Abstract
Studies of firefighters have shown increased exposures to carcinogenic compounds and elevated rates of certain cancers compared to the general population, yet this research has focused almost exclusively on men. To address this gap, the Women Firefighters Biomonitoring Collaborative created a biological sample archive and analyzed levels of perfluoroalkyl substances (PFAS) among women firefighters (N=86) and office workers (N=84) in San Francisco. Serum samples were collected and analyzed using liquid chromatography tandem mass spectrometry (LC MS/MS) to measure and compare PFAS levels between firefighters and office workers. Seven of twelve PFAS congeners were detected in least 70% of the study population, and four congeners were detected in 100% of participants. In regression models comparing PFAS levels by occupation and adjusting for potential confounders, firefighters had higher geometric mean concentrations of PFAS compared to office workers PFHxS (2.22 (95%CI = 1.55,3.18)), PFUnDA (1.83 (95% CI = 0.97,3.45)) and PFNA 1.26 (95% CI = 1.01, 1.58)). Among firefighters, occupational position predicted exposure—firefighters and officers had higher PFNA, PFOA, PFDA, and PFUnDA levels compared to drivers. Women firefighters are exposed to higher levels of some PFAS compared to office workers, suggesting that some of these exposures may be occupationally related.
Introduction
Firefighters have higher rates of some cancers compared to the general population. A meta-analysis of 32 studies found elevated rates of lymphoma, testicular, and prostate cancer among male firefighters.1 Additionally, a review by the International Agency for Research on Cancer (IARC) found increased cancer rates among firefighters, and designated the occupation of firefighting as “possibly carcinogenic” or “class 2b”.2 More recently, a study of over 19,000 United States firefighters conducted by the National Institute for Occupational Health and Safety (NIOSH) found that total time spent at fires was associated with increased lung cancer incidence and mortality, and total number of fire responses was associated with leukemia mortality.3 Furthermore, studies in other countries have found increased rates of several cancers among male firefighters and other first responders including brain, thyroid, bladder, kidney, prostate, testicular, breast, digestive cancers, multiple myeloma, and non-Hodgkin’s lymphoma.4–10 Despite mounting concern about cancer among male firefighters, few studies have assessed chemical exposures or cancer risk among women firefighters, many of whom are concerned about the potential increased risk of breast cancer and other reproductive cancers. Only two studies have examined the incidence of cancer among women firefighters. Daniels et al. found that women firefighters had higher incidence and mortality rates of breast cancer compared to the general US population, though neither effect estimate was statistically significant.11 A study of Florida firefighters found that women firefighters had an increase in overall cancer risk and, in particular, an increased incidence of Hodgkin’s disease and cervical and thyroid cancers compared to the general Florida population.9
Occupational exposures may be an important contributor to the increased risk of cancer among firefighters. Firefighters’ exposure to environmental chemicals may arise from fire suppression activities and during the salvage and overhaul phase of a fire event.12–16 Additionally, hazardous chemicals have been identified in fire station dust, firefighting foams, diesel emissions, contaminated fire equipment and firefighter protective gear.17–21 Previous studies have shown that firefighters are occupationally exposed to polycyclic aromatic hydrocarbons,14,22–25 formaldehyde, dioxins, polybrominated diphenyl eithers (PBDEs), organophosphate flame retardants,26,27 and perfluoroalkyl substances (PFAS),20,26,28,29 among others.26,30,31 Many of these chemicals have been associated with adverse health outcomes including breast cancer and breast tumor development in both animal and human studies.32,33
PFAS may be of particular relevance to firefighting because these compounds are used in turnout gear and are a major ingredient of some firefighting foams, such as aqueous film-forming foams (AFFF).20,29,34 More generally, PFAS chemicals are frequently applied to food contact paper, fabrics and furniture to make them stain, water and grease resistant.35 PFAS have long half-lives and bioaccumulate in the environment and human body.36 Because of their widespread use and persistence, they have been detected in nearly everyone tested in large biomonitoring studies.37,38 Biomonitoring studies within the National Health and Nutrition Examination Survey (NHANES), a nationally representative sample of the U.S. population, have found that more than 98% of people tested had multiple congeners of PFAS detected in their bodies.37
PFAS exposure has been linked to multiple adverse health outcomes including cancer, immune suppression, thyroid and sex hormone disruption, and decreased semen quality.39–42 Studies also indicate that exposure is associated with metabolic effects, ulcerative colitis and adverse effects on liver and kidney function.43–46
Several firefighter biomonitoring studies measured PFAS levels and found higher levels among firefighters compared to the general population.26,28,29 These studies, however, included few or no women. Overall, women remain underrepresented in studies of firefighters, and very little is known about the extent of their chemical exposures or occupational health risks for diseases such breast cancer.
Although women make up 5.1% of firefighters across the United States,47 their numbers can be higher in urban jurisdictions, including in San Francisco, which has one of the highest proportions of women firefighters (15%) of any large urban fire department in the U.S.48 As fire departments and other first responder professions diversify and recruit more women to their ranks, it is important to characterize chemical exposures and implications for health outcomes of particular relevance to women, such as breast cancer. To address this data gap, a partnership of firefighters, environmental health scientists, and environmental health advocates created the Women Firefighters Biomonitoring Collaborative (WFBC). The WFBC is a community-based, participatory biomonitoring project that aims to better understand how women firefighters are exposed to potential breast carcinogens, while also developing a biospecimen archive of women firefighters and office workers in San Francisco. As part of the WFBC, we conducted a cross-sectional chemical biomonitoring study to compare levels of PFAS in human serum collected from women firefighters from the San Francisco Fire Department (SFFD) and non-firefighter women who are office workers for the City and County of San Francisco. To our knowledge, this is the first biomonitoring study to measure environmental chemical exposures in an exclusively female cohort of firefighters and office workers.
Methods
Recruitment
Participant recruitment and sample collection took place between June 2014 and March 2015. Firefighter partners of the WFBC assisted with recruitment of both firefighter and office worker participants. To recruit firefighters, members of the United Fire Service Women (UFSW), the San Francisco Firefighters Cancer Prevention Foundation (SFFCPF) and the International Association of Firefighters--Local 798 sent out announcements through their listservs and newsletters. Firefighter members of the WFBC and study staff held informational meetings at firehouses and one-on-one to describe the study to potential participants. In addition, the SFFD supported recruitment efforts by sending material through the department listserv and publishing an article about the study in the “The Mainline,” a department newsletter written and edited by both active and retired firefighters. Similarly, office workers, who were non-first responder employees of the City and County of San Francisco, were recruited at city offices via public meetings led by WFBC firefighters and study staff, tabling at health fairs, and through listserv emails targeting employees of the City and County of San Francisco.
Study inclusion criteria for both firefighters and office workers included being female, over 18 years old, a full-time employee, and a non-smoker. In addition, firefighters needed to have at least five years of service with the SFFD and currently be on “active duty” (i.e. assigned to a fire station) at the time of recruitment. All participants were consented into the study following protocols approved by the Institutional Review Board of the University of California, Berkeley (# 2013–07-5512).
Exposure assessment interview
After consent and enrollment into the WFBC study, we conducted an hour-long in-person exposure assessment interview with each participant. The interview captured demographic information, basic health information, and possible sources of PFAS exposure from occupational activities, consumer product use, and dietary factors that prior literature indicates are potential sources of PFAS exposure.28,49,50 Food frequency responses were converted to times per week and categorized into quartiles, tertiles, or ever/never.
Sample collection and processing
Blood samples were collected by a certified phlebotomist in 40 mL additive-free glass tubes and transported in a cooler with ice for processing within 3 hours of collection. Serum was separated by allowing clotting at room temperature, then centrifuging at 3000 rpm for 10 minutes. Serum was aliquoted into 1.2 mL cryo-vial tubes and stored at −80 oC until analysis per standard protocols.51 All samples were processed and analyzed at the University of California, San Francisco.
Laboratory analysis
Twelve PFAS (perfluorobutane sulfonic acid, PFBS; perfluorohexane sulfonic acid, PFHxS; perfluoroheptanoic acid, PFHpA; perfluorooctanoic acid, PFOA; perfluorooctane sulfonic acid, PFOS; perfluorooctane sulfonamide, PFOSA; perfluorononanoic acid, PFNA; perfluorodecanoic acid, PFDA; perfluoroundecanoic acid, PFUnDA; perfluorododecanoic acid, PFDoA; perfluorobutanoic acid, PFBA; perfluorohexanoic acid, PFHxA) were selected for analysis. The first ten PFAS of this list were selected because they are also monitored in the NHANES so levels in our study can be compared with those in the US general population52. The final two PFAS (PFBA and PFHxA) are not currently biomonitored and were included in the study because they are produced and used in the US and because their structural similarity to the other commonly-detected PFAS suggests they may have similar health effects.53 Congeners were analyzed in each serum sample (0.5 mL) using liquid chromatography- tandem mass spectrometry (LC-MS/MS). An Agilent LC1260 (Sta. Clara, CA)- AB Sciex API 5500 (Foster City, CA) platform was used in the analysis. Prior to injection into the LC-MS/MS, each sample was prepared for analysis by solid phase extraction using a Waters Oasis HLB cartridge (10 mg, 1cc). Extracted aliquots of each sample (25uL) were run in duplicates. The twelve analytes were separated by elution gradient chromatography using Phenomenex Kinetex C18 column (100 × 4.6 mm, 2.6μ) at 40ºC. An electrospray ionization source operated in the negative mode was used to ionize each analyte in the mass spectrometer.
Analytes were detected in each sample by multiple reaction monitoring using two transitions per analyte. To determine the presence of each analyte retention matching (within 0.15 min) along with the peak area ratio between its qualifier and quantifier ions (within 20%) were used. Quantification of each detected analyte was done by isotope dilution method using a 10-point calibration curve (0.02–50 ng/mL) and employing two C13-labelled PFAS isotopologues. The limits of quantification for the twelve analytes range from 0.05 to 0.1 ng/mL. Analyte identification from total ion chromatograms was evaluated using AB Sciex Analyst v2.1 software while quantification of each analyte was processed using AB Sciex MultiQuant v2.02 software. Analysts were blinded to firefighter and office worker status of the serum samples during the analysis. Results were reported in ng/mL for all 170 study participants.
Statistical analysis
We examined the distribution of each PFAS congener across the study population and then separately for firefighters and office workers and calculated summary statistics including geometric mean (GM), 95% confidence intervals (CI), and percentiles. As is common with environmental data, PFAS concentrations were non-normally distributed, thus we used non-parametric methods (Wilcoxon rank-sum test) to test unadjusted differences in PFAS concentrations between firefighters and office workers. We used lognormal regression analyses to assess differences in PFAS concentrations between firefighters and office workers, controlling for potential confounders. We then limited the analysis to firefighters and used lognormal regression analyses to explore the association between firefighter occupational activities and PFAS concentrations controlling for potential confounders. Congeners with at least a 70% detection frequency were included in the data analysis and we used maximum likelihood estimation (MLE) with the NADA R package to account for left censored data (data below the limit of detection (LOD)) for all regression models.54
Potential confounders were identified a priori based on previous literature suggesting an independent relationship with PFAS levels. We assessed the relationship between each identified variable and PFAS levels in our data and tested differences between firefighters and office workers for each potential confounder associated. Variables were included in final regression models if there was a statistically significant association with PFAS levels in our data and if the variable demonstrated a statistically significant difference between firefighters and office workers (p-value ≤ 0.05) for at least one PFAS congener.
We ran linear regression models to test the association between occupation and log-transformed PFAS concentrations controlling for age, race and ethnicity, and education (Model 1). A second model controlled for variables in Model 1 as well as consumption frequency of fish and shellfish, red meat, poultry, fast-food or take-out food, and frozen food heated in paper or cardboard packaging (Model 2). Exponentiated beta coefficients estimate the proportional change in the PFAS geometric means associated with being a firefighter compared to being an office worker and controlling for potential confounders.
We then limited our analysis to firefighters to evaluate the association between firefighter practices in the workplace with PFAS levels adjusting for age, race and ethnicity, and number of years of service with SFFD. Firefighter practices assessed included use of self-contained breathing apparatus (SCBA) during salvage and overhaul, use of firefighting foam in the year prior to sample collection, and the participants’ assigned position at the time of the questionnaire (firefighter, officer, driver). Likewise, because airport fire stations are required to stock, test and use PFAS-containing firefighting foam due to federal regulations, we included an indicator variable for those firefighters assigned to San Francisco Airport fire stations at the time of study.55 We also examined the relationship between PFAS concentrations and the frequency of handwashing during a work shift and showering after a fire event, as well as the relationship with responding to a fire within 24 hours and one year prior to providing a biospecimen sample. Again, we exponentiated the beta coefficient to obtain the proportional change in the PFAS geometric means associated with a unit change of each independent variable controlling for potential confounders.
Lastly, we evaluated how PFAS levels in our study population compared with those measured in the general U.S. population and in firefighters in Southern California. Specifically, we plotted the geometric mean (GM) and 95% confidence interval from the WFBC firefighter and office worker groups and compared them to adult women from the 2013–2014 cycle of the National Health and Nutrition Examination Survey (NHANES) and the Firefighter Occupational Exposure (FOX) study, in which samples were collected from a cohort of mostly male firefighters in Southern California between 2010 and 2011 (N=101).28,52,56 WFBC firefighter and office worker levels below the LOD were replaced by the LOD reported for each congener divided by √2 to facilitate comparison of our results to the FOX and NHANES cohorts, which also used this approach (LOD/√2).
All analyses were performed in R version 3.5.2 and R Studio 1.2.1335.57,58
Results
176 participants were recruited into the study. Six individuals, (three firefighters and three office workers) met the study inclusion criteria and were interviewed but did not provide a blood sample and therefore were excluded from the analysis. Our final study sample consisted of 86 firefighters and 84 office workers (N=170) (Table 1).
Table 1.
Demographic characteristics of firefighters and office workers in the Women Firefighters Biomonitoring Collaborative (2014–2015)
| Variables: mean ± SD or N(%) | Firefighters N=86 | Office workers N=84 | P-valuea |
|---|---|---|---|
| Age (years) | 47.5 (±4.6) | 48.3 (±10.5) | 0.38 |
| Years working for SFFD or SF City & County | 17.4 (±4.2) | 14.2 (±10.1) | 0.0005 |
| U.S. Born | 77 (89.5%) | 62 (73.8%) | 0.01 |
| Race/ethnicity | |||
| NH White | 40 (46.5%) | 37 (44.0%) | 0.29 |
| Latina/Hispanic | 19 (22.1%) | 13 (15.5%) | |
| NH Asian | 11 (12.8%) | 19 (22.6%) | |
| NH Black | 9 (10.5%) | 5 (6.0%) | |
| NH Other | 7 (8.1%) | 10 (11.9%) | |
| Last grade completed | |||
| Some college or less | 48 (55.8%) | 15 (17.9%) | < 0.0001 |
| Bachelors or higher | 38 (44.2%) | 69 (82.1%) | |
| Marital status | |||
| Married | 37 (43.0%) | 47 (56.0%) | 0.039 |
| Widowed | 1 (1.2%) | 2 (2.4%) | |
| Separated/Divorced | 26 (30.2%) | 11 (13.1%) | |
| Never married | 22 (25.6%) | 24 (28.6%) | |
| Reported yes, ever been pregnant | 60 (70.6%) | 52 (61.9%) | 0.26 |
| Body mass indexb | |||
| Healthy weight | 33 (40.7%) | 43 (52.4%) | 0.13 |
| Overweight | 35 (43.2%) | 23 (28.0%) | |
| Obese | 13 (16.0%) | 16 (19.5%) |
NH = Non-Hispanic
To account for non-normally distributed variables we used Wilcoxon Rank Sum test to compare continuous variables by firefighter status and the Fisher Test for categorical variables.
CDC guidelines for BMI classification (lb/in2): Healthy weight 18.5–24.9; Overweight 25.0–29.9, Obese >30
Firefighters and office workers had similar demographic characteristics in terms of age, and racial/ethnic make-up, while a significantly higher proportion of office workers were foreign-born, married, and had higher levels of educational attainment. Firefighters had an average of seventeen years of service with the SFFD while office workers had an average of fourteen years of service with the City and County of San Francisco.
Occupational activities and characteristics of the firefighter group are shown in Table 2. The majority of participants were assigned to the position of firefighter compared to officer or driver positions, and fourteen firefighters were assigned to one of the San Francisco airport fire stations. Twenty-five firefighters reported using firefighting foam in the year prior to the sample collection and when asked about the class of foam they used, most participants reported using Class A or both Class A and B foams. Over half of participants reported rarely using their SCBA during salvage and overhaul activities after a fire. When asked about recent fires, most firefighters had not responded to a fire or participated in live-fire training in the 24 hours prior to their biospecimen sample collection, while the SFFD fire history data indicated that most firefighters had ten or more fires in the year prior to biospecimen collection.
Table 2.
Occupational characteristics for WFBC firefighters 2014–15 (N = 86)
| Variables | Mean(±SD) or N(%) |
|---|---|
| Frequency of handwashing while at work (times/shift) | 18.8 (±12.5) |
| Frequency of handwashing while not at work (times/day) | 10.3 (±5.3) |
| Reported using firefighting foam in the past year | 25 (29.1%) |
| Class of firefighting foam used (ever)a | |
| Class A only | 39 (45.3%) |
| Class B only | 6 (7.0%) |
| Class A & B | 28 (32.6%) |
| Assigned to airport fire station | 14 (16.3%) |
| Response to fire in last 24 hoursb | 15 (17.4%) |
| Number of fires responded to in year prior to sample collection (N = 66)c | |
| ≤9 | 17 (25.8%) |
| 10–15 | 17 (25.8%) |
| 16–19 | 15 (22.7%) |
| ≥20 | 17 (25.8%) |
| Assignment in the SFFD | |
| Driver | 21 (24.4%) |
| Officer | 25 (29.1%) |
| Firefighter | 40 (46.5%) |
| Used self-contained breathing apparatus (SCBA) during salvage/overhauld | |
| Always/often | 12 (15.0%) |
| Sometimes | 14 (17.5%) |
| Rarely/never | 54 (67.5%) |
Missing data on class of foam used for 13 firefighters.
Includes fire response and training involving live fires
Includes firefighters who consented to give access to SFFD fire history records (n = 66)
Six firefighters reported ‘do not participate’ in salvage/overhaul.
Perfluoroalkyl substance exposures
Table 3 shows the LOD, detection frequency, GM (95%CI), and percentiles of each PFAS compound analyzed. Of the twelve PFAS we measured in participants’ serum, four congeners were not detected in any of the study participants (PFBA, PFHxA, PFHpA, PFOSA). Eight PFAS had measurable levels, seven of which were detected in at least 70% of study participants and four were detected in 100% of study participants (PFHxS, PFNA, PFOA, and PFOS). We excluded PFDoA from further analyses since it was detected in fewer than 25% of study participants. Distributional comparisons of PFAS levels between WFBC firefighters and office workers for those compounds with detection frequencies of at least 70% are shown in Figure S1. Levels of PFNA, PFHxS and PFUnDA were statistically significantly higher among the firefighter group compared to office workers.
Table 3.
Geometric mean (GM) and 95% confidence interval (CI), detection frequency (DF), level of detection (LOD) (ng/mL) and percentilesa for each PFAS analyzed in the WFBC cohort.
| Percentiles |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Compound Name | abbr. | DF % | LOD | GM (95% CI) | Min | Max | 25th | 50th | 75th | 95th |
| perfluorohexane sulfonic acid | PFHxS | 100 | 0.02 | 3.79 (3.24, 4.43) | 0.22 | 90.57 | 1.87 | 3.04 | 6.79 | 22.28 |
| perfluorooctanoic acid | PFOA | 100 | 0.02 | 1.15 (1.05, 1.25) | 0.29 | 5.18 | 0.83 | 1.11 | 1.56 | 3.22 |
| perfluorooctane sulfonic acid | PFOS | 100 | 0.02 | 4.11 (3.68, 4.59) | 0.54 | 81.02 | 2.56 | 4.14 | 6.53 | 12.61 |
| perfluorononanoic acid | PFNA | 100 | 0.05 | 0.67 (0.61, 0.74) | 0.15 | 4.49 | 0.42 | 0.64 | 1.03 | 2.2 |
| perfluorodecanoic acid | PFDA | 98 | 0.02 | 0.25 (0.23, 0.28) | <LOD | 3.69 | 0.17 | 0.24 | 0.36 | 0.83 |
| perfluoroundecanoic acid | PFUnDA | 80 | 0.02 | 0.18 (0.14, 0.22) | <LOD | 10.85 | 0.11 | 0.26 | 0.48 | 1.11 |
| perfluorobutane sulfonic acid | PFBS | 73 | 0.02 | 0.13 (0.10,0.16) | <LOD | 1.45 | <LOD | 0.23 | 0.34 | 0.84 |
| perfluorododecanoic acid | PBDoA | 24 | 0.02 | * | <LOD | 1.73 | <LOD | <LOD | <LOD | 0.3 |
| perfluorobutanoic acid | PFBA | 0 | 0.05 | * | <LOD | <LOD | <LOD | <LOD | <LOD | <LOD |
| perfluorhexanoic acid | PFHxA | 0 | 0.02 | * | <LOD | <LOD | <LOD | <LOD | <LOD | <LOD |
| perfluorheptanoic acid | PFHpA | 0 | 0.02 | * | <LOD | <LOD | <LOD | <LOD | <LOD | <LOD |
| perfluorooctane sulfonamide | PFOSA | 0 | 0.02 | * | <LOD | <LOD | <LOD | <LOD | <LOD | <LOD |
Percentiles and summary statistics calculated using LOD/sqrt2 for those with less than 100% detection frequency.
GM and 95%CI not calculated for PFAS with less than 70% DF
Table 4 shows the results from multiple linear regression models assessing the relationship between log-transformed PFAS concentrations and occupation, comparing firefighters to office workers (referent) controlling for potential confounders (Tables S1 and S2). Multiple regression models found higher serum levels of PFHxS, PFUnDA and PFNA among firefighters compared to office workers in both unadjusted in adjusted models. PFHxS levels were 2.22 (95%CI = 1.55, 3.18,) times higher, PFUnDA levels were 1.83 (95%CI = 0.97, 3.45) times higher and PFNA levels were 1.26 (95%CI = 1.01, 1.58) times higher in firefighters compared to office workers after adjusting for age, race and ethnicity, and education, as well as the frequency of consumption of fish/shellfish, red meat, poultry, fast-food, food heated in packaging.
Table 4.
Unadjusted and adjusteda,b proportional change in geometric mean (95% confidence interval) of PFAS concentrations by firefighter status (office worker as referent), from maximum likelihood estimation (MLE) models
| model | βCoef | expβ (95% CI) | p-value |
|---|---|---|---|
| Perfluorononanoic Acid PFNA | |||
| unadjusted | 0.23 | 1.25 (1.03, 1.53) | 0.0245 |
| model 1a | 0.22 | 1.25 (1.01, 1.54) | 0.0369 |
| model 2b | 0.23 | 1.26 (1.01, 1.58) | 0.0399 |
| Perfluorooctanoic Acid PFOA | |||
| unadjusted | −0.04 | 0.96 (0.81, 1.13) | 0.6070 |
| model 1a | −0.02 | 0.98 (0.83, 1.18) | 0.8666 |
| model 2b | 0.07 | 1.07 (0.89, 1.30) | 0.4730 |
| Perfluorooctanoic Sulfonate PFOS | |||
| unadjusted | 0.09 | 1.10 (0.88, 1.36) | 0.4097 |
| model 1a | 0.15 | 1.16 (0.93, 1.45) | 0.1887 |
| model 2b | 0.10 | 1.10 (0.87, 1.40) | 0.4334 |
| Perfluorohexane Sulfonate PFHxS | |||
| unadjusted | 0.43 | 1.54 (1.14, 2.07) | 0.0051 |
| model 1a | 0.57 | 1.77 (1.29, 2.43) | 0.0004 |
| model 2b | 0.80 | 2.22 (1.55, 3.18) | 0.0000 |
| Perfluordecanoic Acid PFDA | |||
| unadjusted | 0.13 | 1.14 (0.92, 1.43) | 0.2324 |
| model 1a | 0.09 | 1.10 (0.87, 1.39) | 0.4420 |
| model 2b | 0.14 | 1.15 (0.89, 1.49) | 0.2947 |
| Perfluorbutane Sulfonate PFBS | |||
| unadjusted | 0.17 | 1.19 (0.65, 2.18) | 0.5731 |
| model 1a | 0.30 | 1.35 (0.70, 2.59) | 0.3710 |
| model 2b | 0.36 | 1.43 (0.71, 2.91) | 0.3192 |
| Perfluoroundecanoic Acid PFUnDA | |||
| unadjusted | 0.55 | 1.74 (1.00, 3.02) | 0.0496 |
| model 1a | 0.48 | 1.61 (0.88, 2.97) | 0.1236 |
| model 2b | 0.60 | 1.83 (0.97, 3.45) | 0.0623 |
model 1 adjusted for: age, race/ethnicity and education.
model 2 adjusted for covariates in model 1 and consumption of: fish/shellfish, red meat, poultry, fastfood or takeout food, frozen food heated in paper or cardboard package. Office worker is referent group.
When limiting our analysis to firefighters, we found that assigned firefighter position was associated with higher levels of five of the seven PFAS (Table 5). Having the occupational position of firefighter or officer (versus driver) was associated with higher average serum levels of PFNA, PFOA, PFOS, PFDA and PFUnDA, while drivers had higher average levels of PFBS compared to those in officer and firefighter positions. Firefighters assigned to the airport had higher levels of PFNA than those assigned to other stations in the fire department. Likewise, firefighters who reported using firefighting foam in the year prior to the sample collection had elevated levels of several PFAS compared to those who reported not using foam in the past year.
Table 5.
Adjusted proportional change in geometric mean (GM) of covariates (95% CI) and serum PFAS concentration among firefighters from Maximum Likelihood Regression (MLE) modelsa
| Variable | n | PFNA | PFOA | PFOS | PFHxS | PFDA | PFBS | PFUnDA |
|---|---|---|---|---|---|---|---|---|
| Frequency of SCBA use during salvage/overhaul | ||||||||
| Rarely/ never | 54 | reference | reference | reference | reference | reference | reference | reference |
| Sometimes | 14 | 1.90 (1.25,2.87)† | 1.19 (0.86,1.64) | 1.29 (0.88,1.89) | 0.75 (0.39,1.47) | 1.44 (1.02,2.04)† | 0.83 (0.25, 2.79) | 3.64 (1.41,9.39)† |
| Often/ always | 12 | 1.47 (0.99,2.18)* | 0.99 (0.73,1.35) | 0.88 (0.61,1.27) | 0.59 (0.31,1.12) | 1.17 (0.84,1.63) | 0.46 (0.15, 1.48) | 1.12 (0.45,2.79) |
| Used firefighting foam in the last year | ||||||||
| No | 50 | reference | reference | reference | reference | reference | reference | reference |
| Yes | 25 | 1.29 (0.94,1.79) | 1.10 (0.86,1.39) | 1.19 (0.92,1.54) | 1.26 (0.79,2.00) | 1.08 (0.82,1.41) | 1.64 (0.64, 4.18) | 1.23 (0.59,2.56) |
| Position in the fire department | ||||||||
| Driver | 21 | reference | reference | reference | reference | reference | reference | reference |
| Officer | 25 | 1.61 (1.13,2.29)† | 1.42 (1.07,1.90)† | 1.25 (0.90,1.74) | 0.98 (0.53,1.79) | 1.45 (1.05,2.00)† | 0.27 (0.09, 0.78)† | 3.18 (1.34,7.51)† |
| Firefighter | 40 | 2.12 (1.54,2.93)‡ | 1.42 (1.09,1.85)† | 1.26 (0.93,1.70) | 0.91 (0.53,1.58) | 1.47 (1.10,1.97)† | 0.54 (0.21, 1.41) | 1.99 (0.91,4.36)† |
| Frequency of hand washing during a 24hr work shift (times/shift) | ||||||||
| <=10 | 21 | reference | reference | reference | reference | reference | reference | reference |
| 11–15 | 24 | 0.92 (0.62,1.36) | 0.90 (0.66,1.22) | 0.87 (0.63,1.20) | 1.83 (1.03,3.23)† | 1.08 (0.77,1.51) | 0.81 (0.27, 2.43) | 0.50 (0.20,1.22) |
| 16–20 | 20 | 1.02 (0.68,1.53) | 0.99 (0.72,1.36) | 1.20 (0.86,1.67) | 2.90 (1.61,5.23)‡ | 0.90 (0.63,1.27) | 0.77 (0.25, 2.40) | 0.65 (0.26,1.64) |
| >20 | 21 | 0.70 (0.46,1.06)* | 0.95 (0.69,1.30) | 0.74 (0.53,1.03)* | 1.42 (0.78,2.58) | 0.76 (0.53,1.07) | 2.13 (0.68, 6.62) | 0.59 (0.23,1.50) |
| Frequency of washing and/or showering after an incident | ||||||||
| Sometimes | 11 | reference | reference | reference | reference | reference | reference | reference |
| Always | 75 | 0.79 (0.50,1.26) | 0.98 (0.69,1.40) | 0.91 (0.62,1.35) | 2.08 (1.04,4.15)† | 1.01 (0.68,1.49) | 0.52 (0.15, 1.83) | 0.89 (0.32,2.52) |
| Assigned to the Airport | ||||||||
| No | 72 | reference | reference | reference | reference | reference | reference | reference |
| Yes | 14 | 2.26 (1.61,3.19)‡ | 1.00 (0.75,1.35) | 1.03 (0.74,1.42) | 0.61 (0.34,1.08)* | 1.05 (0.75,1.45) | 1.05 (0.75, 1.45) | 2.04 (0.88,4.73) |
| Any fire in 24 hours prior to sample collection | ||||||||
| No | 71 | reference | reference | reference | reference | reference | reference | reference |
| Yes | 15 | 0.94 (0.64,1.37) | 0.95 (0.71,1.27) | 1.14 (0.83,1.56) | 1.48 (0.84,2.63) | 0.84 (0.61,1.16) | 1.68 (0.60, 4.74) | 0.94 (0.40,2.20) |
| Number of fires in the year prior to the sample collectionb | ||||||||
| <=9 | 17 | reference | reference | reference | reference | reference | reference | reference |
| 10–15 | 17 | 0.80 (0.54,1.19) | 0.84 (0.60,1.18) | 0.98 (0.66,1.44) | 0.98 (0.50,1.95) | 1.04 (0.70,1.54) | 1.04 (0.70, 1.54) | 0.50 (0.18,1.40) |
| 16–19 | 15 | 0.90 (0.60,1.36) | 1.04 (0.73,1.48) | 1.01 (0.67,1.53) | 1.32 (0.64,2.69) | 1.02 (0.68,1.54) | 1.02 (0.68, 1.54) | 0.70 (0.24,2.02) |
| >=20 | 17 | 0.64 (0.43,0.97) | 0.74 (0.52,1.05) | 0.72 (0.48,1.08) | 0.84 (0.41,1.72) | 0.78 (0.51,1.18) | 0.78 (0.51, 1.18) | 0.72 (0.25,2.09) |
Models adjusted for race/ethnicity, age and years of service with SFFD.
Data from participants who consented to grant access to their fire history from SFFD
pvalue≤ 0.1
pvalue≤ 0.05
pvalue≤ 0.001
Surprisingly, using SCBA, washing hands during a work shift and showering after a fire incident were associated with increased levels of some PFAS. Average PFNA, PFDA, and PFUnDA concentrations were higher among participants who said they sometimes used their SCBA during salvage/overhaul versus rarely or never. Similarly, average PFHxS levels were higher among participants who said they washed their hands more frequently or who responded that they always showered after a fire event compared to those who washed hands or showered after a fire event the least often. Those who washed their hands 16–20 times during a work shift had 2.90 (95%CI = 1.61, 5.23) times higher concentration of PFHxS compared to those who reported washing their hands 10 times or less per shift. Those who reported always showering after a fire event had 2.08 (95% CI = 1.04, 4.05) times higher PFHxS levels compared to those who reported that they sometimes showered.
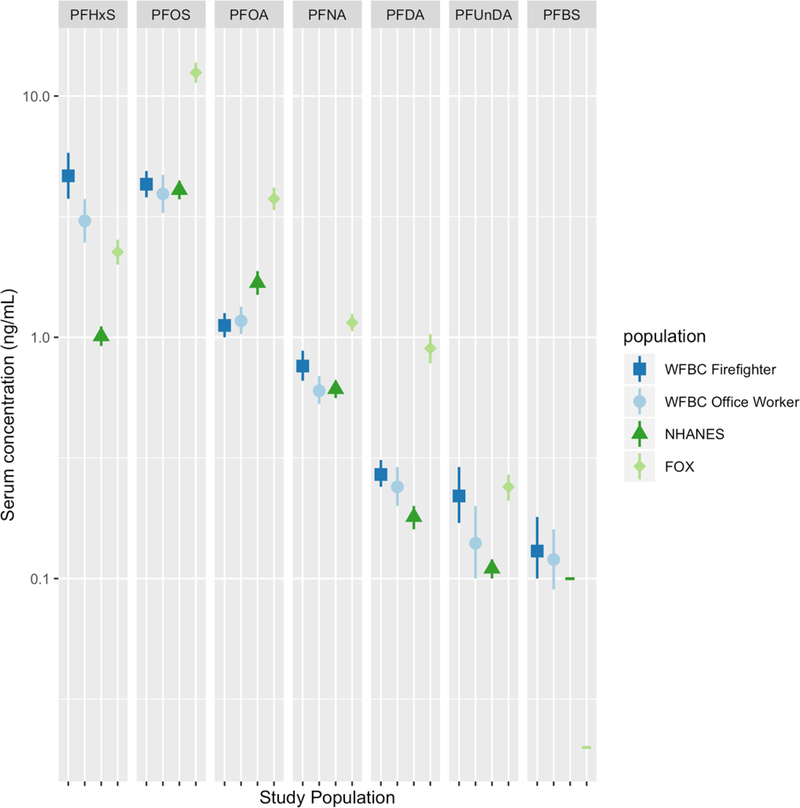
Figure 1 compares PFAS levels measured in our WFBC participants with other cohorts, including adult women from the 2013–2014 NHANES52 and the predominantly male 2010–2011 FOX study.56 WFBC firefighters and office workers had higher serum levels of PFHxS and a higher detection frequency for PFBS than both NHANES and FOX; while PFBS had low detection frequencies in both the FOX and NHANES studies (DF: 6.9% and 0.7%, respectively) the WFBC had a PFBS detection frequency of 74% for firefighters and 70% for office workers. WFBC firefighters also had higher levels of PFNA, PFDA and PFUnDA levels compared to NHANES, whereas office workers had similar levels to NHANES for PFOS and PFNA. Both WFBC firefighter and office worker groups had lower levels of PFOA compared to NHANES and lower levels of PFOS, PFOA, PFNA, PFDA, and PFUnDA than those measured in the FOX study.
Figure 1.
Comparison of geometric mean (GM) and 95% confidence intervals (CI) of PFAS levels measured in WFBC firefighters and office workers (2014–15) with adult women in NHANES (2013–14) and male firefighters in the FOX study (2010–11).
Figure footnote: Figure shows GM and 95% CI for those PFAS with detection frequencies of at least 70% among WFBC participants. PFBS had low DF for FOX (6.9%) and NHANES (0.7%); therefore, we plotted the LOD, represented by horizontal green lines, in lieu of GM and 95% CI. We replaced levels below the LOD with LOD/√2 and applied the LOD respective to each study population. Tests of statistical significance for differences between WFBC groups is shown in Table 4.
Discussion
This biomonitoring study is the first to assess levels of PFAS compounds in an all-female cohort of firefighters and office workers. Of the twelve PFAS we measured, detection frequencies ranged from 0 to 100% and all participants had at least four PFAS congeners (PFHxS, PFOA, PFOS and PFNA) detected in their serum samples. Widespread use of PFAS in consumer products, contamination of food and water sources, and their environmental persistence may contribute to the high background levels of these compounds in both firefighters and office workers. Indeed PFAS are ubiquitous in the environment and have been found in dust, food and humans worldwide.35,59 In addition, the widespread use of PFAS containing products on clothing, furniture fabrics, carpets and paper food packaging also contributes to levels found in people.49,60 Drinking water contamination is considered an important source of PFAS exposure in many communities,49,61,62 and people with contaminated drinking water have elevated PFAS in their blood.63 However, local San Francisco Bay Area water systems are not likely to be a significant source of PFAS exposure for WFBC study participants. Municipal water systems in the locations where most study participants live were tested for PFAS under the Environmental Protection Agency’s Unregulated Contaminant Monitoring Rule in 2016; tests of San Francisco Public Utilities Commission (SFPUC) water sources between 2012 and 2018 did not find measurable levels of PFBS, PFHxS, PFHPA, PFNA, PFOA, or PFOS in San Francisco or surrounding community municipal water systems.64,65
Multivariate models showed that PFHxS, PFUnDA, and PFNA exposure was higher in firefighters compared to office workers after controlling for age, race and ethnicity, and education. When we additionally controlled for the frequency of eating certain foods the association remained higher in firefighters compared to office workers and the strength of association increased or remained the same after adjustment for potential confounders. When we limited the analysis to firefighters, we found that several occupational activities were associated with higher PFAS levels. Firefighters’ assigned position was the most strongly associated with higher PFAS levels, with those assigned as firefighters or officers having higher levels of PFNA, PFOA, PFDA and PFUnDA compared to drivers. Compared to drivers, PFOS was higher among those assigned to the firefighter position however, PFBS was higher among drivers compared to officers. Differential PFAS exposures by position may be explained by different roles at fire events. Engine drivers typically remain with the apparatus because they supply water for initial interior fire suppression work, as well as set the ladders for ventilation procedures. In addition, drivers in the SFFD do not typically perform overhaul procedures after a fire is extinguished, and thus may avoid a critical source of exposure.66 We did not find an association between PFAS levels and fighting a fire in the previous 24 hours or with the number of fires in the year prior to sample collection.
Firefighting foams may be another important source of PFAS exposure. Aqueous Film Forming Foams (AFFF) are known to contain PFAS surfactants, including PFOS, PFOA and PFHxS.20,67 Our data suggest that firefighters who reported using firefighting foam in the past year had higher levels of several PFAS than those who reported not using firefighting foams in the past year. Among airport firefighters, we found that PFNA levels were two times higher compared to firefighters assigned to other stations in San Francisco. Although PFNA is not considered a main ingredient in AFFF, a study in Finland found that firefighters using AFFF in training activities had increased levels of PFNA after the training activities.20
Unexpectedly, procedures that generally are intended to reduce contaminant exposures were associated with increased exposures for some PFAS. Washing hands more frequently during the work shift and always showering after a fire event were associated with increased PFHxS levels while sometimes using SCBA during salvage overhaul was associated with increased PFNA, PFDA and PFUnDA. One explanation is that firefighters may differentially report hand washing, showering frequency, and SCBA use; those firefighters involved in more fire suppression activities could possibly report these activities more than those who respond to fewer fire calls, because washing and SCBA use are expected occupational hygiene practices. Self-reporting bias in terms of occupational safety and health procedures, which has been shown in other studies,68,69 may have also affected our results. Similarly, duration of SCBA use during fire events may also be an important factor to examine in future studies, as it is possible that although firefighters may wear SCBA frequently, they may remove it after extinguishing a fire and during salvage and overhaul operations because gear is heavy, conditions are hot, and the location appears to be free of smoke.15,66 In addition, there may be unknown and unmeasured occupational sources of PFAS exposure in firefighting that could help explain observed associations.
We compared the levels of PFAS congeners in WFBC participants with levels from two other exposure studies: A cohort of mostly male firefighters in Southern California (FOX) and a nationally representative sample of adult women (NHANES). In general, WFBC firefighters and office workers had lower PFAS levels than those measured in the FOX study, except for PFHxS which was significantly higher in both WFBC firefighters and office workers. In particular, the lower levels of PFOA and PFOS in the WFBC participants compared to NHANES and FOX may reflect the temporal trends associated with the phase-out of these compounds in consumer products and firefighting equipment. The FOX study samples were collected between 2010 and 2011, three years before the start of the WFBC study and during the phase out period of PFOA and PFOS.70 Studies have shown that PFAS levels have changed over time with many PFAS that have been phased out decreasing and their replacements increasing.37,38,71,72 Interestingly, we did see overall higher levels of PFHxS in both groups of WFBC participants collected in 2013–2014 relative to the 2010–2011 FOX cohort. The increased levels in WFBC participants may be due to PFHxS’ long half-life (8.5 years) compared to PFOS (5.4 years) or PFOA (3.8 years).73 In addition, there may be other sources of PFHxS exposures that continue to affect California residents overall.71 The elevated PFHxS among WFBC firefighters in relation to FOX participants may be due, in part, to its use as a replacement for PFOA and PFOS in firefighting foams.67 Additionally, the lower levels of most PFAS among WFBC participants compared to the mostly male cohort of FOX participants may be further explained by excretion pathway differences between men and women, where women may have lower PFAS levels from their binding affinity with fatty acid proteins of the blood thus increased excretion during menstruation.74,75
WFBC and NHANES data were collected at around the same time (2013–14 for NHANES and 2014–15 for the WFBC) and levels between WFBC and adult women of NHANES were more similar to each other than with the FOX study, where the FOX study had higher PFAS levels except for PFHxS and PFUnDA. However, PFHxS, PFDA, and PFBS levels were higher in WFBC firefighters and office workers compared to NHANES adult women. While we compared WFBC chemical levels to adult women in NHANES, due to our small sample size we did not consider other comparisons by factors such as occupation or race/ethnicity. The lower PFAS levels among WFBC and NHANES compared to FOX may be due in part to the aforementioned increased excretion of PFAS among women. The increased levels of PFBS among WFBC firefighters and office workers may indicate its use as a replacement PFAS while its relatively short half-life of approximately 25 days, may indicate other common and occupational exposures to this compound.76
Health effects observed in people exposed to PFOA include high cholesterol, ulcerative colitis, thyroid disease, testicular and kidney cancers, and pregnancy-induced hypertension.77 PFOS exposure has also been associated with immunotoxicity, as indicated by a decreased response to vaccine in children;78 and other studies of people exposed to PFAS show effects on liver and decreased birth weight.79 In animal studies, PFAS have been shown to have a variety of similar toxicological effects including liver toxicity, suppressed immune function, altered mammary gland development, obesity, and cancer.80,81 The concordance between endpoints identified in animal studies and human studies, most notably effects on liver, kidney, fetal growth and development, and suppression of the immune system, add confidence to the findings.82,83 Based on these studies in humans and animals, some government agencies have established allowable levels of PFOA and PFOS in drinking water.82,84 For PFOA, these benchmarks are designed to prevent people from having blood serum levels above 14 ng/ml.85 The maximum value in this study was 5 ng/mL. However, PFOA has been shown to alter mammary gland development in mice following in utero exposure at even lower levels, and estimates of target serum levels to protect against those effects are less than 1 ng/ml85. The health effects of the other PFAS found in elevated levels in firefighters have not been well studied and target serum concentrations that are expected to protect against adverse effects are not available for PFNA, PFBS, PFHxS, PFUnDA, so it is difficult to compare measured levels in firefighters with benchmarks intended to protect against health effects. Allowable daily intake amounts intended to protect against adverse health effects are in the same range as PFOA for PFNA, while for PFHxS they are about 10 times higher and for PFBS they are 100 times higher.86 However the higher allowable daily intakes for PFBS and PFHxS do not necessarily correspond to higher allowable serum levels for these chemicals. Instead they reflect differences in the relationship between intake and serum concentration for each of the chemicals.
Our study has several limitations. There may still be unmeasured confounders and unknown sources of PFAS for which data was not possible to obtain. For example, while we were able to ask participants about their use of AFFF, we do not know the formulations of foam stocked and used in the SFFD. We also do not have information on the extent to which formulations have changed since PFOS and PFOA have been phased out, or if existing stocks of AFFF in SFFD have been replaced with newer formulations. It was also difficult to assess the relationship between fire events and exposures. Since we did not time the sample collection with fire events, very few firefighters had responded to a fire event in the 24 hours prior to the sample collection. We were able to access historical fire event data from the fire department through the Human Resources Management System (HRMS) database, which allowed us to estimate the number of fires each firefighter had attended in the year prior to sample collection. However, this information was limited to participants who consented to giving us access to their HRMS (n=66) which diminished statistical power to assess the relationship between fire events and chemical exposure levels. In addition, the HRMS data does not provide details about the intensity of the fire or the participant’s assigned role at the fire event (e.g. whether the firefighter was involved in direct fire suppression activities or providing back up and support).
We used a community-based participatory research design that entailed the active involvement of firefighters to develop study protocols and recruit participants (both firefighters and office workers) into the study. By including office workers from the City and County of San Francisco, we were able to compare firefighter exposures to a working population of women who were not involved in firefighting activities, but who live and work in the same geographical region allowing us to examine which PFAS chemicals are most strongly associated with firefighting. Understanding the extent to which PFAS exposures differ between firefighters and office workers can elucidate which compounds are likely to have occupational sources, highlight opportunities for prevention strategies, and assess the effectiveness of workplace exposure reduction efforts.
Supplementary Material
Acknowledgements
The authors thank all of the WFBC study participants for their contribution to the study. This work is supported by the California Breast Cancer Research Program #19BB-2900 (JT, RG, TL, RAR, HB, VB, RMF), the National Institute of Environmental Health Sciences R01ES027051 (RMF), the National Institute for Occupational Safety and Health, Targeted Research Training Program T42 OH008429 (JT), the San Francisco Firefighter Cancer Prevention Foundation (HB) and the International Association of Firefighters-Local 798. We thank Anthony Stefani, Cassidy Clarity, Emily O’Rourke, Nancy Carmona, Karen Kerr, Julie Mau, Natasha Parks, Lisa Holdcroft, San Francisco Fire Chief Jeanine Nicholson, former San Francisco Fire Chief Joanne Hayes-White, Sharyle Patton, Connie Engel and Nancy Buermeyer for their contributions to the study.
RAR and VB, are employed at the Silent Spring Institute, a scientific research organization dedicated to studying environmental factors in women’s health. The Institute is a 501(c)3 public charity funded by federal grants and contracts, foundation grants, and private donations, including from breast cancer organizations. HB is former president and member of United Fire Service Women, a 501(c)3 public charity dedicated to supporting the welfare of women in the San Francisco Fire Department.
Footnotes
The authors declare they have no actual or potential competing financial interests.
Supporting information available. This information is available free of charge at http://pubs.acs.org.
References
- (1).LeMasters GK; Genaidy AM; Succop P; Deddens J; Sobeih T; Barriera-Viruet H; Dunning K; Lockey J Cancer Risk among Firefighters: A Review and Meta-Analysis of 32 Studies. J. Occup. Environ. Med 2006, 48 (11), 1189–1202. 10.1097/01.jom.0000246229.68697.90. [DOI] [PubMed] [Google Scholar]
- (2).IARC. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans Volume 98 Painting, Firefighting, and Shiftwork.; WHO: Lyon, France, 2010. [PMC free article] [PubMed] [Google Scholar]
- (3).Daniels RD; Bertke S; Dahm MM; Yiin JH; Kubale TL; Hales TR; Baris D; Zahm SH; Beaumont JJ; Waters KM; Pinkerton LE Exposure-Response Relationships for Select Cancer and Non-Cancer Health Outcomes in a Cohort of U.S. Firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup. Environ. Med 2015, 72 (10), 699–706. 10.1136/oemed-2014-102671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (4).Ahn Y-S; Jeong K-S; Kim K-S Cancer Morbidity of Professional Emergency Responders in Korea. Am. J. Ind. Med 2012, 55 (9), 768–778. 10.1002/ajim.22068. [DOI] [PubMed] [Google Scholar]
- (5).Bates MN Registry-Based Case-Control Study of Cancer in California Firefighters. Am. J. Ind. Med 2007, 50 (5), 339–344. 10.1002/ajim.20446. [DOI] [PubMed] [Google Scholar]
- (6).Delahunt B; Bethwaite PB; Nacey JN Occupational Risk for Renal Cell Carcinoma. A Case-Control Study Based on the New Zealand Cancer Registry. Br. J. Urol 1995, 75 (5), 578–582. 10.1111/j.1464-410X.1995.tb07410.x. [DOI] [PubMed] [Google Scholar]
- (7).Kang D; Davis LK; Hunt P; Kriebel D Cancer Incidence among Male Massachusetts Firefighters, 1987–2003. Am. J. Ind. Med 2008, 51 (5), 329–335. 10.1002/ajim.20549. [DOI] [PubMed] [Google Scholar]
- (8).Ma F; Fleming LE; Lee DJ; Trapido E; Gerace TA; Lai H; Lai S Mortality in Florida Professional Firefighters, 1972 to 1999. Am. J. Ind. Med 2005, 47 (6), 509–517. 10.1002/ajim.20160. [DOI] [PubMed] [Google Scholar]
- (9).Ma F; Fleming LE; Lee DJ; Trapido E; Gerace TA Cancer Incidence in Florida Professional Firefighters, 1981 to 1999. J. Occup. Environ. Med 2006, 48 (9), 883–888. 10.1097/01.jom.0000235862.12518.04. [DOI] [PubMed] [Google Scholar]
- (10).Tsai RJ; Luckhaupt SE; Schumacher P; Cress RD; Deapen DM; Calvert GM Risk of Cancer among Firefighters in California, 1988–2007. Am. J. Ind. Med 2015, 58 (7), 715–729. 10.1002/ajim.22466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (11).Daniels RD; Kubale TL; Yiin JH; Dahm MM; Hales TR; Baris D; Zahm SH; Beaumont JJ; Waters KM; Pinkerton LE Mortality and Cancer Incidence in a Pooled Cohort of US Firefighters from San Francisco, Chicago and Philadelphia (1950–2009). Occup. Environ. Med 2014, 71 (6), 388–397. 10.1136/oemed-2013-101662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Adetona O; Zhang JJ; Hall DB; Wang J-S; Vena JE; Naeher LP Occupational Exposure to Woodsmoke and Oxidative Stress in Wildland Firefighters. Sci. Total Environ 2013, 449, 269–275. 10.1016/j.scitotenv.2013.01.075. [DOI] [PubMed] [Google Scholar]
- (13).Bolstad-Johnson DM; Burgess JL; Crutchfield CD; Storment S; Gerkin R; Wilson JR Characterization of Firefighter Exposures during Fire Overhaul. AIHAJ J. Sci. Occup. Environ. Health Saf 2000, 61 (5), 636–641. [DOI] [PubMed] [Google Scholar]
- (14).Fent KW; Eisenberg J; Snawder J; Sammons D; Pleil JD; Stiegel MA; Mueller C; Horn GP; Dalton J Systemic Exposure to PAHs and Benzene in Firefighters Suppressing Controlled Structure Fires. Ann. Occup. Hyg 2014, 58 (7), 830–845. 10.1093/annhyg/meu036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (15).Gainey SJ; Horn GP; Towers AE; Oelschlager ML; Tir VL; Drnevich J; Fent KW; Kerber S; Smith DL; Freund GG Exposure to a Firefighting Overhaul Environment without Respiratory Protection Increases Immune Dysregulation and Lung Disease Risk. PloS One 2018, 13 (8), e0201830 10.1371/journal.pone.0201830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (16).Navarro KM; Cisneros R; Noth EM; Balmes JR; Hammond SK Occupational Exposure to Polycyclic Aromatic Hydrocarbon of Wildland Firefighters at Prescribed and Wildland Fires. Environ. Sci. Technol 2017, 51 (11), 6461–6469. 10.1021/acs.est.7b00950. [DOI] [PubMed] [Google Scholar]
- (17).Alexander BM; Baxter CS Flame-Retardant Contamination of Firefighter Personal Protective Clothing - A Potential Health Risk for Firefighters. J. Occup. Environ. Hyg 2016, 13 (9), D148–155. 10.1080/15459624.2016.1183016. [DOI] [PubMed] [Google Scholar]
- (18).Brown FR; Whitehead TP; Park J-S; Metayer C; Petreas MX Levels of Non-Polybrominated Diphenyl Ether Brominated Flame Retardants in Residential House Dust Samples and Fire Station Dust Samples in California. Environ. Res. 2014, 135, 9–14. 10.1016/j.envres.2014.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Fent KW; Evans DE; Booher D; Pleil JD; Stiegel MA; Horn GP; Dalton J Volatile Organic Compounds Off-Gassing from Firefighters’ Personal Protective Equipment Ensembles after Use. J. Occup. Environ. Hyg 2015, 12 (6), 404–414. 10.1080/15459624.2015.1025135. [DOI] [PubMed] [Google Scholar]
- (20).Laitinen JA; Koponen J; Koikkalainen J; Kiviranta H Firefighters’ Exposure to Perfluoroalkyl Acids and 2-Butoxyethanol Present in Firefighting Foams. Toxicol. Lett 2014, 231 (2), 227–232. 10.1016/j.toxlet.2014.09.007. [DOI] [PubMed] [Google Scholar]
- (21).Shen B; Whitehead TP; McNeel S; Brown FR; Dhaliwal J; Das R; Israel L; Park J-S; Petreas M High Levels of Polybrominated Diphenyl Ethers in Vacuum Cleaner Dust from California Fire Stations. Environ. Sci. Technol 2015, 49 (8), 4988–4994. 10.1021/es505463g. [DOI] [PubMed] [Google Scholar]
- (22).Robinson MS; Anthony TR; Littau SR; Herckes P; Nelson X; Poplin GS; Burgess JL Occupational PAH Exposures during Prescribed Pile Burns. Ann. Occup. Hyg 2008, 52 (6), 497–508. 10.1093/annhyg/men027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (23).Caux C; O’Brien C; Viau C Determination of Firefighter Exposure to Polycyclic Aromatic Hydrocarbons and Benzene during Fire Fighting Using Measurement of Biological Indicators. Appl. Occup. Environ. Hyg 2002, 17 (5), 379–386. 10.1080/10473220252864987. [DOI] [PubMed] [Google Scholar]
- (24).Austin CC; Wang D; Ecobichon DJ; Dussault G Characterization of Volatile Organic Compounds in Smoke at Experimental Fires. J. Toxicol. Environ. Health A 2001, 63 (3), 191–206. 10.1080/15287390151101547. [DOI] [PubMed] [Google Scholar]
- (25).Feunekes FD; Jongeneelen FJ; vd Laan H; Schoonhof FH Uptake of Polycyclic Aromatic Hydrocarbons among Trainers in a Fire-Fighting Training Facility. Am. Ind. Hyg. Assoc. J 1997, 58 (1), 23–28. 10.1080/15428119791013035. [DOI] [PubMed] [Google Scholar]
- (26).Shaw SD; Berger ML; Harris JH; Yun SH; Wu Q; Liao C; Blum A; Stefani A; Kannan K Persistent Organic Pollutants Including Polychlorinated and Polybrominated Dibenzo-p-Dioxins and Dibenzofurans in Firefighters from Northern California. Chemosphere 2013, 91 (10), 1386–1394. 10.1016/j.chemosphere.2012.12.070. [DOI] [PubMed] [Google Scholar]
- (27).Park J-S; Voss RW; McNeel S; Wu N; Guo T; Wang Y; Israel L; Das R; Petreas M High Exposure of California Firefighters to Polybrominated Diphenyl Ethers. Environ. Sci. Technol 2015, 49 (5), 2948–2958. 10.1021/es5055918. [DOI] [PubMed] [Google Scholar]
- (28).Dobraca D; Israel L; McNeel S; Voss R; Wang M; Gajek R; Park J-S; Harwani S; Barley F; She J; Das R Biomonitoring in California Firefighters: Metals and Perfluorinated Chemicals. J. Occup. Environ. Med 2015, 57 (1), 88–97. 10.1097/JOM.0000000000000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Jin C; Sun Y; Islam A; Qian Y; Ducatman A Perfluoroalkyl Acids Including Perfluorooctane Sulfonate and Perfluorohexane Sulfonate in Firefighters. J. Occup. Environ. Med 2011, 53 (3), 324–328. 10.1097/JOM.0b013e31820d1314. [DOI] [PubMed] [Google Scholar]
- (30).Brandt-Rauf PW; Fallon LF; Tarantini T; Idema C; Andrews L Health Hazards of Fire Fighters: Exposure Assessment. Br. J. Ind. Med 1988, 45 (9), 606–612. 10.1136/oem.45.9.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (31).Edelman P; Osterloh J; Pirkle J; Caudill SP; Grainger J; Jones R; Blount B; Calafat A; Turner W; Feldman D; Baron S; Bernard B; Lushniak BD; Kelly K; Prezant D Biomonitoring of Chemical Exposure among New York City Firefighters Responding to the World Trade Center Fire and Collapse. Environ. Health Perspect 2003, 111 (16), 1906–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Rudel RA; Fenton SE; Ackerman JM; Euling SY; Makris SL Environmental Exposures and Mammary Gland Development: State of the Science, Public Health Implications, and Research Recommendations. Environ. Health Perspect 2011, 119 (8), 1053–1061. 10.1289/ehp.1002864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Rudel RA; Ackerman JM; Attfield KR; Brody JG New Exposure Biomarkers as Tools for Breast Cancer Epidemiology, Biomonitoring, and Prevention: A Systematic Approach Based on Animal Evidence. Environ. Health Perspect 2014, 122 (9), 881–895. 10.1289/ehp.1307455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Moody CA; Field JA Perfluorinated Surfactants and the Environmental Implications of Their Use in Fire-Fighting Foams. Environ. Sci. Technol 2000, 34 (18), 3864–3870. 10.1021/es991359u. [DOI] [Google Scholar]
- (35).Björklund JA; Thuresson K; de Wit CA Perfluoroalkyl Compounds (PFCs) in Indoor Dust: Concentrations, Human Exposure Estimates, and Sources. Environ. Sci. Technol 2009, 43 (7), 2276–2281. 10.1021/es803201a. [DOI] [PubMed] [Google Scholar]
- (36).Olsen GW; Mair DC; Reagen WK; Ellefson ME; Ehresman DJ; Butenhoff JL; Zobel LR Preliminary Evidence of a Decline in Perfluorooctanesulfonate (PFOS) and Perfluorooctanoate (PFOA) Concentrations in American Red Cross Blood Donors. Chemosphere 2007, 68 (1), 105–111. 10.1016/j.chemosphere.2006.12.031. [DOI] [PubMed] [Google Scholar]
- (37).Calafat AM; Wong L-Y; Kuklenyik Z; Reidy JA; Needham LL Polyfluoroalkyl Chemicals in the U.S. Population: Data from the National Health and Nutrition Examination Survey (NHANES) 2003–2004 and Comparisons with NHANES 1999–2000. Environ. Health Perspect 2007, 115 (11), 1596–1602. 10.1289/ehp.10598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Olsen GW; Mair DC; Lange CC; Harrington LM; Church TR; Goldberg CL; Herron RM; Hanna H; Nobiletti JB; Rios JA; Reagen WK; Ley CA Per- and Polyfluoroalkyl Substances (PFAS) in American Red Cross Adult Blood Donors, 2000–2015. Environ. Res 2017, 157, 87–95. 10.1016/j.envres.2017.05.013. [DOI] [PubMed] [Google Scholar]
- (39).Barry V; Winquist A; Steenland K Perfluorooctanoic Acid (PFOA) Exposures and Incident Cancers among Adults Living near a Chemical Plant. Environ. Health Perspect 2013, 121 (11–12), 1313–1318. 10.1289/ehp.1306615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Joensen UN; Bossi R; Leffers H; Jensen AA; Skakkebæk NE; Jørgensen N Do Perfluoroalkyl Compounds Impair Human Semen Quality? Environ. Health Perspect 2009, 117 (6), 923–927. 10.1289/ehp.0800517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (41).Lopez-Espinosa M-J; Mondal D; Armstrong B; Bloom MS; Fletcher T Thyroid Function and Perfluoroalkyl Acids in Children Living Near a Chemical Plant. Environ. Health Perspect 2012, 120 (7), 1036–1041. 10.1289/ehp.1104370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Lopez-Espinosa M-J; Mondal D; Armstrong BG; Eskenazi B; Fletcher T Perfluoroalkyl Substances, Sex Hormones, and Insulin-like Growth Factor-1 at 6–9 Years of Age: A Cross-Sectional Analysis within the C8 Health Project. Environ. Health Perspect 2016, 124 (8), 1269–1275. 10.1289/ehp.1509869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (43).Bassler J; Ducatman A; Elliott M; Wen S; Wahlang B; Barnett J; Cave MC Environmental Perfluoroalkyl Acid Exposures Are Associated with Liver Disease Characterized by Apoptosis and Altered Serum Adipocytokines. Environ. Pollut. Barking Essex 1987 2019, 247, 1055–1063. 10.1016/j.envpol.2019.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (44).Blake BE; Pinney SM; Hines EP; Fenton SE; Ferguson KK Associations between Longitudinal Serum Perfluoroalkyl Substance (PFAS) Levels and Measures of Thyroid Hormone, Kidney Function, and Body Mass Index in the Fernald Community Cohort. Environ. Pollut. Barking Essex 1987 2018, 242 (Pt A), 894–904. 10.1016/j.envpol.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (45).Liu G; Dhana K; Furtado JD; Rood J; Zong G; Liang L; Qi L; Bray GA; DeJonge L; Coull B; Grandjean P; Sun Q Perfluoroalkyl Substances and Changes in Body Weight and Resting Metabolic Rate in Response to Weight-Loss Diets: A Prospective Study. PLoS Med. 2018, 15 (2), e1002502 10.1371/journal.pmed.1002502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (46).Steenland K; Zhao L; Winquist A; Parks C Ulcerative Colitis and Perfluorooctanoic Acid (PFOA) in a Highly Exposed Population of Community Residents and Workers in the Mid-Ohio Valley. Environ. Health Perspect. 2013, 121 (8), 900–905. 10.1289/ehp.1206449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (47).US Department of Labor, B. of L. S. Employed persons by detailed occupation, sex, race, and Hispanic or Latino ethnicity https://www.bls.gov/cps/cpsaat11.htm (accessed Mar 19, 2019).
- (48).Hulett DM; Bendick M Jr; Thomas SY; Moccio F Enhancing Women’s Inclusion in Firefighting in the USA. Int. J. Divers. Organ. Communities Nations 2008, 8 (2). [Google Scholar]
- (49).Boronow KE; Brody JG; Schaider LA; Peaslee GF; Havas L; Cohn BA Serum Concentrations of PFASs and Exposure-Related Behaviors in African American and Non-Hispanic White Women. J. Expo. Sci. Environ. Epidemiol 2019, 29 (2), 206–217. 10.1038/s41370-018-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (50).Ji K; Kim S; Kho Y; Paek D; Sakong J; Ha J; Kim S; Choi K Serum Concentrations of Major Perfluorinated Compounds among the General Population in Korea: Dietary Sources and Potential Impact on Thyroid Hormones. Environ. Int 2012, 45, 78–85. 10.1016/j.envint.2012.03.007. [DOI] [PubMed] [Google Scholar]
- (51).Tuck MK; Chan DW; Chia D; Godwin AK; Grizzle WE; Krueger KE; Rom W; Sanda M; Sorbara L; Stass S; Wang W; Brenner DE Standard Operating Procedures for Serum and Plasma Collection: Early Detection Research Network Consensus Statement Standard Operating Procedure Integration Working Group. J. Proteome Res 2009, 8 (1), 113–117. 10.1021/pr800545q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (52).Center for Disease Control. NHANES 2013–2014 Laboratory Data https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Laboratory&CycleBeginYear=2013 (accessed Aug 2, 2018).
- (53).Liu S; Yang R; Yin N; Faiola F The Short-Chain Perfluorinated Compounds PFBS, PFHxS, PFBA and PFHxA, Disrupt Human Mesenchymal Stem Cell Self-Renewal and Adipogenic Differentiation. J. Environ. Sci. China 2020, 88, 187–199. 10.1016/j.jes.2019.08.016. [DOI] [PubMed] [Google Scholar]
- (54).Helsel DR More than Obvious: Better Methods for Interpreting Nondetect Data. Environ. Sci. Technol 2005, 39 (20), 419A–423A. [DOI] [PubMed] [Google Scholar]
- (55).Federal Aviation Administration. CertAlerts for Part 139 Airport Certification – Airports https://www.faa.gov/airports/airport_safety/certalerts/ (accessed Jun 5, 2019).
- (56).Biomonitoring California. Project Results for Firefighter Occupational Exposures (FOX) Project | Measuring Chemicals in Californians https://biomonitoring.ca.gov/results/projects/410 (accessed Jul 17, 2018).
- (57).RStudio Team. RStudio: Integrated Development for R; RStudio Inc: Boston, MA, 2016. [Google Scholar]
- (58).R Development Core Team. R: A Language and Environment for Statistical Computing.; R Foundation for Statitical Computing: Vienna, Austria, 2008. [Google Scholar]
- (59).Petersen MS; Halling J; Jørgensen N; Nielsen F; Grandjean P; Jensen TK; Weihe P Reproductive Function in a Population of Young Faroese Men with Elevated Exposure to Polychlorinated Biphenyls (PCBs) and Perfluorinated Alkylate Substances (PFAS). Int. J. Environ. Res. Public. Health 2018, 15 (9). 10.3390/ijerph15091880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (60).Domingo JL; Nadal M Per- and Polyfluoroalkyl Substances (PFASs) in Food and Human Dietary Intake: A Review of the Recent Scientific Literature. J. Agric. Food Chem 2017, 65 (3), 533–543. 10.1021/acs.jafc.6b04683. [DOI] [PubMed] [Google Scholar]
- (61).Hu XC; Andrews DQ; Lindstrom AB; Bruton TA; Schaider LA; Grandjean P; Lohmann R; Carignan CC; Blum A; Balan SA; Higgins CP; Sunderland EM Detection of Poly- and Perfluoroalkyl Substances (PFASs) in U.S. Drinking Water Linked to Industrial Sites, Military Fire Training Areas, and Wastewater Treatment Plants. Environ. Sci. Technol. Lett 2016, 3 (10), 344–350. 10.1021/acs.estlett.6b00260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (62).Hurley S; Houtz E; Goldberg D; Wang M; Park J-S; Nelson DO; Reynolds P; Bernstein L; Anton-Culver H; Horn-Ross P; Petreas M Preliminary Associations between the Detection of Perfluoroalkyl Acids (PFAAs) in Drinking Water and Serum Concentrations in a Sample of California Women. Environ. Sci. Technol. Lett 2016, 3 (7), 264–269. 10.1021/acs.estlett.6b00154. [DOI] [Google Scholar]
- (63).New Jersey Drinking Water Quality Institute. Maximum Contaminant Level Recommendation for Perfluorooctanoic Acid in Drinking Water; 2015.
- (64).US EPA. Occurrence Data for the Unregulated Contaminant Monitoring Rule https://www.epa.gov/dwucmr/occurrence-data-unregulated-contaminant-monitoring-rule (accessed Aug 20, 2019).
- (65).San Francisco Public Utilities Commision. Screening and Recommended Actions for Contaminants of Emerging Concern (CECs) in SFPUC Drinking Water System: 2019 Progress Update; San Francisco: Department of Public Health, 2019. [Google Scholar]
- (66).Fent KW; Evans DE; Babik K; Striley C; Bertke S; Kerber S; Smith D; Horn GP Airborne Contaminants during Controlled Residential Fires. J. Occup. Environ. Hyg 2018, 15 (5), 399–412. 10.1080/15459624.2018.1445260. [DOI] [PubMed] [Google Scholar]
- (67).Rotander A; Toms L-ML; Aylward L; Kay M; Mueller JF Elevated Levels of PFOS and PFHxS in Firefighters Exposed to Aqueous Film Forming Foam (AFFF). Environ. Int 2015, 82, 28–34. 10.1016/j.envint.2015.05.005. [DOI] [PubMed] [Google Scholar]
- (68).Griffin SC; Neitzel R; Daniell WE; Seixas NS Indicators of Hearing Protection Use: Self-Report and Researcher Observation. J. Occup. Environ. Hyg 2009, 6 (10), 639–647. 10.1080/15459620903139060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (69).McCullagh MC; Rosemberg M-A Social Desirability Bias in Self-Reporting of Hearing Protector Use among Farm Operators. Ann. Occup. Hyg 2015, 59 (9), 1200–1207. 10.1093/annhyg/mev046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (70).Scheringer M; Trier X; Cousins IT; de Voogt P; Fletcher T; Wang Z; Webster TF Helsingør Statement on Poly- and Perfluorinated Alkyl Substances (PFASs). Chemosphere 2014, 114, 337–339. 10.1016/j.chemosphere.2014.05.044. [DOI] [PubMed] [Google Scholar]
- (71).Hurley S; Goldberg D; Wang M; Park J-S; Petreas M; Bernstein L; Anton-Culver H; Nelson DO; Reynolds P Time Trends in Per- and Polyfluoroalkyl Substances (PFASs) in California Women: Declining Serum Levels, 2011–2015. Environ. Sci. Technol 2018, 52 (1), 277–287. 10.1021/acs.est.7b04650. [DOI] [PubMed] [Google Scholar]
- (72).Kato K; Calafat AM; Wong L-Y; Wanigatunga AA; Caudill SP; Needham LL Polyfluoroalkyl Compounds in Pooled Sera from Children Participating in the National Health and Nutrition Examination Survey 2001– 2002. Environ. Sci. Technol 2009, 43 (7), 2641–2647. [DOI] [PubMed] [Google Scholar]
- (73).Olsen GW; Burris JM; Ehresman DJ; Froehlich JW; Seacat AM; Butenhoff JL; Zobel LR. Half-Life Serum Elimination of Perfluorooctanesulfonate, Perfluorohexanesulfonate, and Perfluorooctanoate in Retired Fluorochemical Production Workers. Environ. Health Perspect 2007, 115 (9), 1298–1305 8p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (74).Zhang Y; Beesoon S; Zhu L; Martin JW Biomonitoring of Perfluoroalkyl Acids in Human Urine and Estimates of Biological Half-Life. Environ. Sci. Technol 2013, 47 (18), 10619–10627. 10.1021/es401905e. [DOI] [PubMed] [Google Scholar]
- (75).Harada K; Inoue K; Morikawa A; Yoshinaga T; Saito N; Koizumi A Renal Clearance of Perfluorooctane Sulfonate and Perfluorooctanoate in Humans and Their Species-Specific Excretion. Environ. Res 2005, 99 (2), 253–261. 10.1016/j.envres.2004.12.003. [DOI] [PubMed] [Google Scholar]
- (76).Olsen GW; Chang S-C; Noker PE; Gorman GS; Ehresman DJ; Lieder PH; Butenhoff JL A Comparison of the Pharmacokinetics of Perfluorobutanesulfonate (PFBS) in Rats, Monkeys, and Humans. Toxicology 2009, 256 (1–2), 65–74. 10.1016/j.tox.2008.11.008. [DOI] [PubMed] [Google Scholar]
- (77).C8 Science Panel. C8 Science Panel Website http://www.c8sciencepanel.org/ (accessed Jul 30, 2019).
- (78).Grandjean P; Andersen EW; Budtz-Jørgensen E; Nielsen F; Mølbak K; Weihe P; Heilmann C Serum Vaccine Antibody Concentrations in Children Exposed to Perfluorinated Compounds. JAMA 2012, 307 (4), 391–397. 10.1001/jama.2011.2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (79).Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Perfluoroalkyls. (Draft for Public Comment).; Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service, 2018. [Google Scholar]
- (80).Lau C Perfluorinated Compounds: An Overview In Toxicological Effects of Perfluoroalkyl and Polyfluroalkyl Substances; DeWitt JC, Ed.; Molecular and Integrative Toxicology; Humana Press, Cham, 2015; pp 1–21. 10.1007/978-3-319-15518-0_1. [DOI] [Google Scholar]
- (81).Post GB; Gleason JA; Cooper KR Key Scientific Issues in Developing Drinking Water Guidelines for Perfluoroalkyl Acids: Contaminants of Emerging Concern. PLoS Biol. 2017, 15 (12), e2002855 10.1371/journal.pbio.2002855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (82).Cordner A; De La Rosa VY; Schaider LA; Rudel RA; Richter L; Brown P Guideline Levels for PFOA and PFOS in Drinking Water: The Role of Scientific Uncertainty, Risk Assessment Decisions, and Social Factors. J. Expo. Sci. Environ. Epidemiol 2019, 29 (2), 157–171. 10.1038/s41370-018-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (83).DeWitt JC; Blossom SJ; Schaider LA Exposure to Per-Fluoroalkyl and Polyfluoroalkyl Substances Leads to Immunotoxicity: Epidemiological and Toxicological Evidence. J. Expo. Sci. Environ. Epidemiol 2019, 29 (2), 148–156. 10.1038/s41370-018-0097-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (84).Interstate Technology and Regulatory Council. Interstate Technology and Regularotry Council (ITRC) PFAS Regulations, Guidance and Advisories Fact Sheet; ITRC PFAS Regulations Section 5 Tables, Ed. 2017; Interstate Technology and Regulatory Council, 2017. [Google Scholar]
- (85).New Jersey Department of Environmental Protection. Health-Based Maximum Recommendation Level Support Document: Perfluorooctanoic Acid (PFOA); New Jersey Drinking Water Quality Institute, Heath Effects Sub-committee: Trenton New Jersey, 2015; p 475. [Google Scholar]
- (86).Michigan Department of Health and Human Services, Division of Environmental Health. Public Health Drinking Water Screening Levels for PFAS; Michigan PFAS Action Response Team Human Health Workgroup: Michigan, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.