Abstract
BACKGROUND
Hypertension (HTN) is one of the most prevalent risk factors for arteriosclerosis and coronary artery disease (CAD). Its side effects can be decreased through the use of some methods and interventions. The present study was conducted with the aim to evaluate the effects of a lifestyle management on blood pressure, heart rate, and body mass index (BMI) of patients with HTN who have undergone angioplasty.
METHODS
This clinical trial was conducted on 2 groups in 3 stages in an educational hospital in Isfahan, Iran, in 2014. The study participants consisted of 60 patients with HTN who had undergone angioplasty. The participants were randomly allocated to the study and control groups. The intervention was implemented in 6 educational sessions during 3 weeks, and then, follow-up was conducted through phone calls in the study group. The collected data were analyzed using independent t-test, chi-square, Mann-Whitney U test, and ANOVA in SPSS software.
RESULTS
Repeated measures ANOVA results indicated that the effect of time (P < 0.001) and group (P = 0.027) on systolic blood pressure (SBP) was significant. The effect of time (P = 0.015) and group (P = 0.040) on diastolic blood pressure (DBP) was also significant. In terms of BMI, both effects of time (P = 0.010) and group (P = 0.034) were significant. However, the effect of time (P = 0.899) and group (P = 0.900) on heart rate was not significant.
CONCLUSION
The lifestyle management program implemented in the present study was effective on decreased DBP, SBP, and BMI in patients with HTN who had undergone angioplasty. Thus, nurses could implement this program as a part of their care provision program for patients.
Keywords: Lifestyle, Hypertension, Body Mass Index, Heart Rate, Angioplasty
Introduction
Hypertension (HTN) is a serious medical condition that significantly increases the risk of heart attack, stroke, kidney failure, and blindness. It is one of the leading causes of premature death worldwide.1 According to the World Health Organization (WHO), 33% of adults in the world are suffering from HTN and it is predicted that its prevalence will increase to 60% by 2025.2 HTN is a manageable and identifiable risk factor for stroke, myocardial infraction (MI), heart failure, aorta dissection, and atrial fibrillation.3
Moreover, HTN is one of the most common risk factors for coronary artery disease (CAD)4, and uncontrolled HTN could lead to extent CAD, which needs different surgical and therapeutic-diagnostic procedures like angioplasty.5
Angioplasty is the most common beneficial therapeutic-diagnostic methods for CAD6 and a low-cost and low-risk method compared to coronary artery bypass. Due to its low risk and high success, today, in the USA, 400000 angioplasties are performed every year.7 In Shahid Chamran Hospital of Isfahan, Iran, alone, 1516 cases of angioplasty and 2550 angioplasties with stent were conducted in the first 6 months of 2003.8
After coronary artery angioplasty, permanence of risk factors, especially HTN, could result in the recurrence of stenosis of the coronary artery or decrease the success rate of treatment.9 Therefore, appropriate interventions to decrease risk factors, especially HTN, are necessary.10
Of the estimated 1.13 billion people who have HTN, fewer than 1 in 5 have it under control.1 According to Eighth Joint National Committee (JNC8) criteria, the algorithm of HTN treatment initiates with correction of lifestyle and continues with different drug regimens.11 Different studies on lifestyle management have showed that changes such as weight loss, Dietary Approaches to Stop Hypertension (DASH), reduced salt consumption, and exercising are effective on lowering blood pressure (BP) and decreasing its complications.12,13
Most people assume themselves healthy and do not sense the necessity to alter their way of life, modify their diet, lower their weight, exercise, and give up smoking until they begin displaying complications.10,14 Only when their disease has reached a progressive phase or they have been diagnosed with diseases such as CAD, do individuals come to the decision to change their lifestyle.15 However, an improvement in the health status of patients with HTN after undergoing angioplasty may cause them to return to their former unhealthy lifestyle. This can potentially result in disease recurrence. However, multiple lifestyle management interventions will hearten and stimulate patients with HTN to adopt and continue lifestyle changes in their everyday life.16
Different methods have been carried out as lifestyle management programs on subjects with HTN and many existing studies have focused on the consequence of a single lifestyle modification plan on BP, pulse rate (PR), and body mass index (BMI). Some previous studies have shown didactic interventions to be effective on the lifestyle of patients with HTN.17-21 Nevertheless, Cook et al. found that their 18-month educational intervention did not have a significant effect on BP monitoring in patients with prehypertension.22
Mokhtari et al. studied a didactic intervention program and found that it was effective on controlling HTN in women suffering from CAD, but it did not have an effect on heart rate (HR).23 Moreover, the study by Paula et al. showed that lifestyle interventions were effective on BP in patients with HTN and diabetes mellitus (DM) type 2, but had no effect on BMI.24 Dekkers et al. conducted a lifestyle intervention among people at risk of ischemic heart disease (IHD) and found that it did not have a significant effect on weight, physical activity, and BP.25
Samiei et al. showed that 4 sessions of lifestyle education during 2 weeks had no effect on reducing BP in patients with HTN.26 Furthermore, the result of another study indicated that purposeful intervention for managing BP did not have a significant effect.27
Due to the difference in the results of studies on the effects of lifestyle modification on hemodynamic parameters and the lack of a comprehensive study with emphasis on all the features of lifestyle change in subjects with HTN who had undergone angioplasty, this research was performed to assess the effect of a management educational program on BP, PR, and BMI in subjects with HTN after angioplasty in Iran.
Materials and Methods
Study design and Participants: This clinical trial was conducted with a 2-group and 3-stage design from November 2014 to April 2015 in an educational hospital in Isfahan, Iran. The trial registration number in the Iranian Registry of Clinical Trials (IRCT) was 2015062420912N3. This study was part of a bigger study titled “Effects of a lifestyle modification program on knowledge, attitude and practice on hypertensive patients with angioplasty.” Another aspect of the results was previously published as another article.28
Based on the studies by Babu,18 and Jafari et al.,28 with the confidence interval (CI) of 95% and test power of 80%, sample size was calculated as 25 subjects in the study and control group. Based on the researchers’ assumption of a 20% drop in the number of subjects, 30 subjects were assigned to each of the two groups.
The study participants were selected using convenient sampling method from among those patients who met the inclusion criteria. A random number table was used to assign the participants to either the study group (n = 30) or the control group (n = 30) which was continued until the predetermined number of subjects was reached.
Using the table of random numbers and moving along the table with odd and even numbers, we selected the number of participants and then put in a block. After the participants were singled out, a numbered cart was opened, whether it was odd or even, the subjects were assigned to each control and study group.
The study inclusion criteria were age of over 40 years, ability to read and write, no experience of dieting, no knowledge of any relaxation technics such as yoga, meditation, and etcetera, lack of any cardiovascular diseases (CVDs) like secondary HTN, DM type 1 and 2, hormone disorders, kidney disorders, and psychiatric diseases, no previous experience of educational programs on BP management, and the presence of the clinical conditions for the intervention. More than 2 sessions of absence from the educational program, experiencing severe acute stress throughout the study, and unexpected changes in BP, which required a change in the dose of drugs, were considered as the exclusion criteria.
To organize the group educational sessions, the study group participants were divided into 2 groups of 8 participants and 2 groups of 7 participants. The follow-up was conducted through contacting each participant by phone call the day before each session.
The educational program was performed in 6 sessions (each lasting 45-60 minutes) during 3 weeks.28,29 Each session consisted of different educational methods such as lecture, question and answer, group discussions and reviewing scenarios, videos, and educational booklets.30 All aspects of lifestyle were included in the lifestyle management program based on the preventive and therapeutic guidelines for HTN (Table 1).31 Moreover, educational booklets were distributed among the participants at the beginning of every session. From the second session onward, after reviewing the previous topics and answering the questions, the performance of patients during the last week was evaluated. Furthermore, one session was held for the patients’ families and the summary of a healthy lifestyle was presented to them. After the last educational session, BP, PR, and weight of each participant in the study and control group were measured. Then, every week for 1 month, the performance of each patient was followed up through phone call conversations about the educational program,30 elimination of performance obstacles, patients' questions, and presentation of encouraging feedback about a healthy lifestyle. The BP, PR, and weight of the participants in both groups were measured again 1 month after the intervention.
Table 1.
Lifestyle management educational program
| Sessions | Content of the educational program |
|---|---|
| First | Definition of HTN, sorting and diagnosing HTN, number of follow-ups and referring to the physician, complications and risk factors of HTN, and methods of treating and controlling HTN |
| Second | "DASH" diet, the importance of diet and its effect on BP control, foods that could lower BP, foods that could increase BP, the right method of cooking food and its importance |
| Third | Appropriate exercise, the importance of increasing physical activity, how to lose weight and its effect on BP control, the risks of weight gain, the advantages of increase in physical activity |
| Fourth | The importance of regular medicine treatment, different types of medicines for lowering BP, medicine interactions and the right consumption method of medicines based on their dose and timing and considering medicine interactions, medicines’ side effects At the end of this session, a scenario about some patients who have experienced acute complications due to lack of BP control was given to the participants and they were asked to study it before the next session. |
| Fifth | Reviewing scenarios in groups, presenting a video about a patient with HTN, methods to manage stress, the advantages of stress management and the effect of stress and tension on BP, relaxation and muscle releasing methods |
| Sixth | The participation of the subjects’ families was demanded to support patients. Participants’ families were informed about the disease, healthy lifestyle, the ways to control the disease, the complications of not controlling the disease, and the role of family’s participation in supporting the patient. At the end of the session, a question and answer session was held for participants and their families. |
HTN: Hypertension; DASH: Dietary Approaches to Stop Hypertension; BP: Blood pressure
Moreover, 2 question and answer sessions were held in the control group on the experience of patients regarding HTN, diet, weight loss, and exercise. Educational booklets were distributed among the participants 1 month after the end of the study.
Data were collected by the researcher's assistant by studying medical records, and measuring BP, PR, height, and weight of the participants.
The researcher-made checklist consisted of information about the disease and background variables (including age, height, sex, education, marital status, and occupation). BP was measured by means of a mercury sphygmomanometer and a standard stethoscope that was calibrated at the beginning and middle of the present research for validity by 2 expert nurses (man and woman) who were authorized by the professors of the School of Nursing and Midwifery in Isfahan University of Medical Sciences, Isfahan, Iran. The study was a single-blind trial, meaning that the assistant researcher who performed the measurements had no knowledge of the study procedure, and BP measurements were controlled. To evaluate BMI, the same digital meter and calibrated scale were used for all participants.
The sphygmomanometer was calibrated by the equipment unit of the hospital, and BP of 10 people was measured twice in 5 minutes to verify its reliability. The interclass correlation coefficient was 0.89, which indicated an acceptable consistency in measurements. To calibrate the scale, a 1 kg sample weight was used. To confirm the reliability of the scale, the weight of 10 people was measured twice in 1 minute. The interclass correlation coefficient was 0.97, which indicated an acceptable consistency in measurements. To calibrate the meter, a metallic meter was used. For calculate BMI, the formulae of weight (kg)/high (m2) was used.
After sampling, written informed consent forms were obtained from all participants. Then, the demographic characteristics form and disease information checklist were completed by the researcher. Considering all the scientific principles, the systolic blood pressure (SBP) and diastolic blood pressure (DBP) of the participants in both groups were measured on their right hand and in sitting position.5,31 A plastic meter was placed on the wall to measure the height of the participants. To measure their weight, the participants were asked to stand on the calibrated scale without shoes and with light clothing.
Verbal and written explanations regarding the study goals and procedures were provided for all the participants and they could leave the study at any stage.
The collected data were analyzed in SPSS software (version 20, IBM Corporation, Armonk, NY, USA). Continuous and categorical variables were reported as mean and standard deviation and absolute number with percentage, respectively. The demographic variables (sex and marital status) were compared between the two groups using chi-square test. In addition, Mann-Whitney test was used for the comparison of education level and economic status, and independent t-test was utilized for the comparison of age, height, and duration of HTN between the groups.
We used dependent t-test to compare mean weight, BMI, SBP, DBP, and PR in each group at three times. In addition, the repeated measures ANOVA with Mauchly’s sphericity test were applied for comparisons between the two groups in the 3 stages in order to show the effect of time and group. P values of lower than 0.05 were considered as significant.
Results
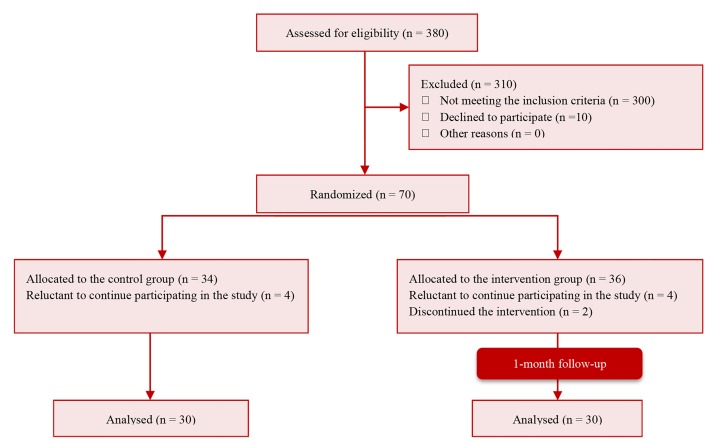
Of the 70 patients with HTN who were entered into the study, 10 were excluded due to their reluctance to continue (8 participants), severe stress (1 participant), and hospitalization during the study (1 participant). Thus, the remaining 60 participants were divided into two groups and their data were analyzed (Figure 1).
Figure 1.
CONSORT flow diagram of the participants
The results showed no statistically significant differences between the two groups in terms of demographic variables. Frequency distribution of marital status was quite similar in the two groups. Chi-square test results showed no significant difference between the groups in terms of the distribution of occupation (P = 0.286). Mann-Whitney test showed no significant differences between the groups in educational level (P = 0.880) and economic level (P = 0.421). Furthermore, independent t-test results showed that the differences in the mean of age (P = 0.114), weight (P = 0.159), height (P = 0.866), and duration of HTN (P = 0.820) between the two groups were not significant before the intervention (Table 2).
Table 2.
Comparison of the mean of demographic variables in the study and control groups before the intervention
| Variable | Study group |
Control group |
P | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Age (year) | 58.4 ± 6.5 | 55.6 ± 6.5 | 0.114* | |
| Height | 169.3 ± 7.9 | 166.2 ± 8.8 | 0.159* | |
| Weight | 79.2 ± 9.5 | 78.8 ± 7.1 | 0.866* | |
| BMI | 27.6 ± 3.1 | 28.7 ± 3.5 | 0.231* | |
| Duration of hypertension (year) | 3.5 ± 3.4 | 3.3 ± 3.1 | 0.820* | |
| n (%) | n (%) | |||
| Occupational status | Employee | 1 (3.3) | 0 | 0.286** |
| Housekeeper | 4 (13.3) | 4 (13.3) | ||
| Retired | 7 (23.3) | 11 (36.7) | ||
| Businessman | 16 (53.3) | 10 (33.3) | ||
| Worker | 2 (6.7) | 5 (16.7) | ||
| Economic level | Low | 12 (40.0) | 9 (30.0) | 0.421*** |
| Moderate | 16 (53.0) | 18 (60.0) | ||
| Good | 2 (7.0) | 3 (10.0) | ||
| Educational level | Primary school | 21 (70.0) | 24 (80.0) | 0.880*** |
| Pre-diploma | 3 (10.0) | 3 (10.0) | ||
| Diploma | 6 (20.0) | 3 (10.0) |
Independent t-test;
Chi-Square test;
Mann-Whitney U test
BMI: Body mass index; SD: Standard deviation
P-value of less than 0.050 was considered as significant.
Independent t-test showed no significant differences between the groups concerning the mean of SBP (P = 0.673), DBP (P = 0.815), BMI (P = 0.231), and PR (P = 0.572) before the intervention.
Mauchly's sphericity test supported homogeneity of variances (P > 0.050). Repeated measures ANOVA showed that the effect of time (P < 0.001) and group (P = 0.027) on SBP was significant.
The effect of time (P = 0.015) and group (P = 0.040) on DBP was also significant. Regarding BMI, both effects of time (P = 0.010) and group (P = 0.034) were significant. However, the effect of time (P = 0.899) and group (P = 0.900) on heart rate was not significant (Table 3).
Table 3.
Comparison of the mean changes in scores of systolic and diastolic blood pressure, pulse rate, and body mass index in the two groups before and immediately and one month after the intervention
| Variable | Time | Study group |
Control group |
Repeated measures |
ANOVA |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | P* | P** | ||
| Systolic blood pressure | Before the intervention | 144.4 ± 18.1 | 142.5 ± 15.2 | 0.027 | < 0.001 |
| Immediately after the intervention | 135.6 ± 13.7 | 140.9 ± 15.3 | |||
| One month after the intervention | 131.7 ± 13.0 | 138.0 ± 15.0 | |||
| Diastolic blood pressure | Before the intervention | 84.3 ± 9.0 | 84.9 ± 10.7 | 0.040 | 0.015 |
| Immediately after the intervention | 80.5 ± 6.5 | 83.3 ± 8.8 | |||
| One month after the intervention | 78.9 ± 6.4 | 83.0 ± 7.3 | |||
| Pulse rate | Before the intervention | 81.9 ± 10.0 | 80.6 ± 7.3 | 0.900 | 0.899 |
| Immediately after the intervention | 79.6 ± 4.6 | 81.8 ± 4.3 | |||
| One month after the intervention | 80.9 ± 5.8 | 80.8 ± 3.8 | |||
| BMI | Before the intervention | 27.7 ± 3.2 | 28.7 ± 3.5 | 0.0340 | 0.010 |
| Immediately after the intervention | 26.7 ± 3.2 | 28.9 ± 3.6 | |||
| One month after the intervention | 26.6 ± 2.7 | 28.9 ± 3.6 |
BMI: Body mass index; SD: Standard deviation
Effect of group;
Effect of time
Discussion
In the present study, the lifestyle management educational program was found to be effective on DBP, SBP, and BMI in patients with HTN who had undergone angioplasty. However, it was not effective on their PR.
Moreover, no significant differences were observed between the two groups in terms of the mean DBP and SBP before and immediately after the intervention. Nevertheless, mean SBP and DBP were significantly lower in the study group compared to the control group 1 month after the intervention. Thus, it seems that the studied lifestyle management program has been effective on these variables during the study period. In different studies, different effects have been reported for non-medical interventions on BP management. Navidian et al. reported a significant reduction in mean SBP and DBP in patients with HTN in the study group compared to the control group 2 months after motivational interviews and lifestyle education.32 No significant difference was observed in SBP between the two groups, but a significant reduction was observed in DBP in the study group compared to the control group in the follow-up period.32 Paula et al. reported a significant reduction in mean SBP 1 month after the intervention (messaging and phone call about dieting and exercising) in patients with HTN and DM type 2 compared to the control group.24
However, they did not observed a significant difference between the two groups in terms of DBP.24 Moreover, the results of a systematic review study showed that multilateral lifestyle interventions implemented during at least 4 weeks could help to reduce SBP in patients with HTN.33 A study conducted in America on a lifestyle management intervention based on the operation the patients had undergone found a reduction in SBP and DBP 3 and 6 months after the interventions.17
Nevertheless, Siavoshi et al. reported that lifestyle management interventions did not have a significant effect on BP.21 Pandit et al. showed that health education did not have a significant effect on BP reduction among patients with HTN.34 Dekkers et al. showed that lifestyle modification interventions did not have a significant effect on BP among individuals at risk of IHD.25 The results of another systematic review study by Aucott et al. showed that magnesium and calcium supplements did not have a significant effect on BP control.16 Furthermore, Reuther et al. found that purposeful interventions regarding BP management did not have a significant effect on SBP and DBP.27
These differences in the results of the present study and that of previous studies could be due to the different educational methods used in these studies (lecture, question and answer, group discussion, reviewing scenarios, videos, and booklets), and the use of an educational program for all aspects of the participants’ lifestyle, supporting the family, and following up on patients who had undergone angioplasty. A decrease in the BP of the study group could be the result of the effectiveness of this lifestyle management program on BP in patients with HTN who had undergone angioplasty.
The results of the present study showed no significant differences between the groups in terms of BMI before the intervention. However, it showed a significant reduction in mean BMI in the study group compared to the control group immediately after the intervention and 1 month after the intervention. This could be indicative of the effectiveness of this lifestyle management program. Moreover, in the study group, synchronous to the reduction in BP, a reduction was also observed in BMI due to utilization of appropriate interventions, trainings, and diets. Mahajan et al. implemented health education interventions regarding BP in the form of group sessions among patients with HTN in India; they reported a reduction in SBP, BMI, and weight in these patients.35
The results of this study showed that after reducing BMI, SBP and DBP had also reduced. Reduction in BMI is one aspect of a healthy lifestyle that could be achieved through an appropriate diet and increase in physical activity. This indicates a relation between a reduction in BP and lifestyle management in the form of losing weight and BMI. It also indicates the effectiveness of the multilateral lifestyle management program in this study.
The findings of Paula et al. were not in accordance with that of the present study; their results indicated that although lifestyle interventions were effective on BP of patients with HTN and DM type 2, they did not have a significant effect on the BMI of these patients.24 Dekkers et al., in their study, displayed that lifestyle management interventions did not have a significant effect on the weight and physical activity of individuals at risk of IHD.25
In the present study, during the study period, a reduction was observed in mean PR in the study group, but this difference was not statistically significant, which could be due to the small sample size or the 1-month follow-up that was not enough for a reduction in PR. Moreover, in the study by Siavoshi et al., the presentation of a cardiac rehabilitation program along with lifestyle educational interventions among coronary artery patients, in addition to the reduction of SBP, reduced PR in these patients.21 Furthermore, Aizawa et al. found that lifestyle intervention, in addition to reducing BMI, decreased PR in patients with prehypertension.36 In the study by Farsi et al., educational interventions had a significant effect on BP and PR of patients with HTN who had undergone coronary artery angiography.37 Mokhtari et al. found that the effect of educational interventions on BP control among women with CAD was significant, but their effect on the patients’ heart rate was not significant.23
The short follow-up period (1 month after the intervention) was an important limitation of this study. Due to the time limitation of the student thesis, we had to limit the follow-up time of these patients after the intervention. Sample volume was another limitation of this study and the selection of a greater number of subjects with the two variables of HTN and angioplasty required more time. Thus, it is recommended that future studies be performed on a larger study population and the follow-up periods be extended.
Conclusion
The present study results showed that the lifestyle management program presented with different educational methods such as group discussion and lectures influenced all aspects of lifestyle along with companionship and support of families. Furthermore, follow-up was effective on reducing SBP, DBP, and BMI in patients with HTN who had undergone angioplasty. Moreover, introducing effective support to families and educating them on how to perform it could be an important factor in improving the lifestyle of patients with HTN. Thus, it seems that in this educational HTN management program, the patients’ families should be regarded as an important factor. In addition, comprehensive lifestyle management programs could be more effective on the well-being of these patients; therefore, it is suggested that nurses use this program as part of their care providing routines for these patients.
Acknowledgments
We are thankful to the personnel of the coronary care unit (CCU) of Shahid Chamran Hospital and patients who participated in this study. This study is adopted from the research project number 393679 from Isfahan University of Medical Sciences. We are thankful for the financial support provided for conducting this research.
Footnotes
Conflicts of Interests
Authors have no conflict of interests.
REFERENCES
- 1.World Health Organization. Cardiovascular disease: World Hypertension Day 2019 [Online]. 2019. Available from: URL: https://www.who.int/cardiovascular_diseases/world-hypertension-day-2019/en.
- 2.Dananagowda H. A study to assess the knowledge and attitude regarding life style modifications to prevent hypertension among bank employees in selected banks at tumkur [Thesis]. Karnataka, India: Rajiv Gandhi University of Health Sciences; 2013. [Google Scholar]
- 3.Kwan MW, Wong MC, Wang HH, Liu KQ, Lee CL, Yan BP, et al. Compliance with the Dietary Approaches to Stop Hypertension (DASH) diet: A systematic review. PLoS One. 2013;8(10):e78412. doi: 10.1371/journal.pone.0078412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eskandarian R, Ghorbani R, Shiyasi M, Momeni B, Hajifathalian K, Madani M. Prognostic role of Helicobacter pylori infection in acute coronary syndrome: A prospective cohort study. Cardiovasc J Afr. 2012;23(3):131–5. doi: 10.5830/CVJA-2011-016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Woods SL, Sivarijan Froelicher ES, Motzer SU, Bridges EJ. Cardiac nursing. Philadelphia, PA: Lippincott Williams & Wilkins; 2009. [Google Scholar]
- 6.Rodrigo R, Hasson D, Prieto JC, Dussaillant G, Ramos C, Leon L, et al. The effectiveness of antioxidant vitamins C and E in reducing myocardial infarct size in patients subjected to percutaneous coronary angioplasty (PREVEC Trial): Study protocol for a pilot randomized double-blind controlled trial. Trials. 2014;15:192. doi: 10.1186/1745-6215-15-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yousef Nejad K. Analysis of survival data in patients with coronary artery after angioplasty to help Kalks regression model [Thesis]. Sari, Iran: Mazandaran University of Medical Sciences; 2012. pp. 101–7. In Persian. [Google Scholar]
- 8.Shahid Chamran Hospital . Medical Record Archive. Isfahan, Iran: Shahid Chamran Hospital; 2013. Unpublished. [Google Scholar]
- 9.Van Belle E, Ketelers R, Bauters C, Perie M, Abolmaali K, Richard F, et al. Patency of percutaneous transluminal coronary angioplasty sites at 6-month angiographic follow-up: A key determinant of survival in diabetics after coronary balloon angioplasty. Circulation. 2001;103(9):1218–24. doi: 10.1161/01.cir.103.9.1218. [DOI] [PubMed] [Google Scholar]
- 10.Sadeghzadeh V, Raoufi Kelachayeh SS, Naserian J. The effect of self-care documented program on performance of patients undergoing coronary angioplasty. Intl Res J Appl Basic Sci. 2013;4(1):86–90. [Google Scholar]
- 11.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 12.Ariff F, Suthahar A, Ramli M. Coping styles and lifestyle factors among hypertensive and non-hypertensive subjects. Singapore Med J. 2011;52(1):29–34. [PubMed] [Google Scholar]
- 13.Svetkey LP, Pollak KI, Yancy WS, Dolor RJ, Batch BC, Samsa G, et al. Hypertension improvement project: randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension. 2009;54(6):1226–33. doi: 10.1161/HYPERTENSIONAHA.109.134874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demaio AR, Otgontuya D, de Court Bygbjerg IC, Enkhtuya P, Meyrowitsch DW, et al. Hypertension and hypertension-related disease in mongolia; findings of a national knowledge, attitudes and practices study. BMC Public Health. 2013;13:194. doi: 10.1186/1471-2458-13-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Song IH, Kim SA, Park WS. Effects of a hypertension management program by Seongcheon primary health care post in South Korea: An analysis of changes in the level of knowledge of hypertension in the period from 2004 to 2009. Health Educ Res. 2012;27(3):411–23. doi: 10.1093/her/cys012. [DOI] [PubMed] [Google Scholar]
- 16.Aucott L, Rothnie H, McIntyre L, Thapa M, Waweru C, Gray D. Long-term weight loss from lifestyle intervention benefits blood pressure?: A systematic review. Hypertension. 2009;54(4):756–62. doi: 10.1161/HYPERTENSIONAHA.109.135178. [DOI] [PubMed] [Google Scholar]
- 17.Schoenthaler A, Luerassi L, Teresi JA, Silver S, Kong J, Odedosu T, et al. A practice-based trial of blood pressure control in African Americans (TLC-Clinic): Study protocol for a randomized controlled trial. Trials. 2011;12:265. doi: 10.1186/1745-6215-12-265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Babu A. Effectiveness of structured teaching programme on knowledge of hypertensive patients regarding dash diet at selected kumbalagudu phc area bangalore [Thesis]. Karnataka, India: Rajiv Gandhi University of Health Sciences; 2013. [Google Scholar]
- 19.Dawes MG, Kaczorowski J, Swanson G, Hickey J, Karwalajtys T. The effect of a patient education booklet and BP 'tracker' on knowledge about hypertension. A randomized controlled trial. Fam Pract. 2010;27(5):472–8. doi: 10.1093/fampra/cmq048. [DOI] [PubMed] [Google Scholar]
- 20.Sharma S, Kc B, Alrasheedy AA, Kaundinnyayana A, Khanal A. Impact of community pharmacy-based educational intervention on patients with hypertension in Western Nepal. Australas Med J. 2014;7(7):304–13. doi: 10.4066/AMJ.2014.2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Siavoshi S, Roshandel M, Zareiyan A, Etefagh L. The effect of cardiac rehabilitation on hemodynamic status in patients after coronary artery bypass surgery. J Cardiovasc Nurs. 2013;2(4):19–27. [Google Scholar]
- 22.Cook NR, Cutler JA, Obarzanek E, Buring JE, Rexrode KM, Kumanyika SK, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: Observational follow-up of the trials of hypertension prevention (TOHP). BMJ. 2007;334(7599):885–8. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mokhtari Z, Alipor A, Hasanzadeh Pashang S, Exirifard M. Effect of emotional intelligence on physical health among heart patient's bed ridden. J Jahrom Univ Med Sci. 2014;12(2):1–12. [Google Scholar]
- 24.Paula TP, Viana LV, Neto AT, Leitao CB, Gross JL, Azevedo MJ. Effects of the DASH diet and walking on blood pressure in patients with type 2 diabetes and uncontrolled hypertension: A randomized controlled trial. J Clin Hypertens (Greenwich) 2015;17(11):895–901. doi: 10.1111/jch.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dekkers JC, van Wier MF, Ariens GA, Hendriksen IJ, Pronk NP, Smid T, et al. Comparative effectiveness of lifestyle interventions on cardiovascular risk factors among a Dutch overweight working population: A randomized controlled trial. BMC Public Health. 2011;11(1):49. doi: 10.1186/1471-2458-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Samiei Siboni F, Alimoradi Z, Sadegi T. Impact of corrective life style educational program on controlling stress, anxiety and depression in hypertensives. J Birjand Univ Med Sci. 2013;19(6):1–9. [Google Scholar]
- 27.Reuther LO, Paulsen MS, Andersen M, Schultz-Larsen P, Christensen HR, Munck A, et al. Is a targeted intensive intervention effective for improvements in hypertension control? A randomized controlled trial. Fam Pract. 2012;29(6):626–32. doi: 10.1093/fampra/cms031. [DOI] [PubMed] [Google Scholar]
- 28.Jafari F, Shahriari M, Sabouhi F, Khosravi FA, Eghbali Babadi M. Effects of a lifestyle modification program on knowledge, attitude and practice of hypertensive patients with angioplasty: A randomized controlled clinical trial. Int J Community Based Nurs Midwifery. 2016;4(4):286–96. [PMC free article] [PubMed] [Google Scholar]
- 29.Rocha-Goldberg MP, Corsino L, Batch B, Voils CI, Thorpe CT, Bosworth HB, et al. Hypertension Improvement Project (HIP) Latino: Results of a pilot study of lifestyle intervention for lowering blood pressure in Latino adults. Ethn Health. 2010;15(3):269–82. doi: 10.1080/13557851003674997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Webber J. The effect of a lifestyle modification adherence tool on risk factors in patients with chronic hypertension compared to usual management [MSc Thesis]. Johannesburg, South Africa: University of the Witwatersrand; 2011. [Google Scholar]
- 31.Wilson DE, Van Vlack T, Schievink BP, Doak EB, Shane JS, Dean E. Lifestyle factors in hypertension drug research: Systematic analysis of articles in a leading cochrane report. Int J Hypertens. 2014;2014:835716. doi: 10.1155/2014/835716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Navidian A, Abedi MR, Baghban I, Fatehizadeh MA, Poursharifi H. Effect of motivational interviewing on blood pressure of referents suffering from Hypertension. Kowsar Medical Journal. 2010;15(2):115–21. [Google Scholar]
- 33.Li J, Zheng H, Du HB, Tian XP, Jiang YJ, Zhang SL, et al. The multiple lifestyle modification for patients with prehypertension and hypertension patients: A systematic review protocol. BMJ Open. 2014;4(8):e004920. doi: 10.1136/bmjopen-2014-004920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pandit AU, Tang JW, Bailey SC, Davis TC, Bocchini MV, Persell SD, et al. Education, literacy, and health: Mediating effects on hypertension knowledge and control. Patient Educ Couns. 2009;75(3):381–5. doi: 10.1016/j.pec.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 35.Mahajan H, Kazi Y, Sharma B, Velhal GD. Health education: An effective intervention in hypertensive patients. International Journal of Recent Trends in Science and Technology. 2012;4(2):77–82. [Google Scholar]
- 36.Aizawa K, Shoemaker JK, Overend TJ, Petrella RJ. Effects of lifestyle modification on central artery stiffness in metabolic syndrome subjects with pre-hypertension and/or pre-diabetes. Diabetes Res Clin Pract. 2009;83(2):249–56. doi: 10.1016/j.diabres.2008.11.016. [DOI] [PubMed] [Google Scholar]
- 37.Farsi Z, Eslami R, Sajadi A, Afaghi E. Comparing the effect of peer education and orientation tour on the hemodynamic indices of patients candidate for coronary angiography. Medical-Surgical Nursing Journal. 2016;4(4):65–72. [Google Scholar]