Abstract
Background
Neonates undergoing skin-to-skin contact (SSC) have shown to have better cardiovascular stability, improved duration of breastfeeding, temperature maintenance and bonding. The primary objective was to estimate the existing prevalence of SSC among mother–infant dyads in the first hour after vaginal delivery, and the secondary objective was to ascertain the factors affecting adherence of SSC after vaginal delivery.
Methods
This cross-sectional study was carried out in a tertiary care teaching hospital between September 2017 and December 2017. All mother–newborn dyads in the labour room were eligible for the study. Mothers with their newborns, who gave multiple births, or with major congenital malformations or those requiring any form of resuscitation or having respiratory distress or requiring observation in neonatal intensive care unit (NICU) were excluded. All included mother–newborn dyads, after exclusion, were observed for SSC, and the duration in each dyad was recorded. All enrolled mothers, the attending doctors and nurses were asked questions based on a prevalidated questionnaire for the possible barriers of implementation.
Results
Of a total of 164 mother–infant dyads studied, only 34 (20.7%) carried out SSC for more than 30 min. Sixty-two (37.8%) mother–infant dyads did not participate in any SSC. The commonest reason for non-adherence to SSC was unawareness about the practice in 82.25%, followed by pain and exhaustion after the labour process in 8%.
Conclusion
The rate of SSC at birth is suboptimal, and the commonest reason is lack of awareness about this important step of essential newborn care.
Keywords: Skin-to-skin contact, Hypothermia, Barriers
Introduction
Early neonatal mortality (in less than 7 days of birth) has not shown a significant decline in our country, despite an array of interventions and programmes in the past.1 Although postnatal care (PNC) has been an important component of various interventions, the focus has been merely on the presence of skilled attendant at birth. Antenatal care and health education component especially pertaining to PNC has often been suboptimal at large.2 In many hospitals setups, hypothermia is tackled through the use of radiant warmers rather than promotion of skin-to-skin contact (SSC). Also in PNC education of health staff, the emphasis has been on early breast feeding and keeping the baby warm to address hypothermia by wrapping the baby in a warm towel, keeping a room heater, switching off the fan, delay bathing, and so on.3, 4 In rural setup, neonatal care by Accredited Social Health Activist (ASHA) has been mainly focussing on postnatal home visits to ensure breast feeding. Mother's specific training on SSC and its advantages to the baby are often missing.5 Moreover, the majority of the health-care staff feels that SSC is a component of kangaroo mother care which is to be practiced by the mothers with a low birth weight baby only.
This no cost intervention has multiple benefits for both the mother and child and needs to be stressed upon by the health staff to the mothers. Neonates undergoing SSC has shown to have higher stability of the cardiovascular system, improving duration of breastfeeding and temperature maintenance. It also facilitates self-regulation and decreases stress associated with birth.6 SSC also has maternal benefits in terms of decreasing mean time of placental expulsion7 and decreased need of analgesics after delivery.8 Despite so many advantages, there is not much acceptance for SSC among both the mothers and the caregivers,9 whereas there are recommendations by both the World Health Organization (WHO) and the Government of India to put the neonate naked and prone on the mother's bare chest and abdomen at birth.10, 11 Hence, we planned this cross-sectional study to estimate the existing prevalence of SSC among mother–baby dyads soon after vaginal delivery in a tertiary care teaching hospital and also to ascertain the barriers, if any, affecting adherence of SSC after vaginal delivery.
Materials & methods
This cross-sectional study was carried out in the labour room of a tertiary care teaching hospital in western India between September 2017 and December 2017. Ours is a teaching hospital for both undergraduate and postgraduate medical and nursing courses. The number of total deliveries in our hospital in a year is about 2400, with about 38% caesarean deliveries. Each delivery is attended by nurses and/or postgraduate resident doctors in obstetrics and gynaecology. The newborn is received by a nurse most of the time, and a resident doctor in paediatrics is called in case of any anticipated or actual complications in the baby. There are also undergraduate students of MBBS and students of BSc nursing in attendance or assisting deliveries. There are functional radiant warmers available in the delivery room with all resuscitation equipment. The health-care workers in the delivery room are regularly educated about need and procedure of placing newborn babies not requiring resuscitation on their mother's chest and abdomen soon after birth. The procedure of SSC that is expected in all uncomplicated deliveries is as follows: as soon as the baby is born, the baby needs to be dried and warmed on mother's chest and abdomen; after this, uninterrupted SSC is to be started immediately or within 5 min after birth (in case baby is taken to radiant warmer), and SSC to be continued ideally for at least an hour. SSC means placing dried, unclothed newborn on the mother's bare chest, with warmed blanket or towel covering baby's back. Covering of head with a cap, legs with socks, and a vest with front open is also encouraged. Breast feeding is to be initiated and supported during SSC.
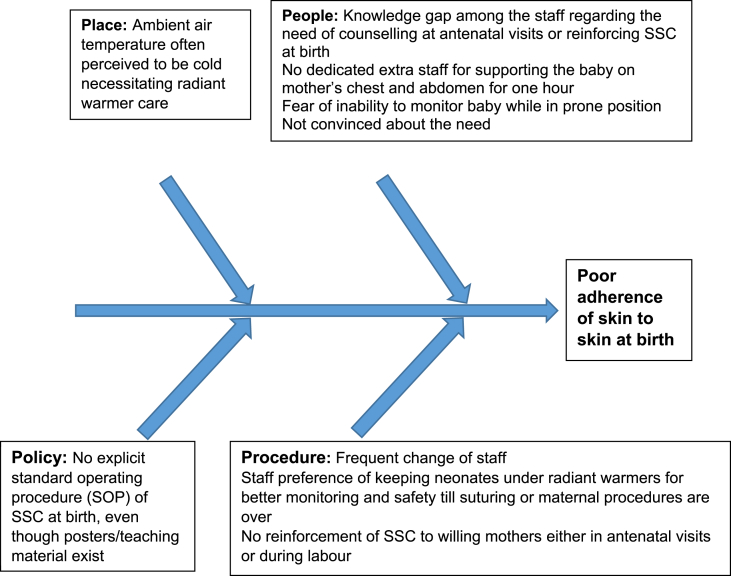
Before commencing the study, an informed written consent was obtained from each mother and the study was approved by the Institutional Ethics Committee. All mother–newborn dyads in the labour room were eligible for the study. Mothers with their newborns who gave multiple births or were with major congenital malformations or those requiring any form of resuscitation or having respiratory distress or requiring observation in NICU were excluded. After excluding the above cases, all included mother–newborn dyads were observed for SSC prospectively, and the duration in each dyad was recorded by the principal investigator, who was not involved with the delivery and immediate PNC. All these enrolled mothers were then asked questions after 1 h of birth to know the factors (barriers) for adherence to SSC, based on the questionnaire which was previously validated among three independent neonatologists. A qualitative study was also performed by asking questions regarding possible barriers to all the attending doctors and nurses of the deliveries. A fishbone analysis was made depending on the responses that we received from the respondents. The primary objective was to estimate the existing prevalence of SSC among mother–baby dyads in the first hour after vaginal delivery, and the secondary objective was to ascertain the factors affecting adherence of SSC after vaginal delivery.
Sample size and statistical analysis
Sample size was calculated to estimate at 95% confidence interval for proportion of mothers adhering to SSC at the first hour after birth, among the newborns born with 5% absolute error of margin and finite correction (600 deliveries in 3 months of which minimum 50% occur vaginally, i.e.300). The sample worked out to be 164 assuming that 50% mothers would adhere to SSC. The collected data were recorded in a Microsoft Excel, sheet and statistical analysis was performed using SPSS 21 version. Descriptive statistics was used to describe the baseline variables (patient particulars, parity, education, Antenatal Care (ANC) visits, birth weight, birth order, obstetric history, maternal complications and neonatal complications). For categorical variables, Chi-square test was used, and for continuous variables, independent t test or Mann–Whitney U test was used. P value of <0.05 was considered as significant.
Results
A total of 164 mother–infant dyads were studied. The baseline characteristics are depicted in Table 1. Most of the participant mothers were between 20 and 29 years of age. Almost all mothers had adequate number of ANC visits. Of 164 mothers interviewed, 143 (87.2%) mothers were at least class X passed. Hundered fifty-four (93.9%) infants born were term and 136 (82.9%) infants weighed more than 2.5 kg. Of the mother–infant dyads studied, overall, only 34 (20.7%) did SSC for more than 30 min and in them 18 (10.9%) did full SSC for an hour. Sixty-eight (41.4%) mothers did SSC for less than 30 min, and 62 (37.8%) mother–infant dyads did not participate in any SSC. The common reasons for non-adherence to SSC (n = 62) were found to be unawareness about the practice in 51 (82.25%), followed by pain and exhaustion after the labour process in 5 (8%) of all mothers studied (Table 2). The most important factor having to bear on SSC acceptance by the mother was awareness about the need of SSC at birth. There was no correlation found with other factors such as educational status of the mother; age of the mother; parity; number of ANC visits; birth weight of the neonate; gender of the neonate; privacy as perceived by the mother; ambient temperature; the immediate surroundings such as bed area, lighting and cleanliness or timings of delivery (Table 3). A total of 17 health-care staff working during this period in the labour room were also interviewed. Even though all believed SSC to be beneficial to both the mother and her baby, only 13 (76.4%) staff advised SSC at birth to the mothers of the newborn, and in those who advised, 12 advised SSC for complete 1 h. A fishbone analysis was also attempted depending on the responses of the health-care staff (Fig. 1), so that necessary corrective actions are taken to improve the situation.
Table 1.
Baseline characteristics (n = 164).
| Baseline variables | N (%) |
|---|---|
| Age | |
| <20 | 8 (4.8) |
| 20–29 | 140 (85.3) |
| >29 | 16 (9.7) |
| Educational status | |
| Below matriculation | 21 (12.8) |
| Matriculation qualified | 89 (54.2) |
| Graduate | 40 (24.3) |
| Postgraduate | 14 (8.5) |
| Parity | |
| Primipara | 60 (36.5) |
| Multipara | 104 (63.4) |
| Number of ANC visits | |
| <4 | 4 (2.4) |
| ≥4 | 160 (97.5) |
| Maturity | |
| Preterm | 10 (6) |
| Term | 154 (93.9) |
| Birth weight | |
| Low birth weight | 28 (17) |
| Normal birth weight | 136 (82.9) |
| Growth status | |
| Appropriate for gestational age | 129 (78.6) |
| Small for gestational age | 15 (9.1) |
| Large for gestational age | 20 (12.1) |
| Gender ofthenewborn | |
| Male | 87 (53%) |
| Female | 77 (46.9%) |
Table 2.
Factors leading to non-adherence (no skin-to-skin contact after birth) and perception of mothers.
| Factors responsible for non-adherence | (n = 62) |
| Unawareness about practice | 51 (82.25%) |
| Pain and exhaustion of labour process | 5 (8.06%) |
| Had prior knowledge but no one reinforced it was necessary | 4 (6.54%) |
| Not interested | 1 (1.6%) |
| Felt uncomfortable | 1 (1.6%) |
| Knowledge about benefits of practice | |
| Yes | 8 (12.9%) |
| No | 54 (87.09%) |
| Lack of privacy in labour room | |
| Yes | 4 (6.46%) |
| No | 58 (93.54%) |
| Inappropriate (low) temperature of labour room | |
| Yes | 11 (17.74%) |
| No | 51 (82.2%) |
| Inappropriate facilities (bed, light, hygieneandcleanliness) | |
| Yes | 2(3.22%) |
| No | 60 (96.7%) |
| Opinion of mother after being counselled about skin-to-skin practice | |
| She thinks it is important for her as well as her baby | 60 (96.77%) |
| What can be done to improvetherate of skin-to-skin care practice | |
| The mother should be communicated about the practice and the correct procedure for the same through demonstrations by the health-care provider | 60 (96.77%) |
Table 3.
Factors affecting skin-to-skin contact (n = 164).
| Variable | Skin-to-skin contact |
Chi-square | p value | |
|---|---|---|---|---|
| Contact | No contact | |||
| Education status | 1.371 | 0.71234 | ||
| Below class X | 11 | 10 | ||
| X to XII | 55 | 34 | ||
| Graduate | 27 | 13 | ||
| Postgraduate | 09 | 05 | ||
| Knowledge about skin-to-skin contact | ||||
| Present | 79 | 08 | 64.504 | 0.0001 |
| Absent | 23 | 54 | ||
| Privacy as issue for skin-to-skin contacta | ||||
| Present | 01 | 04 | 2.273 | 0.1316 |
| Absent | 101 | 58 | ||
| Ambient temperature of the labour room | ||||
| Comfortable | 11 | 11 | 1.607 | 0.2049 |
| Uncomfortable | 91 | 51 | ||
| Surrounding (Bed area,lightingandcleanliness) | ||||
| Issue | 04 | 02 | 0.053 | 0.8180 |
| Not an issue | 98 | 60 | ||
| Birth weight ofthebaby | ||||
| <2.5 Kg | 31 | 14 | 2.638 | 0.1043 |
| >2.5 Kg | 71 | 48 | ||
| Number of ANC visitsa | ||||
| <4 | 03 | 02 | 0.005 | 0.9462 |
| >4 | 99 | 62 | ||
| Age ofthemother | ||||
| <21 years | 14 | 13 | 1.470 | 0.225 |
| >21 years | 88 | 49 | ||
| Gender of the newborn | ||||
| Female | 46 | 30 | 1.910 | 0.385 |
| Male | 56 | 31 | ||
| Parity of the mother | ||||
| Primipara | 35 | 25 | 0.600 | 0.439 |
| Multipara | 67 | 37 | ||
| Time of Delivery | ||||
| 0000–0800 h | 25 | 21 | 1.674 | 0.1957 |
| 0801hrs-2359 h | 77 | 41 | ||
Chi-square test with the Yates correction was applied.
Fig. 1.
Fishbone analysis of poor adherence of skin-to-skin contact (SSC) at birth.
Discussion
As a standard hospital practice, newborn babies are often taken to radiant warmer soon after birth or may be wrapped or dressed in their mother's arms, or even placed in open cribs, whereas SSC soon after birth results in so many physiological, social and psychological benefits to both the mother and her newborn.12 In spite of guidelines by the WHO10 and the Government of India,11 implementation of SSC is far from optimal. The overall adherence of some SSC (any time duration, not necessarily for full 1 h) was about 62.2% in our study. In sub-Saharan Africa, the rates of SSC is as dismal as 2%–13%,13 whereas the rates of SSC in developed countries such as the United States range between 49% and 83%.14 Thus, we miss a great opportunity to help babies in the first golden hour of their lives in maintenance of temperature, first breast feeding,7 minimising problems faced by the mothers in breast feeding15 and development of a sacred emotional bond between the mother and the baby.16
A recent study from Bangalore, India, revealed that the barriers in implementation of SSC were primarily lack of awareness, skewed health-care staff-to-client ratio in the labour room leading to lack of personnel and time constraints, apprehensions of safety of the newborn, interference with other clinical procedures, and gender preferences.9 In our study, the lack of awareness was found to be the most important factor in not implementing SSC, followed by pain of episiotomy and its suturing. There was no statistically significant difference between the time of delivery, whether at day or night, on the adherence to SSC. The additional barriers in our study were knowledge gap in staff of need of reinforcement for SSC at birth and staff preference of keeping neonates under radiant warmers (Fig. 1). The study from countries such as Japan and Australia report non-existent policy of SSC at birth, staff preference of not doing SSC and institutional protocol of examination of neonate under radiant warmer to be the barriers in implementing SSC,12 whereas in Africa, transmission of potential maternal disease, maternal pain, maternal inability to take rest and potential of hurting the baby were the main barriers for doing SSC.13 On the other hand, in the study by Alenchery et al., mothers perceived less pain while doing SSC, when the episiotomy suturing was going on. In the same study, the possible solutions suggested by the mothers were dedicated bystanders to support the baby while doing SSC (a relative or a dedicated health-care staff), antenatal awareness and training of health-care staff and repeated reinforcements.9 Evidence also exists supporting SSC even after caesarean births, leading to temperature stability in the operating room.17
General belief in health-care staff is that the SSC is akin to Kangaroo Mother Care (KMC),18 and unlike low birth weight neonates, the normal neonates need not undergo SSC. There should be continuous endeavour to educate all health-care staff working in delivery rooms, across all the facilities, that SSC is a mandatory part of essential neonatal care for all babies not needing immediate resuscitation at birth. With increasing awareness, it is possible to have a near universal acceptance as we see today in care of low birth weight neonates using KMC.
The strength of our study is that the study participants were observed prospectively and their perceptions regarding SSC were recorded diligently. The weaknesses of the study are that we did not explore those babies born through caesarean sections and multiple pregnancies. In addition, the study results may not be generalizable in settings where there is an additional skewed health-care staff-to-client ratio.
Conclusion
To conclude, the rate of SSC after vaginal delivery was suboptimal in the labour room of our tertiary care teaching hospital, and the commonest reason was lack of awareness about this vital step of newborn care. The duration of SSC in those who attempted was far less than the recommendations. SSC should be universally practiced and for full 1 h for all neonates, with an attempt to include even caesarean-born neonates. There is an urgent need of sensitization of all health-care providers and mothers about the need of undergoing this very important step of early essential newborn care. This would not only keep the baby warm at zero cost, it would also ensure early breast feeds of the newborn, eventually improving breastfeeding exclusivity.
Conflicts of interest
All authors have none to declare.
Acknowledgement
Maharashtra University of Health Sciences {Study was conducted as STRG, MUHS project (MUHS/URD/649/2018)}.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mjafi.2018.11.008.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Sankar M.J., Neogi S.B., Sharma J. State of newborn health in India. J Perinatol. 2016;36:S3–S8. doi: 10.1038/jp.2016.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garg R., Deepti S.S., Singh T., Padda A.S. Characteristics and utilization of ante natal care services amongst women of rural Punjab, India-a community based study. Int J Med Pub Health. 2017 Feb 22;4(3):752–758. [Google Scholar]
- 3.Varma D.S., Khan M.E., Hazra A. Increasing postnatal care of mothers and newborns including follow-up cord care and thermal care in rural Uttar Pradesh. J Fam Welfare. 2010;56:31–42. [Google Scholar]
- 4.Sarin J., Jeeva S., Geetanjli P.S. Practices of Auxiliary Nurse Midwives regarding care of baby at birth. Nursing and Midwifery Research. 2011;7(3):110–119. [Google Scholar]
- 5.Sinha L.N., Kaur P., Gupta R., Dalpath S., Goyal V., Murhekar M. Newborn care practices and home-based postnatal newborn care programme–Mewat, Haryana, India, 2013. J WPSAR. 2014 Jul;5(3):22. doi: 10.5365/WPSAR.2014.5.1.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore E.R., Bergman N., Anderson G.C., Medley N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2016;11 doi: 10.1002/14651858.CD003519.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marin G.M.A., Martin L.I., Escobar L.A., Villalba F.E., Blanco R.I., Pol T.P. Randomized controlled trial of early skin-to-skin contact: effects on the mother and her newborn. ActaPediatr. 2010;99(11):1630–1634. doi: 10.1111/j.1651-2227.2009.01597.x. [DOI] [PubMed] [Google Scholar]
- 8.Wagner D.L., Lawrence S., Xu J., Melsom J. Retrospective chart review of skin-to-skin contact in the operating room and administration of analgesic and anxiolytic medication to women after cesarean birth. Nursing for Women's Health. 2018;22(2):116–125. doi: 10.1016/j.nwh.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 9.Alenchery A.J., Thoppil J., Britto C.D., de Onis J.V., Fernandez L., Suman Rao P.N. Barriers and enablers to skin-to-skin contact at birth in healthy neonates - a qualitative study. BMC Pediatr. 2018;18:48. doi: 10.1186/s12887-018-1033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for Essential Practice. 3rd ed. World Health Organization; Geneva: 2015. https://www.ncbi.nlm.nih.gov/books/NBK326678 Available from: [PubMed] [Google Scholar]
- 11.Facility Based Newborn Care Operational Guide: Guidelines for Planning and Implementation. Ministry of Health & Family Welfare, Government of India; 2011. [Google Scholar]
- 12.Brimdyr K., Cadwell K., Stevens J., Takahashi Y. An implementation algorithm to improve skin-to-skin practice in the first hour after birth. Matern Child Nutr. 2018;14:e12571. doi: 10.1111/mcn.12571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bee M., Shiroor A., Hill Z. Neonatal care practices in sub-Saharan Africa: a systematic review of quantitative and qualitative data. J Health Popul Nutr. 2018;37:9. doi: 10.1186/s41043-018-0141-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boundy E.O., Perrine C.G., Barrera C.M., Li R., Hamner H.C. Trends in maternity care practice skin-to-skin contact indicators: United States, 2007-2015. Breastfeed Med. 2018;13(5):381–387. doi: 10.1089/bfm.2018.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nimbalkar A.S., Patel D.V., Nimbalkar S.M., Patel V.K., Patel D.N., Phatak A.G. Infant and young child feeding practices in infants receiving skin to skin care at birth: follow up of randomized cohort. J Clin Diagn Res. 2016;10(2):SC09–SC12. doi: 10.7860/JCDR/2016/22930.9003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duhn L. The importance of touch in the development of attachment. Adv Neonatal Care. 2010;10(6):294–300. doi: 10.1097/ANC.0b013e3181fd2263. [DOI] [PubMed] [Google Scholar]
- 17.Billner-Garcia R., Spiker A., Goyal D. Skin to skin contact: newborn temperature stability in the operating room. MCN Am J Matern Child Nurs. 2018 May/Jun;43(3):158–163. doi: 10.1097/NMC.0000000000000430. [DOI] [PubMed] [Google Scholar]
- 18.Parmar V.R., Kumar A., Kaur R. Experience with kangaroo mother care in a neonatal intensive care unit (NICU) in Chandigarh, India. Indian J Pediatr. 2009;76:25–28. doi: 10.1007/s12098-009-0024-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.