Abstract
Background:
The purpose of this study was to determine the prevalence and genotype of Cryptosporidium spp. in different groups of immunocompromised patients admitted to the referral hospitals in center of Iran during 2015–2016.
Methods:
This cross-sectional study was conducted on 346 immunocompromised patients (HIV+/AIDS, Lymphoma, Leukemia and organ transplants) in referred hospitals from central parts of Iran including Isfahan, Markazi, Yazd and Chaharmahale Bakhtiari provinces. Stool samples were analyzed for Cryptosporidium species, modified Ziehl–Neelsen staining techniques followed by the semi-nested PCR and DNA sequencing methods.
Results:
The total rate of Cryptosporidium spp. was 3.46% (12/346) in the patients, however, the prevalence of the parasite, was 4.6% (4/87) in HIV+/AIDS patients, 3.6% (6/168) in patients with blood malignancy and 2.1% (2/91) in organ transplant recipients. The SSU rRNA gene of Cryptosporidium spp. in all microscopic-positive samples was effectively amplified by the semi-nested PCR and DNA sequences, exposed the existence of two Cryptosporidium species, including C. hominis 91.6% (11/12) and C. parvum 8.3% (1/12).
Conclusion:
The predominance of C. hominis in the present study may be certifies the importance of anthroponotic transmission of cryptosporidiosis in center of Iran.
Keywords: Cryptosporidium, Immunocompromised patients, Genotype, Iran
Introduction
Nowadays, the number of immunocompromised patients is increasing. They are those with congenital anomalies, HIV/AIDS, organ transplant recipients, cancer patients as well as an enormous population that take immunosuppressive drugs for other disorders (1). Numerous opportunistic infections happen in immunocompromised patients, as a result of impairment of immune system (2) among them Cryptosporidium spp. has been known as an important opportunistic enteric parasite in these patients (3). The organism has a wide-range host that comprises humans and domestic animals all over the world. In developing countries, Cryptosporidium infections take place generally in children younger than 5 yr and in industrialized societies, epidemic cryptosporidiosis can occur in adults via foodborne or waterborne outbreaks (4). Humans acquire Cryptosporidium infections through several routes, such as direct contact with infected persons and animals and/or the ingestion of contaminated food and water (5). This microorganism is an opportunistic parasite causing severe diarrhea, fever, anorexia, dehydration and eventually weakness in immunocompromised patients. The main problem in proper identification of Cryptosporidium spp. is to distinguish oocysts from other small particles in fecal and environmental specimens such as yeasts, molds, algae, and plant debris (6). Currently, 26 species are recognized as valid on the basis of morphological, biological and molecular data. Of the nearly 20 Cryptosporidium species and genotypes reported in humans, Cryptosporidium hominis and Cryptosporidium parvum are responsible for the majority of infections (7). However, handful of studies on the epidemiology and classification of Cryptosporidium species in central Iran are available.
Therefore, the present study aimed to genotypes isolated from immunocompromised patients, in four provinces including Chaharmahale Bakhtiari, Isfahan, Markazi and Yazd, central Iran
Methods
Ethical consideration
This study was approved by Ethics Committee of Isfahan University of Medical Sciences (Isfahan, Iran). In addition, written informed consent was obtained from all the participants before stool sampling. (Ethical approval number: IR.MUI.REC.1396.3.305).
Sampling
Overall, 346 fecal samples were obtained from different groups of immunocompromised ambulatory and hospitalized patients (>15 yr old) including HIV/AIDS, lymphoma, leukemia and organ transplants as of four provinces including Isfahan, Markazi, Yazd and Chaharmahale Bakhtiari located in the central parts of Iran during 2015–2016 (Fig. 1). Of these, 26 patients conferred with diarrhea and 320 did not have diarrhea. All samples were examined by microscopic observation of direct smears applying normal saline and formalin ether concentration techniques and a slide were prepared for each sample, stained with the modified Ziehl-Neelsen acid-fast technique to finding Cryptosporidium as described previously (8). The samples diagnosed as Cryptosporidium positive by microscopic examination were stored in 2.5% potassium dichromate at 4 °C before to DNA extraction.
Fig. 1:
Studied provinces in central Iran including Isfahan, Yazd, Markazi, and Chaharmahal and Bakhtiari
DNA extraction
To maximize DNA extraction for the molecular processing, an initial step of 10 freeze-thaw cycles (freezing in liquid nitrogen for 2 min and heating at 95 °C for 4 min in a water bath) were used to rupture the oocysts for all positive samples and then DNA extraction was carried out using the QIAamp ® Fast DNA Stool Mini Kit 50 (Qiagen, Germany) according to the company’s instructions. Finally, based on the kit instruction, DNA was purified and stored at −20 °C until it was used for PCR analyses.
Semi-nested PCR
A two-step semi-nested PCR protocol for the 18S rRNA gene was performed. The outer forward primer 5′-GGA AGG GTT GTA TTT ATT AGA TAA AG-3′ and common reverse primer Cr 550 5′-TGA AGG AGT AAG GAA CAA CCT CC-3′ were described previously (9). They amplified a ∼835-bp fragment applying the following procedure: 95 °C for 5 min followed by 25 cycles of 94 °C for 40 sec, 53 °C for 30 sec, and 72 °C for 45 sec, and the last extension of 72 °C for 5 min. The second round was performed using the forward primer Cr250 5′-GGA ATG AGT KRA GTA TAA ACC CC-3′ and the reverse primer Cr 550 5′-TGA AGG AGT AAG GAA CAA CCT CC-3′ that could amplify a region with ∼530 bp. The second PCR reaction used 95 °C for 5 min, followed by 35 cycles of 94 °C for 35 sec, 55 °C for 30 sec, and 72 °C for 40 sec, and over a final extension step at 72 °C for 5 min. Amplification done in final volume of 25 μL, containing 12.5 μL of 2X PCR master mix (Ampliqon, Denmark), 10.5 pM of each primer, and 2 μL of DNA using Biorad thermocycler. A sample excluding DNA as negative and a known C. parvum as positive controls were added in each set of PCR. The PCR product was transferred to a 1.5% agarose gel, electrophoresed for 1 h. The gel was stained with safe green and the products were visualized under a UV transilluminator (Uvitec, UK).
DNA sequencing
PCR products were rubbed out from the agarose gel, purified and sequenced directly with the secondary PCR primers using an ABI 3730 sequencer (Bioneer, South Korea), and results were compared with sequences previously pledged in the GenBank database, using National Center for Biotechnology Information (NCBI-BLAST) software.
Statistical analysis
The results were analyzed by Mann–Whitney, chi-square and Fisher exact tests by statistical software SPSS ver. 16 (Chicago, IL, USA) with a P-value of <0.05.
Results
Stool samples from 346 individuals consisted of 87 (25.1%) patients with HIV+/AIDS, 168 (48.5%) patients with malignancy (Lymphoma and Leukemia), and 91 (26.3%) patients with transplant recipient were submitted to the parasitology laboratory of Isfahan University of Medical Sciences, Isfahan, Iran to find Cryptosporidium (Fig. 2). Numbers and percentages of people diagnosed with cryptosporidiosis in the studied provinces in Iran are shown in Table 1.
Fig. 2:
Cryptosporidium oocysts in the stool sample of an immunocompromised patient (×1000)
Table 1:
The provincial frequency of Cryptosporidium species among immunocompromised Patients, central Iran
| Province | Tested Cases n (%) | Infected Cases n (%) | Cryptosporidium Species |
|---|---|---|---|
| Isfahan | 204 | 8(3.9) | C. hominis |
| Yazd | 41 | 2 (4.8) | C. hominis |
| Markazi | 60 | 0 (0.0) | - |
| Chaharmahal and Bakhtiari | 41 | 2 (4.8) | C. hominis, C. parvum |
High prevalence of HIV/AIDS patients is reported from Chaharmahale Bakhtiari Province (31.7%) and in case of blood malignancy, Yazd and Markazi provinces have the higher percentage of patients with hematologic malignancies (63.4% and 63.3% respectively) and finally, we found the highest rate of organ transplantation in Isfahan province (31.8%). The total rate of Cryptosporidium infection was 3.46% (12 /346) in the patients however the prevalence of the parasite was 4.6% (4/ 87) in HIV/AIDS patients, 3.6% (6/168) in patients with blood malignancy and 2.1% (2/91) in organ transplant recipients by modified Ziehl-Neelsen technique.
We found a statistically significant difference in material status (P=0.005) and type of stool (P=0.001) among the immunocompromised patients. A higher infection rate was observed in patients more 60 yr of age. There was no significant correlation between the prevalence rate of Cryptosporidium infection and other study variables (Table 2).
Table 2:
Sociodemographic characteristics of immunocompromised patients, according to the presence or absence of Cryptosporidium species, central Iran
| Variable | Infected (%) | Non-infected (%) | Total | P-value | |
|---|---|---|---|---|---|
| Sex | Female | 4 (2.4) | 162(97.6) | 166 | 0.301 |
| Male | 8(4.4) | 172(95.6) | 180 | ||
| Age group(yr) | ≤ 45 | 4(3.4) | 113(96.6) | 117 | 0.76 |
| 46–59 | 4(3.0) | 131(97.0) | 135 | ||
| ≥60 | 4(4.3) | 90(95.7) | 94 | ||
| Education | Illiterate | 1 (1.8) | 56(98.2) | 57 | 0.53 |
| Elementary school | 8(6.2) | 121(93.8) | 129 | ||
| Secondary school or higher | 3(1.9) | 157(98.1) | 160 | ||
| Residence | Urban | 10(3.5) | 274(96.5) | 284 | 0.91 |
| Rural | 2(3.2) | 60(96.8) | 62 | ||
| Occupation | Employee | 2(3.1) | 62(96.9) | 64 | 0.82 |
| Retired | 2(8.0) | 23(92.0) | 25 | ||
| Self-employer | 4(3.7) | 103(96.3) | 107 | ||
| House keeper | 3(2.6) | 113(97.4) | 116 | ||
| Unemployed | 1(2.9) | 33(97.1) | 34 | ||
| Marital status | Single | 0(0.0) | 78(100) | 78 | 0.005 |
| Married | 12(5.3) | 213(94.7) | 225 | ||
| Divorced | 0(0.0) | 43(100) | 43 | ||
| Type of Stool | Normal | 7 (2.2) | 313(97.8) | 320 | 0.001 |
| Diarrhea | 5(19.2) | 21(80.8) | 26 |
The SSU rRNA gene of Cryptosporidium in all 12 microscopy-positive samples was effectively amplified by the semi-nested PCR (Fig. 3).
Fig. 3:

PCR of Cryptosporidium isolates from Iranian immunocompromised patients based on SSU rRNA gene. Lanes 1–3 Cryptosporidium isolates, NC: Negative control, PC: Positive control, M: DNA size marker (100 bp)
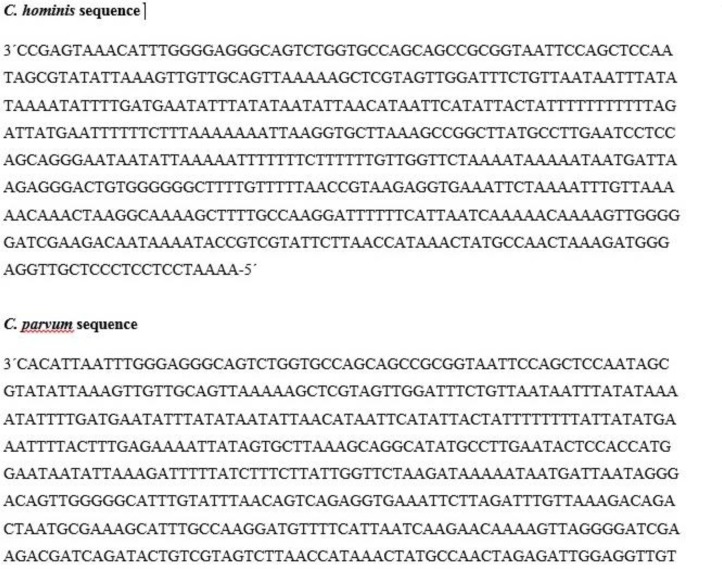
For species and genotype identification, the PCR positive products of the 18s rRNA gene of 12/346 specimens from immunocompromised patients were sequenced. Of these human specimens, 1 had 99% similarity with the C. parvum (GenBank accession no. AF159111); 12 had 98% similarity with the C. hominis (GenBank accession no. KJo19854). Fig. 4 shows the sequences of Cryptosporidium parasites isolated from the studied patients.
Fig. 4:
DNA sequences related to C. hominis and C. parvum
All of the positive samples from Isfahan and Yazd provinces (8 and 2 cases respectively) were C. hominis and one case (of 2) from Chaharmahale Bakhtiari was typed as C. parvum and another one was C. hominis. We did not find any Cryptosporidium in Markazi province neither with Ziehl-Neelsen nor by molecular techniques.
Discussion
As a result of increasing the rate of immunodeficiency syndromes, cases with congenital/acquired immunodeficiency disorders, persons who suffering from malignancy undergoing chemotherapy, organ transplant recipients and patients with Human Immunodeficiency Virus (HIV), we have to pay more attention to the intestinal opportunistic parasites. Among the parasites that affect the gastrointestinal system, the protozoan parasite, Cryptosporidium is one of the most important intestinal organism that is a principal cause of digestive diseases in humans. This microorganism often causes chronic, and serious intestinal diseases leads to morbidity and mortality (10), therefore, cryptosporidiosis is a considerable public health problem across the world with a high variety of prevalence.Our results showed statistically significant differences between material status (P=0.005) and type of stool (P=0.001). These findings are similar to Mohaghegh et al (1) and Izadi et al (11). There was no correlation between the infection and age, sex etc. (Table 2) similar to recent studies (12, 13).
The prevalence of Cryptosporidium infection in immunocompromised patients in Iran was reported as 4.7% in Isfahan (2), 11.5% in Kashan (14), 35.9% in Mashhad (15) and 0.9% in Tehran (16). Epidemiological studies in Ethiopia, India, Egypt, Cameron, Malaysia, Indonesia, China, Australia, Turkey, Philippines, Iraq and Uganda was 13.2%, 21%, 60.2%, 19%, 12.4%, 4.7%, 8.3%, 2.3%, 4%, 1.9%, 18.9% and 25% respectively (17–28).
Our findings revealed that the overall frequency of the parasite was 3.46% (12 /346) in the patients. Many studies have been conducted on the prevalence of various intestinal parasites in Iran (14, 29–32) but few molecular studies have been done on the parasite in immunocompromised patients in center of Iran. Based on two studies in southern Iran, 5.1% and 9.5% of immunocompromised patients were infected with Cryptosporidium spp. respectively which is more than our findings and despite of our study, in another research the ELISA technique was used (12, 31).
This study accented that dominant species of Cryptosporidium was C. parvum (33 out of 34 patients), and only one patient was infected with C. andersoni (31), whereas in our study C. parvum and C. hominis were detected. The high proportion of C. hominis may be due to the great prevalence of anthroponotic cryptosporidiosis in this region. In Iran, isolates of Cryptosporidium from human and animal hosts were described and three species, C. parvum, C. hominis, and C. meleagridis, were identified, so that, C. parvum was the principal species found in humans which is not in agreement with our findings (33). The obvious prevalence of C. parvum in the report might be considered the result of zoonotic transmission (33). In Mazandaran Province in the north of Iran, in the 64 HIV+/AIDS patients, 9.4% were infected with Cryptosporidium. In this study, researchers have used regular techniques including formalin-ether concentration and modified Ziehl Neelsen staining, while we used the above conventional methods followed by molecular procedures. However, compared to the mentioned report, our finding revealed a less rate of Cryptosporidium spp. in center of Iran (34).
This difference may be due to the climate variation between the north and the central regions of Iran and also, the group studied in the study was only those with AIDS, but our study included AIDS, blood malignancies and organ transplantation. In a study on HIV/AIDS patients in Tehran, the capital of Iran, HIV-positive patients were studied and 21 subjects were found to be infected with C. hominis (71%) or C. parvum (29%). These results are similar to our study, so our findings showed the most prevalent Cryptosporidium species was C. hominis, seen in 91.6% of the study patients (35). Based on another report from Tehran, during a study conducted on children, in the 794 collected samples, 19 (2.4%) were positive for Cryptosporidium oocysts.
Sequences analysis showed that 17 (89.4%) of the positive isolates were C. parvum and 2 (10.5%) were C. hominis that the result is in contrast with our findings. The author overlooks the importance of zoonotic Cryptosporidium transmission in Iran (36). In Tehran Province, on humans and cattle, C. parvum was the dominant parasite causing cryptosporidiosis in humans in Iran (37) which is similar to results that revealed, all of the collected samples from children in the north of Iran (100%) were C. parvum and, emphasized the zoonotic transmission of cryptosporidiosis in this area (38). According to WHO reports, intestinal parasite infections are widely spread throughout the world so that some 3.5 billion people worldwide are affected, also in Iran, intestinal parasite infections are still a considerable public health problem (39).
Conclusion
The importance of opportunistic parasitic infections among immunocompromised patients must not be neglected and we recommend additional, larger, Well-designed studies to determine the prevalence of these microorganisms. C. hominis was the most prevalent species in this survey, which this result is an insistence of anthroponotic transmission of cryptosporidiosis in center of Iran, however, such emphasis is still on conflict.
Acknowledgements
Authors appreciate counseling help of M. Agholi, M. Falahati, R. Mohamadimanesh, M. Ghomashlooyan and remarkable assistance of staff from Department of Medical Parasitology and Mycology, Isfahan University of Medical Sciences and the related hospitals during sampling.
Footnotes
Financial support
This survey was supported by Isfahan University of Medical Sciences with grant number: 396305.
Conflict of interests
The authors declare that there is no conflict of interest.
References
- 1.Mohaghegh MA, Hejazi SH, Ghomashlooyan M, Kalani H, Mirzaei F, Azami M. Prevalence and clinical features of Cryptosporidium infection in hemodialysis patients. Gastroenterol Hepatol Bed Bench. 2017;10(2):137–42. [PMC free article] [PubMed] [Google Scholar]
- 2.Azami M, Moghaddam DD, Salehi R, Salehi M. The identification of Cryptosporidium species (protozoa) in Ifsahan, Iran by PCR-RFLP analysis of the 18S rRNA gene. Mol Biol (Mosk). 2007;41(5):934–9. [PubMed] [Google Scholar]
- 3.Cranendonk RJ, Kodde CJ, Chipeta D, Zijlstra EE, Sluiters JF. Cryptosporidium parvum and Isospora belli infections among patients with and without diarrhoea. East Afr Med J. 2003;80(8):398–401. [PubMed] [Google Scholar]
- 4.Xiao L, Ryan UM. Cryptosporidiosis: an update in molecular epidemiology. Curr Opin Infect Dis. 2004;17(5):483–90. [DOI] [PubMed] [Google Scholar]
- 5.Xiao L. Molecular epidemiology of cryptosporidiosis: an update. Exp Parasitol. 2010;124(1):80–9. [DOI] [PubMed] [Google Scholar]
- 6.Fayer R, Morgan U, Upton SJ. Epidemiology of Cryptosporidium: transmission, detection and identification. Int J Parasitol. 2000;30(12–13):1305–22. [DOI] [PubMed] [Google Scholar]
- 7.Ryan U, Fayer R, Xiao X. Cryptosporidium species in humans and animals: current understanding and research needs. Parasitol. 2014;141:1667–85. [DOI] [PubMed] [Google Scholar]
- 8.Casemore DP, Armstrong M, Sands RL. Laboratory diagnosis of cryptosporidiosis. J Clin Pathol. 1985;38(12):1337–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranjbar R, Mirhendi H, Izadi M, Behrouz B, Mohammadi Manesh R. Molecular identification of Cryptosporidium spp. in Iranian dogs using semi-nested PCR; a first report. Vector-Borne Zoonotic Dis. 2018;18(2):96–100. [DOI] [PubMed] [Google Scholar]
- 10.Pawlowski SW, Warren CA, Guerrant R. Diagnosis and treatment of acute or persistent diarrhea. Gastroenterology. 2009;136(6):1874–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Izadi M, Jonaidi-Jafari N, Saburi A, Eyni H, Rezaiemanesh MR, Ranjbar R. Prevalence, molecular characteristics and risk factors for cryptosporidiosis among Iranian immunocompromised patients. Microbiol Immunol. 2012;56(12):836–42. [DOI] [PubMed] [Google Scholar]
- 12.Dehkordy AB, Rafiei A, Alavi SM, Latifi SM. Prevalence of Cryptosporidium infection in immunocompromised patients,in South-West of Iran,2009–10. Iran J Parasitol.2010;5(4):42–7. [PMC free article] [PubMed] [Google Scholar]
- 13.Yang Y, Zhou YB, Xiao PL, et al. Prevalence of and risk factors associated with Cryptosporidium infection in an underdevelopedrural community of southwest China. Infect Dis Poverty. 2017;9;6(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rasti S, Hassanzadeh M, Hooshyar H, Momen-Heravi M, Mousavi SGA, Abdoli A. Intestinal parasitic infections in different groups of immunocompromised patients in Kashan and Qom cities, central Iran. Scand J Gastroenterol. 52(6–7):738–41. [DOI] [PubMed] [Google Scholar]
- 15.Zabolinejad N, Berenji F, Eshkaftaki EB, Badeii Z, Banihashem A, Afzalaqaei M. Intestinal parasites in children with lymphohematopoietic malignancy in Iran, Mashhad. Jundishapur J Microbiol. 2013;6(6): e7765. [Google Scholar]
- 16.Meamar A, Rezaian M, Mohraz M, Zahabian F, Hadighi R, Kia E. A comparative analysis of intestinal parasitic infections between HIV+/AIDS patients and non-HIV infected individuals. Iranian J Parasitol. 2007;2(1):1–6. [Google Scholar]
- 17.Shimelis T, Tassachew Y, Lambiyo T. Cryptosporidium and other intestinal parasitic infections among HIV patients in southern Ethiopia: significance of improved HIV-related care. Parasites & Vectors. 2016;9:270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yadav P, Khalil S, Mirdha BR. Molecular appraisal of intestinal parasitic infection in transplant recipients. Indian J Med Res. 2016;144(2):258–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdel-Hafeez EH, Ahmad AK, Ali BA, Moslam FA. Opportunistic parasites among immunosuppressed children in Minia district, Egypt. Korean J Parasitol. 2012;50(1):57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nkenfou CN, Nana CT, Payne VK. Intestinal Parasitic Infections in HIV infected and non-infected patients in a low HIV prevalence region, West-Cameroon. PLoS ONE. 2013;8(2):e57914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asma I, Johari S, Sim BL, Lim YA. How common is intestinal parasitism in HIV-infected patients in Malaysia? Trop Biomed. 2011;28(2):400–10. [PubMed] [Google Scholar]
- 22.Idris NS, Dwipoerwantoro PG, Kurniawan A, Said M. Intestinal parasitic infection of immunocompromised children with diarrhoea: clinical profile and therapeutic response. J Infect Dev Ctries. 2010;4(5):309–17. [DOI] [PubMed] [Google Scholar]
- 23.Tian LG, Chen JX, Wang TP, et al. Co-infection of HIV and intestinal parasites in rural area of China. Parasit Vectors. 2012;5:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stark D, Fotedar R, van Hal S, et al. Prevalence of enteric protozoa in human immunodeficiency virus (HIV)-positive and HIV-negative men who have sex with men from Sydney, Australia. Am J Trop Med Hyg. 2007;76(3):549–52. [PubMed] [Google Scholar]
- 25.Aksoy U, Erbay A, Akisu C, Apa H, Ozkoc S, Ozturk S. Intestinal parasites in children with neoplasms. Turk J Pediatr. 2003;45(2):129–32. [PubMed] [Google Scholar]
- 26.Natividad FF, Buerano CC, Lago CB, et al. Prevalence rates of Giardia and Cryptosporidium among diarrheic patients in the Philippines. The Southeast Asian J Trop Med Public Health. 2008;39(6):991–9. [PubMed] [Google Scholar]
- 27.Al-alousi TI, Mahmood OI, editors. Detection of Cryptosporidium oocysts in calves and children in Mosul, Iraq. Proc 11th Vet Sci Conf 2012. [Google Scholar]
- 28.Tumwine JK, Kekitiinwa A, Nabukeera N, et al. Cryptosporidium parvum in children with diarrhea in Mulago Hospital, Kampala, Uganda. Am J Trop Med Hyg. 2003;68(6):710–5. [PubMed] [Google Scholar]
- 29.Barazesh A, Fouladvand M, Tahmasebi R, Heydari A, Fallahi J. The prevalence of intestinal parasites in hemodialysis patients in Bushehr, Iran. Hemodial Int. 2015;19(3):447–51. [DOI] [PubMed] [Google Scholar]
- 30.Omrani VF, Fallahi S, Rostami A, et al. Prevalence of intestinal parasite infections and associated clinical symptoms among patients with end-stage renal disease undergoing hemodialysis. Infection. 2015;43(5):537–44. [DOI] [PubMed] [Google Scholar]
- 31.Agholi M, Hatam GR, Motazedian MH. Microsporidia and coccidia as causes of persistence diarrhea among liver transplant children: incidence rate and species/genotypes. Pediatr Infect Dis J. 2013;32(2):185–7. [DOI] [PubMed] [Google Scholar]
- 32.Azami M, Sharifi M, Hejazi SH, Tazhibi M. Intestinal parasitic infections in renal transplant recipients. Braz J Infect Dis. 2010;14(1):15–8. [DOI] [PubMed] [Google Scholar]
- 33.Meamar AR, Guyot K, Certad G, et al. Molecular characterization of Cryptosporidium isolates from humans and animals in iran. Appl Environ Microbiol. 2007;73(3):1033–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Daryani A, Sharif M, Meigouni M, et al. Prevalence of intestinal parasites and profile of CD4+ counts in HIV+/AIDS people in north of Iran, 2007–2008. Pak J Biol Sci. 2009;12(18):1277–81. [DOI] [PubMed] [Google Scholar]
- 35.Zavvar M, Sadraei J, Emadi H, Pirestani M. The use of a semi-nested PCR-RFLP technique, based on the parasite’s 18S ribosomal RNA, to characterise Cryptosporidium isolates from HIV/AIDS patients. Ann Trop Med Parasitol. 102(7):597–601. [DOI] [PubMed] [Google Scholar]
- 36.Taghipour N, Nazemalhosseini-Mojarad E, et al. molecular epidemiology of cryptosporidiosis in iranian children, Tehran, Iran. Iran J Parasitol. 2011;6(4):41–5. [PMC free article] [PubMed] [Google Scholar]
- 37.Nazemalhosseini-Mojarad E, Haghighi A, Taghipour N, et al. Subtype analysis of Cryptosporidium parvum and Cryptosporidium hominis isolates from humans and cattle in Iran. Vet Parasitol. 2011;179(1–3):250–2. [DOI] [PubMed] [Google Scholar]
- 38.Sharbatkhori M, Nazemalhosseini Mojarad E, Taghipour N, Pagheh AS, Mesgarian F. Prevalence and genetic characterization of Cryptosporidium Spp. in diarrheic children from Gonbad Kavoos city, Iran. Iran J Parasitol. 2015;10(3):441–7. [PMC free article] [PubMed] [Google Scholar]
- 39.Luong TV. De-worming school children and hygiene intervention. Int J Environ Health Res. 2003,13 Suppl 1:S153–9. [DOI] [PubMed] [Google Scholar]