, analysis, or data interpretation. All authors had final responsibility for the decision to submit for publication.
3. RESULTS
3.1. Participant Flow
Out of 351 patients who met eligibility criteria for any of the STEP Trials, 95 were randomized (Figure 1). Despite a multi-pronged approach (Edelman et al., 2017), we only recruited 42% of the target population (n=95/228). Among the 95 randomized participants, 84 (88%) completed the study (i.e., not lost to follow-up), with 87 (92%) providing data at week 4, 82 (86%) providing data at week 12, 81 (85%) providing data at week 24 and 76 (80%) providing data at week 52.
3.2. Baseline Demographic and Clinical Characteristics
The mean age was 61 years (range 33-87), 94 (99%) were men, and 81 (85%) were black. The mean AUDIT-C score was 3 (range 1 –8) and drinks per week was 3.46 (range 0.03-26). Characteristics of participants randomized to ISAT and TAU did not differ (Table 1).
Table 1.
Participant Baseline Demographic and Clinical Characteristics
| No. (%) | p value | |||
|---|---|---|---|---|
| Characteristic | Integrated Stepped Alcohol Treatment (n=49) | Treatment as Usual (n=46) | ||
| Men | 49 (100.0) | 45 (97.8) | 0.48 | |
| Race | 0.39 | |||
| White | 8 (16.3) | 3 (6.5) | ||
| Black | 40 (81.6) | 41 (89.1) | ||
| Other | 1 (2.0) | 2 (4.4) | ||
| Hispanic | 4 (8.2) | 0 (0) | 0.12 | |
| Age, mean (SD), y | 59.7 (6.3) | 61.7 (7.8) | 0.16 | |
| Education | 0.24 | |||
| High school or less | 24 (49.0) | 17 (37.0) | ||
| >High school | 25 (51.0) | 29 (63.0) | ||
| Married or domestic partner | 10 (20.4) | 9 (19.6) | 0.36 | |
| Employment statusa | 0.47 | |||
| Employed | 17 (34.7) | 14 (30.4) | ||
| Retired/disability | 24 (49.0) | 27 (58.7) | ||
| Unemployed or unable to work | 8 (16.3) | 4 (8.7) | ||
| AUDIT-C score, mean (SD)b | 2.94 (1.81) | 3.11 (1.69) | 0.64 | |
| Other substance use, past 30 daysc | ||||
| Smoke cigarettes | 21 (42.9) | 25 (56.8) | 0.18 | |
| Cannabis | 13 (26.5) | 8 (18.2) | 0.34 | |
| Cocaine | 3 (6.1) | 5 (10.9) | 0.48 | |
| Heroin | 0 (0) | 0 (0) | NA | |
| Prescription opioids | 1 (2.0) | 1 (2.2) | 0.99 | |
| Comorbid conditions and biomarkers | ||||
| Hepatitis C co-infectiond | 36 (73.5) | 26 (59.1) | 0.14 | |
| FIB-4 score> 1.45e,f | 40 (81.6) | 41 (91.1) | 0.18 | |
| Depressive symptomsg | 7 (14.3) | 6 (13.0) | 0.86 | |
| HIV related measures | ||||
| VACS Index, median (range)f,h | 33 (5, 99) | 42 (5, 116) | 0.09 | |
| Detectable HIV viral loadf,i | 13 (26.5) | 13 (28.9) | 0.80 | |
| CD4 cell count, cells/mm3, median (range)f | 572 (186, 1221) | 521 (16, 1258) | 0.33 | |
Employment status, employment during past 3 years: assessed based on the Addiction Severity Index Lite-CF55
Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) scores range from 0 to 12.
Other substance use, past 30 days: assessed based on item “Do you know smoke cigarettes (as of 1 month ago)?” and the Addiction Severity Index Lite-CF55
Hepatitis C coinfection status – based on positive antibody and detectable HCV RNA viral load
FIB-4 score – a noninvasive measure of liver fibrosis calculated based on aspartate aminotransferase, alanine aminotransferase, and platelets with scores greater than 1.45 concerning for liver fibrosis
Laboratory testing performed within 30 days prior to randomization date
Depressive symptoms determined using the Patient Health Questionnaire (PHQ)-9 with score >9 defined as having depressive symptoms56
VACS index – validated measure of morbidity and mortality risk57
Detectable HIV viral load – defined as ≥50 copies/mL
3.3. ISAT Intervention Receipt
Regarding Step 1, 76% received the BNI and 35% received the telephone booster. Twenty-seven (27/49, 55%)met criteria for advancing to Step 2, and 19 of 27 in Step 2 (70%) met criteria for advancing to Step 3. Among those advanced to Step 2, 14 (52%) attended the first visit while 7 (26%) attended the fourth visit (Figure 2). Among those advanced to Step 3, 8 (42%) attended the first APM visit, while 3 (16%) attended the fifth visit. Across the four MET sessions, the mean duration was 28 minutes, ranging from 3 to 60 minutes; across the five APM sessions, the mean duration was 41 minutes, ranging from 10 to 90 minutes. There was no significant difference by treatment group in receipt of alcohol treatment medications (Table 2).
Figure 2. Visit attendance among those randomized to integrated stepped alcohol treatment*.
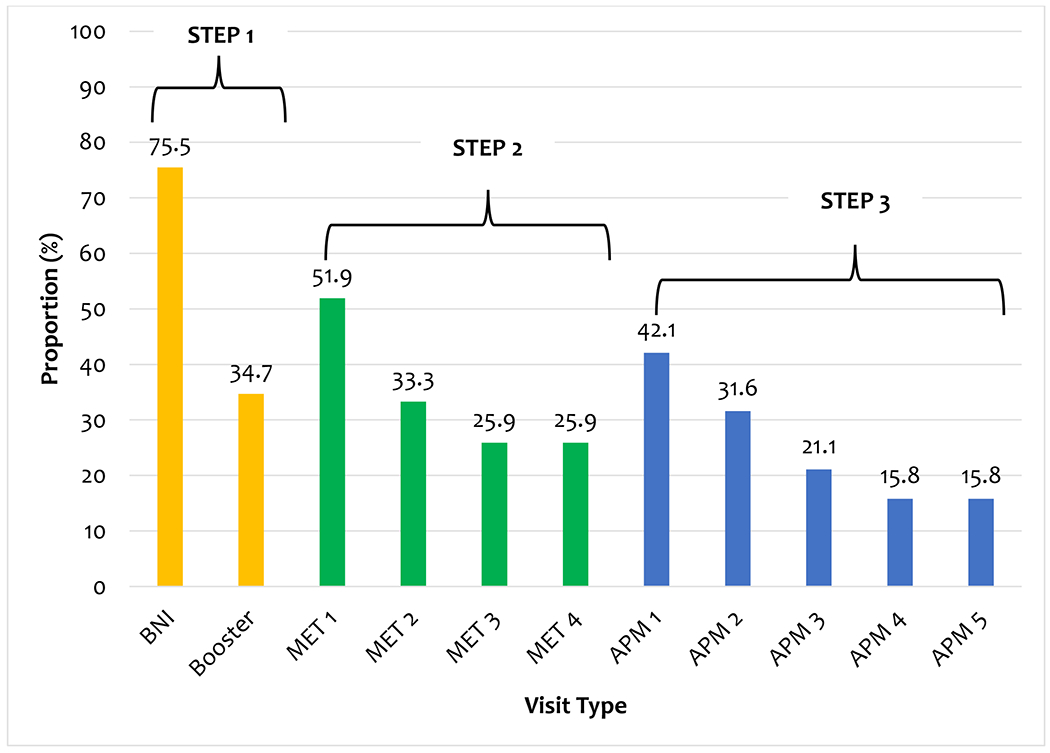
Note: *Denominator is among those eligible for the intervention: STEP 1, n=49; Step 2, n=27; Step 3, n=19. BNI=brief negotiated interview; MET=motivational enhancement therapy; APM=addiction physician management.
Table 2.
Past 6 month receipt of alcohol treatment medications at baseline and follow-up by treatment group
| Medication, n (%) | Integrated Stepped Alcohol Treatment (n=46) | Treatment as Usual (n=49) | p value |
|---|---|---|---|
| Any alcohol treatment medicationa | |||
| Baseline | 6 (12.2) | 3 (6.5) | 0.49 |
| Week 24 | 8 (16.3) | 3 (6.5) | 0.14 |
| Week 52 | 5 (10.2) | 4 (8.7) | 1.0 |
| Disulfiram | |||
| Baseline | 0 (0) | 0 (0) | NA |
| Week 24 | 0 (0) | 0 (0) | NA |
| Week 52 | 0 (0) | 0 (0) | NA |
| Acamprosate | |||
| Baseline | 0 (0) | 0 (0) | NA |
| Week 24 | 0 (0) | 0 (0) | NA |
| Week 52 | 0 (0) | 0 (0) | NA |
| Naltrexone | |||
| Baseline | 0 (0) | 0 (0) | NA |
| Week 24 | 2 (4.1) | 0 (0) | 0.50 |
| Week 52 | 0 (0) | 0 (0) | NA |
| Topiramate | |||
| Baseline | 0 (0) | 0 (0) | NA |
| Week 24 | 0 (0) | 0 (0) | NA |
| Week 52 | 0 (0) | 1 (2.2) | 0.48 |
| Baclofen | |||
| Baseline | 0 (0) | 1 (2.2) | 0.48 |
| Week 24 | 0 (0) | 1 (2.2) | 0.48 |
| Week 52 | 0 (0) | 2 (4.4) | 0.23 |
| Gabapentin | |||
| Baseline | 6 (12.2) | 3 (6.5) | 0.49 |
| Week 24 | 7 (14.3) | 3 (6.5) | 0.32 |
| Week 52 | 5 (10.2) | 2 (4.4) | 0.44 |
. Based on receipt of disulfiram, acamprosate, naltrexone, topiramate, baclofen and/or gabapentin.
3.4. Alcohol Consumption Outcomes
3.4.1. Primary outcome, past 30 day self-reported abstinence
Both groups reported increased abstinence over time (Figure 3a, Appendix Table 1). At week 24 (primary outcome), we did not detect a statistically significant difference between the ISAT and TAU in self-reported abstinence (38.1% vs. 23.1%, adjusted odds ratio [AOR] [95% CI]= 2.6 [0.8, 9.0], p=0.12). At week 52, we were unable to detect a difference among those randomized to ISAT and TAU in the proportion with self-reported abstinence (32.5 % vs. 36.1%, AOR [95% CI]= 0.8 [0.3, 2.7], p=0.75).
Figure 3. Drinking outcomesa.
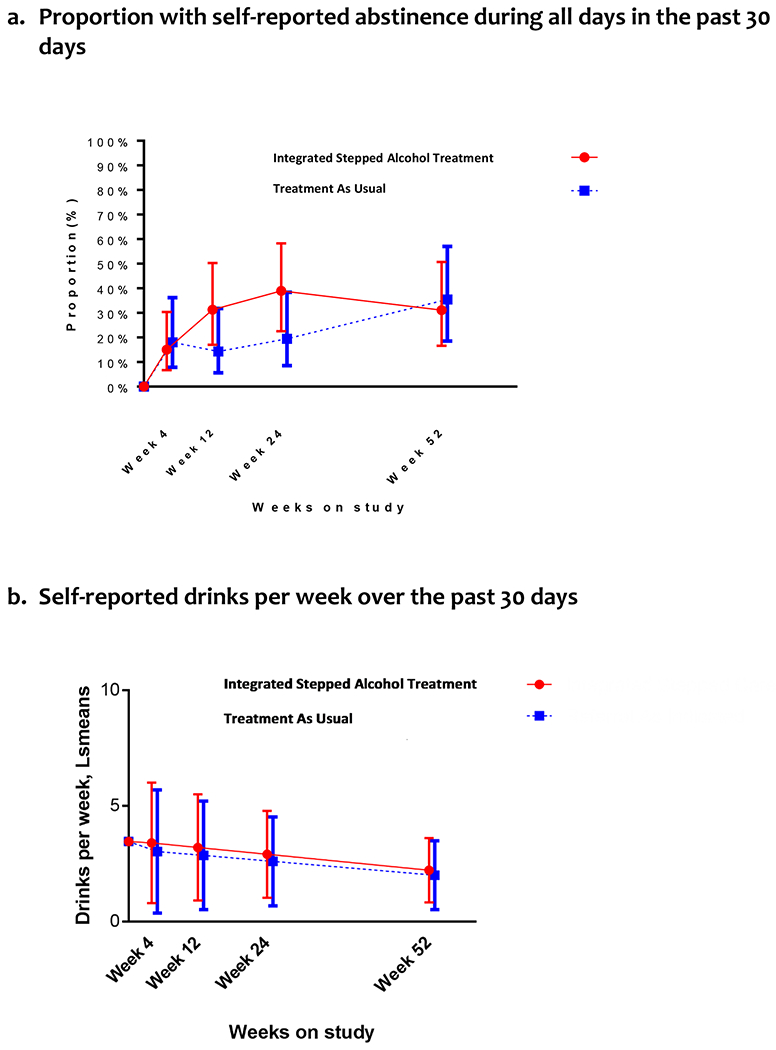
a. Random intercept and, for the continuous outcome, time effects were included for each participant with an unstructured covariance pattern for serial correlation. Abstinence was defined as no reported alcohol use on any day in the past 30 days.
3.4.2. Other alcohol consumption outcomes
We did not detect a difference in drinks per week between the ISAT and TAU groups (Least square mean (Lsmean) = 2.5 vs. 3.5, adjusted mean difference [AMD] [95% CI]= 0.3 [−2.0, 2.6], p=0.79). Findings were consistent at week 52 (Lsmean= 2.5 vs. 1.9, AMD= 0.2 [−1.2, 1.6], p=0.75). The percent of participants with no heavy drinking days was similar among those randomized to ISAT compared to TAU at week 24 (81% vs. 90%, adjusted odds ratio [AOR] [95% CI]= 0.4 [0.1, 1.9], p=0.22) and at week 52 (88% vs. 89%, AOR [95% CI]= 0.47 [0.08, 2.82], p=0.41)]. The drinks per drinking day was non-significantly lower among those randomized to ISAT compared to TAU at week 24 [(Lsmean: 2.5 vs. 4.6), AMD= −2.02 (−6.72, 2.68), p=0.39] and at week 52 [(Lsmean: 2.7 vs. 1.9), AMD= −7.7 (−23.2, 7.8), p=0.32]. The percentage of days abstinent was non-significantly higher among those randomized to ISAT compared to TAU at week 24 (Lsmean = 89% vs. 82%), AMD [95% CI]= 2% [−4%, 7%)], p=0.47) and at week 52 (LSmean= 89% vs. 86%, AMD=2% [−6%, 9%], p=0.68). The proportion with abstinence by PEth was non-significantly higher among those randomized to ISAT compared to TAU at week 24 (43% vs. 32%, AOR [95% CI]= 1.8 [0.5, 6.3], p=0.35) and consistent with self-reported data.
3.5. HIV and Liver Biomarker Outcomes
At week 24, participants randomized to ISAT had similar VACS Index scores as those randomized to TAU (Lsmean = 36 vs. 42, AMD= 1 [−3, 6], p=0.60). Findings were consistent at week 52 (LSmean=38 vs. 41; AMD [95% CI]=0.8 [−5, 6], p=0.77). The proportion of participants with an undetectable HIV viral load did not differ among those randomized to ISAT and TAU at week 24 (72% vs. 86%, AOR [95% CI]= 0.3 [0.1, 1.3], p=0.09) or at week 52 (84% vs. 79%, AOR=1.7 [0.4, 8.4], p=0.49). Participants randomized to ISAT had non-significantly lower FIB-4 scores (AMD [95% CI]= −0.2 [−0.9, 0.5]), ALT (AMD [95% CI]= −7 (−20, 7)] and AST (AMD [95% CI]= −4 (−15, −7)] at week 24 compared to those randomized to TAU. Findings were consistent at week 52: FIB-4 scores (AMD [95% CI]= −0.6 [−1.6, 0.4]), ALT (AMD [95% CI]= −19 (−42, 4)] and AST (AMD [95% CI]= −17 (−36, 2)].
3.6. Healthcare use
At 24 weeks, a higher proportion of those randomized to ISAT had received outpatient alcohol treatment services compared to those randomized to TAU (31% vs. 15%, p=0.08). These differences were smaller at week 52 (18% vs. 11%, p=0.30). The ISAT and TAU groups did not differ on inpatient alcohol treatment, Emergency Department visit number or hospitalizations. Findings were consistent at week 52.
3.7. Post-Hoc and Sensitivity Analyses
In the post-hoc per protocol analysis adjusted for intervention adherence, ISAT participants who completed at least 30% of intervention visits were more likely to report abstinence than those randomized to TAU (adjusted proportion= 61% vs. 26%; AOR [95% CI]= 2.37 [0.88, 6.37], p=0.09). Sensitivity analyses yielded consistent findings.
4. DISCUSSION
The STEP MALD Trial, focused on evaluating the effectiveness of integrated stepped alcohol treatment to promote alcohol abstinence among patient with HIV and liver disease, yielded several important findings. First, in this population with lower levels of alcohol use but reasons for abstinence due to liver disease, it was difficult to both recruit and retain patients in an alcohol-focused intervention. Second, ISAT translated into increased receipt of evidence-based alcohol treatments with over 50% meeting criteria for additional services beyond the standard BNI and booster and over 70% meeting criteria for additional services after the addition of MET; this supports the feasibility and relevance of a stepped care model for these interventions. Third, although not statistically significant, findings lend support for the preliminary effectiveness of ISAT on promoting alcohol abstinence based on both self-report and biomarker data and fewer drinks per drinking day. Notably, ISAT had a stronger effect on promoting alcohol abstinence among those patients who completed at least 30% of the intervention visits. Fourth, we found preliminary evidence that ISAT translates into improved liver-related markers, including FIB-4, ALT and AST, likely reflecting increased alcohol abstinence. Taken together, these findings are an important contribution to the literature by being the first study to our knowledge to: 1) target alcohol use specifically in PWH and liver disease, 2) focus on lower levels of alcohol consumption with a target of abstinence, and 3) include a stepped care model in a clinic that did not routinely provide specialty addiction treatment.
Despite guidelines that people with liver disease should abstain from alcohol, prior alcohol treatment interventions focused on PWH have been limited to those with higher levels of alcohol use (i.e., heavy drinking, alcohol use disorder) (Chander, Hutton, Lau, Xu, & McCaul, 2015; Edelman et al., 2018; Kahler et al., 2018; Korthuis et al., 2017; Springer et al., 2017). Given this, the STEP MALD Trial results are highly relevant as work by Elliot and colleagues demonstrated that 33% among a sample of HIV/HCV coinfected patients were unaware that they had a medical condition made worse by alcohol use (Elliott et al., 2014). This finding is consistent with results from a recent survey of HIV providers demonstrating that only 25% reported “always” or “usually” provide advice on safer drinking limits to patients who drink but do not have alcohol problems (Chander et al., 2016). These findings together may, at least in part, explain our challenges in recruitment as patients may be unaware of the impact of alcohol on their health, in part because it has not been addressed by their hepatologist or HIV clinician.
While it may be hard to engage non-treatment seeking patients with lower levels of alcohol use for an alcohol intervention, our findings indicate that when patients do receive ISAT, they benefit. Specifically, we found that ISAT increased provision of evidenced-based alcohol care with non-statistically significant improvements in alcohol abstinence and in liver-related health. Our findings are consistent with prior work focused on evaluating the impact of a 2-session Brief intervention for women with HIV and hazardous alcohol use (Chander et al., 2015). Consistent with work by Chander and colleagues, we found that BI was not consistently effective given that 55% of participants had evidence of continued alcohol use at week 4 and were “stepped up” to Step 2. Furthermore, many subsequent interventionist visits were not completed suggests that these visits may not be highly prioritized by patients and/or the providers delivering the intervention. Our findings, however, are encouraging as they suggest that when patients are offered and, especially when they receive, ISAT, they may experience important health benefits. Further, given the observed drop-off after the first interventionist visit within each step, our findings suggest that interventions to promote retention in alcohol treatment should be initiated at treatment onset and greater health benefits may have been observed if participants had higher visit completion rates.
Our study should be interpreted in the context of its limitations. First, we did not meet recruitment targets and were, therefore, underpowered. Second, research assessments were used to determine whether participants met criteria to be “stepped up;” translation into routine clinical practice will require ongoing monitoring to ensure stepping up occurs as indicated. Third, the study was conducted in the VA and may not be generalizable to non-VA based settings. Fourth, consistent with the population served at VA-based HIV clinics, our sample was nearly entirely men and may not be generalizable to women. Lastly, our sample included individuals with levels of alcohol use that may have exceeded moderate levels of use based on their baseline AUDIT-C score; however, we found no differences in our findings after excluding these participants.
Our study should also be interpreted in the context of its strengths. First, the STEP MALD Trial focused on patients with lower-risk levels of alcohol use. Given recent findings that “alcohol use, regardless of amount, leads to health loss across populations” ISAT could be adapted to reach other populations (Collaborators, 2018). Second, ISAT is potentially highly relevant for specialty settings, including liver clinics, to improve delivery of alcohol related care for patients with liver fibrosis and HCV, as well as those with non-alcohol associated fatty liver disease, given findings that abstinence is associated with greater improvements in steatosis and resolution of non-alcohol associated steatohepatitis compared to moderate levels (defined as 2 or fewer drinks on a typical day) of alcohol use (Ajmera et al., 2018). Third, we achieved a follow-up rate of 80% or higher at each follow-up, decreasing bias in our findings.
In summary, ISAT is feasible and potentially effective at enhancing delivery of evidence-based alcohol related care to promote alcohol abstinence among patients with HIV and liver disease and moderate alcohol use. Future studies should evaluate strategies to enhance delivery of ISAT components via different modalities, such as telehealth, and promote retention in alcohol-related care. Furthermore, future studies should aim to evaluate the impact of ISAT in larger study populations served in liver disease treatment settings with a range of alcohol use, as well as other settings where promoting alcohol-abstinence is highly relevant such as in HIV clinics, to decrease alcohol-related morbidity and mortality.
Supplementary Material
Table 3.
Past 6-month treatment services, emergency department visits and hospitalizations at baseline and follow-up by treatment group
| Integrated Stepped Alcohol Treatment (N=49) | Treatment as Usual (N=46) | p value | |
|---|---|---|---|
| Any outpatient alcohol treatmenta,b | |||
| Baseline | 1 (2.0) | 0 (0) | NA |
| Week 24 | 15 (30.6) | 7 (15.2) | 0.08 |
| Week 52 | 9 (18.4) | 5 (10.9) | 0.30 |
| Any inpatient alcohol treatmenta,b | |||
| Baseline | 1 (2.0) | 0 (0.0) | NA |
| Week 24 | 2 (4.1) | 0 (0) | 0.50 |
| Week 52 | 3 (6.1) | 0 (0) | 0.24 |
| Emergency department visitsb | |||
| Baseline | 13 (26.5) | 12 (26.1) | NA |
| Week 24 | 13 (26.5) | 10 (21.7) | 0.59 |
| Week 52 | 13 (26.5) | 12 (26.1) | 0.96 |
| Hospitalizationb | |||
| Baseline | 3 (6.1) | 4 (8.8) | NA |
| Week 24 | 9 (18.4) | 5 (10.9) | 0.30 |
| Week 52 | 7 (14.3) | 5 (10.9) | 0.62 |
. Based on presence of an alcohol or drug related ICD-9 or ICD-10 code at any time and, for outpatient services, if they had a SUD clinic stop code or CPT code; for inpatient services, included if they had a SUD bed section stop code or ICD-9 or ICD-10 procedure code.
. Assessed using VA electronic medical record data and during the 180 day period prior to baseline, week 24, and week 52, respectively.
Highlights.
Alcohol abstinence is recommended among patients with HIV+liver disease
Patients with moderate alcohol use are rarely interested in treatment trials
Stepped care promotes evidence-based care for patients
Stepped care may also promote alcohol abstinence and improve liver markers
Acknowledgements and Disclosures
The authors would like to thank the patients and providers who participated in this research. We would like to acknowledge Ms. Laura Simone for her efforts in development and design of the data tracking system, Ms. Melissa Skanderson for her efforts in data management and Ms. Elizabeth Porter for her efforts in coordinating and implementing this research.
This work was generously support by grants from the National Institute on Alcohol Abuse and Alcoholism (grant #U01AA020795, U01AA020790, U24AA020794). EJ Edelman was supported as a Yale-Drug Abuse, HIV and Addiction Research Scholar (NIDA grant #K12DA033312) during the conduct of this work.
Funding support: This work was generously support by grants from the National Institute on Alcohol Abuse and Alcoholism (grant #U01AA020795, U01AA020790, U24AA020794). EJ Edelman was supported as a Yale-Drug Abuse, HIV and Addiction Research Scholar (NIDA grant #K12DA033312) during the conduct of this work.
Abbreviations
- HIV
Human Immunodeficiency Virus
- PWH
People with HIV
- ART
Antiretroviral Therapy
- HCV
Hepatitis C Virus
- NIAAA
National Institute of Alcohol Abuse and Alcoholism
- STEP
Starting Treatment for Ethanol in Primary Care
- MALD
Moderate Alcohol Use with Liver Disease
- VA
Veterans Administration
- AUDIT-C
Alcohol Use Disorders Identification Test
- TLFB
Timeline Followback
- RNA
Ribonucleic Acid
- FIB-4
Fibrosis-4
- SCID
Structured Clinical Interview for DSM-5 Disorders
- HIPAA
Health Insurance Portability and Accountability Act
- ISAT
Integrated Stepped Alcohol Treatment
- TAU
Treatment as Usual
- BNI
Brief Negotiated Interview
- MET
Motivational Enhancement Therapy
- APM
Addiction Physician Management
- FDA
Food and Drug Administration
- PEth
Phosphatidylethanol
- VACS (Index)
Veterans Aging Cohort Study Index
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- EMR
Electronic Medical Record
- ITT
Intention to Treat
- CI
Confidence Interval
- MSM
Marginal Structural Model
- GEE
Generalized Estimating Equations
- AOR
Adjusted Odds Ratio
- Lsmean
Least Squared Mean
- AMD
Adjusted Mean Difference
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
An earlier version of this work was presented as an oral presentation at the INEBRIA conference held on September 15, 2017 in New York, New York.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Declaration of interests: none
REFERENCES
- Ajmera V, Belt P, Wilson LA, Gill RM, Loomba R, Kleiner DE, … Nonalcoholic Steatohepatitis Clinical Research, N. (2018). Among patients with nonalcoholic fatty liver disease, modest alcohol use is associated with less improvement in histologic steatosis and steatohepatitis. Clinical Gastroenterology and Hepatology, 16(9), 1511–1520 e1515. doi: 10.1016/j.cgh.2018.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental_Disorders (Fifth Edition) Washington, D.C.: American Psychiatric Press. [Google Scholar]
- Bair MJ, Ang D, Wu J, Outcalt SD, Sargent C, Kempf C, … Kroenke K (2015). Evaluation of Stepped Care for Chronic Pain (ESCAPE) in veterans of the Iraq and Afghanistan conflicts: A randomized clinical trial. Journal of the American Medical Association Internal Medicine, 175(5), 682–689. doi: 10.1001/jamainternmed.2015.97 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDITalcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine, 158(16), 1789–1795. [DOI] [PubMed] [Google Scholar]
- Chander G, Hutton HE, Lau B, Xu X, & McCaul ME (2015). Brief intervention decreases drinking frequency in HIV-infected, heavy drinking women: Results of a randomized controlled trial. Journal of Acquired Immune Deficiency Syndrome, 70(2), 137–145. doi: 10.1097/QAI.0000000000000679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chander G, Monroe AK, Crane HM, Hutton HE, Saag MS, Cropsey K, … McCaul ME (2016). HIVprimary care providers--screening, knowledge, attitudes and behaviors related to alcohol interventions. Drug and Alcohol Dependence, 161, 59–66. doi: 10.1016/j.drugalcdep.2016.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collaborators, G. B. D. A. (2018). Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the global burden of disease study 2016. Lancet. doi: 10.1016/S0140-6736(18)31310-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Onofrio G, Fiellin DA, Pantalon MV, Chawarski MC, Owens PH, Degutis LC, … O’Connor PG (2012). A brief intervention reduces hazardous and harmful drinking in emergency department patients. Annals of Emergency Med, 60(2), 181–192. doi: 10.1016/j.annemergmed.2012.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Hansen NB, Cutter CJ, Danton C, Fiellin LE, O’Connor PG, … Fiellin DA (2016). Implementation of integrated stepped care for unhealthy alcohol use in hiv clinics. Addiction Science and Clinical Practice, 11(1), 1. doi: 10.1186/s13722-015-0048-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Maisto SA, Hansen NB, Cutter CJ, Dziura J, Deng Y, … Fiellin DA (2019). Integrated stepped alcohol treatment for patients with HIV and alcohol use disorder: A randomised controlled trial. Lancet HIV. doi: 10.1016/S2352-3018(19)30076-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Maisto SA, Hansen NB, Cutter CJ, Dziura J, Fiellin LE, … Fiellin DA (2017). The Starting Treatment for Ethanol in Primary Care Trials (STEPTrials): Protocol for three parallel multi-site stepped care effectiveness studies for unhealthy alcohol use in HIV-positive patients. Contemporary Clinical Trials, 52, 80–90. doi: 10.1016/j.cct.2016.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Moore BA, Holt SR, Hansen N, Kyriakides TC, Virata M, … Fiellin LE (2018). Efficacy of extended-release naltrexone on HIV-related and drinking outcomes among HIV-positive patients: A randomized-controlled trial. AIDS and Behavior. doi: 10.1007/10461-018-2241-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott JC, Aharonovich E, O’Leary A, Johnston B, & Hasin DS (2014). Perceived medical risks of drinking, alcohol consumption, and hepatitis Cstatus among heavily drinking HIVprimary care patients. Alcohol Clinical and Experimental Research, 38(12), 3052–3059. doi: 10.1111/acer.12570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farahani M, Mulinder H, Farahani A, & Marlink R (2017). Prevalence and distribution of non-AIDS causes of death among HIV-infected individuals receiving antiretroviral therapy: A systematic review and meta-analysis. International Journal of STD & AIDS, 28(7), 636–650. doi: 10.1177/0956462416632428 [DOI] [PubMed] [Google Scholar]
- Fiellin DA, Pantalon MV, Chawarski MC, Moore BA, Sullivan LE, O’Connor PG, & Schottenfeld RS (2006). Counseling plus buprenorphine-naloxone maintenance therapy for opioid dependence. New England Journal of Medicine, 355(4), 365–374. doi: 10.1056/NEJMoa055255 [DOI] [PubMed] [Google Scholar]
- Fleming MF, Barry KL, Manwell LB, Johnson K, & London R (1997). Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. Journal of the American Medical Association, 277(13), 1039–1045. [PubMed] [Google Scholar]
- Fultz SL, Justice AC, Butt AA, Rabeneck L, Weissman S, Rodriguez-Barradas M, & Team V-P (2003). Testing, referral, and treatment patterns for hepatitis Cvirus coinfection in a cohort of veterans with human immunodeficiency virus infection. Clinical Infectious Diseases, 36(8), 1039–1046. doi: 10.1086/374049 [DOI] [PubMed] [Google Scholar]
- Fuster D, & Samet JH (2018). Alcohol use in patients with chronic liver disease. New England Journal of Medicine, 379(13), 1251–1261. doi: 10.1056/NEJMra1715733 [DOI] [PubMed] [Google Scholar]
- Hasin DS, Aharonovich E, O’Leary A, Greenstein E, Pavlicova M, Arunajadai S, … Johnston B (2013). Reducing heavy drinking in HIVprimary care: A randomized trial of brief intervention, with and without technological enhancement. Addiction, 108(7), 1230–1240. doi: 10.1111/add.12127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2005). Improving the quality of health care for mental and substance-use conditions Quality Chasm Series. Washington, D.C. [Google Scholar]
- Jonas DE, Amick HR, Feltner C, Bobashev G, Thomas K, Wines R, … Garbutt JC (2014). Pharmacotherapy for adults with alcohol use disorders in outpatient settings: A systematic review and meta-analysis. Journal of the American Medical Association, 311(18), 1889–1900. doi: 10.1001/jama.2014.3628 [DOI] [PubMed] [Google Scholar]
- Justice AC, McGinnis KA, Tate JP, Braithwaite RS, Bryant KJ, Cook RL, … Fiellin DA (2016). Risk of mortality and physiologic injury evident with lower alcohol exposure among HIVinfected compared with uninfected men. Drug and Alcohol Dependence, 161, 95–103. doi: 10.1016/j.drugalcdep.2016.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Pantalone DW, Mastroleo NR, Liu T, Bove G, Ramratnam B, … Mayer KH (2018). Motivational interviewing with personalized feedback to reduce alcohol use in HIV-infected men who have sex with men: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 86(8), 645–656. doi: 10.1037/ccp0000322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A, Tansel A, White DL, Kayani WT, Bano S, Lindsay J, … Kanwal F (2016). Efficacy of psychosocial interventions in inducing and maintaining alcohol abstinence in patients with chronic liver disease: A systematic review. Clinical Gastroenterology and Hepatology, 14(2), 191–202 e191–194; quiz e120. doi: 10.1016/j.cgh.2015.07.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korthuis PT, Lum PJ, Vergara-Rodriguez P, Ahamad K, Wood E, Kunkel LE, … Investigators, C.-C. (2017). Feasibility and safety of extended-release naltrexone treatment of opioid and alcohol use disorder in HIV clinics: A pilot/feasibility randomized trial. Addiction. doi: 10.1111/add.13753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim JK, Tate JP, Fultz SL, Goulet JL, Conigliaro J, Bryant KJ, … Lo Re V 3rd. (2014). Relationship between alcohol use categories and noninvasive markers of advanced hepatic fibrosis in HIV-infected, chronic hepatitis Cvirus-infected, and uninfected patients. Clinical Infectious Diseases. doi: ciu097 [pii] 10.1093/cid/ciu097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, & Kelley ME (2001). Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. Journal of Studies on Alcohol, 62(5), 605–614. [DOI] [PubMed] [Google Scholar]
- Marcus JL, Hurley LB, Chamberland S, Champsi JH, Gittleman LC, Korn DG, … Silverberg MJ (2018). Disparities in initiation of direct-acting antiviral agents for hepatitis Cvirus infection in an insured population. Public Health Reports, 133(4), 452–460. doi: 10.1177/0033354918772059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis KA, Fultz SL, Skanderson M, Conigliaro J, Bryant K, & Justice AC (2006). Hepatocellular carcinoma and non-Hodgkin’s lymphoma: The roles of HIV, hepatitis Cinfection, and alcohol abuse. Journal of Clinical Oncology, 24(31), 5005–5009. doi: 10.1200/JCO.2006.05.7984 [DOI] [PubMed] [Google Scholar]
- Nadkarni PM, Brandt C, Frawley S, Sayward FG, Einbinder R, Zelterman D, … Miller PL (1998). Managing attribute--value clinical trials data using the ACT/DBclient-server database system. Journal of the American Medical Informatics Association, 5(2), 139–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. What’s “at-risk” or “heavy” drinking? Retrieved 7.18, 2011, from http://rethinkingdrinking.niaaa.nih.gov/IsYourDrinkingPatternRisky/WhatsAtRiskOrHeavyDrinking.asp
- Proeschold-Bell RJ, Evon DM, Makarushka C, Wong JB, Datta SK, Yao J, … Muir AJ (2018). The Hepatitis C-Alcohol Reduction Treatment (HepART) intervention: Study protocol of a multi-center randomized controlled trial. Contemporary Clinical Trials, 72, 73–85. doi: 10.1016/j.cct.2018.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA-HRSA Center for Integrated Health Solutions. Retrieved 3.19.2018, from https://www.integration.samhsa.gov/
- Sims OT, Maynard QR, & Melton PA (2016). Behavioral interventions to reduce alcohol use among patients with hepatitisC: A systematic review. Social Work in Public Health, 31(6), 565–573. doi: 10.1080/19371918.2016.1160346 [DOI] [PubMed] [Google Scholar]
- Singal AK, Bataller R, Ahn J, Kamath PS, & Shah VH (2018). ACG clinical guideline: Alcoholic liver disease. American Journal of Gastroenterology, 113(2), 175–194. doi: 10.1038/ajg.2017.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, & Sobell SM (1996). Alcohol TimelineFollowback (TLFB); Handbook of Psychiatric Measures. Washington, D.C. : American Psychiatric Association. [Google Scholar]
- Sobell MB, & Sobell LC (2000). Stepped care as a heuristic approach to the treatment of alcohol problems. Journal of Consulting and Clinical Psychology, 68(4), 573–579. [PubMed] [Google Scholar]
- Soyka M, & Lieb M (2015). Recent developments in pharmacotherapy of alcoholism. Pharmacopsychiatry, 48(4-5), 123–135. doi: 10.1055/s-0035-1547237 [DOI] [PubMed] [Google Scholar]
- Springer SA, Di Paola A, Azar MM, Barbour R, Krishnan A, & Altice FL (2017). Extended-release naltrexone reduces alcohol consumption among released prisoners with HIVdisease as they transition to the community. Drug and Alcohol Dependence, 174, 158–170. doi: 10.1016/j.drugalcdep.2017.01.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner J, … Investigators, A. C. (2006). Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCVcoinfection. Hepatology, 43(6), 1317–1325. doi: 10.1002/hep.21178 [DOI] [PubMed] [Google Scholar]
- Tetrault JM, Moore BA, Barry DT, O’Connor PG, Schottenfeld R, Fiellin DA, & Fiellin LE (2012). Brief versus extended counseling along with buprenorphine/naloxone for HIV-infected opioid dependent patients. Journal of Substance Abuse Treatment, 43(4), 433–439. doi: 10.1016/j.jsat.2012.07.011 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veteran Affairs. (2011). Alcohol misuse: Primary care of veterans withHIV. Retrieved from https://www.hiv.va.gov/provider/manual-primary-care/alcohol-misuse.asp.
- van Straten A, Hill J, Richards DA, & Cuijpers P (2015). Stepped care treatment delivery for depression: A systematic review and meta-analysis. Psychological Medicine, 45(2), 231–246. doi: 10.1017/S0033291714000701 [DOI] [PubMed] [Google Scholar]
- Williams EC, McGinnis KA, Edelman EJ, Matson TE, Gordon AJ, Marshall BDL, … Bradley KA (2018). Level of alcohol use associated with HIVcare continuum targets in a national US. Sample of persons living with HIVreceiving healthcare. AIDS and Behavior. doi: 10.1007/s10461-018-2210-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Finney JW, Harris AH, Kivlahan DR, & Kranzler HR (2015). Recommendations for the design and analysis of treatment trials for alcohol use disorders. Alcoholism: Clinical and Experimental Research, 39(9), 1557–1570. doi: 10.1111/acer.12800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization.HIV/AIDS: HIV and hepatitis coinfections.
- Wurst FM, Thon N, Yegles M, Schruck A, Preuss UW, & Weinmann W (2015). Ethanol metabolites: Their role in the assessment of alcohol intake. Alcoholism: Clinical and Experimental Research. doi: 10.1111/acer.12851 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


