Abstract
We present a 26-year-old woman who came to the emergency department with chest pain of 1 hour duration that started while she was exercising on the treadmill. At presentation, ECG showed sinus bradycardia. Initial troponin level was 0.05 ng/mL and her chest pain resolved within 3 hours of onset. Troponins were trended serially, which continued to rise and peaked at 28.77 ng/mL and so heparin drip was started. On the second day of admission, a coronary angiogram was performed along with intravascular ultrasound, which revealed type 3 spontaneous coronary artery dissection. No obstructive atherosclerotic disease was noted in any of the coronary vessels. No coronary intervention was performed. Patient was started on aspirin and clopidogrel. Patient was discharged home in stable condition and was followed outpatient, where she remained in excellent health condition at her first clinic visit.
Keywords: cardiovascular medicine, sports and exercise medicine, interventional cardiology
Background
Spontaneous coronary artery dissection (SCAD) is an uncommon cause of acute coronary syndrome (ACS) in relatively younger female population without any risk factors of atherosclerotic coronary artery disease (CAD). It is responsible for 0.1%–0.4% of cases of ACS in the general population.1 Although the incidence of SCAD has been increasing in the last few decades, this is likely related to newer intravascular diagnostic modalities. The data regarding management of SCAD are scarce, and most of the currently available evidence are from case reports, case series and expert opinions. It is important to have a high index of suspicion for SCAD especially in young female patients who present with chest pain and elevated troponin in the absence of traditional cardiovascular disease risk factors.
Case presentation
We present a 26-year-old healthy woman who came to the emergency department with chest pain of 1 hour duration that started while she was exercising on the treadmill. The pain was retrosternal, sharp and radiated to both arms, 10/10 in intensity at onset, but improved to 5/10 by the time of presentation. She exercises 6 days a week doing cardio but never experienced a similar pain in the past. At presentation, she was loaded with aspirin and ECG showed sinus bradycardia. Initial troponin level was 0.05 ng/mL. Meanwhile, her chest pain resolved completely and she was admitted to the telemetry floor for serial troponin checks, which continued to rise and peaked at 28.77 ng/mL. Intravenous unfractionated heparin infusion was initiated, and a urine drug screen was obtained, which was negative for any substance abuse.
Investigations
Bedside two-dimensional transthoracic echocardiography was performed, which showed normal biventricular systolic function. Given the typical nature of her chest pain, a CT coronary angiography was performed, which showed normal coronaries without any atherosclerotic disease.
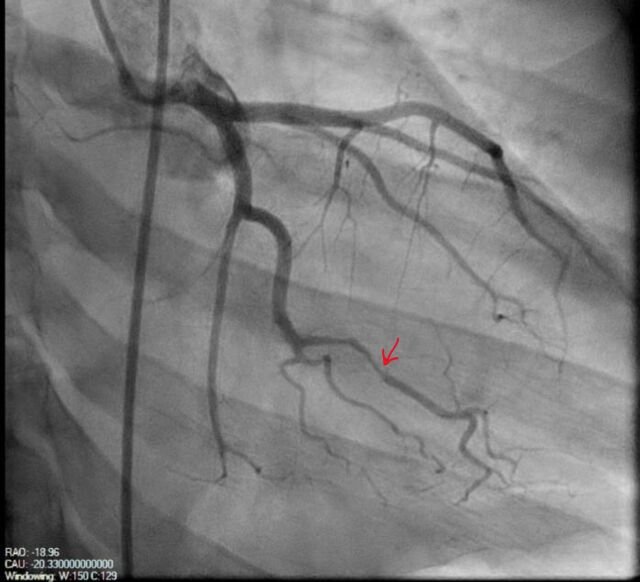
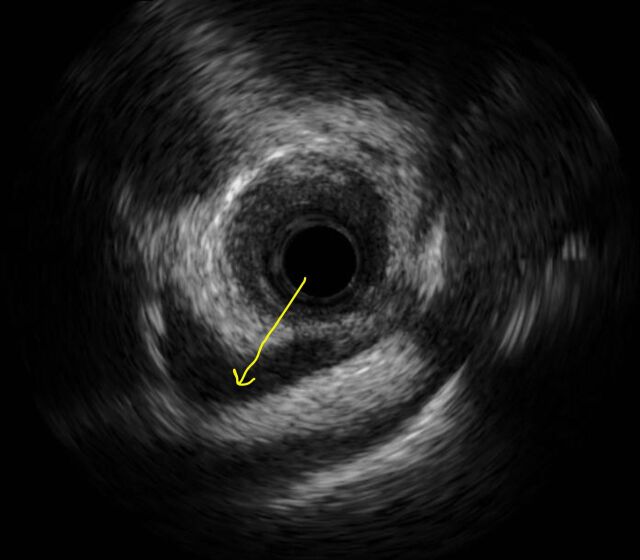
On the second day of admission, a coronary angiogram was performed along with intravascular ultrasound, which revealed an irregular lesion in first obtuse marginal branch of left circumflex artery with 80% luminal diameter reduction suggesting a type 3 SCAD (figures 1 and 2). No atherosclerotic disease was noted in any of the coronary vessels. Conservative approach was planned; hence, no coronary intervention was performed.
Figure 1.
Coronary angiogram showing stenosis of first obtuse marginal branch of left circumflex artery (red arrow).
Figure 2.
Coronary intravascular ultrasound scan showing intramural hematoma (yellow arrow).
Differential diagnosis
The differential diagnoses of patient’s presentation include obstructive coronary atherosclerosis, coronary vasospasm, aortic dissection and acute pericarditis. Obstructive coronary atherosclerosis is an important differential as it is the most common cause of ACS but was not the culprit in this patient as she was young, lacked the traditional cardiovascular disease risk factors like hypertension, diabetes mellitus and advanced age, and there was no evidence of atherosclerosis on coronary angiogram. Coronary vasospasm is a differential as it can present with typical chest pain as in this case but unlikely to give such a high level of troponin. Patient also did not smoke or use cocaine, which are known to be associated with coronary vasospasm. Aortic dissection is another differential but was unlikely as patient did not have hypertension or other cardiovascular risk factors, patient’s chest pain completely resolved a few hours after presentation, which will be unusual in aortic dissection. Acute pericarditis is yet another differential, this will likely have resulted in classic positional chest pain that improves with leaning forward and ECG findings of diffuse upward concave ST segment elevation except for aVR with PR segment depression, which were absent in our patient.
Treatment
Patient was started on dual antiplatelet therapy with aspirin and clopidogrel. Beta blocker was avoided because of patient’s sinus bradycardia.
Outcome and follow-up
Patient was discharged home in stable condition and was followed outpatient, where she remained in excellent health condition at her first clinic visit. Patient was followed up by phone about 2 years after discharge from the hospital and she remained in excellent health condition continuing to follow-up with her cardiologist annually with no recurrence of symptoms.
Discussion
SCAD is a non-iatrogenic and non-traumatic separation of the coronary artery wall and is an uncommon cause of acute myocardial infarction and is usually seen in younger women. Predisposing arteriopathies include atherosclerosis and non-atherosclerotic conditions like: fibromuscular dysplasia, pregnancy, connective tissue disorder (like Marfan syndrome, Ehlers-Danlos syndrome, alpha-1 antitrypsin deficiency and polycystic kidney disease), systemic inflammatory conditions (like systemic lupus erythematosus, Crohn’s disease, ulcerative colitis, polyarteritis nodosa, sarcoidosis and Celiac disease), hormonal therapy, coronary vasospasm and idiopathic.2 Precipitating stressors include labour and delivery, intense emotional stress, intense exercises (isometric or aerobic forms), intense valsalva-type activities (like vomiting, coughing and retching), recreational drugs (like cocaine and amphetamines) and intense hormonal therapy (like beta-Human chorionic gonadotropin injections).2 There are two theories of how SCAD develops. The first theory proposes that the primary pathological event is the development of a disruption in the vessel wall (intimal tear), which allows blood from the true lumen to enter and form a false lumen. The second theory proposes that the primary event is a spontaneous haemorrhage arising from the vasa vasorum within the vessel wall.3
The data regarding management of SCAD are scarce and most of the currently available evidence are from case reports, case series and expert opinions. Conservative therapy is the preferred option in most patients with SCAD, many patients have been managed with 1 year of clopidogrel and long-term aspirin in addition to statins in patients with dyslipidaemia.4 5 Our patient was managed conservatively with aspirin and clopidogrel but not with statin as she did not have dyslipidaemia. Patients who have thrombolysis in myocardial infarction 0–1 flow or clinically unstable should be revascularised and considered for Coronary Artery Bypass Graft surgery in high volume surgical centres. The reported rates of a recurrent episode of SCAD vary significantly (0%–37%).5 The information in this case report will not necessarily modify existing clinical practice but will rather add to the available body of evidence that supports the relationship between intense exercise and SCAD particularly in young women.2 This case report demonstrates the need for increased index of suspicion for SCAD in young women presenting with chest pain especially after intense exercise to achieve early diagnosis and provision of accurate and prompt treatment. Future research should be directed towards randomised controlled trials on the most effective management for SCAD, although this may be difficult given the low incidence of SCAD.
Patient’s perspective.
My experience at Einstein was great! I really appreciate all of the doctors and the full team that helped to diagnose me with this rare condition. This was such a scary time for my family and I seeing that I was a young, active and healthy woman who had a heart attack. From the moment I stepped into Einstein, they were very accommodating, understanding and kept me informed along the way. The communication was excellent and there was never a time when I felt that I did not know what was going on with my body. I appreciate all of the time, research and effort that the doctors put into my case.
Learning points.
Always consider the possibility of SCAD in a young woman presenting with typical chest pain.
Current evidence for management of SCAD are based on case reports, case series and expert opinions; although conservative management makes sense as it is less invasive, management should be individualised.
Coronary angiography is the modality of choice for diagnosing SCAD. Intravascular imaging may further help in confirming the diagnosis.
SCAD requires absence of coronary atherosclerosis as part of the criteria for angiographic definition.
Footnotes
Contributors: ASO and HUIHV contributed to planning, conduct, reporting, conception, design, acquisition and interpretation of data. CW contributed to planning, conduct, reporting, conception, design and interpretation of data.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mortensen KH, Thuesen L, Kristensen IB, et al. Spontaneous coronary artery dissection: a Western Denmark heart registry study. Catheter Cardiovasc Interv 2009;74:710–7. 10.1002/ccd.22115 [DOI] [PubMed] [Google Scholar]
- 2.Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645. 10.1161/CIRCINTERVENTIONS.114.001760 [DOI] [PubMed] [Google Scholar]
- 3.Kwon T-G, Gulati R, Matsuzawa Y, et al. Proliferation of coronary adventitial vasa vasorum in patients with spontaneous coronary artery dissection. JACC Cardiovasc Imaging 2016;9:891–2. 10.1016/j.jcmg.2015.11.030 [DOI] [PubMed] [Google Scholar]
- 4.Tweet MS, Eleid MF, Best PJM, et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777. 10.1161/CIRCINTERVENTIONS.114.001659 [DOI] [PubMed] [Google Scholar]
- 5.Hayes SN, Kim ESH, Saw J, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American heart association. Circulation 2018;137:e523–57. 10.1161/CIR.0000000000000564 [DOI] [PMC free article] [PubMed] [Google Scholar]