Abstract
Background
Warts or verrucae are benign proliferations of the skin and mucosa resulting from infection with papilloma viruses. Warts form a small subset of patients attending skin out-patient department (OPD), out of which the plantar warts are one of the common presentation. The present study is an attempt to compare two modalities of treatment that is electrosurgery and cryotherapy in patients with plantar warts. There are no studies available where comparison of complications between two modalities has been done in plantar warts thus making it one of unique studies of its kind.
Methods
A prospective, comparative study was conducted over a period of 6 years. After exclusion criteria, one hundred forty-seven male patients having plantar warts were included in the study. Selection of patients suffering from warts subjected to treatment was done by simple random selection. After treatment, 39 patients were lost to follow-up, and finally 48 patients treated by electrosurgery and 60 by cryotherapy were compared and analysed statistically for response to treatment and incidence of complications.
Results
The overall clearance rate was 75% in electrosurgery versus 73.3% in cryotherapy patients. The pain, delayed wound healing and scarring were observed significantly in more patients treated with electrosurgery than cryotherapy. In our study, recurrence at 24 weeks was observed in 21.9% of the electrosurgery patients which was slightly higher than cryotherapy, where it was 16.6%.
Conclusion
This study highlighted that cryotherapy is quick, safe and comparatively painless procedure with less complications with success almost similar to electrosurgery making it more suitable for plantar warts.
Keywords: Human papilloma virus, Plantar warts, Electrosurgery, Cryotherapy, Nitrogen spray technique
Introduction
Warts are benign growths of the skin and mucous membranes caused by infection with the human papillomavirus (HPV). To date, more than 100 HPV types have been identified.1 Plantar warts are more common in adolescents and young adults, perhaps as a consequence of inadequate maturity of the immune system, repetitive microtrauma to the foot occurring in sports, use of public showers2 and excessive perspiration. Plantar warts can be painful especially if they are on pressure areas of the sole. Pain in lateral compression may assist in diagnosis, but patient may report pain by direct pressure due to ambulation.3 Patients seek treatment of the plantar warts because of embarrassment or pain.4 Warts in general and the plantar type in particular pose a therapeutic challenge for the dermatologists. A broad range of therapeutic options exists for treating warts including cytodestructive methods, antimetabolic therapy, antiviral therapy, chemotherapeutic compounds, topical acid and immunomodulators. Recurrence rates for most therapies are relatively high because clinically unaffected tissue surrounding warts often still harbours HPV.5 Choice of treatment depends upon the patient's age, duration, location and extent of lesions, motivation for therapy, pain associated with destructive procedures, potential for scarring, cost and physician experience.6 The most commonly employed treatments include destroying the affected tissue by cytodestructive methods including electrosurgery (electrodesiccation or electrofulguration), cryotherapy, topical acids (salicylic acid and lactic acid) and podophyllotoxin. In electrodesiccation, an active electrode touches or is inserted into the skin to produce tissue destruction.7 Large warts on the torso and plantar warts8 may respond to a single treatment with electrodessication or coagulation.
In cryotherapy, electron microscopy studies have showed that with a second freeze–thaw cycle, the degree of cellular damage increases.9 For this reason, at least two cycles (freeze-thaw, freeze-thaw) generally are recommended as done in our study. The duration of therapy varies and depends on the size and location of the wart; small warts on the face may be frozen for 5–20 s, whereas plantar warts may require an entire minute of freezing.8 Plantar warts usually respond to cryotherapy, making it an excellent second line of treatment when topical agents have failed.10 We undertook this study to compare two modalities, either electrosurgery or cryotherapy, by comparing complications and efficacy of treatment. Though these two methods of treatment are common individually, but there are very few studies where response to treatment has been compared between the two procedures. Also, there are no published studies where safety of treatment has been studied by comparing complications between the two so far, thus making this study one of its kind where complications are compared and analysed statistically in plantar warts.
Material and methods
A prospective, randomised and comparative study was carried out in male patients attending the skin OPD from Jan 2011 to Dec 2016 after taking clearance from institute ethical committee. After detailed history and examination, 180 cases were clinically diagnosed as plantar warts (Fig. 1).
Fig. 1.
Multiple plantar warts on right foot of patient.
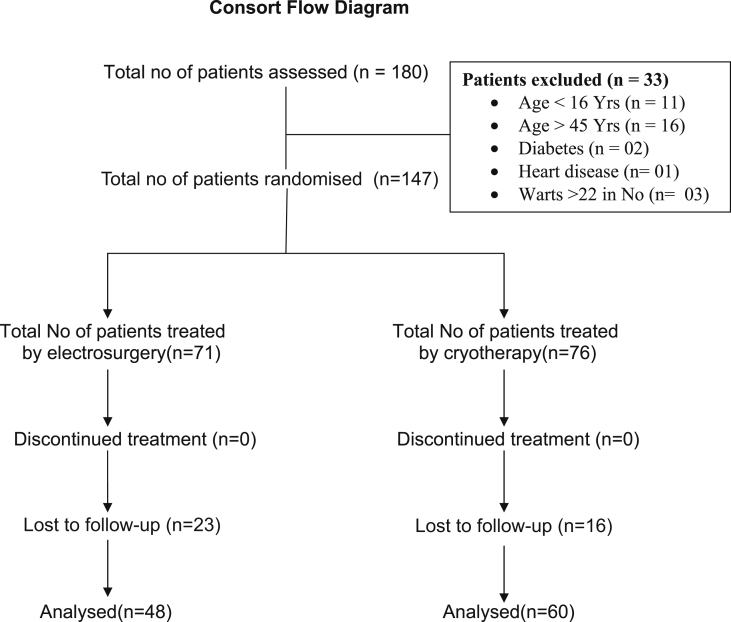
Fig. 1 were assessed for the study. Patients with history of cold or cholinergic urticaria, heart disease, diabetes, collagen vascular disease and tendency for hypertrophic scar or keloids were excluded. Out of total 180 patients, 33 were excluded from the study as shown in consort flow diagram (Fig. 6). Patients with warts less than 22 in number with age between 16 and 45 years were included in the study.
Fig. 6.
Consort statement for study.
For the purpose of this study, the patients were recruited and allocated to the two modalities of treatment by basic method of simple randomisation after flipping a coin by the patient (i.e., heads—electrosurgery, tails—cryotherapy). Before randomisation, both procedures were explained to the patients. A total of 147 patients were treated, out of which 71 were treated by electrosurgery using monopolar electrosurgical unit by electrodessication method and 76 by cryotherapy with hand-held liquid nitrogen spray equipment using liquid nitrogen cryogen, and the outcome was assessed by another dermatologist in the centre, and the results were analysed. Out of which, 23 in electrosurgery group and 16 in cryotherapy group were lost to follow-up, and the remaining 48 and 60 in electrosurgery and cryotherapy group, respectively, were followed successfully for analysis. Before treatment, the procedure was explained, and the written informed consent of the patients was taken.
Electrosurgery procedure was done after infiltration anaesthesia with lignocaine and adrenaline. The end-point was where the lesion shriveled up and lightened in colour with the formation of superficial ash. The gelatinous charred tissue was removed with gauze piece or curette (Fig. 2), and the base was desiccated. Cryotherapy was administered with the ‘Cryogun’ hand-held spray equipment by spot freeze method. The hand-held spray equipment was filled with liquid nitrogen until filled two inches below the brim. After waiting for 3–4 min and selecting the spray tip, the periphery of the wart was marked including 1–2 mm of normal tissue (Fig. 3). The plantar warts were scraped with the scalpel blade before the treatment. The spray tip was held 1 cm away from the lesion, and steady spray of liquid nitrogen was directed towards the centre of the lesion. Three freeze thaw cycles, each having 10 s freezing time and 20 s thaw time, were employed, and the procedure was repeated after 2 weeks.
Fig. 2.
Photograph showing patient treated by electrosurgery.
Fig. 3.
Photograph showing marking of wart before cryotherapy.
Posttreatment follow-up was done, and the therapeutic results were clinically assessed for clearance (success of treatment), complications and recurrences. The treatment response was evaluated as successful treatment (S): clinically no visible lesion at 6 weeks after procedure (Fig. 4, Fig. 5), recurrence (R): clinically visible lesion at 24 weeks after procedure in patients with successful treatment (no visible lesion at 6 weeks). The benchmark time for comparison of complications was 4 weeks for pain, wound infection and delayed wound healing, where as it was 12 weeks for postinflammatory dyspigmentation (hypo/hyper) and scarring. Analytical comparison of the two modalities of treatment was done by p value using Fisher exact test method.
Fig. 4.
Photograph showing successful treatment in the same patient as Fig. 2.
Fig. 5.
Photograph showing successful treatment in the same patient as Fig. 3.
Results
Over the period of 6 years (2011–2016), 147 male patients aged 16–45 years were recruited for the study after excluding the patients by exclusion criteria, out of which 39 were lost to follow-up, and 108 were able to complete the study The average age, duration, size and number of warts treated with cryosurgery and cryotherapy is given in Table 1.
Table 1.
Baseline characteristics of patients included in the study.
| Characteristics | Electrosurgery average (range) | Cryotherapy average (range) |
|---|---|---|
| Age of patients (years) | 25.2 (16–45) | 25.7 (16–44) |
| Duration of warts (weeks) | 29.3 (6–62) | 27.4 (6–58) |
| No of warts | 04 (1–21) | 04 (1–19) |
| Size of warts (mm2) | 7.6 (2–21) | 7.7 (2–23) |
| Total no of patients treated | 48 | 60 |
The pain, wound infection delayed wound healing and postinflammatory dyspigmentation (hypo/hyper) noticed in patients treated with electrosurgery and cryotherapy is given in Table 3. In electrosurgery, incidence of scarring was observed 33.3% of the patients as compared with cryotherapy where it was in 6.7%. The recurrence was observed in 21.9% and 16.6% of patients treated with electrosurgery and cryosurgery, respectively.
Table 3.
Comparison of complications between two modalities of treatments in plantar warts.
| Complication | Electrosurgery (n = 48) | Cryotherapy (n = 60) | p value |
|---|---|---|---|
| Pain | 13 | 4 | 0.003 |
| Wound infection | 3 | 0 | 0.195 |
| Delayed wound healing | 4 | 0 | 0.036 |
| Postinflammatory dyspigmentation (hypo/hyper) | 4 | 9 | 0.378 |
| Scarring | 16 | 4 | 0.0008 |
| Recurrence | 11 | 10 | 0.468 |
Discussion
Treatment of plantar warts is often challenging, and various therapeutic modalities that have been used for treating it have not been successful every time.11, 12, 13, 14
One hundred eight male patients with plantar warts who were treated with either of the two modalities were analysed for the study. Analysis included 48 patients with electrosurgery and 60 with cryotherapy. The two groups of patients were comparable in their age, size, duration and number of warts.
In electrosurgery and in cryotherapy, 75% and 73.3% of the patients cleared of warts at 6 weeks (Table 2). Since no previous study has compared success rate between the two in plantar warts, this cannot be compared. Also, there is no study where efficacy of electrosurgery treatment has been carried out, however there are few studies about cryotherapy treatment response in plantar warts. Cryotherapy cure rate ranges from 39% to 92% depending upon the technique with more aggressive therapy yielding better results.4 In the previous study conducted by Buckley15 reported clearance rate of 83.5% with single cryosurgery by liquid nitrogen spray technique after debulking with surgical blade which is slightly lower in our study. Focht et al16 noticed 60% success in 25 patients of common warts treated with cryotherapy in age group of 3–22 yrs. Limmer et al,17 in a study of 29 patients found that combination of cryotherapy along with daily application of salicylic acid resulted in success in 86.2% of patients. In our study, statistical analysis depicted that there was no significant difference between two modalities of treatment with p = 0.827 (>0.05).
Table 2.
Response of treatment in plantar warts.
| Electrosurgery (n = 48) |
Cryotherapy (n = 60) |
p value | ||
|---|---|---|---|---|
| Successful Treatment (S) | Percentage | Successful treatment (S) | Percentage | |
| 36 | 75% | 43 | 73.3% | 0.827 |
In electrosurgery and in cryotherapy, 27.1% patients and 13.3% patients, respectively, had pain. Statistical analysis in our study has noticed that there was significant difference between the two modalities of treatment with p = 0.003 (<0.05%), and the pain was significantly higher in case of electrosurgery compared with cryotherapy. Wound infection and delayed wound healing were observed in 6.2% and 8.3%, respectively, in patients treated by electrosurgery; whereas, none of the patients had wound infection or delayed wound healing in patients treated by cryotherapy. Statistical analysis showed that there was no significant difference between the two in wound infection with p = 0.195 (>0.05%), but significant difference was observed between the two in delayed wound healing with p = 0.036 (<0.05%). The incidence of postinflammatory dyspigmentation (hypo/hyperpigmentation) were observed in 8.3% treated with electrosurgery compared with 15% of patients treated with cryotherapy. This is attributed to melanocytes being more sensitive to cold than keratinocytes; temporary hypopigmentation is to be expected in areas treated with cryosurgery though repigmentation occurs in most instances. In this study, hypopigmentation or dyspigmentation was found in almost all lesions during treatment with cryosurgery, but after follow-up, most of the lesions noticed to have normal or hyperpigmentation. Statistical analysis indicated that there was no significant difference between the two modalities of treatment; however, the postinflammatory dyspigmentation was slightly higher in lesions treated with cryotherapy. In electrosurgery, 33.3% of the patients noted to have scarring as compared with 6.7% of the patients in cryotherapy, which was statistically significant with p = 0.0008 (<0.05%). Since no previous studies have been carried out to compare pain, wound, infection, delayed wound healing, postinflammatory dyspigmentation and scarring between electrosurgery and cryosurgery, this study cannot be compared. The recurrence at 24 weeks in electrosurgery patients was 21.9%, whereas in cryotherapy, it was 16.6%. The statistical analysis found that there was no significant difference between two modalities with p = 0.468 (>0.05); however, the recurrence was slightly higher in case of electrosurgery compared with cryotherapy.
Conclusion
The present study was an attempt to assess the efficacy of electrosurgery and cryotherapy in treating plantar warts. It was found out that the success rate of treatment of cryotherapy is comparable to electrosurgery. Pain during infiltrating local anaesthetic occured in all patients with electrosurgery; whereas, in cryotherapy, some patients during procedure experienced temporary pain or discomfort like stinging/burning sensation. The pain, wound infection and delayed wound healing at 4 weeks were significantly higher with electrosurgery compared with cryotherapy. The incidence of pain was very high with electrosurgery, thus making the procedure unsuitable for warts over the plantar aspect. Delayed wound healing in lesions was higher with electrosurgery than cryotherapy because of open wounds, and it occurred in lesions, which got infected. In our study, scarring incidence was significantly higher, and the recurrence was slightly more for electrosurgery than cryotherapy.
This study highlights that cryotherapy is safe, comparatively painless procedure with less delayed wound healing and scarring with success and relapse rate comparable with electrosurgery, making it more acceptable and suitable for plantar warts.
Conflicts of interest
All authors have none to declare.
References
- 1.Gharizadeh B., Kalantari M., Garcia C.A. Typing of human papillomavirus by pyrosequencing. Lab Invest. 2001;81:673. doi: 10.1038/labinvest.3780276. [DOI] [PubMed] [Google Scholar]
- 2.Johnson L.W. Communal showers and the risk of plantar warts. J Fam Pract. 1995;40:136–138. [PubMed] [Google Scholar]
- 3.Tracey C., Vlahovic, M Tariq Khan. The Human Papillomavirus and its role in plantar warts. A comprehensive review of diagnosis and management. Clin Podiatr Med Surg. 2016;39:337–353. doi: 10.1016/j.cpm.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Lipke M.M. An armamentarium of wart treatments. Clin Med Res. 2006;4:273–293. doi: 10.3121/cmr.4.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bonnez W., Oakes D., Choi A. Therapeutic efficacy and complications of excisional biopsy of condyloma acuminatum. Sex Transm Dis. 1996;23:273. doi: 10.1097/00007435-199607000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Committee on Guidelines of Care Guidelines of care for warts: human papillomavirus. J Am Acad Dermatol. 1995;32:98–103. doi: 10.1016/0190-9622(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 7.Goldfarb T Michael, Reid M.D. Human papillomas virus infection. Dermatol Clin. 1991;9:287–297. [Google Scholar]
- 8.Landsman M.J., Mancuso J.E., Abramow S.P. Diagnosis, pathophysiology, and treatment of plantar verruca. Clin Podiatr Med Surg. 1996;13:55–71. [PubMed] [Google Scholar]
- 9.Kuflick E.G. Cryosurgery updates. J Am Acad Dermatol. 1994;31:925–944. doi: 10.1016/s0190-9622(94)70261-6. [DOI] [PubMed] [Google Scholar]
- 10.Benton E.C. Therapy of cutaneous warts. Clin Dermatol. 1997;15:449–455. doi: 10.1016/s0738-081x(96)00153-8. [DOI] [PubMed] [Google Scholar]
- 11.Gibbs S., Harvey I., Sterling J., Stark R. Local treatdments for cutaneous warts: systematic review. BMJ. 2002;325:461. [PMC free article] [PubMed] [Google Scholar]
- 12.Bacelieri R., Johnson S.M. Cutaneous warts: an evidence-based approach to therapy. Am Fam Physician. 2005;72:647–652. [PubMed] [Google Scholar]
- 13.Sterling J.C., Handfield Jones S., Hudson P.M. Guidelines for the management of cutaneous warts. Br J Dermatol. 2001;144:4–11. doi: 10.1046/j.1365-2133.2001.04066.x. [DOI] [PubMed] [Google Scholar]
- 14.Kwok C.S., Gibbs S., Bennett C., Holland R., Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;9:CD001781. doi: 10.1002/14651858.CD001781.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buckley D. Cryosurgery treatments of plantar warts. Med J. 2000;93:140–143. [PubMed] [Google Scholar]
- 16.Focht D.R., 3rd, Spicer C., Fairchok M.P. The efficacy of duct tape vs cryotherapy in the treatment of verruca vulgaris (the common wart) Arch Pediatr Adolesc Med. 2002;156:971–974. doi: 10.1001/archpedi.156.10.971. [DOI] [PubMed] [Google Scholar]
- 17.Limmer B.L., Bogy L.T. Cryosurgery of plantar warts. J Am Podiatry Assoc. 1979;69:713–716. doi: 10.7547/87507315-69-12-713. [DOI] [PubMed] [Google Scholar]