Abstract
BACKGROUND:
Vaginal birth is a risk factor for pubovisceral muscle tear, decreased urethral closure pressure, and urinary incontinence. The relationship between these three factors is complicated. Urinary continence relies on maintaining urethral closure pressure; particularly when low urethral closure pressure can usefully be augmented by a volitional pelvic muscle (Kegel) contraction just before and during stress events like a cough. However, it is unknown whether a torn pubovisceral muscle decreases the ability to increase urethral closure during an attempted pelvic muscle contraction.
OBJECTIVE:
We tested the null hypothesis that a pubovisceral muscle tear does not affect the ability to increase urethral closure pressure during a volitional pelvic muscle contraction in the Evaluating Maternal Recovery from Labor and Delivery (EMRLD) study.
STUDY DESIGN:
We studied 56 women 8 months after their first vaginal birth. All had at least one risk factor for pubovisceral muscle tear (e.g., forceps and long 2nd stage). A tear was assessed bilaterally by magnetic resonance imaging. Urethral closure pressure was measured both at rest and during an attempted volitional pelvic muscle contraction. Student’s t test was used to compare urethral closure pressures. Multiple linear regression was used to estimate the effect of a magnetic resonance imaging-confirmed pubovisceral muscle tear on volitionally contracted urethral closure pressure after adjusting for resting urethral closure pressure.
RESULTS:
The mean age was just over 30 years with the majority being Caucasian. By magnetic resonance imaging measure, unadjusted for other factors, the 21 women with tear had significantly lower urethral closure pressure during an attempted contraction compared to the 35 women without tear (65.9 vs 86.8 cm H2O respectively, P=.004), leading us to reject the null hypothesis. No significant group difference was found in resting urethral closure pressure. After adjusting for resting urethral closure pressure, pubovisceral muscle tear was associated with lower urethral closure pressure (beta = − 21.1, P=.001).
CONCLUSIONS:
In the first postpartum year the presence of a pubovisceral muscle tear did not influence resting urethral closure. However, women with a pubovisceral muscle tear achieved a 25% lower urethral closure pressure during an attempted pelvic muscle contraction than those without a pubovisceral muscle tear. These women with pubovisceral muscle tear may not respond to classic behavioral interventions, such as “squeeze when you sneeze” or strengthen through repetitive pelvic muscle exercises. When a rapid rise to maximum urethral pressure is used as a conscious volitional maneuver, it appears to be reliant on ability to recruit the intact pubovisceral muscle in order to simultaneously contract the urethral striated muscle.
Keywords: Birth-related injury, Kegel, levator ani tear, lower urinary tract symptoms, pelvic muscle defect, pelvic muscle exercise, pelvic floor muscle training, prevention, stress urinary incontinence, urodynamics
Introduction
Estimates of the prevalence of urinary incontinence range from approximately 5% to 70% of women.1 The most common type of incontinence is stress urinary incontinence (SUI)2 caused by inadequate urethral closure pressure (UCP), as defined by the arithmetic difference between urethral pressure and bladder pressure.3 An increase in bladder pressure due to an increase in intraabdominal pressure can then cause involuntary urine loss during physical activities, such as lifting, coughing, or sneezing.4–5
To prevent leakage, it has been shown that an intentional increase in UCP can be achieved by volitionally contracting the pelvic muscles just before and during the rise in intraabdominal pressure. The timing of this skilled maneuver (termed the ‘Knack’ in the studies that tested its ability to reduce leakage when a Kegel contraction was timed with a cough), can be learned to be a consciously activated preventive behavior implemented as an adaptive response6 to expected urine leakage.7–8 However, these Knack studies also observed a substantial number of women demonstrating leakage with cough who were unable to reduce that leakage, and sometimes trying to do so with the Knack made it worse.7–8 This observation raises the possibility that a birth-related muscle tear might adversely affect the efficacy of this maneuver.
The pubovisceral muscle (PVM), the ventral-most portion of the pelvic floor muscles, acts on either side of the urethra, helping to stabilize it during increases in intraabdominal pressure by preventing its movement caudally. Because of the PVM body’s proximity to the urethra, its lines-of-action and ability to elevate the mid urethra9 during a volitional contraction, we hypothesized that a PVM tear adversely affects a woman’s potential to raise her UCP during volitional pelvic muscle contraction. The PVM is the portion of the levator ani most vulnerable to being torn from the pubic bone during vaginal birth.10–12
Birth-related PVM tears are well-documented.13–14 In women with specific risk factors associated with vaginal birth experience up to 66% have been known to experience PVM tears.14 Although the association between the presence of a PVM tear (partial or complete) and SUI is presently unknown, an inverse relationship between SUI and UCP is known. A low resting UCP is well accepted to be a primary cause of the leakage15–16 because it is generally accepted that a resting UCP greater than 60 cm H2O is necessary for continence.
We therefore tested the hypothesis that a PVM tear adversely affects a woman’s potential to raise her UCP during volitional pelvic muscle contraction.
Materials and Methods
Study population
This was a planned secondary analysis of women from the parent study, Evaluating Maternal Recovery from Labor and Delivery (EMRLD). Institutional Review Board approval was obtained (HUM #00051193) which included informed consent. This longitudinal observational cohort study of women within the first year after childbirth was designed to determine whether a birth-related PVM “defect” on MRI was indicative of a torn muscle, as opposed to nerve- or crush-related childbirth injury. The hypothesis of tear was supported.13
Parent study inclusion criteria included primiparous postpartum women who delivered vaginally, with at least one potential risk factor for PVM tear: maternal age greater than 33 years, second stage of labor greater than 150 minutes or less than 30 minutes, infant weight greater than 4,000 gm, instrumented delivery, or anal sphincter laceration, as reported elsewhere.13,17 In the parent study, clinical assessments occurred early postpartum (7 weeks) and later postpartum (8 months). For this paper, fifty-six women form the sample (Figure 1). All had MRI-documented PVM status and UCP measures made at the 8-months postpartum timepoint.
Figure 1.
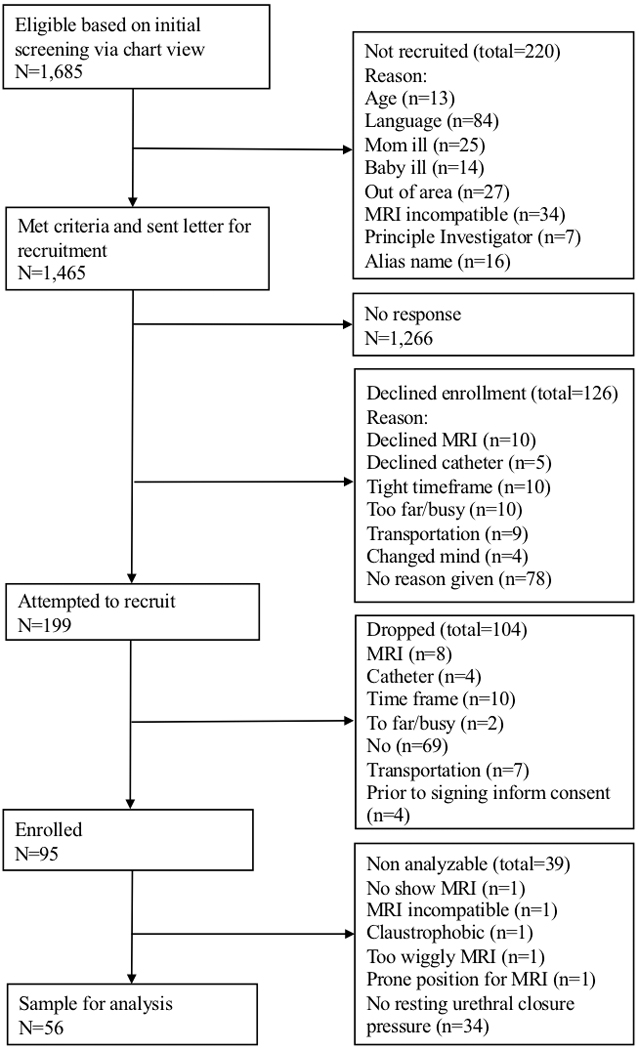
Flow diagram for selection of study participants
MRI, magnetic resonance imaging.
Instruments
Urethral Pressure Measures:
Urethral pressure profiles were conducted using the classic techniques described by Hilton and Stanton,18 as discussed in previous research. 19–20 Women lay in a semi-recumbent lithotomy position while a 6 F Millar catheter, with dual pressure transducers separated by 5 cm, was inserted into the bladder, which was noted when both transducers read the same relatively low resting pressures. Women were then asked to stay in relaxed condition while the catheter was hand-pulled by the examiner through the urethra until the second transducer reached a highest pressure point in the urethra, with the first transducer remaining in the bladder. Resting UCP was then calculated as the arithmetic difference between highest urethral resting pressure and within-bladder resting pressure. Similarly, to obtain contracting urethral pressure, women were coached to attempt pelvic muscle contraction without any visible straining down. Once lack of straining was confirmed, the second transducer was again returned to that point of highest resting urethral pressure, and held at that point while the woman was asked to attempt a volitional pelvic muscle contraction without straining (if straining was observed, the coaching to not strain was repeated and the measurement was repeated). Contracting UCP was then calculated as the arithmetic difference between the peak urethral pressure during volitional contraction and the bladder pressure during contraction state. For both resting and contracting UCP, measures were obtained twice.
Pubovisceral Muscle Measures:
The parent study used MRI as the diagnostic assessment for PVM tear, with details reported elsewhere.13,21 In brief, the measures used a 3T Philips Achieva (Philips Medical System, Eindhoven, The Netherlands) with an eight channel cardiac coil. Two millimeter slices thickness for images were obtained in the coronal, axial, and sagittal planes with proton density-weighted sequences and additional tailored imaging additionally to obtain better definition of the anterior pelvic floor anatomy. The MRIs were evaluated for discontinuity of PVM fibers or loss of visible muscle by a board-certified, fellowship-trained MSK radiologist blinded as to UCP status.
Data reduction and management
With two values for both resting UCP and contracting UCP, as defined above, we used the higher of the two as ‘best effort’ measure rather than averaging. For the MRI readings, gradings for each side of the PVM were combined into a dummy variable. Gradings of No PVM tear were coded as “0” (no tear or subtle on both sides). Any PVM tear was coded as “1” (any grading greater than “subtle” on at least one side).
Data analysis
Mean (standard deviation) and ranges were calculated for continuous data and frequencies (percentages) for categorical data for our sample characteristics, including age, body mass index (BMI), race, education, and positive standing stress test. For the UCP variables, an independent two-sided t test was performed to test the significance of the difference between groups by PVM status. Levene’s test was used to test the equality of variances between the two independent groups. Pairwise comparison was performed using a two-sided, paired t-test to compare the difference of the mean resting UCP and mean contracting UCP within each PVM tear group.
A multiple linear regression model was conducted to examine the effect of PVM tear on the contracting UCP after adjusting for resting UCP. A Wald chi-squared test was used to check the significance of the effect. A preliminary analysis was conducted to check whether assumptions for linear regression were met. A linear relationship between contracting UCP and PVM tear was checked by a plot of the standardized residuals versus the predicted Y values. Normality (for error, not outcome) was tested by normal Q-Q plot and was also checked with a goodness of fit test, Kolmogorov-Smirnov test, and Shapiro-Wilk test. Potential multicollinearity of independent variables was tested by the variance inflation factor statistic less than 10, indicating the variables were independent. Autocorrelation in residuals from regression analysis was tested with the Durbin-Watson test (1.5 < d < 2.5 show no auto-correlation). All statistical analyses were carried out using SPSS statistical software (Version 25; IBM SPSS Inc, Chicago IL). The results were considered to achieve the significance when p value was less than 0.05.
Results
Mean age of participants was 30.1 years with a range of 20–42 years for the group without PVM tear (n = 35) and 31.8 years with range of 19–46 years for the group with PVM tear (n = 21) (Table 1). Most participants had at least some college education and were white. Only 4 women demonstrated SUI on a standing stress test at the 8-month postpartum timepoint for this report. There were no differences in age, education, race, BMI or leakage between the groups with and without PVM tear. Among the 56 women, 35 (62%) had none or only a subtle PVM tear, and 21 (38%) had some degree of PVM tear.
Table 1.
Characteristics of participants by status of pubovisceral muscle tear
| No pubovisceral muscle tear (N= 35) | Pubovisceral muscle tear (N = 21) | ||||
|---|---|---|---|---|---|
| Characteristics | Mean (SD) or count | Range or % | Mean (SD) or count | Range or % | Pvalue |
| Age, y | 30.1 (5.2) | 20 – 42 | 31.8 (6.1) | 19 – 46 | .255 |
| Education level | 34 | .700 | |||
| High school graduate or less | 1 | 3% | 1 | 5% | |
| Some college | 7 | 21% | 4 | 19% | |
| College/technical school graduate | 11 | 32% | 4 | 19% | |
| Graduate school | 15 | 44% | 12 | 57% | |
| Race | 34 | .700 | |||
| African-American | 2 | 6% | 0 | 0% | |
| White | 29 | 85% | 19 | 90% | |
| Asian | 2 | 6% | 1 | 5% | |
| Other Race | 1 | 3% | 1 | 5% | |
| Body mass index, kg/m2 | 25.6 (5.7) | 17.6 – 43.5 | 24.8 (5.4) | 17.2 – 37.6 | .591 |
| Positive standing stress test | 1 | 3% | 3 | 15% | .095 |
Chi-squared test was applied to categorical variables and independent t-test for continuous variables.
Table 2 shows results of urethral pressure profiles by status of MRI-documented PVM tear and test condition (at rest and during an attempted pelvic muscle contraction). The average resting UCPs were similar between groups (68.2 cm H2O in women with tear vs 67.9 cm H2O in women without PVM tear; P=.958). The average contracting UCP differed between those with and without PVM tear (65.9 cm H2O vs 86.8 cm H2O, respectively; P=.004). Women with a PVM tear had about 25% ((86.8–65.9)/86.8) lower UCP during an attempted pelvic muscle contraction compared with those without the tear. Resting UCP and contracting UCP differed in women without PVM tear (P<.001), but they were similar in women with PVM tear (P=.602).
Table 2.
Group differences in urethral closure pressures by status of MRI-documented pubovisceral muscle tear
| UCP (cm H2O) | No PVM tear, N = 35 Mean (SD) | PVM tear, N = 21 Mean (SD) | P value |
|---|---|---|---|
| Resting UCP | 67.9 (22.5) | 68.2 (19.0) | .958 |
| Contracting UCP | 86.8 (27.4) | 65.9 (21.3) | .004* |
| P value | < .001* | .602 |
Two urethral closure pressure states (at rest and during attempted PVM contraction) are provided for the two groups of women at 8 months postpartum: One group with PVM tear by MRI and the other group without PVM tear by MRI.
MRI,magnetic resonance imaging; SD, standard deviation; UCP, urethral closure pressure; PVM, pubovisceral muscle.
indicated the significance at the level of P < .05
The regression model showed that PVM tear was associated with lower contracting UCP after adjusting for resting UCP (P=.001, Table 3). Mean contracting UCP was lower in women with PVM tear by an average of 21.1 cm H2O pressure compared to women without tear after adjusting for resting UCP. Given PVM tear status, mean contracting UCP increased by 6.7 cm H2O pressure for every 10 cm H2O pressure increase in resting UCP. Forty-two percent of the total variation in contracting UCP was explained by PVM tear and resting UCP. When standardized coefficients (β) for independent variables were used to compare the effects on the dependent variable, the higher the absolute value of the β, the stronger the effect of the independent variable on the dependent variable, controlling for other independent variables. The standardized βs for PVM tear and resting UCP were 0.4 and 0.5 respectively, and both were statistically significant (P<.05). This indicates that PVM tear and resting UCP have approximately equally important effects on UCP during an attempted contraction.
Table 3.
Association of MRI-documented pubovisceral muscle tear with urethral closure pressure during an attempted PVM contraction among postpartum women
| Contracting UCP (cm H2O) (N = 56) | ||||
|---|---|---|---|---|
| Variables | Unstandardized coefficients (B) | Std. error of B | Standardized coefficients (β) | PValue |
| MRI-documented PVM tear (vs. no tear) | −21.1 | 5.8 | −0.4 | .001* |
| Resting UCP (per each 10 cm H2O) | 6.7 | 1.4 | 0.5 | < .001* |
indicates the significance at the level of P < .05, R2 = .42.
MRI, magnetic resonance imaging; PVM, pubovisceral muscle; UCP, urethral closure pressure.
Comment
Principal findings
The new finding in this study of women in their first postpartum year who had a risk factor for birth-related PVM tear is that those with tear had a lower UCP during an attempted pelvic muscle contraction than those without. It is noteworthy that the women with a PVM tear exhibited no increase in UCP from the resting value when they attempted a volitional contraction.
Clinical implications/interpretation of the findings
Our findings suggest that the presence of the tear was associated with a reduced ability to volitionally increase their UCP. These findings corroborate and extend the results from a study that reported a negative relationship between PVM tear and the degree of increased UCP during a pelvic muscle contraction.22 The results are also supported by a second study showing that women with PVM loss had a 50% decreased ability to increase UCP by a contraction.20 A systematic review found that the degree of increased UCP during a contraction varied widely.23 We speculate that those results could be explained by the combination of PVM tear and resting UCP differences, though the underlying mechanism was not revealed in that sample of 21 women, some with and others without urinary incontinence.
Our findings are not consistent with a prior study reporting no significant difference in UCP during a pelvic muscle contraction between women with and without PVM tear one year postpartum.19 This inconsistency may be attributable to the larger percentage of women with PVM tear in the present study, 38%, compared to only 18% in Brincat’s study, as well as the different study designs. The participants in Brincat’s study came from a case-control parent study, half of whom had SUI within one year postpartum, the other half having no symptoms at any time in life. Hence, it is conceivable that, compared to our sample, the resting UCP of the Brincat’s group was lower in the SUI group even before any of those women gave birth, whereas our sample was selected solely on the basis of obstetric risk factors for PVM injury.
The majority of studies15–16,24 have focused on resting UCP rather than UCP during a pelvic muscle contraction in incontinent women, despite the fact that resting UCP is not recommended as a diagnostic test for SUI.25 Our findings in regard to the effect of a PVM tear on UCP during a contraction may help explain why parous women seem more likely to develop SUI over time. The underlying mechanism is still not clear. The speculation that women sustaining a PVM tear during vaginal birth are also more likely to have also sustained an injury to their urethral sphincter muscles (via denervation or prolonged compression, for example26) is not supported by these data. This is because the presence or absence of PVM tear did not affect resting UCP, one-third of which is contributed equally by the urethral vascular plexus, smooth and striated muscle.27 It is possible that the loss of contracting urethral pressure during an attempted pelvic muscle contraction in a woman with a PVM tear could be due to her no longer being able to correctly sense how to contract her PVM, and by extension her urethral striated muscle when that contraction is needed to prevent leakage prior to and during a cough. However, that hypothesis remains to be tested and we have no data-based explanation as to why the volitional increase in UCP was affected by the presence of a PVM tear but resting UCP was not. Clearly a knowledge gap remains.
Consistent with Brincat’s results,19 our data reported no association between PVM tear and resting UCP. However, the results in both studies differ from other reports that women with major PVM tear showed significantly lower resting UCP compared to women with none or mild PVM tear.28–29 The inconsistency may simply be due to age differences. For example, the present study and Brincat’s19 study both focused on postpartum women, whereas the other reports included women beyond reproductive years. Aging may be the main contributor to lower resting UCP in previous work since resting UCP is known to decrease with age for both incontinent30–31 and nulliparous continent women.25,32 While a torn muscle may not cause a problem with resting UCP in young women, as resting pressure decreases with increasing age,33 the impact of the torn muscle on the ability to optimize urethral pressure under situations of intraabdominal pressure rise (such as a cough or sneeze) may be compromised.
Lower resting UCP and higher tear rate has previously been documented in incontinent women when compared to continent women.15–16,24 We were unable to determine in the present study whether women with a torn PVM and low contracting UCP were more likely to develop SUI since only four women had leakage in the quantified standing paper towel test, three of whom had PVM tear at 8 months. Further work might focus on whether a torn PVM is a risk factor for developing SUI over time. Within the clinical setting, using palpatory assessment34 to attempt to locate the PVM body through the vaginal wall, may help clinician and patient understand why stress-induced leakage is not responsive to behavioral interventions such as Knack maneuver7–8 or pelvic muscle strengthening exercises. Using the quantitative standing paper towel test with and without volitional contraction35,36 can also help confirm lack of adequate urethral pressure rise. Taken together, counseling the woman regarding her lower likelihood of response to these otherwise evidence-based therapeutic interventions may be appropriate, especially when difficulty to refrain from straining down is present. A pessary trial or consideration of surgical approaches to provide adequacy of urethral pressure may be indicated if leakage is severe enough.
Strengths and limitations
A strength of the present study is that only women of reproductive age were included allowing us to minimize the influences of aging on UCP. The focus on only women with risk factors for PVM tear provided an enriched sample of those with PVM tear, hence greater statistical power. Our measure for assessing the PVM employed gold-standard MRI and our results show the effects of the compromised PVM state on UCP during a contraction.
Limitations of our study include a small sample size and the fact that the results from these postpartum women might not generalize to study populations recruited for reasons other than having risk factors for PVM tear. Other potential confounding factors not considered due to the nature of the data collection might have affected our results. For example, to measure the UCP during a contraction the pressure transducer was located in the mid urethra at the point of highest resting UCP. A successful PVM contraction might have elevated the mid urethra relative to the urethral pressure transducer on the catheter thereby causing the transducer to read luminal pressure more distally in the urethra where the pressure is lower. This would have caused women with torn PVM to appear to have higher UCP during a pelvic muscle contraction (i.e., mid urethra and transducer remain in apposition at highest resting pressure site) rather than the lower pressures that we actually observed in the cases with torn PVM. Hence, it is reasonable to conclude that the transducer did not shift distally in the women with torn PVM. On the other hand, for women with intact PVM, we likely underestimated their UCP during a contraction since they are likely to have been able to elevate their mid urethra relative to the urethral transducer, resulting in a lower apparent UCP than we should have recorded had the transducer been allowed to move with the mid urethra.
Conclusions
A vaginal birth-related PVM tear has a negative impact on a woman’s ability to use a pelvic muscle contraction to volitionally and rapidly increase her UCP. The results highlight why commonly prescribed self-care practices, such as pelvic floor muscle training, may not work for all patients and offer an explanation as to why that may be the case.
AJOG at a Glance.
A. What was this study conducted?
We tested the null hypothesis that a pubovisceral muscle tear does not influence urethral closure pressure during an attempted volitional pelvic muscle contraction.
B. Key Findings
At 8 months postpartum, with at least one risk factor for pubovisceral muscle tear for their first vaginal childbirth, women with pubovisceral muscle tear exhibited a significantly lower urethral closure pressure during an attempted volitional pelvic muscle contraction than women without the tear (86.8 vs. 65.9 cm H2O, respectively). There was, however, no significant difference in resting urethral closure pressure between those with and without a tear.
C. What does this add to what is known?
A pubovisceral muscle tear was associated with a 25% lower increase in urethral closure pressure during an attempted volitional contraction.
Acknowledgements
The Evaluating Maternal Recovery from Labor and Delivery (EMRLD) study is grant-supported by the National Institutes of Health (NIH) through the Office for Research on Women’s Health Specialized Center of Research (SCOR) on Sex and Gender Factors Affecting Women’s Health and National Institute on Child and Human Development (Grant #P50 HD044406 002) and the National Institute on Child and Human Development (Grant #R21 HD049818).
Source of Funding/Role of the Funding Source: The Evaluating Maternal Recovery from Labor and Delivery (EMRLD) study is grant-supported by the National Institutes of Health (NIH) through the Office for Research on Women’s Health Specialized Center of Research (SCOR) on Sex and Gender Factors Affecting Women’s Health and National Institute on Child and Human Development (Grant #P50 HD044406 002) and the National Institute on Child and Human Development (Grant #R21 HD049818). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or its institutes. The sponsor had no involvement in study design; collection, analysis, and interpretation of data; writing of the report; or decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosure: The authors report no conflict of interest.
Condensation: Urethral capacity differs when studied in women with and without pubovisceral muscle tear (lay term, torn Kegel muscle) at 8 months postpartum.
References
- 1.Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217–222. doi: 10.1080/13697137.2018.1543263 [DOI] [PubMed] [Google Scholar]
- 2.Reynolds WS, Dmochowski RR, Penson DF. Epidemiology of stress urinary incontinence in women. Curr Urol Rep. 2011;12(5):370–6. doi: 10.1007/s11934-011-0206-0 [DOI] [PubMed] [Google Scholar]
- 3.Ashton-Miller JA, DeLancey JO. Functional anatomy of the female pelvic floor. Ann N Y Acad Sci. 2007;1101:266–96. [DOI] [PubMed] [Google Scholar]
- 4.Abrams P, Andersson KE, Birder L, et al. Fourth international consultation on incontinence recommendations of the international scientific committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29(1):213–40. doi: 10.1002/nau.20870 [DOI] [PubMed] [Google Scholar]
- 5.Haylen BT, De Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21:5–26. [DOI] [PubMed] [Google Scholar]
- 6.Villot A, Deffieux X, Billecocq S, Auclair L, Amarenco G, & Thubert T. Influence of cognitive rehabilitation on pelvic floor muscle contraction: a randomized controlled trial. Neurourol Urodyn. 2017;36:1636–44. [DOI] [PubMed] [Google Scholar]
- 7.Miller JM, Ashton-Miller JA, DeLancey JO. A pelvic muscle precontraction can reduce cough-related urine loss in selected women with mild SUI. J Am Geriatr Soc. 1998;46(7):870–4. [DOI] [PubMed] [Google Scholar]
- 8.Miller JM, Sampselle C, Ashton-Miller JA, Hong GR, DeLancey JO. Clarification and confirmation of the Knack maneuver: the effect of volitional pelvic floor muscle contraction to preempt expected stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):773–82. doi: 10.1007/s00192-007-0525-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betschart C, Kim J, Miller JM, Ashton-Miller JA, DeLancey JO. Comparison of muscle fiber directions between different levator ani muscle subdivisions: in vivo MRI measurements in women, Int Urogynecol J. 2014;25(9):1263–8. doi: 10.1007/s00192-014-2395-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG: An Int J Obstet Gynaecol. 2006;113(2): 225–30. [DOI] [PubMed] [Google Scholar]
- 12.Kim J, Betschart C, Ramanah R, Ashton-Miller JA, DeLancey JOL. Anatomy of the pubovisceral muscle origin: Macroscopic and microscopic findings within the injury zone. Neurourol Urodyn. 2015;34(8):774–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller JM, Low LK, Zielinski R, Smith AR, DeLancey JO, Brandon C. Evaluating maternal recovery from labor and delivery: bone and levator ani injuries. Am J Obstet Gynecol. 2015;213(2):188.e1–188.e11. doi: 10.1016/j.ajog.2015.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol. 2012;39(4):372–83. doi: 10.1002/uog.11080 [DOI] [PubMed] [Google Scholar]
- 15.DeLancey JO, Trowbridge ER, Miller JM et al. Stress urinary incontinence: Relative importance of urethral support and urethral closure pressure. J Urol. 2008;179(6):2286–90. doi: 10.1016/j.juro.2008.01.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeLancey JO. Why do women have stress urinary incontinence? Neurourol Urodyn. 2010;29 (Suppl 1):S13–17. doi: 10.1002/nau.20888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Low KL, Zielinski R, Tao Y, Galecki A, Brandon CJ, Miller JM. Predicting birth-related levator ani tear severity in primiparous women: Evaluating Maternal Recovery from Labor and Delivery (EMRLD study). Open J Obstet Gynecol. 2014;4(6):266–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hilton P, Stanton SL. Urethral pressure measurement by microtransducer: the results in symptom-free women and in those with genuine stress incontinence. Br J Obstet Gynaecol. 1983;90(10):919–33. [DOI] [PubMed] [Google Scholar]
- 19.Brincat CA, DeLancey JO, Miller JM. Urethral closure pressures among primiparous women with and without levator ani muscle defects. Int Urogynecol J. 2011. ;22(12):1491-doi: 10.1007/s00192-011-1458-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller JM, Umek WH, DeLancey JO, Ashton-Miller JA. Can women without visible pubococcygeal muscle in MR images still increase urethral closure pressures? Am J Obstet Gynecol. 2004;191(1):171–5. [DOI] [PubMed] [Google Scholar]
- 21.Brandon C, Jacobson J, Low L et al. Pubic bone injuries in primiparous women: magnetic resonance imaging in detection and differential diagnosis of structural injury. Ultrasound Obstet Gynecol. 2012;39(4):444–51. doi: 10.1002/uog.9082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dietz HP, Shek KL. Levator function and voluntary augmentation of maximum urethral closure pressure. Int Urogynecol J. 2012;23(8):1035–40. doi: 10.1007/s00192-012-1705-3 [DOI] [PubMed] [Google Scholar]
- 23.Zubieta M, Carr RL, Drake MJ, B0 K. Influence of voluntary pelvic floor muscle contraction and pelvic floor muscle training on urethral closure pressures: a systematic literature review. Int Urogynecol J. 2016;27(5):687–96. doi: 10.1007/s00192-015-2856-9 [DOI] [PubMed] [Google Scholar]
- 24.DeLancey JO, Miller JM, Kearney R et al. Vaginal birth and de novo stress incontinence: Relative contributions of urethral dysfunction and mobility. Obstet Gynecol. 2007;110(2 Pt 1):354–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kapoor DS, Housami F, White P, Swithinbank L, Drake M. Maximum urethral closure pressure in women: normative data and evaluation as a diagnostic test. Int Urogynecol J. 2012;23(11):1613–8. doi: 10.1007/s00192-012-1770-7 [DOI] [PubMed] [Google Scholar]
- 26.Smith AR, Hosker GL, Warrell DW. The role of pudendal nerve damage in the aetiology of genuine stress incontinence in women. Br J Obstet Gynaecol. 1989;96(1):29–32. [DOI] [PubMed] [Google Scholar]
- 27.Rud T, Andersson K-E, Assmussen M, Hunting A, Ulmsten U, Factors Maintaining the Urethral Closure Pressure in Women. Investigative Urol. 1980;17(4): 343–7. [PubMed] [Google Scholar]
- 28.Morgan DM, Cardoza P, Guire K, Fenner DE, DeLancey JO. Levator ani defect status and lower urinary tract symptoms in women with pelvic organ prolapse. Int Urogynecol J. 2010;21(1):47–52. doi: 10.1007/s00192-009-0970-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hegde A, Aguilar VC, Davila GW. Levator ani defects in patients with stress urinary incontinence: three-dimensional endovaginal ultrasound assessment. Int Urogynecol J. 2017;28(1):85–93. doi: 10.1007/s00192-016-3068-7 [DOI] [PubMed] [Google Scholar]
- 30.Murphy M, Culligan PJ, Graham CA, Kubik KM, Heit MH. Is the leak-point pressure alone an accurate indicator of intrinsic sphincteric deficiency? Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(5):294–7. [DOI] [PubMed] [Google Scholar]
- 31.Pfisterer MH, Griffiths DJ, Schaefer W, Resnick NM. The effect of age on lower urinary tract function: a study in women. J Am Geriatr Soc. 2006;54(3):405–12. [DOI] [PubMed] [Google Scholar]
- 32.Trowbridge ER, Wei JT, Fenner DE, Ashton-Miller JA, DeLancey JO. Effects of aging on lower urinary tract and pelvic floor function in nulliparous women. Obstet Gynecol. 2007;109(3):715–20. [DOI] [PubMed] [Google Scholar]
- 33.Rud T. Urethral pressure profile in continent women from childhood to old age. Acta Obstet Gynecol Scand. 1980;59(4):331–5. [DOI] [PubMed] [Google Scholar]
- 34.Sheng Y, Low LK, Liu X, Ashton-Miller JA, Miller JM. Association of index finger palpatory assessment of pubovisceral muscle body integrity with MRI-documented tear. Neurourol Urodyn. 2019;38(4):1120–28. doi: 10.1002/nau.23967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller JM, Ashton-Miller JA, DeLancey JOL. Quantification of cough-related urine loss using the paper towel test. Obstet Gynecol. 1998;91(5):705–9. [DOI] [PubMed] [Google Scholar]
- 36.Miller JM, Ashton-Miller JA, Carchidi LT, DeLancey JOL. On the lack of correlation between self-report and urine loss measured with standing provocation test in older stress-incontinent women. J Womens Health. 1999;8(2):157–62. [DOI] [PubMed] [Google Scholar]


