Introduction
Respiratory failure during pregnancy can be multifactorial in etiology.1, 2 Although early mechanical ventilation is recommended in these patients,3 there is a strong case for the use of non-invasive ventilation (NIV) in a carefully selected subset of pregnant women with respiratory failure.4, 5 We report a case of a pregnant female patient who presented with acute respiratory failure due to pulmonary tuberculosis. This patient delivered on NIV, and to our knowledge, this is the first case with a history of lower segment caesarean section (LSCS), for whom a successful delivery has been conducted on NIV.
Case report
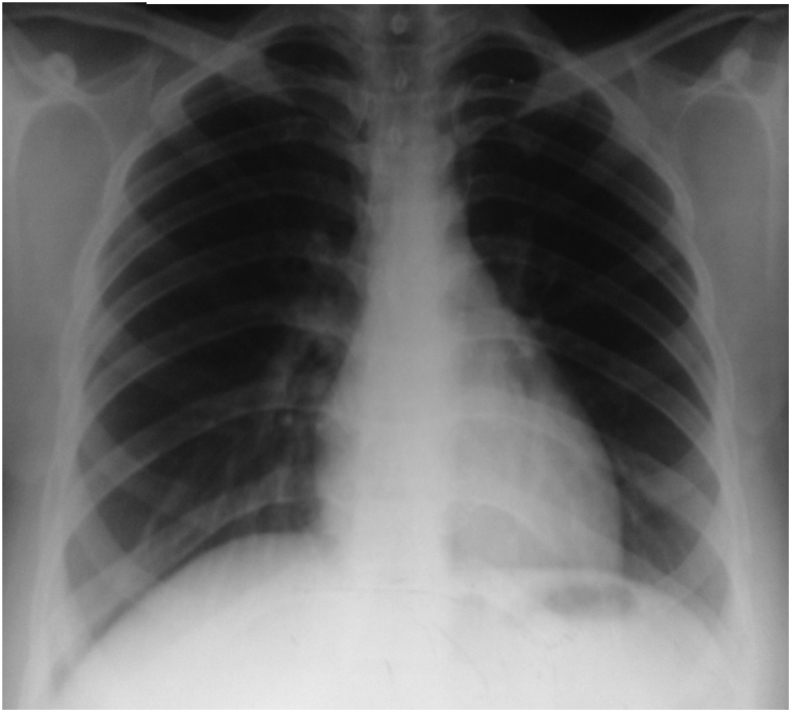
A 33-year-old female patient, G2P1A0L1, presented to our center at 29 weeks 4-day gestation period with symptoms of premature labor. She had undergone LSCS during her first pregnancy at 32 weeks. She was a booked case, and all her antenatal investigations were within normal limits. In view of preterm labor, she was given betamethasone for surfactant induction and isoxsuprine infusion for tocolysis. After 48 h of admission, she had an episode of high-grade fever with chills, and she also complained of dry cough. She was managed with antipyretics. Over the next 12 h, her general condition deteriorated as she developed progressive breathlessness, intermittent high-grade fever, and persistent cough. On general examination, positive findings included tachycardia (120 beats/min), tachypnea (32 breaths/min), oxygen saturation of 78% in room air, and 88–90% on high flow oxygen and pallor. An examination of the respiratory system revealed bilateral infrascapular crackles. Other systemic examinations were within normal limits with uterus palpable between umbilicus and xiphisternum commensurate with the period of gestation. At this point, the differential diagnosis considered mainly included causes of acute onset breathlessness in a pregnant female patient viz isoxsuprine-induced pulmonary edema, pulmonary thromboembolism, amniotic fluid embolism, and pneumonia. In view of chronic cough with failure to gain weight, possibility of a chronic respiratory infection such as tuberculosis was also considered. Investigations were performed to find out the cause among the listed differentials. Investigations revealed anemia (Hb of 10.4 gm%), normal total leukocyte count (8900/cmm) with raised polymorphs (95%), normal renal and liver function test results, and raised serum procalcitonin (3.0 ng/dl). Her 2D echocardiography revealed normal left ventricular function with no evidence of pulmonary arterial hypertension/right atrial or right ventricular dilatation or any clot in the proximal branches. Her chest radiograph (Fig. 1) revealed bilateral nodular opacities with right paratracheal lymphadenopathy with left mid-zone consolidation. Throat swab for H1N1 and sputum for acid fast bacilli (AFB) were negative. Patient's blood gas analysis revealed hypoxemia with a ratio of partial pressure of oxygen in arterial blood to the fraction of inspired oxygen (PaO2/FiO2) being 180. GeneXpert sputum test was performed which detected mycobacteria without any rifampicin resistance. Her blood, urine, and sputum cultures did not reveal the presence of any organism. She was managed in the intensive care unit with broad-spectrum antibiotics and anti-tuberculous therapy along with NIV, oxygen, and other supportive measures. A possible requirement of mechanical ventilation was explained to her husband, and it was decided to intubate and ventilate the patient in case of any further deterioration. She had a mild improvement in her general condition over the next few days with reduction in breathlessness and improvement in oxygen saturation to > 95% on NIV and oxygen; however, she was still requiring almost continuous NIV. On day 5 of admission, she went into active labor. As the patient was tolerating NIV and maintaining saturation of > 95%, it was decided to give her a trial of labor on NIV with intubation and emergency LSCS if her conditions worsened at any point of time during delivery. Her entire process of labor was carried out on NIV, and she persistently maintained oxygen saturation of more than 95%. She delivered a 1.3-kg male child. The child cried immediately after birth and was shifted to the neonatal intensive care unit. After delivery, the patient showed gradual improvement and was weaned off NIV and oxygen over the next 3 weeks. Her antibiotics were stopped after 2 weeks, and anti tuberculous therapy (ATT) was continued. Both the child and the mother were discharged from the hospital 3 weeks after delivery. Her sputum culture for mycobacteria showed growth of Mycobacterium tuberculosis, which was sensitive to all first-line drugs. Her chest radiograph showed complete resolution of opacities (Fig. 2), and sputum for AFB was negative at 6 months; hence, her ATT was stopped.
Fig. 1.
Chest radiograph (bedside anteroposterior view) showing bilateral military opacities and right paratracheal lymphadenopathy with left mid-zone consolidation.
Fig. 2.
Chest radiograph (posteroanterior view) showing complete resolution of opacities and right paratracheal lymphadenopathy at 6 months.
Discussion
The causes of respiratory failure during pregnancy include asthma, pulmonary infections, pulmonary edema, pulmonary thromboembolism, acute respiratory distress syndrome (ARDS), amniotic fluid embolism, and interstitial lung diseases.1 Pneumonia complications, including respiratory failure, are more commonly seen during pregnancy.1 Also various pregnancy complications such as small for gestational age baby, premature labor, and intrauterine death may be seen in patients with pneumonia during pregnancy.1 Bacterial pneumonia during pregnancy is most commonly caused by Pneumococcus.2 H1N1 influenza virus also causes higher mortality and morbidity during pregnancy.2 Tocolytics such as isoxsuprine can lead to pulmonary edema in one of 400 patients receiving the agents, but fluid overload remains the most common cause.2 Unlike general population, a PaO2 of 70 mm Hg (SpO2 of 95%) is required during pregnancy to ensure adequate fetal oxygenation.2 Vaishnav et al. in their study on critically ill obstetric patients requiring mechanical ventilation found that pulmonary edema, ARDS, and acute lung injury were the most common indications for mechanical ventilation in these patients. In their study, the authors concluded that early mechanical ventilation in patients with imminent cardiovascular collapse reduced mortality.3 However, the authors did not study the patients who require NIV and their outcomes. The use of NIV in pregnant patients with ARDS4 and severe pneumonia5 has been reported in literature earlier. Banga et al. reported the use of NIV in a pregnant woman with acute respiratory distress syndrome due to pneumonia, while Mazlan et al.5 reported the use of NIV in a pregnant woman with severe pneumonia. Masclans et al.6 studied the use of early NIV in hypoxemic respiratory failure due to influenza pneumonia and reported a success rate of 40%. All this literature4, 5, 6 clearly suggests that although standard of care in hypoxemic respiratory failure is mechanical ventilation, NIV can be used judiciously in the intensive care unit by trained personnel under close observation.4, 5, 6 In patients for whom a trial of NIV is given, it is prudent to keep equipment ready for intubation if required. In our patient also, while giving a trial of NIV, we had decided to keep a very low threshold for intubation if her condition deteriorated further. Tuberculosis causing ARDS is rare but well documented.7 In a study of 187 patients of ARDS, tuberculosis was found to be the cause in nine patients.8 Our patient had pulmonary tuberculosis as was evident on chest radiograph, and GeneXpert sputum and mycobacterial cultures were positive. Her symptoms being non-specific and reluctance to carry out a chest radiograph in a pregnant patient resulted in a slight delay in the diagnosis of tuberculosis in her case. Also, the history of chronic cough was revealed by the patient only on direct questioning, and she had never reported the same to her gynecologist during her antenatal visits. As she did not have any contraindications to the use of NIV, such as hemodynamic instability, altered consciousness, or worsening on NIV,5 she was considered a fit candidate for NIV. The use of NIV for various conditions causing respiratory failure during pregnancy is well documented,2 but this is the first case report on the use of NIV during labor to conduct a successful vaginal delivery in a post-LSCS pregnancy. Although useful in a selected group of patients with respiratory failure, NIV is contraindicated in patients with altered sensorium, high risk for aspiration, copious secretions, and anatomical abnormalities of upper airway.5 Aspiration pneumonia has been reported in up to 5% of patients on NIV and requires special consideration, especially while using NIV in a pregnant woman with acute respiratory failure.9
Conclusion
Various conditions can result in acute respiratory failure during pregnancy which can be harmful for both the mother and the child. Careful assessment of the underlying cause of respiratory failure with appropriate specific and supportive therapy can result in successful outcomes. The use of NIV for acute respiratory failure during pregnancy can avoid intubation and mechanical ventilation but requires strict monitoring and frequent reassessment for the need of mechanical ventilation.
Conflicts of interest
The authors have none to declare.
References
- 1.Lapinsky S. Acute respiratory failure in pregnancy. Obstet Med. 2015;8(3):126–132. doi: 10.1177/1753495X15589223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhatia P.K., Biyani G., Mohammed S., Sethi P., Bihani P. Acute respiratory failure and mechanical ventilation in pregnant patient: a narrative review of literature. J Anaesthesiol Clin Pharmacol. 2016;32:431–439. doi: 10.4103/0970-9185.194779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vaishnav B.S., Vaishnav B., Desai N.K., Raithatha S.N., Bose S.N. Critically ill obstetric patients requiring mechanical ventilation in rural western India: a retrospective analysis. Natl Med J India. 2016;29:68–72. [PubMed] [Google Scholar]
- 4.Banga A., Khilnani G.C. Use of non invasive ventilation in a pregnant woman with acute respiratory distress syndrome due to pneumonia. Indian J Chest Dis Allied Sci. 2009;51:115–117. [PubMed] [Google Scholar]
- 5.Mazlan Z.M., Ali S., Abidin Z.H. Non invasive ventilation in a pregnancy with severe pneumonia. Respir Med Case Rep. 2017;21:161–163. doi: 10.1016/j.rmcr.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Masclans J.R., Perez M., Almirall J. Early non invasive ventilation treatment for severe influenza pneumonia. Clin Microbiol Infect. 2013;19(3):249–256. doi: 10.1111/j.1469-0691.2012.03797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andresen M., Tapia P., Mercado M., Bugedo G., Bravo S., Regueira T. Catastrophic respiratory failure from tuberculosis pneumonia: survival after prolonged extracorporeal membrane oxygenation support. Respir MedCase Rep. 2013;10:19–22. doi: 10.1016/j.rmcr.2013.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal R., Gupta D., Aggarwal A.N., Behera D., Jindal S.K. Experience with ARDS caused by tuberculosis in a respiratory intensive care unit. Intensive Care Med. 2005;31:1284–1287. doi: 10.1007/s00134-005-2721-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carron M., Freo U., BaHammam A.S. Complications of non-invasive ventilation techniques: a comprehensive qualitative review of randomized trials. BJA. 2013;110(6):896–914. doi: 10.1093/bja/aet070. [DOI] [PubMed] [Google Scholar]