Abstract
Purpose
Chronic lymphocytic leukemia (CLL) is the most common lymphoproliferative disorder in the western world. The involvement of the central nervous system (CNS) or the optic nerve in CLL, however, is rare. We report a case of a previously untreated patient with CLL whose first manifestation of the disease was a progressive visual loss caused by optic neuropathy.
Observations
Clinical manifestations, optical coherence tomography (OCT), and automated visual fields pointed to the diagnosis of neuropathy. Leukemic involvement of the CNS was confirmed after cells suggestive of CLL were found by cerebrospinal fluid analysis. Optic nerve infiltration is thought to be the cause of this optic neuropathy, and the clinical course and treatment are described herein.
Conclusions
When readily diagnosed, optic nerve infiltration is a rare, yet manageable complication of CLL.
Keywords: Optic neuropathy, Chronic lymphocytic leukemia, Optic nerve infiltration
1. Introduction
Chronic lymphocytic leukemia (CLL) is the most common lymphoproliferative disorder in the western world, with an annual incidence of 3:100 000.1, 2, 3, 4, 5 It is usually an indolent disease, and most patients are diagnosed in the early stages (Binet A, Rai 0/1).4,6 CLL more commonly affects the elderly and is most frequently diagnosed in the 7th and 8th decades of life, with a male predominance (2:1).1,4,5 The median survival is approximately six years, with infections being the most frequent complication of CLL and a common cause of death.5, 6, 7
Clinically, involvement of the central nervous system (CNS) in CLL is rare, with an incidence rate ranging from 0.8 to 2% in antemortem studies.1, 2, 3, 4,7 However, autopsy studies reveal that, even in asymptomatic patients, the incidence of infiltration of the brain, meninges, or spinal cord is high (8–71%).1, 2, 3, 4,7 The most cited CNS manifestations of CLL include cognitive and cerebellar dysfunction and cranial nerve palsies; however, optic nerve involvement remains rare, which may explain why it is seldom considered in the differential diagnosis of visual loss in CLL.1,3,4,8 In leukemias, CNS involvement usually develops in the final stages of the disease.8 In CLL, however, this may not be the case, as Rai stage, duration of CLL, immunologic phenotype, or peripheral white blood cell (WBC) count are not symptomatic of CNS involvement.4
To our knowledge, few cases of optic nerve infiltration in CLL have been described.1, 2, 3, 4,7, 8, 9, 10, 11 Although uncommon, knowledge of diagnostic criteria for this condition is imperative, as permanent blindness can occur if CLL is left undiagnosed and untreated. We report a rare clinical case with good supporting facts of a progressive visual loss caused by optic neuropathy in a previously untreated patient with CLL diagnosed two years ago.
2. Case report
A 48-year-old man presented with a 2-week history of vision loss in the left eye with mild retrobulbar discomfort and dyschromatopsia. The patient had been diagnosed with CLL two years prior (FISH with trisomy 12). Diagnosis was conferred after a thorough investigation following a change in WBC during a routine check-up. The patient did not require treatment for CLL and remained asymptomatic. He had a body mass index of 28.86 kg/m2 and was under chronic treatment for arterial hypertension and dyslipidemia with telmisartan and pitavastatin, respectively.
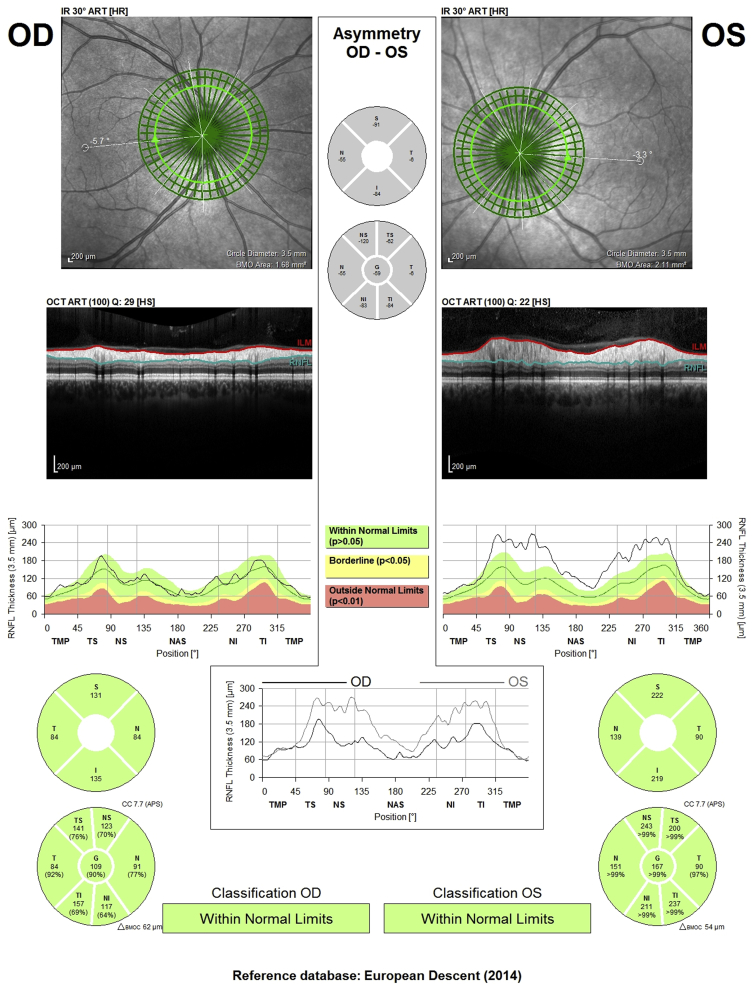
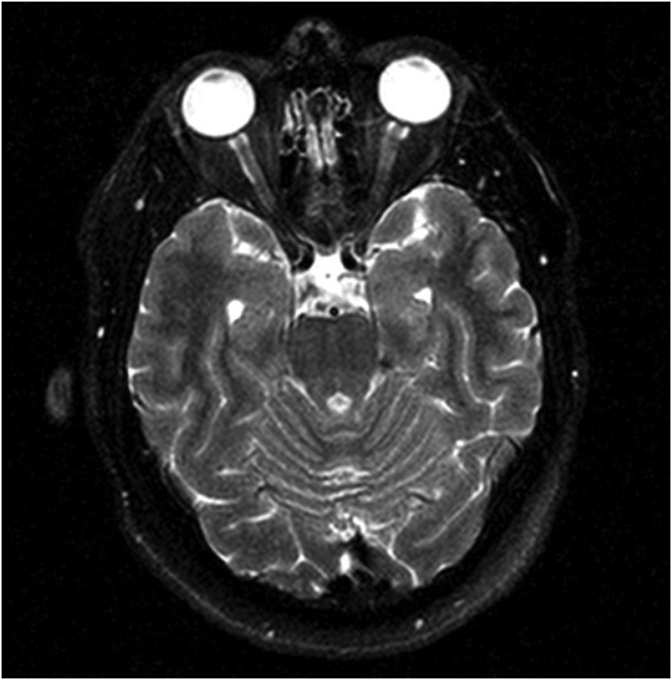
Upon examination, best corrected visual acuity (BCVA) was 10/10 for the right eye (OD) and finger counting at 30 cm for the left eye (OS), with a left relative afferent pupillary defect. Slit lamp biomicroscopy, intraocular pressures, and ocular motility were normal. Fundoscopy was normal in OD, and revealed generalized optic disc edema in OS. Automated visual field testing was normal for OD and showed central/cecocentral scotoma in OS (Fig. 1). Optical coherence tomography (OCT) displayed a normal retinal nerve fiber layer (RNFL) thickness of optic nerve in OD, and was increased in all sectors in OS, compatible with optic disc edema (Fig. 2). Macular OCT was normal in both eyes; after automatic retinal segmentation, the thickness of ganglion cell layers from OD and OS were compared and found to be similar. Brain magnetic resonance imaging showed T2 enlarged thickness of the caliber of the optic nerve in OS (Fig. 3). Initial lumbar puncture revealed an opening pressure of 13 cmH2O. Cerebrospinal fluid (CSF) analysis revealed no evidence of microorganisms, but a pathological monoclonal population of B cells was found. The immunophenotype of this population was CD19+, CD20+, CD5+, CD38−, and CD45+, suggestive of CLL cells present in CSF. These results were confirmed with a second CSF analysis days later.
Fig. 1.
Automated visual fields testing of both eyes (at onset).
Fig. 2.
Optical coherence tomography (OCT): retinal nerve fiber layer (RNFL) map of both eyes (at onset).
Fig. 3.
Brain magnetic resonance imaging at onset.
Complete blood count revealed a hemoglobin of 15.7 g/dL (normal: 13–17 g/dL), 18,000 WBC/mL (normal: 4,500−11,000 WBC/mL) with 67% lymphocytes and platelets count of 179 × 103. Leukocyte morphology was compatible with a chronic lymphoproliferative syndrome. Remaining analytical evaluation was normal, including serology for common infectious and immunologic diseases.
The patient began treatment with high doses of intravenous methylprednisolone (five days, 1,000 mg/day). After three weeks, he had no ocular pain, considerable improvement in dyschromatopsia, and a BCVA of 10/10 and 8/10 in OD and OS, respectively. The ophthalmoscopy of the left eye revealed a slight generalized pallor of the left optic disc. Visual field testing was normal in both eyes. In the OS OCT, there was a reduction of RNFL thickness reaching nearly normal values, indicating a reduction in the swelling of this layer (Fig. 4). Automatic retinal segmentation was repeated, revealing that ganglion cell layer thickness of OS was decreased relative to OD and relative to OS at the onset, possibly indicating atrophy of this layer (Fig. 5). Total macular retina thickness of OS was also decreased relative to OD, and to OS at the onset. Practically all the variability in the total retina thickness of OS was attributable to the change in the ganglion cell layer.
Fig. 4.
Optical coherence tomography (OCT): retinal nerve fiber layer (RNFL) map of both eyes three weeks after onset.
Fig. 5.
Ganglion cell layer thickness analysis of both eyes at onset and three weeks later.
The patient was started on four cycles of intrathecal therapy (IT) with dexamethasone and methotrexate. One month after the last IT cycle (i.e., four months after the onset), no complications from the treatment were found. Automated visual field testing was normal and RNFL OCT was within normal limits. CSF analysis was repeated and cells suggestive of CLLs remained present. At this point, ibrutinib is being considered to be initiated.
The analysis of the mitochondrial DNA sequences of MT-ND1, MT-ND4, and MT-ND6 was also performed. The most common mutations were not found, but in MT-ND1, the m.4216T > C variant was present, which is associated with Leber hereditary optic neuropathy (LHON) phenotype of unclarified pathogenicity.
3. Discussion
Optic neuropathy in patients with CLL is a challenge. There is an extensive differential diagnosis, with more common considerations being inflammatory disorders such as sarcoidosis and opportunistic infections by fungi, parasites, viruses, and bacteria11; these diagnoses were excluded by thorough blood and CSF analyses.
The conclusive diagnosis of CLL nerve infiltration requires a nerve biopsy.11 In most cases, biopsy of the optic nerve is discouraged given its high risk of damage. For this reason, and considering the positive response to the initial methylprednisolone treatment, this diagnostic method was not used.1,11 Although not definitive, CSF analysis by flow cytometry can be helpful for diagnosis by identifying malignant lymphocytes, as was the case with our patient.1,11 Flow cytometry should always be used because it significantly increases the detection rate of malignant cells in the CSF and can differentiate a polyclonal reactive B-cell population from a monoclonal malignant population.7 CSF analysis is also essential to eliminate the possibility of opportunistic infections of the CNS, which can be presented in a similar way.1,3
Optic nerve infiltration by CLL cells that causes optic neuropathy is a rare but devastating condition that can lead to permanent blindness if left undiagnosed and untreated.1,3,11 In this case, optic neuropathy was the first clinical manifestation of a previously asymptomatic CLL. Previous studies suggest that this may indicate a clinical worsening of the CLL.8 CNS symptoms could signal the first manifestation of a more malignant variant arising from a dedifferentiation of the underlying CLL.7
The mechanism by which CNS is infiltrated in CLL remains unknown1,4,7; however, many theories have been hypothesized: leukemia cells may (1) reach the CNS from sporadic intracranial petechial hemorrhages; (2) migrate across perforating vessels into the subarachnoid space; (3) direct extension from seeded meninges into CSF; or (4) spread through perineural sheaths on cranial nerves.1,4,7,12
Although inferred from other types of leukemias, three factors have been associated with CNS involvement in CLL: transformation into a more aggressive variant of CLL (Richter syndrome), thrombocytopenia, and a T-cell variant.3,8,12 Patients with thrombocytopenia may be more likely to have small hemorrhages in the CNS, spreading leukemia cells at this site.12 None of these factors were present in our patient.
When optic nerve infiltration symptomatology includes visual changes, rapid and aggressive treatment is thought to be most effective to prevent more widespread loss of nerve fibers.8 Classically, patients with this diagnosis underwent orbital irradiation with considerable clinical improvement; in more recent years, however, intrathecal methotrexate without irradiation has been used to positive effect.3,8 Ibrutinib, a Bruton tyrosine kinase inhibitor, has also been used with methotrexate with positive results.1 This drug is often considered in patients with CLL who present neurological symptoms.2
CSF analysis post-treatment might be important. Studies show that patients who achieved CSF clearance after treatment were less likely to experience a relapse in their neurologic symptoms, although neurologic resolution can be achieved even in the setting of persistently positive CSF.7
The study of optic neuropathies is always demanding. This case highlights the need to never ignore optic nerve infiltration by CLL, even in patients who were previously asymptomatic and whose conditions were apparently controlled. CSF analysis is an invaluable tool that was crucial in this diagnosis, and it should always be considered when a patient with CLL develops symptoms of optic neuropathy. A timely diagnosis can be extremely important; not only could it spare the patient's vision, but it could also detect an underlying disease with prognostic implications.
Funding
No funding was received for this work.
Intellectual property
We confirm that we have given due consideration to the protection of intellectual property associated with this work and that there are no impediments to publication, including the timing of publication, with respect to intellectual property. In so doing we confirm that we have followed the regulations of our institutions concerning intellectual property.
Research ethics
We further confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies and that such approvals are acknowledged within the manuscript.
IRB approval was obtained (required for studies and series of 3 or more cases).
Written consent to publish potentially identifying information, such as details or the case and photographs, was obtained from the patient(s) or their legal guardian(s).
Declaration of competing interest
No conflict of interest exists.
Contributor Information
Diogo Maleita, Email: dmaleita@hotmail.com, diogo.maleita@chlc.min-saude.pt.
Rita Serras Pereira, Email: ritaserraspereira@gmail.com.
Diogo Hipolito-Fernandes, Email: cdiogo777@gmail.com.
Nuno Moura-Coelho, Email: nunomouracoelho.oft@gmail.com.
João Paulo Cunha, Email: cunha.oft@gmail.com.
Joana Tavares Ferreira, Email: joanaptf@gmail.com.
References
- 1.Khan K., Malik A.I., Almarzouqi S.J. Optic neuropathy due to chronic lymphocytic leukemia proven with optic nerve sheath biopsy. J Neuro Ophthalmol. 2016;36:61–66. doi: 10.1097/WNO.0000000000000300. [DOI] [PubMed] [Google Scholar]
- 2.Wanquet Anne, Birsen Rudy, Bonnet Charlotte. Management of central nervous system involvement in chronic lymphocytic leukaemia: a retrospective cohort of 30 patients. Br J Haematol. 2016;176:37–49. doi: 10.1111/bjh.14387. [DOI] [PubMed] [Google Scholar]
- 3.Mowatt L., Matthews T., Anderson I. Sustained visual recovery after treatment with intrathecal methotrexate in a case of optic neuropathy caused by chronic lymphocytic leukemia. J Neuro Ophthalmol. 2005;25:113–115. doi: 10.1097/01.WNO.0000165104.01237.3F. [DOI] [PubMed] [Google Scholar]
- 4.Cramer S.C., Glaspy J.A., Efird J.T., Louis D.N. Chronic lymphocytic leukemia and the central nervous system: a clinical and pathological study. Neurology. 1996;46:19–25. doi: 10.1212/wnl.46.1.19. [DOI] [PubMed] [Google Scholar]
- 5.Lange C.P.E., Brouwer R.E., Brooimans R., Vecht C.J. Leptomeningeal disease in chronic lymphocytic leukemia. Clin Neurol Neurosurg. 2007;109:896–901. doi: 10.1016/j.clineuro.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 6.Schmidt-Hieber M., Thiel E., Keilholz U. Spinal paraparesis due to leukemic meningitis in early-stage chronic lymphocytic leukemia. Leuk Lymphoma. 2005;46:619–621. doi: 10.1080/14767050400029681. [DOI] [PubMed] [Google Scholar]
- 7.Moazzam A.A., Drappatz J., Kim R.Y., Kesari S. Chronic lymphocytic leukemia with central nervous system involvement: report of two cases with a comprehensive literature review. J Neuro Oncol. 2012;106:185–200. doi: 10.1007/s11060-011-0636-z. [DOI] [PubMed] [Google Scholar]
- 8.Benson E.M., Albert D.M., Currie J.N. Optic neuropathy in chronic lymphocytic leukemia. Arch Ophthalmol. 1988;106:654–660. doi: 10.1001/archopht.1988.01060130708030. [DOI] [PubMed] [Google Scholar]
- 9.Berryman J., Moshiri A., Chang M. BMJ Case Rep bcr-2018-227691. 2018. Chronic lymphocytic leukaemia presenting as branch retinal artery occlusion and optic disc infiltration. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cash J., Fehir K.M., Pollack M.S. Meningeal involvement in early stage chronic lymphocytic leukemia. Cancer. 1987;59:798–800. doi: 10.1002/1097-0142(19870215)59:4<798::AID-CNCR2820590423>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 11.Gonsalves Wilson I., Zent Clive S., Pulido Jose S., MMP Visual loss in early-stage chronic lymphocytic leukemia. J Clin Oncol. 2013;31:280–282. doi: 10.1200/jco.2012.46.7431. [DOI] [PubMed] [Google Scholar]
- 12.West R.J., Graham-Pole J., Hardisty R.M., Pike M.C. Factors in pathogenesis of central-nervous-system leukaemia. Br Med J. 1972;3:311–314. doi: 10.1136/bmj.3.5822.311. [DOI] [PMC free article] [PubMed] [Google Scholar]