1. Introduction
COVID-19, a severe viral respiratory infection caused by SARS-CoV-2, affects all age groups, yet it is more severe in elderly and individuals with co-morbidities. Recently, a severe multi-system inflammatory syndrome has been reported in individuals <21 years of age. This document details our multidisciplinary approach to this syndrome, and discusses current knowledge on the case definition and clinical manifestations, and proposes guidelines on diagnosis and treatment. As many of these children may deteriorate quickly and initially present to non-tertiary care facilities, a general guide for an approach to such children is warranted.
Recent reports from Europe and the United States support the emergence of a new phenomenon with significant hyperinflammatory response in previously healthy asymptomatic children related to SARS-CoV-2 infection. COVID-19 is the clinical presentation of acute disease associated with infection by the betacoronavirus SARS-CoV-2. Severe respiratory disease is the most concerning clinical presentation in adult patients. Initial reports during the pandemic suggested children have milder illness during acute infection [1]. Recent reports suggest a new COVID-19 related clinical syndrome, with significant inflammation and similarities to Kawasaki disease (KD), can present in children. Some children have had features of toxic shock syndrome and myocarditis with cardiogenic shock. Clinical reports have recently been published from the United States [2], Italy [3], the United Kingdom [4], France and Switzerland [5], and the Center for Disease Control (CDC) has issued an emergency alert [6].
Clinical presentation is variable, with most centers reporting significant gastrointestinal (GI) symptoms, cardiac disease, mild or absent respiratory symptoms, and variable incidence of rash, red eyes, and oral mucous membrane changes. As this is an emerging condition, a number of names have been used: “Kawashocky”, “Coronasacki”, hyperinflammatory shock in children with COVID-19, Pediatric COVID-19 Associated Inflammatory Disorder (PCAID), Pediatric Multisystem Inflammatory Syndrome (PMIS) and Multisystem Inflammatory Syndrome in Children (MIS-C). It is still unclear if this is a post-infectious complication or a primary complication of infection with SARS-CoV-2, however, initial epidemiologic descriptions are highly suggestive of a correlation. We will refer to this syndrome herein as MIS-C, the moniker adopted by the CDC.
2. Case definition
This syndrome is not well defined and the recommendations put forth will likely be amended as we learn more. MIS-C can present at any time, although based on recent (primarily anecdotal) reports, often occurs 1–6 weeks following infection, and may overlap with an acute respiratory COVID-19 presentation [2,3]. It can appear similar to KD with coronary artery aneurysms and extracardiac manifestations. Many described cases of KD-like MIS-C fall outside the typical age group (older) and ethnic background (predominantly non-Asian) than classic KD. It remains unclear if this syndrome is unique to children or if it occurs in adults with COVID-19. Besides potentially presenting with some or most of the symptoms associated with KD (hand and foot inflammation/swelling, mucous membrane changes/strawberry tongue, non-exudative conjunctivitis, rash, and unilateral significant lymphadenopathy) [7], MIS-C can present with evidence of multiorgan failure including neurologic involvement, hyperferritinemia, and cardiogenic or vasoplegic shock. Most reports describe significant GI manifestations on presentation, such as vomiting, diarrhea, and severe abdominal pain. The multi-faceted nature of the disease course and various presentations underlines the need for multispecialty input (emergency medicine, critical care, cardiology, infectious diseases, hematology, nephrology, and rheumatology). Our knowledge of this newly described entity is evolving by the day, as are the proposed diagnostics, pharmacological and non-pharmacological management, and recommendations.
3. Proposed guidelines for evaluation
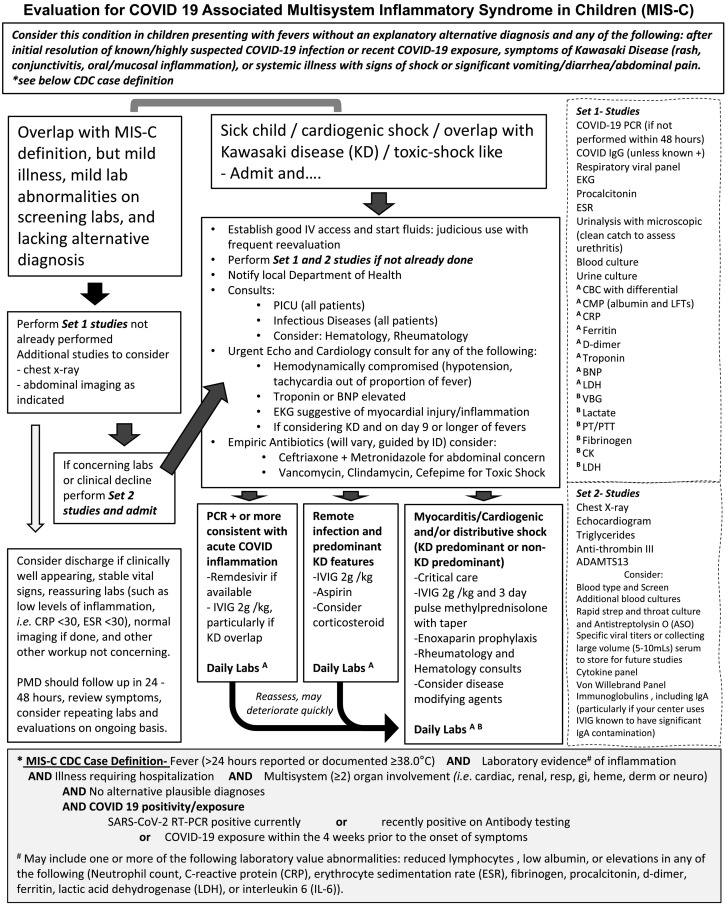
The following proposed guidelines were created by a multidisciplinary team at our center consisting of pediatric emergency medicine physicians, hospitalists, intensivists, and specialists in the areas of infectious diseases, cardiology, rheumatology, and hematology (see Fig. 1 ). The guidelines are based, in part, on reported cases (unpublished and published), recommendations from the CDC, New York State Department of Health, and the Royal College of Pediatrics and Child Health.
Fig. 1.
Proposed guidelines for evaluation of a child with suspected MIS-C.
Guideline was created following the CDC case definition with input from emergency medicine physicians, hospitalists, intensivists, and specialists in the areas of infectious diseases, cardiology, rheumatology, and hematology.
3.1. Initial consideration in the emergency department
Health care providers in the emergency department face a challenge as fever in children is a common presentation and currently many children have potentially been recently exposed to COVID-19. Patients in whom there is a low index of suspicion presenting with some but not all of the features of MIS-C should be considered for inflammation screening, at minimum, a complete blood count (CBC) and C-reactive protein (CRP) with strong consideration for SARS-CoV-2 PCR and antibody testing. Patients with signs and symptoms fulfilling the case definition of MIS-C (see Fig. 1) should undergo a more extensive workup. Discussion with local pediatric emergency medicine physicians that serve your area is encouraged for further guidance on the workup of suspected cases.
It has been reported that patients can initially be well appearing with reassuring laboratory workup, only to return to the hospital days later with worsening symptoms and rapid clinical deterioration. We propose that the patients evaluated for this condition who are discharged from the emergency department are given MIS-C specific discharge instructions and have a follow-up clinic or telehealth visit within 24–72 h. Discussion with local pediatric infectious disease physicians that serve your area for questions that may arise during follow-up is recommended.
3.2. Criteria for hospitalization
Proposing detailed criteria for hospital admission is challenging and it will depend on multiple factors. Children initially being evaluated in a rural area or a local emergency department/urgent care center/hospital, should be stabilized and transferred as quickly and safely as possible to a tertiary medical center. Taking into account the European and New York City experiences where many children required intensive care unit (ICU) care, we suggest a pediatric ICU consultation in children meeting MIS-C criteria, and to have a low threshold to transfer to a center with a pediatric ICU if pediatric ICU care is not available.
3.3. Treatments
There has been a broad range of pharmacologic therapy used and proposed for patients with MIS-C. It must be taken into account that every child will have a different presentation and clinical course, and therapy must be tailored to each case individually with input from consulting specialists. We propose some general guidelines for treatment based on published data, anecdotal data, and personal experience (see Fig. 1).
Antibiotic coverage should be empiric in patients diagnosed and hospitalized with MIS-C, with initial broad-spectrum antibiotics recommended as symptoms overlap with severe bacterial infections. If they have milder illness, we suggest ceftriaxone. If GI symptoms are predominant add metronidazole, and in cases of severe illness or shock we advise vancomycin, clindamycin, and cefepime or vancomycin, meropenem, and gentamicin. We strongly encourage consultation with local pediatric infectious disease experts prior to transfer of care or quickly after initial evaluation (see Fig. 1). If there is access to remdesivir (an antiviral agent with activity against SARS-CoV-2 that is currently available for compassionate use in young children and limited clinical trials), this should be considered, particularly for those known to be PCR positive and/or with a presentation consistent with typical COVID-19. The current proposed dose for children is 5 mg/kg load IV once (max dose 200 mg) on day 1, then 2.5 mg/kg (100 mg max dose) IV daily for nine days.
Children presenting predominantly with shock benefit from cardiac and respiratory support (see Cardiology and Critical Care discussion sections). A number of adjunct therapies have been used because of the profound inflammatory response and KD-like features, with intravenous immunoglobulin (IVIG), corticosteroids, anakinra (an interleukin-1 receptor antagonist), and tocilizumab (an anti-interleukin-6 receptor monoclonal antibody) being most often reported. Many centers have treated children that present most similar to KD with traditional therapy used for KD. We recommend giving IVIG 2 g/kg and aspirin 20–25 mg/kg/dose every 6 h (80–100 mg/kg/day) for all patients with KD-like illness, evidence of excessive inflammation (ferritin >700 ng/mL, CRP >30 g/dL, or multisystem organ failure), or cardiac involvement. Aspirin dosage may also vary at individual centers. Patients with KD-like illness in high-risk categories (infants, KD shock syndrome, CRP >130 g/dL, admission echo Z score >2.5 or aneurysms, Asian race) should receive IVIG 2 g/kg as single infusion with a three-day pulse methylprednisolone. If the presentation is most consistent with KD and there is failure of first line treatment a second dose of IVIG or infliximab (a Tumor necrosis factor (TNF)-alpha inhibitor) could be considered. For critically ill children, decisions regarding thrombosis prophylaxis should be guided by hematology.
Some patients have presented with severe inflammation with or without KD features consistent with cytokine storm syndrome (CSS) (see Rheumatology section for a more detailed description). For these patients we would consider use of anakinra and corticosteroids, in particular if they are not responding to supportive care or first line treatments [8]. Anakinra has a short half-life, and quick onset, therefore if the patient does not respond quickly, other medications can be considered.
3.4. Hospital course
This will vary depending on initial presentation; we recommend daily laboratory evaluation be done on all hospitalized children depending on the disease classification (see Fig. 1). We advise stopping antibiotics if cultures are negative after 48 h. Children presenting with KD symptoms should be reassessed 24–36 h after the end of IVIG infusion for evidence of fevers or ongoing inflammation. If clinical inflammation continues or worsens, retreatment or new therapy should be considered (guided by infectious diseases and rheumatology consultation). Typically, our center decreases aspirin dose to 3–5 mg/kg as a single daily dose when afebrile for 24 h or more, which will continue after discharge.
3.5. Discharge criteria and follow-up
We recommend the following guide for deciding on discharge: three to four days of down trending inflammatory markers (ferritin, CRP, D-Dimer), troponin consistently declining and < 1.0 ng/mL, 48 h without supplemental oxygen, 48 h without fever, 48 h off vasopressors, normal EKG, therapeutic antifactor-Xa level if going home on enoxaparin, eating and drinking adequately, heart failure symptoms controlled with oral medications (if applicable), and stable or improved findings on repeat echocardiogram (particularly stable or improved: ventricular function, coronary artery abnormalities; and valve function).
Follow-up visits should be planned with the primary care physician within 24–72 h after discharge. Infectious disease follow-up should be at one week with a repeat of the following lab values (CBC with differential, CRP, brain-natriuretic peptide (BNP), D-dimer, ferritin and follow-up of other specific abnormalities). Cardiology follow-up should be at minimum two weeks from initial echocardiogram. With KD, another echocardiogram at six weeks is typical, but if the patient has myocarditis or a large aneurysm, this may need more frequent monitoring. If corticosteroids were used, a slow taper as an outpatient can be guided by clinical and laboratory parameters. Other follow-up visits will depend on the initial course.
4. Discussion
As initial reports of cases of MIS-C are all under 21 years of age, this emerging condition presents a challenge for pediatricians. For children that fall into the case definition, a multi-disciplinary team approach is necessary to decide ongoing care as the disease manifestations can be significantly different. Advancing the level of care (transferring to tertiary care and intensive care) of children that fulfill the criteria for MIS-C is also crucial.
4.1. Cardiology
Prior to the COVID-19 pandemic, it was very uncommon for children presenting with KD to have shock or myocardial involvement [9]. Cardiac findings in KD typically manifest with coronary artery changes and rarely with depression of ventricular function. Initial published and non-published reports of COVID-19 associated MIS-C cases describe ventricular dysfunction, coronary artery changes, atrioventricular valve regurgitation and pericardial effusions [[2], [3], [4], [5]]. Therefore, it is prudent for cardiac screening to be completed early in hospital course; including measures of cardiac injury and ventricular dysfunction. In children presenting with shock (most have reported vasodilatory shock) fluid resuscitation is imperative in the initial management. As there is a high potential for underlying cardiac dysfunction, patients should be frequently reassessed during fluid resuscitation for evidence of fluid overload such as pulmonary edema or hepatomegaly. In centers with bedside ultrasound available, evaluation of cardiac function may be considered early in resuscitation to determine best management. Complete transthoracic echocardiogram should be performed urgently in all patients with clinical or laboratory evidence of cardiac injury and/or shock (see Fig. 1). In children with reassuring initial cardiac evaluation or mild to moderate disease, it is reasonable to consider ongoing cardiac screening throughout hospitalization due to reports of rapid decompensation. It is also reasonable to follow serum troponin and/or BNP and consider repeating echocardiogram with any significant laboratory or clinical changes.
4.2. Critical care
Critical care management of these patients is warranted in most recent reports [4,5]. Early recognition of shock state (vasoplegic vs cardiogenic), proper and judicious fluid resuscitation, early establishment of invasive monitoring, intubation and mechanical ventilation, optimization of oxygen delivery (DO2), minimization of oxygen consumption (VO2), and appropriate initiation of inotropes and vasopressors are key factors to successful and favorable outcome [5,10,11]. This initial approach combined with multidisciplinary management and initiation of early but comprehensive diagnostics help to guide further therapeutic choices (e.g. antithrombotics, antibiotics, and immunomodulators). Extracorporeal therapies like plasmapheresis (therapeutic plasma exchange) [12] and extracorporeal membrane oxygenation (ECMO) [5] may have a role in treating and supporting these patients especially in cases of severe cytokine storm, refractory vasoplegia and cardiogenic or septic shock. The recent report from Switzerland and France supports such an approach [5]. They described the experience of thirty-five critically ill children with MIS-C presenting with acute myocardial injury/myocarditis and cardiogenic shock. Initial symptoms on presentation were mainly fever, fatigue and GI manifestations. Inotropic support was required in 80%, while veno-arterial (VA) ECMO was initiated in 28% in this cohort. Despite the rapid deterioration at presentation, a rapid resolution of the systolic myocardial function was noted. All patients survived and none had embolic or thrombotic events. All patients received IVIG and 65% received heparin for anticoagulation.
4.3. Hematology
COVID-19 infection causes widespread endothelial injury and activation of coagulation resulting in high fibrinogen, D-dimer, and Factor VIII, and low antithrombin III. It has been associated with high rates of venous thromboembolic events (VTE) including deep vein thromboses, pulmonary emboli, digital ischemia, arterial thrombosis, microvascular thrombosis and strokes [13]. Prophylactic anticoagulation for adults hospitalized with COVID has been widely accepted, with many centers escalating to intermediate-dose or therapeutic anticoagulation for adults with signs of coagulopathy and/or organ failure, given the high rates of breakthrough VTE for adults on prophylactic anticoagulation [14]. Strategies regarding prophylactic anticoagulation in COVID-19 pediatric patients vary institutionally, but many have elected for a minimum prophylactic anticoagulation strategy in adolescents and the critically ill. Whether or not MIS-C patients have the same risk of VTE as during acute COVID-19 is unclear; however, these patients also have evidence of activation of coagulation (high D-dimer, high fibrinogen), inflammation, multi-organ dysfunction and require critical care intervention including the placement of central lines. Prophylactic anticoagulation with enoxaparin is reasonable to consider in critically ill patients, and hospitalized patients with significant derangements of coagulation. Patients with expanding or large coronary artery aneurysms will require therapeutic anticoagulation and antiplatelet therapy. In low-risk patients with KD or KD-like disease, aspirin monotherapy in accordance with established guidelines can be considered [7]. The effect of these interventions in ameliorating disease severity needs further study.
4.4. Infectious diseases
Sepsis and/or toxic-shock should be considered and addressed in all cases presenting with cardiovascular compromise. Other causes of systemic inflammation (e.g. adenovirus, Epstein-Barr virus) should be entertained as well, particularly as community social gathering limitations are changing. A number of these children will fall into KD classification. The children that fulfilled classic criteria of KD within early reports of MIS-C generally had less myocardial involvement (near normal ventricular function, lower troponins, lower BNPs) and seemed to respond well to care directed at KD [3]. KD shock presentation has been reported in up to 7% of cases of KD previously and is known to have elevations in BNP and troponins [9] with a clinical picture consistent with myocarditis. In the MIS-C cases reported, there have been a number with both inflamed coronaries and shock that would fit into the diagnosis of KD Shock Syndrome, however, not all of these reported patients have been shown to have preceding SARS-CoV-2. It is unclear at this time if these more typical KD cases occurring in this time period are unrelated or a post-infectious complication of SARS-CoV-2.
4.5. Rheumatology
In some critically ill children, a cytokine storm syndrome (CSS) appears to develop in response to the virus. This syndrome is characterized by an overproduction of pro-inflammatory cytokines including TNF, IL-6, and IL-1β resulting in clinical symptoms of high fevers, rashes, coagulopathy, and neurologic changes, with some progressing to multiple organ failure and death [15]. Lab abnormalities frequently associated with CSS include thrombocytopenia, lymphopenia, and elevations of the following: transaminase levels, D-dimers, lactate dehydrogenase (LDH), coagulation times, CRP, and ferritin (ferritin is often profoundly elevated). This syndrome is very similar to macrophage activation syndrome (MAS) or secondary hemophagocytic lymphohistiocytosis (HLH) which is commonly encountered and treated by rheumatologists. Treatments that have proven effective for treatment of MAS include corticosteroids, anakinra and tocilizumab among others [16]. Early reports, mainly from China, described adult patients that fit the description of COVID-19 associated CSS, and had successful outcomes after treatment with tocilizumab [17]. For this reason, many across the US have proposed this medication be used if evidence of CSS exists. Many rheumatologists, including our group, would propose using anakinra (IV is suggested specifically as subcutaneous dosing was not found to be as effective in one study) if children have evidence of CSS or are severely ill with multiorgan failure [18]. Anakinra has a quick onset, short half-life (4 h), large therapeutic window, and a good safety profile. We find this a favorable treatment option; if there is not a quick and adequate response an alternate medication can be considered.
5. Conclusion
The limited reports available indicate that children with COVID-19 associated MIS-C can deteriorate quickly, so increased index of suspicion and discussion regarding higher level of care (transferring to pediatric tertiary care centers or to intensive care) are warranted early. As outlined herein, a broad initial approach with a multidisciplinary team for those meeting the case definition is crucial for successful outcomes.
Funding
This work did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
Teresa R. Hennon, Michelle D. Penque, Mark D. Hicar: Conceptualization, Visualization, Writing - Original draft preparation, Reviewing and Editing. Rabheh Abdul-Aziz, Omar S. Alibrahim, Oscar G. Gomez-Duarte, Megan B. McGreevy, Andrew J. Prout, Beverly A. Schaefer: Writing - Original draft preparation, Reviewing and Editing. Steven J. Ambrusko, John V. Pastore, Stephen J. Turkovich: Writing - Reviewing and Editing.
Declaration of competing interest
Authors declare no conflict of interest.
References
- 1.Qiu H., Wu J., Hong L. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020 Mar 25 doi: 10.1016/S1473-3099(20)30198-5. S1473-3099(20)30198-5, ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeBiasi R.L., Song X., Delaney M. Severe COVID-19 in children and young adults in the Washington, DC Metropolitan Region. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.05.007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verdoni L., Mazza A., Gervasoni A. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31103-X. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riphagen S., Gomez X., Gonzalez-Martinez C., Wilkinson N., Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet. 2020 May 7 doi: 10.1016/S0140-6736(20)31094-1. S0140-6736(20)31094-1, ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belhadjer Z., Meot M., Bajolle F. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020 May 17 doi: 10.1161/CIRCULATIONAHA.120.048360. ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.CDC Multisystem Inflammatory Syndrome in Children (MIS-C) associated with coronavirus disease 2019 (COVID-19) https://emergency.cdc.gov/han/2020/han00432.asp
- 7.McCrindle B.W., Rowley A.H., Newburger J.W. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association. Circulation. 2017;135(17):e927–e999. doi: 10.1161/CIR.0000000000000484. [DOI] [PubMed] [Google Scholar]
- 8.Rajasekaran S., Kruse K., Kovey K. Therapeutic role of anakinra, an interleukin-1 receptor antagonist, in the management of secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction/macrophage activating syndrome in critically ill children*. Pediatr Crit Care Med. 2014;15(5):401–408. doi: 10.1097/PCC.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 9.Ma L., Zhang Y.Y., Yu H.G. Clinical manifestations of Kawasaki disease shock syndrome. Clin Pediatr (Phila) 2018;57(4):428–435. doi: 10.1177/0009922817729483. [DOI] [PubMed] [Google Scholar]
- 10.Weiss S.L., Peters M.J., Alhazzani W. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020;46(Suppl. 1):10–67. doi: 10.1007/s00134-019-05878-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alhazzani W., Moller M.H., Arabi Y.M. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intensive Care Med. 2020;46(5):854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fortenberry J.D., Nguyen T., Grunwell J.R. Therapeutic plasma exchange in children with thrombocytopenia-associated multiple organ failure: the thrombocytopenia-associated multiple organ failure network prospective experience. Crit Care Med. 2019;47(3):e173–e181. doi: 10.1097/CCM.0000000000003559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klok F.A., Kruip M., van der Meer N.J.M. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020 Apr 30 doi: 10.1016/j.thromres.2020.04.041. S0049-3848(20)30157-2, ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Middeldorp S., Coppens M., van Haaps T.F. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost. 2020 May 5 doi: 10.1111/jth.14888. ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tisoncik J.R., Korth M.J., Simmons C.P. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76(1):16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cron R.Q., Chatham W.W. The rheumatologist’s role in COVID-19. J Rheumatol. 2020;47(5):639–642. doi: 10.3899/jrheum.200334. [DOI] [PubMed] [Google Scholar]
- 17.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect. 2020;80(6):607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cavalli G., D.L.G., Campochiaro C. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. The Lancet Rheumatology. 2020 doi: 10.1016/S2665-9913(20)30127-2. (p. Online, May 7, 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]