Key Teaching Points.
-
•
The use of synthetic cannabinoids is on a rise in the United States, more so in the younger population.
-
•
Synthetic cannabinoids are not detected by routine toxicology screens.
-
•
Synthetic cannabinoids may have cardiovascular side effects including cardiac arrhythmias and even cardiac arrest.
-
•
Patients admitted with nonarrhythmic side effects of synthetic cannabinoid use should still be monitored for potential sudden cardiac arrest (SCA).
-
•
Drug-related SCA should not always be considered reversible until a thorough evaluation to determine if other sudden cardiac death (SCD) predispositions are present that may impact decisions regarding secondary prevention of SCD with implantable cardioverter-defibrillator therapy.
Introduction
Synthetic cannabinoids (SC), often referred to as K2 or spice, comprise a significant burden of overall illicit drug use in the United States. Contributing to its popularity may be the longer-lasting marijuana-like effects and lack of detection by standard toxicology screens, compared to natural cannabinoids. There is mounting evidence that SC may be responsible for potentially fatal cardiac arrhythmias. How to manage long-term risk of sudden cardiac death (SCD) in such patients has not been studied. Patients with drug use–related cardiac arrest are considered to have a reversible cause of the arrest and thus do not fit the class I indication for receiving an implantable cardioverter-defibrillator (ICD). However, the degree of reversibility is poorly defined when genetic predisposition for SCD may be unmasked rather than caused by SC use. Concern for continued drug use could also challenge the label of reversibility.
Case report
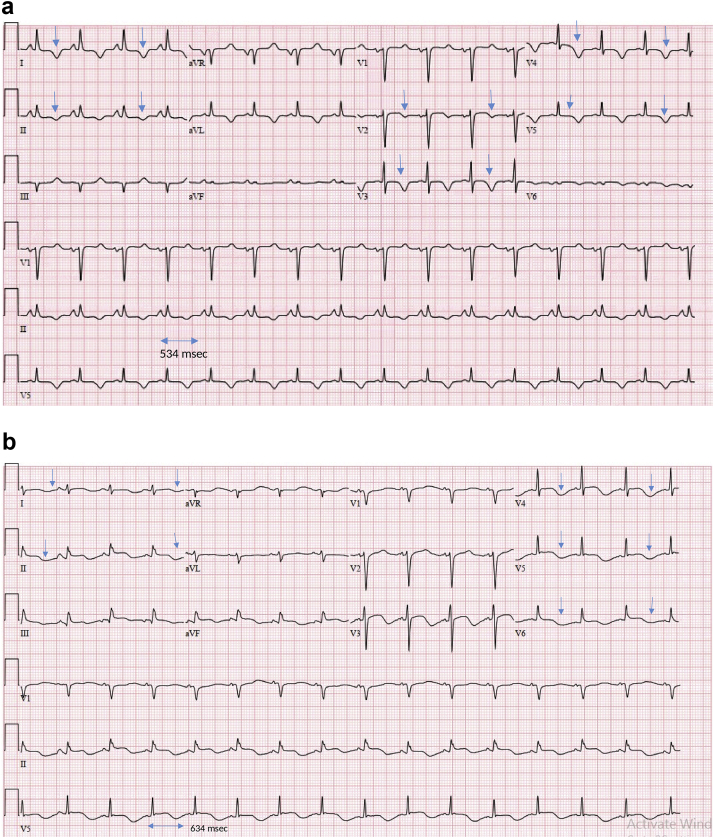
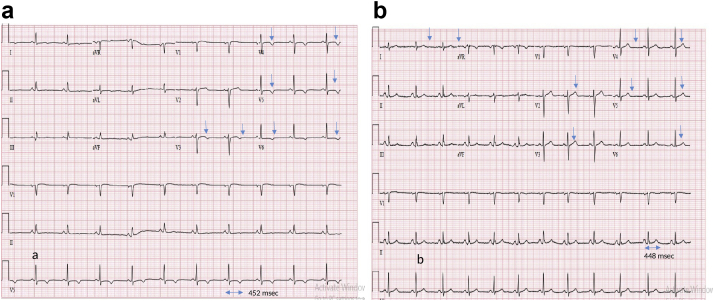
A 52-year-old woman with no significant past medical history was found unresponsive shortly after consuming K2-laced cigarettes. Cardiopulmonary resuscitation was started and Emergency Medical Service (EMS) was called. Return of spontaneous circulation was attained in the field by EMS after 15 minutes of cardiopulmonary resuscitation. Her initial rhythm was ventricular fibrillation (v-fib), for which she required 2 shocks and in addition 1 dose of epinephrine and lidocaine each. Therapeutic hypothermia was initiated in the Emergency Department. Initial electrocardiogram (ECG) 1 hour after the sudden cardiac arrest (SCA) was notable for normal sinus rhythm, prolonged QTc of 534 ms, and lateral lead T-wave inversion in V2–V6 (Figure 1a). Her history did not reveal any home medications, nor did she receive any QT interval–prolonging medications by EMS or the hospital. Initial serum electrolyte levels revealed potassium of 3.6 mmol/L, magnesium of 1.6 mg/dL, and calcium of 8.6 mg/dL. The patient had another SCA with torsades de pointes degenerating to v-fib after admission to the Cardiac Care Unit, with successful resuscitation. Immediately after return of spontaneous circulation was achieved, a temporary transvenous pacemaker was inserted owing to significant bradycardia requiring transcutaneous pacing, atropine boluses, and dopamine and epinephrine infusions. ECG 20 minutes after initial arrest revealed a prolonged QTc of 634 ms (Figure 1b). Serum electrolyte levels checked immediately after the second arrest showed a potassium level of 4.3 mmol/L, magnesium of 2.6 mg/dL, and calcium of 8.1 mg/dL. Cardiac troponin levels were unremarkable. Urine toxicology screen was negative. Blood alcohol level was undetectable. Echocardiogram showed a depressed left ventricle ejection fraction (LVEF) of 20% with global hypokinesis. Cardiac magnetic resonance imaging 3 days later showed improving LVEF of 42% with no evidence of infiltrative disease or evidence of an ischemic insult. A dual-chamber, transvenous ICD (TV-ICD) was implanted owing to recurrent SCA associated with QTc prolongation and reduced LVEF with atrial pacing support to allow for beta-blocker titration and atrial overdrive pacing, as durable future resolution of QTc prolongation and cardiomyopathy were still uncertain. Device settings included the following: 2 tachycardia zones with a ventricular tachycardia (VT) zone between 188 and 230 beats per minute (bpm) detected for 24 consecutive beats, treated with 3 decremental scanning bursts of antitachycardia pacing prior to cardioversion shocks; a v-fib zone > 231 bpm detected for 30 of 40 intervals with antitachycardia pacing during charging prior to defibrillation shocks; and bradycardia support at DDD 40–130 bpm. ECG done on day 4 of the presentation before discharge and at 2 years follow-up showed normalization of QTc interval (Figure 2a and b).
Figure 1.
a: Electrocardiogram after return of spontaneous circulation post first cardiac arrest showing prolonged QTc and lateral lead (V2–V6) T-wave inversions (blue arrows). b: Electrocardiogram done in Intensive Care Unit after return of spontaneous circulation post second cardiac arrest, again showing prolonged QTc and lateral lead (V3–V6) T-wave inversions (blue arrows).
Figure 2.
Electrocardiograms done a: on day 4 of admission and b: at 2 years follow-up after discharge, showing normalization of QTc interval with inverted T waves in leads V3–V6 at day 4 and upright T waves in lateral leads at 2 years (blue arrows).
The patient was seen at a follow-up visit 8 months after initial presentation and was found to have an improved LVEF of 55% on guideline-directed medical therapy including angiotensin-converting enzyme inhibitors and low-dose beta blockers. Her ECG showed a normal QTc interval at the visit. Eighteen months following ICD implant, she suffered both inappropriate ICD shocks for supraventricular tachycardia and less frequent appropriate shocks for VT in the setting of continued nonsynthetic marijuana use. The dose of beta blockers was up-titrated to limit the recurrence of episodes of supraventricular tachycardia.
Discussion
Cannabis is the most prevalent illicit drug used in the United States, with legalization in some states. It is estimated that 89.5% and 10.5% of cannabis use is recreational and medicinal, respectively.1 SC, commonly known as synthetic marijuana, spice, K2, black magic, or crazy clown, are being increasingly abused, especially among high school students.2 They have marijuana-like effects and are not detectable by routine urine drug screen. SC chemical composition differ, as they lack delta-9-tetrahydrocannabinol (THC), the key component of cannabinoids. They stimulate the human cannabinoid receptors (CB1) with a greater binding affinity, as they are full agonists rather than partial agonists. SC are rapidly absorbed into the blood and have longer half-lives, resulting in more rapid and durable cannabinoid effects compared to other cannabinoids (usually 3–5 days).3,4 With an increase in the use of these drugs, an increasing number of patients are being seen in facilities for various complications including rhabdomyolysis, seizures, acute kidney injury, and arrhythmias leading to SCA. Establishing causality of these adverse effects is difficult owing to the lack of available drug assays, and associations have been based on patient- or witness-reported drug use preceding hospital presentation. SCD is the leading cause of death in the United States, with estimates of 350,000–450,000 cases per year. As substance abuse prevalence rises, rates of death including SCD is expected to increase proportionately.5,6
To date, there have been few cases describing SCA related to reported SC use. We systematically searched the published literature for reports of SC-induced out-of-hospital and in-hospital SCA. The articles were collected as of September 2019 using PubMed and Google Scholar. After redundant articles were removed, 5 papers were included in the present study for the final review and analysis. A thorough reading of these articles yielded a total of 6 cases of SC-associated SCA.6, 7, 8, 9, 10 The data of the patients, including demographics, clinical features, comorbid conditions, diagnostic tools, prognosis, and outcomes, are summarized (Supplementary Table S1).
A comprehensive review of these 6 cases revealed male predominance (men, n = 6) and ages from 15 to 56 years (mean = 32 years). This is consistent with results from studies that have reported SC use in male more than in female subjects, specifically in college students.3 Three patients suffered out-of-hospital and 3 patients in-hospital SCA. Two patients had pulseless electrical activity arrest, 2 had asystole (both in-hospital), and 2 pediatric patients had out-of-hospital v-fib arrest. SC use was reported in all of the cases, either by the patients or by any witness immediately preceding the event. Only 1 patient had a positive urine toxicology screen (cocaine and cannabinoids), while the screen was negative in other patients. ECG findings post–cardiac arrest were variable and included sinus tachycardia, atrial fibrillation, sinus bradycardia with asystole, and prolonged QTc. On further cardiac testing including echocardiogram, stress testing, and left heart catheterization, no other cause of arrhythmias was identified, including native coronary artery disease. One patient with known coronary artery disease but with near-normal ejection fraction received an ICD for secondary prevention of SCD. One of the pediatric patients who received an ICD was found to have appropriate therapy for VT. The other pediatric patient underwent electrophysiology study and ablation of an accessory pathway combined with medical management. In the pediatric patient with bradycardia and asystole, who did not require resuscitation, no intervention was done. One patient died and could not be resuscitated, while 1 had a complicated hospital course that led to change in code status and discharge to a long-term care facility.
There is a paucity of data owing to the rarity of this presentation and follow-up regarding the use of secondary-prevention ICD in patients who have SC-associated SCA. Two of 6 patients had an ICD placed and device interrogation data were reported for 1 of them, revealing a potentially appropriate shock. In our patient who received an ICD, follow-up device interrogation revealed multiple appropriate therapies for VT.
Placement of a subcutaneous ICD (S-ICD) or TV-ICD requires individualized shared decision-making. Factors that may favor S-ICD vs TV-ICD include patient age, battery longevity, pacing or antitachycardia pacing indications, detection algorithm–associated risks of inappropriate ICD therapy, risks of endovascular infection, device position, incision size and number, and personal choice based on review of these factors. S-ICD may be a better option in patients with previous infections or those who are at risk of infections, such as intravenous drug users, because they lack the transvenous lead and hence possess lower chances of lead-related infections or lead malfunction.11 The rationale for choosing a TV-ICD in our patient was her young age, the potential need for pacing therapy to allow for optimal therapy of cardiomyopathy and prolonged QTc, and lack of intravenous drug use history.
Appropriate use criteria for ICD implantation lists drug-induced arrhythmias as “rarely appropriate” indication for secondary prophylaxis. The panel consisted of experts in electrophysiology, heart failure, and cardiology.12 However, drug-related arrhythmias may unmask other predispositions to SCD that may not be reversible. In our case, the QTc interval returned to normal after the patient quit SC use; however, appropriate shocks for VT were still observed. We suggest that cases of drug-induced cardiac arrest should not be placed into “reversible causes of cardiac arrest” by default until other SCD susceptibilities have been fully evaluated.13
There is ample data regarding arrhythmogenic potential of nonsynthetic marijuana. While adrenergic stimulation and atrial ischemia from cannabis can lead to atrial arrhythmias, catecholamine surges have been linked with v-fib. The postulated mechanism of long QTc seen in cannabis users involves blocking of the hERG channels. In 1 retrospective analysis of a nationwide pediatric database, QTc prolongation was the most common arrhythmia reported in cannabis users (353 patients, or 513.1 per 100,000 cases of cannabis users).14 Our patient, who initially presented for cardiac arrest from prolonged QTc owing to SC use, later continued to use nonsynthetic marijuana and experienced appropriate shocks for VT.14
Conclusion
This case demonstrates that the reversibility of drug use–related cardiac arrhythmias may uncover other arrhythmic predispositions such as genetic risks or accessory pathways, as described in our literature review. There remains a potential of continued drug use and genetic predispositions may exist in patients that make them susceptible to fatal arrhythmias that are unmasked by drug use. We conclude that in these patients, the reversibility of illicit drug-related SCA should be scrutinized more to identify other predispositions to SCD that would prompt placement of secondary-prevention ICD.
Footnotes
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2020.02.002
Appendix. Supplementary data
References
- 1.Schauer G.L., King B.A., Bunnell R.E., Promoff G., McAfee T.A. Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. Am J Prev Med. 2016;50:1–8. doi: 10.1016/j.amepre.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 2.Mathews E.M., Jeffries E., Hsieh C., Jones G., Buckner J.D. Synthetic cannabinoid use among college students. Addict Behav. 2019;93:219–224. doi: 10.1016/j.addbeh.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Castaneto M.S., Gorelick D.A., Desrosiers N.A., Hartman R.L., Pirard S., Huestis M.A. Synthetic cannabinoids: epidemiology, pharmacodynamics, and clinical implications. Drug Alcohol Depend. 2014;144:12–41. doi: 10.1016/j.drugalcdep.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kocabay G., Yildiz M., Duran N.E., Ozkan M. Acute inferior myocardial infarction due to cannabis smoking in a young man. J Cardiovasc Med (Hagerstown) 2009;10:669–670. doi: 10.2459/JCM.0b013e32832bcfbe. [DOI] [PubMed] [Google Scholar]
- 5.Gunderson E.W., Haughey H.M., Ait-Daoud N., Joshi A.S., Hart C.L. A survey of synthetic cannabinoid consumption by current cannabis users. Subst Abus. 2014;35:184–189. doi: 10.1080/08897077.2013.846288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ibrahim S., Al-Saffar F., Wannenburg T. A unique case of cardiac arrest following K2 abuse. Case Rep Cardiol. 2014;2014:120607. doi: 10.1155/2014/120607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kariyanna T.P., Williams D., Nunez A., Ihsan M., Jayarangaiah A. A case of cardiac arrest following synthetic marijuana (K2) use. Sch J App Med Sci. 2015;3(8A):2779–2782. [Google Scholar]
- 8.Sharma N., Xavier F., Imundo R.J. Synthetic marijuana causing cardiac arrest and seizure in a 16-year-old teenager and review of the literature. J Clin Toxicol. 2016;6:5. [Google Scholar]
- 9.Wan E.E., Frank D., Bang E. Synthetic cannabinoid (k2) related cardiac arrest and death in young drug abuser, D42 critical care case reports: cardiovascular disease and hemodynamics II 2018. Am J Respir Crit Care Med. 2016;193:A6983. [Google Scholar]
- 10.Alam S., Anderson S., Deshpande S., Section on Pediatric Trainees Program Sudden cardiac arrest in the setting of synthetic marijuana use: two interesting cases posing a difficult but important diagnostic dilemma. Pediatrics. 2018;142:478. (1 Meeting Abstract) [Google Scholar]
- 11.Lambiase P.D., Barr C., Theuns D.A. Worldwide experience with a totally subcutaneous implantable defibrillator: early results from the EFFORTLESS S-ICD Registry. Eur Heart J. 2014;35:1657–1665. doi: 10.1093/eurheartj/ehu112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Russo A.M., Stainback R.F., Bailey S.R. ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 appropriate use criteria for implantable cardioverter-defibrillators and cardiac resynchronization therapy: a report of the American College of Cardiology Foundation appropriate use criteria task force, Heart Rhythm Society, American Heart Association, American Society of Echocardiography, Heart Failure Society of America, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Coll Cardiol. 2013;61:1318–1368. doi: 10.1016/j.jacc.2012.12.017. [DOI] [PubMed] [Google Scholar]
- 13.Patel A.M., Singh J.P., Ruskin J.N. Role of implantable cardioverter-defibrillators in patients with methadone-induced long QT syndrome. Am J Cardiol. 2008;101:209–211. doi: 10.1016/j.amjcard.2007.07.068. [DOI] [PubMed] [Google Scholar]
- 14.Ramphul K., Joynauth J. Cardiac arrhythmias among teenagers using cannabis in the United States. Am J Cardiol. 2019;124:1966. doi: 10.1016/j.amjcard.2019.09.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.