Abstract
A 68-year-old woman with a long history of relapsing chronic rhinosinusitis with nasal polyps (CRSwNP) underwent a complete reboot surgery and nasal biopsy prior to and after surgery. Remarkable improvement of symptoms and no signs of mucosal oedema and no complaints of initially worsening nasal functions were still present 12 months after reboot surgery. Biopsy demonstrated an outstanding reduction in eosinophilic infiltration and re-epithelisation of nasal mucosa with normal features after reboot approach compared with previous surgeries. Therefore, reboot approach may become an effective instrument in plurioperated patients with CRSwNP who suffer from a nasal condition that is recalcitrant to pharmacological therapies and is unsatisfactorily treated by standard surgical techniques.
Keywords: nasal polyps, otolaryngology / ENT
Background
Chronic rhinosinusitis with nasal polyps (CRSwNP) is a frequent, often recalcitrant and difficult to treat disease, impacting patients’ quality of life.1 An innovative surgical technique (‘reboot approach’), recently proposed by Alsharif et al, consists in removing the entire inflamed mucosa up to the periosteum and has showed very interesting outcomes in otherwise hardly treated patients.2
We here present the case of a patient with CRSwNP who underwent multiple surgical and medical treatments without achieving satisfactory disease control prior to reboot approach.
Case presentation
A 68-year-old woman with an 11-year-long history of asthma and eosinophilic CRSwNP was referred to our olaryngology department with a completely obstructed nasal cavity, anosmia and hypogeusia, frequent headache unresponsive to standard analgesics and relevant anterior and posterior rhinorrhea.
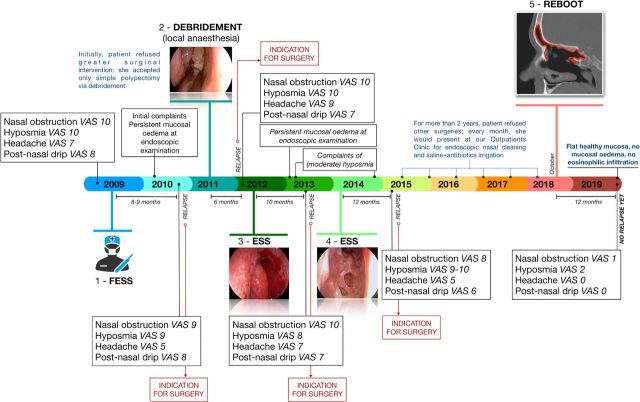
For her chronic rhinosinusitis, she underwent four endoscopic sinus surgeries in the last 10 years. Among all symptoms she had especially complained of nasal obstruction and hyposmia because they were relevantly affecting her quality of life and were the first symptoms that relapsed within 6–12 months after every surgery (figure 1). Her headache worsened over the years despite medical treatment. She habitually used intranasal corticosteroids and saline with antibiotics irrigation in the timeframe between surgeries, but control of symptoms was very low even with concomitant oral corticosteroid treatment.
Figure 1.
Patient’s clinical history. ESS, endoscopic sinus surgery; FESS, functional endoscopic sinus surgery; VAS, Visual Analogue Scale.
These non-satisfactory outcomes, by means of standard medical and surgical treatments, brought her to refuse further surgery for many years even when indicated by medical evaluation. At her referral to our unit when she again sought medical help, she was proposed a wider surgical management by novel but promising reboot approach.
Investigations
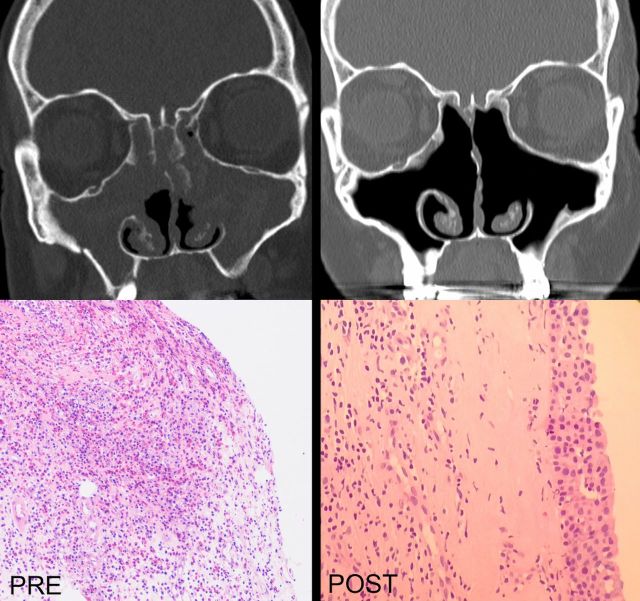
A CT scan was performed to evaluate the anatomical state of paranasal sinuses and the extension of chronic rhinosinusitis before surgery. The CT showed nasal cavities highly impacted by the disease and previous surgeries, partial residual of anterior and posterior ethmoid bone cells from previous operations, residual of right middle nasal concha and remodelling of the left one, a very wide maxillary antrostomy, no bone erosions of sinonasal outer walls and a total Lund-Mackay score3 of 22 out of 24 (figure 2). She also underwent a preoperative biopsy at the level of the medial maxillary wall, revealing a greatly inflamed mucosa with extensive eosinophilic infiltrate (figure 2).
Figure 2.
Radiological (upper panels) and pathological (lower panels) features prereboot (left side) and postrebbot (right side) surgery.
Visual Analogue Scale (VAS, 0–10) for the evaluation of severity of nasal obstruction, hyposmia, hypogeusia, frontal pain/pressure, frontorbital headache, anterior rhinorrhea and postnasal drip scored greater than 7 in most of them. Eventually, Sinonasal Outcome Test (SNOT-22) Score4 was 34, with decreased sense of smell and taste as the most impacting item affecting her health. Nasal endoscopy revealed cavities fully obstructed by nasal polyps with a Nasal Polyp Score5 of 7 (3 on the right nostril and 4 on the left).
Treatment
In November 2018, we performed a complete reboot surgery which consisted in removal of the whole mucosa from the ethmoidal cavity, maxillary and frontal sinuses. The procedure was associated with Draf IIb drainage, achieved by resecting the floor of the frontal sinus between the lamina papyracea and the nasal septum, anterior to the ventral margin of the olfactory fossa.
After a one-night hospitalisation, the patient was dismissed in good postoperative conditions. Regular daily saline nasal irrigation was indicated for the following months, along with a low maintenance dose of intranasal corticosteroid therapy: budesonide 50 μg/day per nostril (figure 1). No systemic corticosteroids were recommended in the follow-up period.
Outcome and follow-up
After reboot surgery, we observed a sharp and rapid improvement of symptoms and a remarkable elongation of time to relapse than she used to refer in previous treatments. She was assessed 1, 2 and 4 weeks after surgery by nasal endoscopy and VAS questionnaire regarding her main symptoms. She referred a significant improvement in the sense of smell and taste (hyposmia/hypogeusia: VAS 1), decreased frequency and severity of headache and facial pain/pressure (VAS 0) and no more nasal obstruction (VAS 1) worsening only during common cold.
At histological level, re-epithelisation was demonstrated by biopsy after 10 months at the level of the maxillary antrostomy, with healthy mucosa that appeared stratified as normal nasal epithelium with no evidence of relevant eosinophilic infiltration (figure 2). Radiologically, CT scan performed 10 months after surgery did not evidence opacification of paranasal sinuses anymore (figure 2). We are currently at 12 months of symptoms-free follow-up, which is a surprisingly much longer time than she used to experience till recurring of symptoms.
Discussion
CRS is a widespread condition affecting a large part of the population, slightly more than 10% in Europe and between 12% and 16% in the USA.1 CRS is a chronic inflammatory disease involving the nose and the paranasal sinuses characterised by at least 8–12 weeks with two typical symptoms (nasal blockage/obstruction/congestion, nasal discharge, facial pain/pressure and/or reduction or loss of smell), accompanied by either endoscopic signs of disease or relevant CT scan changes.1 6
According to European position paper on rhinosinusitis and nasal polyps (EPOS) Guidelines,1 to perform correct management of patients with CRS, they first have to be categorised based on disease severity (mild/moderate/severe), as it appears from endoscopic evaluation and symptoms’ VAS. First-line treatment is topical steroid spray and saline irrigation but, as severity progresses, topical doses augmentation, antibiotics and short courses of oral steroids are part of management indications.6 7 Cases of anatomical variants in the nose and sinuses that impede the normal mucus drainage through the sinuses ostia and put at risk of exacerbations or persistence of rhinosinusitis deserve surgical treatment, as well as those patients with unsatisfactory results after 1–3 months of medical treatment, according to initial disease severity.
If adequate surgery, intranasal corticosteroid treatment and up to two short courses of antibiotics or systemic corticosteroids in the last year are not sufficient to reach disease control, patients can be considered uncontrolled and with ‘difficult-to-treat rhinosinusitis’.1 8 9
The majority of cases with disease relapse after surgical treatment are those of CRSwNP, ranging from 38% to 60% at 1-year follow-up,1 10 but substantial variations in recurrence rates are also observed according to the presence of comorbidities such as asthma and non-steroidal antinflammatory drugs exacerbated respiratory disease (N-ERD): at 5-year follow-up since surgery, the chance of relapse is 16% in subjects with no such comorbidities, while it is 45% and 90% in patients with asthma and with N-ERD, respectively.10 Also surgical revision rates show increase from 10% to 25%, and to 37% for the aforementioned three groups.10 Furthermore in the worst scenarios, regardless of proper surgical interventions, it is not rare to observe constant mucosal oedema and rhinorrhea with recurring exacerbations at some time postoperatively, which therefore leads to long-term intranasal corticosteroids administration and repeated short courses of systemic corticosteroids,7 with possible drug-related adverse events and without a sufficient effectiveness in controlling CRSwNP.
Repetitive access of patients to hospital specialists, high costs of disease management and reduction in quality of life1 are features that make CRSwNP a very expensive condition for both patients and health services. Indeed, the economic and social burden of rhinosinusitis, both in acute and chronic conditions, is significant.11–14 Costs of medication, hospitalisation, physician’s examinations and surgery account only for direct healthcare expenses, while there is a concurrent and likewise substantial indirect cost from absenteeism, disability and therefore loss in productivity and work performance.13 An interesting systematic review,12 based on 44 studies, analysed the range for CRS-related healthcare costs in the USA, normalised according to 2014 US dollar inflection, which resulted in an estimated overall annual economic burden of $22 billion 2014 US dollar (direct and indirect costs).
In 2018, an innovative surgical technique entered the therapeutic scenario of chronic rhinosinusitis in recalcitrant cases and highly impacted patients. It has been proposed by Alsharif et al2 and aims to restore epithelial non-inflammatory state by means of removal of all dysfunctional eosinophilic-infiltrated mucosa up to the periosteum of nasal and paranasal cavities, partially sparing the mucosa of the inferior conchas. The rationale is that removal of type 2 inflammatory environment might allow unaffected re-epithelisation of sinuses walls. This approach, which should be accompanied by a Draf III or at least Draf IIb frontal drainage, is indicated in patients with recalcitrant and difficult-to-treat CRSwNP who are repeatedly exposed to surgical management.
In literature, besides Alsharif et al’s article, there are no similar reports of reboot surgery to nasal and paranasal cavities. Our case provides evidence of a marked and long-lasting clinical and radiological improvement of CRSwNP achieved along with a complete mucosal re-epithelisation with no residual oedema and absence of eosinophilic inflammation, thanks to reboot surgical approach, in a patient with severe and frequently relapsing disease. In contrast with what Alsharif et al suggested, in our case we confidently decided to perform a Draf IIb drainage instead of a Draf III because of the intraoperative finding of a sufficient opening to remove the frontal mucosa bilaterally. Unfortunately, the several previous surgeries did not allow us to preserve the middle nasal turbinates, unstable and remodelled by inflammation.
It suggests that demucosisation may become an effective instrument in pluri-operated patients and with symptoms recalcitrant to pharmacological therapies. This innovative technique seems noteworthy and its rationale reliable, but larger numbers of patients are likely still needed to further validate the reboot approach proposal and longer follow-up to prove its lasting results.
Patient’s perspective.
I have been experiencing a substantial amelioration of quality of life since reboot surgery. I believe this surgery was satisfying and gave me very good results on nasal respiration, headache and sense of smell. Outcomes were unexpected because of the multiple prior attempts having had temporary results. This time, not just symptoms improvement was remarkable to me, but also its duration, which has been much longer than I expected. My recovery was a little harder from this extended surgery: I felt weary for about a week, but I did not suffer from any other complications afterwards. After 1 year from this special surgery, results are significantly lasting and positively affecting my everyday’s quality of life, in a manner that I wasn’t used to anymore.
Learning points.
An innovative surgical method for chronic rhinosinusitis with nasal polyps (CRSwNP), the so-called ‘reboot approach’, has been proposed by Alsharif et al in 2018. The complete reboot consists in removal of the whole inflamed mucosa up to the periosteum of the ethmoidal cavity, maxillary, sphenoid and frontal sinuses, associated with Draf III drainage.
Reboot surgery is associated with restored normal epithelium of the respiratory mucosa.
Our case shows that reboot surgery is effective in improving CRSwNP symptoms, reducing the need of oral corticosteroids and of revision surgery, in a patient with a previous history of severe, uncontrolled and frequently and rapidly relapsing disease after classical surgery procedures.
We also demonstrated complete restored respiratory mucosa after reboot surgery, suggesting that this surgical procedure may have an effect on immunopathogenic mechanisms underlying CRSwNP.
Reboot surgery is a novel promising surgical approach to patients with severe CRSwNP.
Footnotes
Contributors: LM and FP evaluated and surgically treated the patient. ADV contributed in interpreting the results. EH contributed in analysing and interpreting the results. All the authors contributed in writing the report and approved it.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fokkens WJ, Lund VJ, Mullol J, et al. Epos 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012;50:1–12. 10.4193/Rhino50E2 [DOI] [PubMed] [Google Scholar]
- 2.Alsharif S, Jonstam K, van Zele T, et al. Endoscopic sinus surgery for type-2 CRS wNP: an Endotype-Based retrospective study. Laryngoscope 2019;129:1286–92. 10.1002/lary.27815 [DOI] [PubMed] [Google Scholar]
- 3.Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology 1993;107:183–4. [PubMed] [Google Scholar]
- 4.Hopkins C, Slack R, Lund V, et al. Long-Term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Laryngoscope 2009;119:2459–65. 10.1002/lary.20653 [DOI] [PubMed] [Google Scholar]
- 5.Meltzer EO, Hamilos DL, Hadley JA, et al. Rhinosinusitis: developing guidance for clinical trials. J Allergy Clin Immunol 2006;118:S17–61. 10.1016/j.jaci.2006.09.005 [DOI] [PubMed] [Google Scholar]
- 6.Heffler E, Malvezzi L, Boita M, et al. Immunological mechanisms underlying chronic rhinosinusitis with nasal polyps. Expert Rev Clin Immunol 2018;14:731–7. 10.1080/1744666X.2018.1512407 [DOI] [PubMed] [Google Scholar]
- 7.Karatzanis A, Chatzidakis A, Milioni A, et al. Contemporary use of corticosteroids in rhinology. Curr Allergy Asthma Rep 2017;17:11. 10.1007/s11882-017-0679-0 [DOI] [PubMed] [Google Scholar]
- 8.Bachert C, Pawankar R, Zhang L, et al. Icon: chronic rhinosinusitis. World Allergy Organ J 2014;7:25. 10.1186/1939-4551-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ten Brinke A, Sterk PJ, Masclee AAM, et al. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J 2005;26:812–8. 10.1183/09031936.05.00037905 [DOI] [PubMed] [Google Scholar]
- 10.Mendelsohn D, Jeremic G, Wright ED, et al. Revision rates after endoscopic sinus surgery: a recurrence analysis. Ann Otol Rhinol Laryngol 2011;120:162–6. 10.1177/000348941112000304 [DOI] [PubMed] [Google Scholar]
- 11.Valero A, Muñoz-Cano R, Sastre J, et al. The impact of allergic rhinitis on symptoms, and quality of life using the new criterion of ARIA severity classification. Rhinology 2012;50:33–6. 10.4193/Rhino11.071 [DOI] [PubMed] [Google Scholar]
- 12.Brożek JL, Bousquet J, Agache I, et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol 2017;140:950–8. 10.1016/j.jaci.2017.03.050 [DOI] [PubMed] [Google Scholar]
- 13.Sahlstrand-Johnson P, Ohlsson B, von Buchwald C, et al. A multi-centre study on quality of life and absenteeism in patients with CRS referred for endoscopic surgery. Rhinology 2011;49:7. [DOI] [PubMed] [Google Scholar]
- 14.Smith KA, Orlandi RR, Rudmik L. Cost of adult chronic rhinosinusitis: a systematic review. Laryngoscope 2015;125:1547–56. 10.1002/lary.25180 [DOI] [PubMed] [Google Scholar]