Introduction
The COVID-19 virus is a devastating pandemic that has impacted the US healthcare system significantly. More than one study reported a significant decrease in acute coronary syndrome admissions during that pandemic which is still due to unknown reasons.
Methods
This is a retrospective non-controlled multi-centered study of 180 patients (117 males and 63 females) with acute coronary syndrome (STEMI and NSTEMI) admitted during March/April of 2019 and March/April 2020 in Upstate New York.
Results
A total of 113 patients (61.9% males, 38.1% females) with a mean age of 72.3 ± 14.2 presented during March/April 2019 with ACS (STEMI + NSTEMI) while only 67 (70.1% males, 29.9% females) COVID-19 negative patients with a mean age of 65.1 ± 14.5 presented during the same period (March/April) in 2020. This is a drop by 40.7% (P < .05) of total ACS cases during the COVID-19 pandemic. In NSTEMI patients, 36.4% presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (27.1%, P = .033).
Conclusion
The COVID-19 pandemic led to a substantial drop by 40.7% (P < .05) of total ACS admissions in our area. This decrease in hospital admissions and late presentations can be a worrisome sign for an increase in future complications of myocardial infarctions.
The severe acute respiratory syndrome Coronavirus 2 more commonly referred to as COVID-19 has been a devastating viral pandemic across the globe. The high transmission rate has led to widespread stay-at-home orders across the United States.
Although COVID-19 has led to surges in hospitalizations, the amount of acute coronary syndrome admissions has substantially decreased.1., 2., 3., 4., 5., 6., 7. This phenomenon has been seen in multiple countries and thought to be due to multiple factors including hesitance of patients to visit the hospitals despite initial symptoms, better medication adherence, lower pollution levels, less smoking, and less physical strain.6 , 7
The spread of the virus has led to stay-at-home orders from almost all states across the country. In New York State these orders were given on March 22, 2020. The first positive case of COVID-19 in Broome County, located in the southern tier of New York State, was on March 17, 2020.8
Our retrospective study investigates the impact that COVID-19 has had on the amount of ST elevation myocardial infarctions and non-ST elevation myocardial infarctions within our area during March and April of 2020.
Methods
This is a retrospective non-controlled multi-centered study of 180 patients (117 males and 63 females) with acute coronary syndrome admitted in March/April of 2019 and March/April of 2020 in Upstate New York. The patient population included patients aged 18 years to 110 years (mean age of 72.3±14.2 in 2019, and 65.1±14.5 in 2020) with Non-ST elevation Myocardial infarction and ST-elevation myocardial infarction admitted at United Health Services – Wilson Memorial Hospital which is a high-volume primary PCI referral center (~800 PCI procedures/year and ~2000 cardiac catheterizations/year), Delaware Valley Hospital, Binghamton General Hospital, and Chenango Memorial Hospital, all located in Broome County, Upstate New York.
The diagnostic criteria for STEMI in this study were new ST elevation at the J point in at least 2 contiguous leads with ≥2 mm (0.2 mV) in men or ≥1.5 mm (0.15 mV) in women in leads V2-V3 and/or of ≥1 mm (0.1 mV) in other contiguous chest leads. The presence of a new LBBB with anginal symptoms was also considered diagnostic of STEMI. NSTEMI was defined as elevated troponin levels with anginal symptoms. Ischemic ECG changes may be present but are not required for the diagnosis.
Data collection
Data were retrieved by reviewing the electronic databases for all patients with positive troponins. Patients with troponin elevation due to non-cardiac causes, or type 2–5 MI were excluded. We retrospectively reviewed all STEMI and NSTEMI patients from March 2019 to April 2019 and March 2020 to April 2020. Relevant patient data including age, gender, home address, traveled miles to the hospital, onset of clinical symptoms, and management strategy were collected. This information was collected regardless of whether the patient underwent PCI or medical management.
Data for the overall hospital census (including surgical, internal medicine, OBGYN, pediatrics, intensive care unit, and cardiac care unit) during March/April 2019 and March/April 202 at the 4 hospitals was obtained.
Statistical analysis
Abstracted medical records were entered into a computer and analyzed using SPSS V24. Categorical data were summarized using percentage and frequency, while numerical data were summarized using means and standard deviations. Differences in means were tested using the independent t test with 95% confidence intervals. Differences in proportions were tested using Pearson's chi-square (independent groups). Statistical significance was assessed at the 0.05 level.
Results
ACS (STEMI and NSTEMI) data
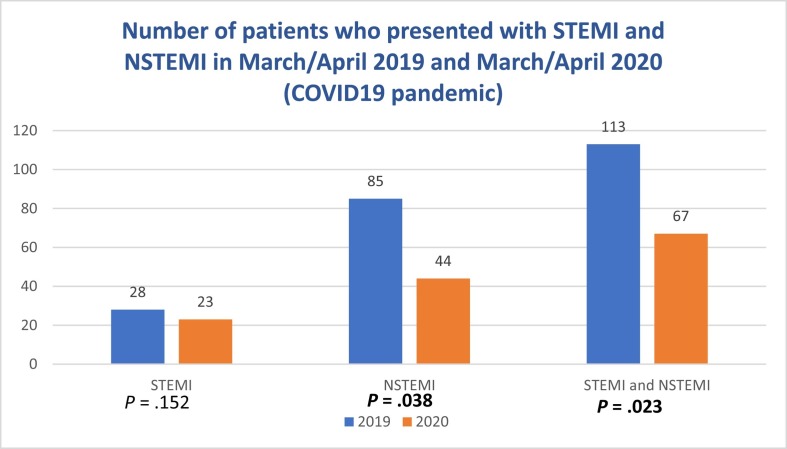
A total of 113 patients (61.9% males, 38.1% females) with a mean age of 72.3 ± 14.2 presented during March/April 2019 with ACS (STEMI + NSTEMI) while only 67 (70.1% males, 29.9% females) COVID-19 negative patients with a mean age of 65.1 ± 14.5 presented during the same period (March/April) in 2020 (Table I ). This is a drop by 40.7% (P < .05) of total ACS cases during the COVID-19 pandemic. ( Figure 1 ).
Table I.
Demographics of patients who presented with ACS (STEMI and NSTEMI) in March/April 2019 and March/April 2020
| STEMI and NSTEMI | |||||
|---|---|---|---|---|---|
| 2019 |
2020 |
||||
| N = 113 | N = 67 | P | [95% CI] | ||
| Age | Mean ± SD | 72.3 ± 14.2 | 65.1 ± 14.5 | .001* | [2.8,11.6] |
| Gender, N (%) | Male | 70 (61.9) | 47 (70.1) | .265** | |
| Female | 43 (38.1) | 20 (29.9) | |||
| Miles away From the hospital |
Mean ± SD | 19.2 ± 19.5 | 15.3 ± 15.5 | .171* | [−1.6,9.3] |
| Treatment, N (%) | PCI | 73 (64.6) | 57 (85.1) | .003** | |
| Medical Management | 40 (35.4) | 10 (14.9) | |||
| Onset of symptoms, N (%) | < 3 h | 21 (18.6) | 5 (7.5) | .072** | |
| < 6 h | 25 (22.1) | 9 (13.3) | |||
| 6–24 h | 41 (36.3) | 32 (47.8) | |||
| >24 h | 26 (23) | 21 (31.3) | |||
*Independent t test; **χ2 test.
Figure 1.
Total number of patients who presented with STEMI, NSTEMI, and ACS (STEMI + NSTEMI) in March/April 2019 and March/April 2020. It showed a drop by 40.7% (P < .05) of total ACS cases during the COVID-19 pandemic.
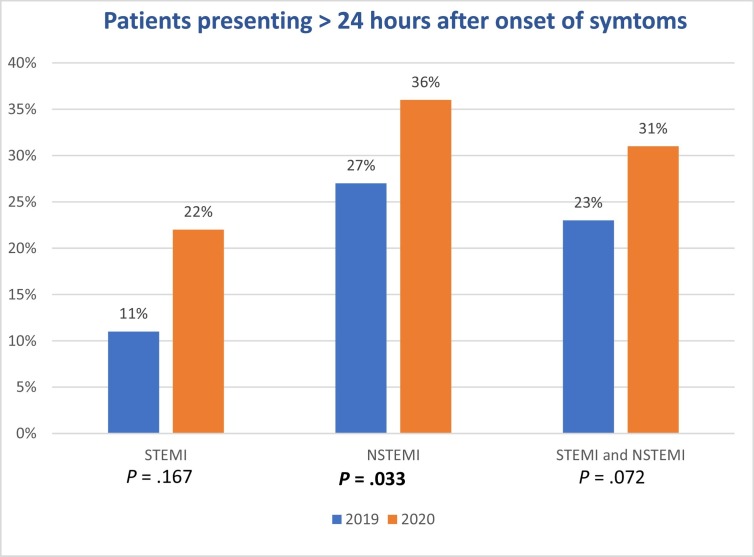
In 2019, 64.6% were treated by PCI and 35.4% were treated medically, while in 2020, 85% had PCI and only 14.9% were treated medically. Interestingly, 31% of the patients presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (23%, P = .072). (Table I, Figure 2 ).
Figure 2.
Data showing significantly more patients with NSTEMI (36%) presented >24-hour after onset of symptoms during the COVID-19 pandemic in comparison with March/April 2019 (27%) (P = .033).
STEMI data
A total of 28 (64.3% males, 35.7% females) with a mean age of 67.4 ± 16 patients presented during March/April 2019 with STEMI while only 23 (60.9% males, 39.1% females) patients with a mean age of 58.6 ± 13 presented during the same period (March/April) in 2020. This is a drop by 17.8% (P = .152) of total STEMI cases during the COVID-19 pandemic. ( Figure 1 ).
In 2019, 85.7% had PCI and 14.3% were treated medically, while in 2020, 100% had PCI, and none were treated medically. 21.7% of the patients presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (10.7%, P = .167). (Table I, Table II , Figure 2 ).
Table II.
Onset of symptoms prior to admission showing a significant difference between 2019 and 2020 in NSTEMI patients with P value of 0.033
| STEMI |
NSTEMI |
||||||
|---|---|---|---|---|---|---|---|
| 2019 | 2020 | P | 2019 | 2020 | P | ||
| Onset of symptoms, N (%) | < 3 Hours | 11 (39.3) | 4 (17.4) | .167 | 10 (11.8) | 1 (2.3) | .033 |
| < 6 Hours | 10 (35.7) | 7 (30.4) | 15 (17.6) | 2 (4.5) | |||
| 6–24 Hours | 4 (14.3) | 7 (30.4) | 37 (43.5) | 25 (56.8) | |||
| >24 Hours | 3 (10.7) | 5 (21.7) | 23 (27.1) | 16 (36.4) | |||
NSTEMI data
A total of 85 patients (61% males, 38.8% females) with a mean age of 73.9 ± 13 presented during March/April 2019 with NSTEMI while only 44 (75% males, 25% females) patients with a mean age of 68.5 ± 14 presented during the same period (March/April) in 2020. This is a drop by 48.2% (P < .05) of total NSTEMI cases during the COVID-19 pandemic. ( Figure 1 ).
In 2019, 57.6% had PCI and 42.4% were treated medically, while in 2020, 77.3% had PCI and only 22.7% were treated medically. Interestingly, 36.4% of the patients presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (27.1%, P = .033). (Table I, Table II, Figure 2 ).
Overall hospital census and inpatient COVID-19 data
A total of 350 COVID-19 cases were diagnosed in Broome County of upstate New York during March/April 2020. The inpatient COVID-19 census was ranging between 10–15 patients throughout the study period.
During March/April 2019, there was a total of 3496 admissions (including surgical, internal medicine, OBGYN, pediatrics, intensive care unit, and cardiac care unit), while in March/April 2020 a total of 2612 admissions were reported. This is a drop by 25.2%. ( Table III ).
Table III.
Overall hospital census and inpatient COVID-19 data including all 4 hospitals
| Data including all 4 hospitals | ||
|---|---|---|
| Total admissions | Inpatient COVID-19 | |
| March/April 2019 | 3496 | None |
| March/April 2020 | 2612 | 10 to 15 |
| Difference (2019/2020) | 25.20% | - |
Discussion
Although Upstate New York was not significantly affected by the number of COVID-19 patient admissions (~350 cases in Broome County as of May 1, 2020) in comparison with New York City (~320,000 cases as of May 1, 2020) and other highly affected cities,9 the reported decrease in number of ACS admissions was similar.1., 2., 3., 4., 5., 6., 7. Our data report a drop by 40.7% (from 113 to 67 patients) (P < .05) of total ACS cases during the COVID-19 pandemic. (Figure 1 ) This is significantly higher than the number of total hospital admissions at all four hospitals which revealed a drop by 25.2% (Table III).
In our study 21.7% of the patients with STEMI presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (10.7%, P = .167) which was not statistically significant while 36.4% of the patients with NSTEMI presented late (>24 hours of symptoms) during the COVID-19 pandemic in comparison with 2019 (27.1%, P = .033) which was statistically significant. (Table II). This is a very interesting finding that suggests many patients with mild or anginal equivalent symptoms are likely staying at home and waiting longer before presenting to the hospital possibly due to the hesitance to be exposed to COVID-19 patients in hospitals.
Moreover, a total of 28 patients presented during March/April 2019 with STEMI while only 23 patients presented during the same period (March/April) in 2020 which is a nonsignificant drop by 17.8% (P = .152) of total STEMI cases during the COVID-19 pandemic. However, 85 patients presented during March/April 2019 with NSTEMI and only 44 patients presented during the same period (March/April) in 2020. This is a significant drop by 48.2% (P < .05) of total NSTEMI cases during the COVID-19 pandemic. That is probably explained by the severity of the condition in STEMI patients, where they present with a more dramatic clinical picture that cannot be ignored or delayed.
In 2019 35.4% of ACS admissions (STEMI and NSTEMI) were treated medically, while in 2020, only 14.9% were treated as such. This can be explained by the high proportion of elderly population with multiple comorbidities within our area. The mean age of patients that were treated medically was 89 ± 10.2. After discussion with the patients and their families, the decision was to treat them medically.
Our results go in conjunction with multiple similar studies performed throughout the world as presented in Table III. Garcia et al in USA that analyzed STEMI activations in 9 high volume cardiac centers from Jan 1, 2020 until March 31, 2020 which revealed a decrease by 38% of STEMI activations during the COVID-19 pandemic1 (Table IV ).
Table IV.
Studies reporting the impact of the COVID-19 pandemic on ACS admissions and STEMI activations
| Authors | Country | No. of centers | Results | Study period |
|---|---|---|---|---|
| Garcia et al | USA | 9 | 38% decrease of STEMI activations | Jan 1, 2020 to March 31, 2020 |
| De Filippo Ovidio et al | Italy | 15 | Admission rate for ACS decreased from | Feb 20, 2020 to March 31, 2020 |
| 18 admissions /day to 13.3 admissions/day | ||||
| Metzler et al | Austria | 19 | 39.4% decrease in ACS admissions | March 2, 2020 to March 29, 2020 |
| Rodriguez-Leor et al | Spain | 81 | 40% decrease in PCI for STEMI | Feb 24, 2020 to March 24, 2020 and March 16, 2020 to March 22, 2020 |
De Filippo Ovidio et al performed a retrospective analysis of ACS patients that were admitted at 15 hospitals in northern Italy. The mean admission rate for ACS was 13.3 admissions per day during the COVID-19 pandemic which is significantly lower (by 26%) than the rate during an earlier period in the same year (18 admissions per day). (Table IV ). 2
Also, Metzler et al conducted a nationwide retrospective survey from March 2, 2020 to March 29, 2020 in 19 PCI centers in Austria to study the impact of COVID-19 on the diagnosis and treatment of ACS. There was a relative reduction of 39.4% in ACS admissions.3
Moreover, Rodriguez-Leor et al in Spain which included 81centers compared data for the week of Feb 24 through March 1 and for the week of March 16 through March 22. It reported a 40% decrease in PCI for STEMI Table IV . 5
Multiple hypothesis can be made as to why there was a significant drop in ACS admissions during the COVID-19 pandemic. Most likely due to the hesitance of patients to visit hospitals despite initial symptoms, but can also be due to misdiagnosis of ACS (since patients can present with cough and shortness of breath due to pulmonary edema) in the setting of multiple COVID-19 admissions, difficult transportation due to lockdowns in multiple countries and cities, better medication adherence, lower pollution levels, less smoking, and less physical strain.6 , 7
Overall, this decrease in ACS admissions is worrisome, and it may reflect a later increase in acute and subacute myocardial infarction complications that result in increased morbidity and mortality.
Study Limitations
Although this study was multi-centered, it was performed at a single county in Upstate New York with a total of 180 patients. Interestingly, our data showed similar results in comparison with other larger studies.1., 2., 3., 4., 5.
We only studied STEMI and NSTEMI patients, while excluding patients presented with only unstable angina.
Conclusion
The COVID-19 pandemic led to a substantial decrease in ACS admissions across the world. In our study we report a drop by 40.7% (P < .05) of total ACS admissions which is similar to other studies. This decrease in hospital admissions and late presentations might be a sign for an increase in future complications of myocardial infarctions.
Footnotes
Declarations of interest: None
Submission declaration: Our work described has not been published previously and is not under consideration for publication elsewhere. This paper is approved by all authors and by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents.
Funding
No extramural funding was used to support this work.
References
- 1.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 Pandemic. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Filippo Ovidio, D'Ascenzo Fabrizio Angelini, Filippo, et al. Reduced Rate of Hospital Admissions for ACS during Covid-19 Outbreak in Northern Italy: NEJM. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMc2009166 [DOI] [PMC free article] [PubMed]
- 3.Metzler B., Siostrzonek P., Binder R.K. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.-C.F., Cheung K.-S., Lam S. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4) doi: 10.1161/circoutcomes.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodríguez-Leor, O., Cid-Álvarez, B., Ojeda, S., Martín-Moreiras, J., Rumoroso, J. R., López-Palop, R., … Moreno, R. (2020). Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC: Interventional Cardiology (English Edition). 10.24875/recice.m20000123 [DOI]
- 6.Wood S. The Mystery of the Missing STEMIs During the COVID-19 Pandemic. 2020, April 8. https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19-pandemic Retrieved from.
- 7.Data shows reduction in U.S. heart attack activations during COVID-19 pandemic. 2020, April 10x. https://www.cathlabdigest.com/content/data-shows-reduction-us-heart-attack-activations-during-covid-19-pandemic Retrieved from.
- 8.Altieri G. Broome Reports First Positive Test; Bans Unnecessary Travel: 2020, March. 17.https://wskg.org/news/broome-reports-first-positive-test-bans-unnecessary-travel/ Retrieved from. [Google Scholar]
- 9.Coronavirus. (n.d.). Retrieved from http://www.gobroomecounty.com/hd/coronavirus