Introduction
In patients with Wolff-Parkinson-White (WPW) syndrome, presence of an accessory pathway (AP) results in a short PR interval, a wide QRS from ventricular preexcitation, and symptoms most commonly due to atrioventricular reentrant tachycardia (AVRT). We describe an unusual case of WPW syndrome in a patient with inappropriate therapies from his biventricular implantable cardioverter-defibrillator (BiV ICD) implanted for primary prevention in the setting of severe nonischemic cardiomyopathy (NICM) and “left bundle branch block” (LBBB).
Case report
A 45-year-old man with NICM, “LBBB” (electrocardiogram shown in Figure 1a), and congestive heart failure with left ventricular ejection fraction of 20% despite chronic therapy with lisinopril and metoprolol tartrate, for which he received a BiV ICD 4 years before, presented for evaluation for recurrent ICD shocks. ICD electrograms showed tachycardia with a 1:1 AV relationship at a cycle length of 320 ms, driven by the A-A intervals that were unaffected by antitachycardia pacing therapies, suggesting the ventricular antitachycardia pacing and shocks were delivered for a supraventricular rhythm. At electrophysiology (EP) study, when BiV pacing was inhibited at the start of the procedure, the underlying rhythm was revealed to be sinus rhythm with LBBB pattern but with a very short PR interval of 100 ms (Figure 1b). A right inferolateral AP was present, but no sustained reentrant arrhythmia was inducible despite extensive programmed stimulation at baseline and with isoproterenol. The AP was successfully mapped and ablated at the inferolateral tricuspid annulus (Figure 2a and b), and resulted in normalization of the QRS (Figure 3). He was continued on the same medications after ablation. The pacing mode on his BiV ICD was changed to AAI 40 beats per minute. During his EP study, his left ventricular (LV) lead was noted to be in a good posterolateral location (Figure 2). With BiV pacing, his ejection fraction improved but had stabilized at 40% for a year prior to ablation. Echocardiogram 2 months after ablation showed his ejection fraction had normalized (65%).
Figure 1.
a: Baseline electrocardiogram (ECG). b: Surface ECG leads I, II, and V1 and intracardiac electrograms from high right atrium, His, coronary sinus, and right ventricular apex at baseline, with vertical line marking the timing of the His bundle electrogram.
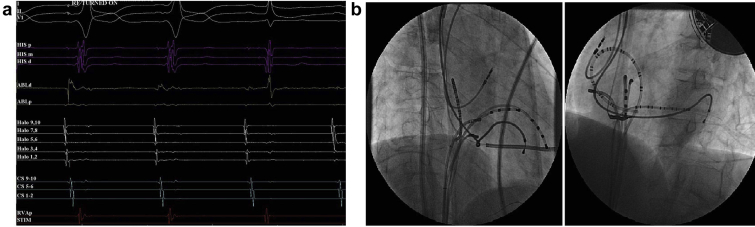
Figure 2.
a: Surface electrocardiogram leads I, II, and V1 and intracardiac electrograms from His, ablation catheter, and Halo catheter positioned around the tricuspid annulus and right ventricular apex showing loss of preexcitation with ablation. b: Fluoroscopic views in right anterior oblique 30 degree and left anterior oblique 55 degree projections demonstrating catheter positions during mapping at site of successful ablation.
Figure 3.
Surface electrocardiogram at electrophysiology study at baseline and after ablation.
Discussion
The cardiomyopathy in this patient was presumably due to LV dyssynchrony from marked ventricular preexcitation resulting from a right inferolateral AP. As usually noted with right-sided APs, the anatomical proximity to the sinus node resulted in significant ventricular preexcitation. LV systolic dysfunction may have resulted from a mechanism similar to that noted in patients who develop cardiomyopathy from right ventricular pacing. Incessant tachycardia is known to be a cause of cardiomyopathy in some patients with WPW syndrome,1 but this patient never had symptoms suggestive of AVRT, and none was inducible at EP study. In retrospect, the ICD shocks were delivered inappropriately for sinus tachycardia in this relatively young patient. The patient obviously had received the BiV ICD because of an erroneous diagnosis of LBBB; a careful examination of the electrocardiogram (Figure 1a) would have revealed the very short PR interval. His LV ejection fraction did appear to improve to 40% with BiV pacing (98% BiV paced, based on device interrogation) prior to ablation. Although no tachycardia was inducible at EP study and none was documented previously, AP ablation was beneficial: the “accessory pathway–mediated cardiomyopathy” resolved and LV function normalized with ventricular pacing turned off post ablation.
Conclusion
Right-sided APs with prominent preexcitation may result in a LBBB pattern, LV dyssynchrony, and NICM even in the absence of tachycardia. Several case reports and small case series have described non-tachycardia-mediated cardiomyopathy in pediatric patients from dyssynchrony owing to ventricular preexcitation, particularly from right-sided APs.2 Persistence of such AP conduction into adulthood may result in diagnosis of NICM. The PR interval should be heeded in younger patients with LBBB and cardiomyopathy before considering device therapy. If there is evidence of ventricular preexcitation, catheter ablation should be considered even in the absence of tachyarrhythmias, as successful ablation of the AP may “cure” not only the LBBB, but the cardiomyopathy also.3
Key Teaching Points.
-
•
PR interval should be noted in presence of left bundle branch block morphology and nonischemic cardiomyopathy in younger patients before considering device therapy.
-
•
Preexcitation from right-sided accessory pathways may result in left ventricular dyssynchrony and contractile dysfunction
-
•
Elimination of the accessory pathway may be beneficial in this situation, even if there is no atrioventricular reentrant tachycardia or atrial fibrillation.
References
- 1.Bensler J., Frank C., Razavi M. Tachycardia-mediated cardiomyopathy and the permanent form of junctional reciprocating tachycardia. Tex Heart Inst J. 2010;37:695–698. [PMC free article] [PubMed] [Google Scholar]
- 2.Tomaske M., Janousek J., Rázek V. Adverse effects of Wolff-Parkinson-White syndrome with right septal or posteroseptal accessory pathways on cardiac function. Europace. 2008;10:181–189. doi: 10.1093/europace/eun005. [DOI] [PubMed] [Google Scholar]
- 3.Uhm J.S., Nam J.H., Yu H.T. Accessory pathway-related left ventricular wall motion abnormality and the effects of radiofrequency catheter ablation in patients with Wolff-Parkinson-White syndrome. J Cardiovasc Electrophysiol. 2019;30:102–108. doi: 10.1111/jce.13753. [DOI] [PubMed] [Google Scholar]