Description
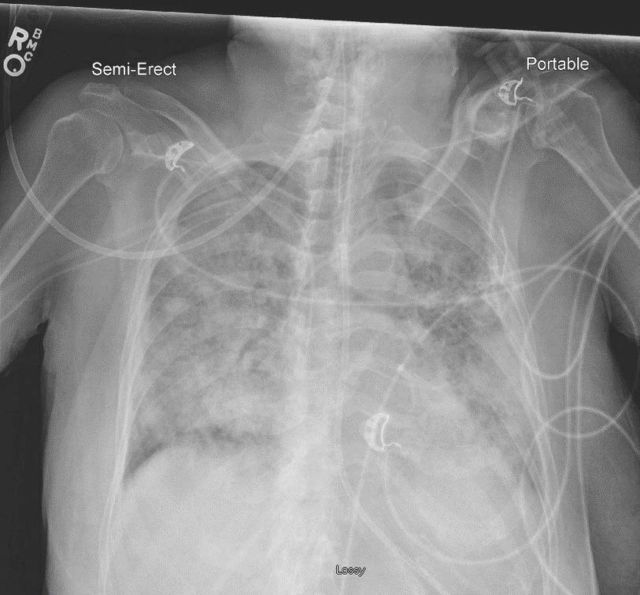
A 63-year-old woman with poorly controlled type 2 diabetes mellitus was admitted to the intensive care unit for increased respiratory support following large-volume fluid administration to treat diabetic ketoacidosis. The patient was intubated and diagnosed with mild acute respiratory distress syndrome; the clinical status was improving when a unit of blood was administered for chronic anaemia. Ten minutes into blood administration, the patient became acutely hypoxic (SpO2 70%) and hypertensive (200/100 mm Hg). Administration was halted, and a stat chest X-ray (CXR) obtained. Clinical examination was notable for prominent jugular venous distension, unremarkable on earlier examination. A morning CXR obtained 90 min prior (figure 1) was compared with the one obtained post-reaction (figure 2), demonstrating sudden, dramatic worsening of bilateral lung opacities. Supportive care was initiated with oxygen and diuresis, and the symptoms resolved 30 min following cessation of blood product administration. Investigation of blood products for human leukocyte antigen (HLA) antibodies and human neutrophil antigen (HNA) antibodies was initiated and ultimately was negative. It was determined that the clinical presentation and symptoms were most consistent with transfusion-associated circulatory overload (TACO).
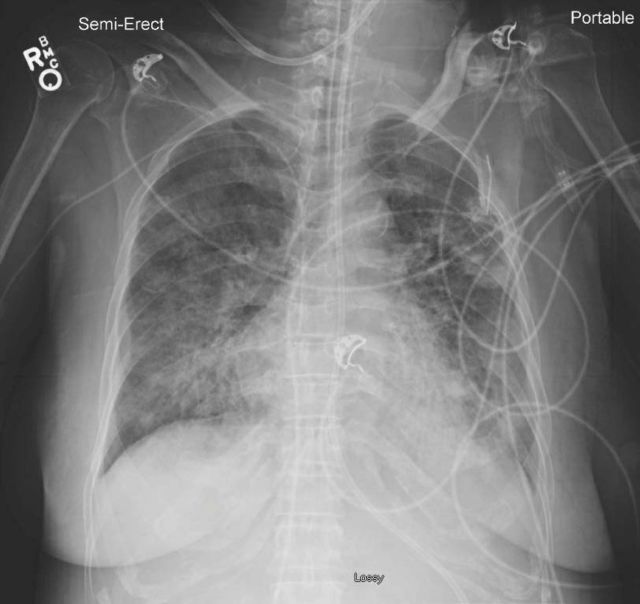
Figure 1.
Portable anteroposterior (AP) chest X-ray prior to transfusion. Diffuse bilateral airspace opacities.
Figure 2.
Portable AP chest X-ray post-transfusion. Complete bilateral airspace opacities.
TACO and transfusion-related acute lung injury (TRALI) are acute respiratory distress syndromes that are often difficult to distinguish.1 Several different clinical definitions of TACO and TRALI have been proposed by various societies.1 However, unifying themes among them are acute respiratory distress, new onset hypoxemia and bilateral pulmonary infiltrates on CXR that occur within 6 hours of a blood transfusion.1 2 TACO is the most frequent pulmonary-related transfusion complication and has recently surpassed TRALI as the leading cause of transfusion-related fatalities in the USA.3 The clinical presentation of TACO is related to pulmonary hydrostatic oedema and includes dyspnea, tachypnea, jugular venous distension and elevated systolic blood pressure.2 Conversely, the clinical presentation of TRALI is related to pulmonary permeability oedema, thought to occur secondary to the release of various leucocyte interleukins, and may include fever, hypotension, tachycardia and rarely a transient drop in the peripheral neutrophil count, though these features are often not present.2 B-type natriuretic peptide (BNP) may be a distinguishing biomarker, as increased myocardial stretching in TACO can be assessed with an increase in pre-transfusion to post-transfusion BNP.2 Frustratingly, treatment is supportive for both syndromes. When any transfusion lung injury is suspected, the transfusion should be immediately stopped. When TACO is suspected, treatment includes supplemental oxygen, diuresis and assisted ventilation when indicated. Supportive treatment for TRALI includes supplemental oxygen, judicious fluid administration and in severe instances ventilatory and pharmacologic pressure support. Strategies to prevent TACO include screening transfusion recipients for occult cardiac insufficiency and reducing the volume and rate of transfusions.1 Strategies to prevent TRALI include increased donor HLA antibody screening, using male only plasma donors, and donor deferral based on history of transfusion.1 These TRALI mitigation strategies have drastically reduced the incidence of TRALI with 35 cases in 2006 compared with 9 cases in 2017, as reported by the Food and Drug Administration.3 Clinicians should be aware of TRALI and TACO and strategies to avoid these complications prior to ordering blood transfusions.
Learning points.
Transfusion-associated circulatory overload (TACO) and transfusion-related acute lung injury (TRALI) are acute respiratory distress syndromes which occur within 6 hours of a blood transfusion and associated with high mortality.
Treatment of TACO and TRALI is largely supportive but intubation with pharmacologic pressure support may be required.
The incidence of TRALI can be reduced with increased donor screening. The incidence of TACO can be reduced with increased recipient screening.
Footnotes
Contributors: CMK contributed to the manuscript. CEM treated the patient and contributed to the manuscript. KFB provided edits.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1.Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury. Blood 2019;133:1840–53. 10.1182/blood-2018-10-860809 [DOI] [PubMed] [Google Scholar]
- 2.Gajic O, Gropper MA, Hubmayr RD. Pulmonary edema after transfusion: how to differentiate transfusion-associated circulatory overload from transfusion-related acute lung injury. Crit Care Med 2006;34(5 Suppl):S109–13. 10.1097/01.CCM.0000214311.56231.23 [DOI] [PubMed] [Google Scholar]
- 3.Fatalities Reported to Food and Drug Administration (FDA) Following Blood Collection and Transfusion; Annual Summary for Fiscal Year 2017. 2019. www.fda.gov/media/124796/downloads.