Highlights
-
•
Examined opioid prescribing and opioid-overdose death rates in Michigan counties.
-
•
Conducted urban-rural county comparisons and tested for changes across 2013–2017.
-
•
Higher rates of overdose deaths in urban, and higher rates of prescribing in rural.
-
•
Opioid-overdose death rates rose in both urban and rural counties across 2013–2017.
-
•
Opioid prescribing rates did not change in urban or rural counties across 2013–2017.
Keywords: Opioid, Prescribing, Overdose, Death, Urban, Rural
Abstract
Background
Opioid-overdose deaths and opioid prescriptions have increased substantially within the past decade, leading to examinations of urban-rural differences for these opioid-related outcomes, and whether annual trends differ by urban-rural status. Most investigations have examined differences using national data, whereas few studies have identified patterns in hard-hit regions. Therefore, we examined urban-rural differences for opioid-related outcomes in Michigan, a state with overdose death and prescribing rates above the national average.
Methods
This study used county-level public data on opioid prescribing and opioid-overdose death rates in Michigan. Bivariate and joinpoint regression analyses tested for annual differences and annual changes in opioid-related outcomes across 2013–2017. Rural Urban Continuum Codes classified urban-rural county status.
Results
Bivariate analyses demonstrated that urban counties had consistently higher opioid-overdose death rates than rural, whereas rural counties had consistently higher opioid prescribing rates than urban. Joinpoint regression (2013–2017) revealed opioid-overdose death rates increased in urban (Annual Percent Change = 25.0%, p = .001) and rural counties (Annual Percent Change = 21.7%, p = .002), though no changes for opioid prescribing rates were observed among urban or rural counties.
Conclusions
Our study highlights nuanced urban-rural patterns in Michigan, a hard-hit state, compared to trends in national data. Both urban and rural counties experienced rising rates of opioid-overdose deaths, and rural counties experienced higher opioid prescribing rates than urban. Though urban counties experienced higher opioid-overdose death rates than rural, the rise in both county types was similar. Future research directions, implications for public health, and healthcare policy recommendations are discussed.
1. Introduction
The number of opioid-overdose deaths and opioid prescriptions increased substantially within the past decade, leading to an abundance of research examining overdose differences by urban-rural area, as well as the influence of opioid prescribing rates on overdose. One important risk factor might be living in a rural area; both state-level (Keyes, Cerdá, Brady, Havens, & Galea, 2014) and national-level data (García et al., 2019) suggest that greater rates of opioid prescribing have been observed in rural areas. Additionally, a systematic review of the literature examining studies conducted in several different states suggests that rural residents are at a higher risk for opioid-overdose and drug-overdose deaths (King, Fraser, Boikos, Richardson, & Harper, 2014). Furthermore, national data suggests, that since the onset of the opioid epidemic (1999), drug-overdose deaths have risen more steeply in rural areas (Hedegaard et al., 2019, Mack et al., 2017) compared with individuals living in urban areas. There are several potential contributing factors for these trends; rural residents are less likely to be administered naloxone during an overdose1 than urban residents in emergency departments (Frank, Levy, Calcaterra, Hoppe, & Binswanger, 2016), and often have fewer available and accessible medication treatment facilities for opioid use disorder (OUD) than individuals living in urban areas (Dick et al., 2015, Kvamme et al., 2013).
Nonetheless, the relationships described above are complex; and some studies using state and regional data have found results which deviated from general trends. For example, one study in Connecticut found urban-rural differences for prescription and heroin overdose deaths; with heroin-only overdose deaths being more concentrated in urban areas, and prescription opioid-overdose deaths commonly occurring in combination with other substances, and more frequent in small towns than cities (Green, Grau, Carver, Kinzly, & Heimer, 2011). Additionally, some have noted that while many of the states with the highest overdose death rates are rural, there are some rural areas with very low overdose death rates (Okie, 2010, Rossen et al., 2014). Finally, the greater impact of opioid and drug supply in urban environments may increase vulnerability to drug use and opioid-overdose deaths (Galea et al., 2005, Monnat, 2019), potentially explaining some of the variation in general trends.
Additionally, trends in opioid prescribing and overdose rates have markedly changed over time during the past several years. Specifically, some evidence suggests that opioid prescribing has been decreasing as physicians have become increasingly less likely to prescribe prescription opioids for pain (Daubresse et al., 2019, Nobel et al., 2019). Additionally, overdose rates have risen as more potent opioids with a higher risk of overdose (e.g., non-pharmaceutical, illicitly manufactured, fentanyl) have begun flooding the market (Jannetto et al., 2019). Urban-rural differences for opioid-overdose deaths and opioid prescribing may have also shifted as these changes occurred. For example, one Rhode Island study found that fentanyl overdose deaths are significantly less likely to occur in rural areas than urban areas (Marshall et al., 2017).
Given the rapidly changing nature of these trends, as well as some state and local data which differs from general trends, there remains a need for regional research that identifies correlates of opioid-overdose deaths and high-volume opioid prescribing to help more precisely inform state and local policy. In particular, few existing studies have examined urban-rural differences (or other antecedents) for opioid-overdose deaths or opioid prescribing in the Midwest. Therefore, the present study examined urban-rural differences in Michigan, a Midwestern state with high opioid prescribing and overdose death rates (National Institute on Drug Abuse, 2019). We examined urban-rural differences in five separate years (2013, 2014, 2015, 2016, and 2017) for each outcome in bivariate analyses. We then examined the significance for changes over time (2013–2017) for these same outcomes by county types (urban and rural) using joinpoint regression.
2. Material and methods
2.1. Data sources
We extracted 2013–2017 county-level public data on the number of opioid prescriptions dispensed and opioid-overdose death rates from the Michigan Department of Health and Human Services (MDHHS) (Michigan Substance Use Disorder Data Repository, 2018a).
The MDHHS obtains information about opioid prescribing from the Michigan Automated Prescription System (MAPS; Department of Licensing and Regulatory Affairs, 2017). The information in this data source reflects the number of opioid agonist and partial agonist prescriptions dispensed in each county. To calculate the prescribing rate, we divided the number of prescriptions dispensed by the county population. This data source is freely available online2 (Repository, 2018b).
The MDHHS obtains information about opioid-overdose deaths from Michigan Death Certificates within the Division for Vital Records and Health Statistics/MDHHS. This information reflects the number of county residents who died from an overdose in which an opioid (including opium, heroin, natural/synthetic opioids, methadone, and synthetic opioids other than methadone) was identified as a contributing cause. This analysis included overdoses that were accidental, intentional (i.e., suicide, homicide), and those where the intent was unable to be determined. This data source is also freely available online (Michigan Substance Use Disorder Data Repository, 2018c).
The number of residents in each county was retrieved from the Michigan Division for Vital Records and Health Statistics (Division for Vital Records and Health Statistics, 2018). Estimates are made on July 1st of each year based on the Population Estimates released by the National Center for Health Statistics (NCHS).
2.2. Measurement
Urban-rural county classification. Rural Urban Continuum Codes (RUCCs), a widely used (Dick et al., 2015, Kvamme et al., 2013) county-level classification scheme developed by the U.S. Department of Agriculture (USDA, 2019a) to measure rurality by population size and adjacency to urban areas, were used to assess the degree of urbanization of Michigan counties. RUCCs have nine categories, ranging from large urban counties (1) to remote rural counties (9). We defined counties as urban (RUCC = 1–3) and rural (RUCC = 4–9), a dichotomization which has been used in other urban-rural comparisons (e.g., Dasgupta et al., 2014, Jackson and Shannon, 2012, Stein et al., 2017, Wang et al., 2013, Wingrove et al., 2016) and noted by the USDA (2019b) as the most commonly used method to conceptualize urban-rural county classification for the purpose of comparison.
Opioid prescribing and opioid-overdose death rate variables. We assessed county-level opioid prescribing and opioid-overdose death rates as continuous measures for each year of data. Opioid prescribing data reflects the number of opioid agonists and partial agonist prescriptions dispensed in each county, per 100,000 people. Crude opioid-overdose death rates reflect the number of deaths in which an opioid was identified as a contributing cause in each county, per 100,000 people. For joinpoint analyses, we calculated crude rates3 for both opioid-related outcomes among all counties, all urban counties, and all rural counties for each of the five years.
2.3. Data analyses
First, in bivariate relationships, we used Mann-Whitney (U) tests to examine urban-rural differences in county-level opioid-prescribing and opioid-overdose death rates. Non-parametric tests were used to address potential outlier values for both opioid-related outcomes. Next, we conducted joinpoint regression analyses using the Joinpoint Regression Program, Version 4.7.0.0 (U.S. National Cancer Institute, 2019a) to test whether the annual changes in both opioid-related outcomes were statistically significant across 2013–2017. For joinpoint analyses, we compared crude urban and crude rural rates to adjust for the different population sizes within each county type (i.e., to avoid weighting all counties the same despite different population size totals). Annual Percent Change (APC) was calculated using the Joinpoint Regression Program. The default maximum number of joinpoints we used is zero as our models have five time points (U.S. National Cancer Institute, 2019b). Prior studies have also used a five-year timeframe with zero joinpoints (e.g., Scholl, Seth, Kariisa, Wilson, & Baldwin, 2019). The purpose of using joinpoint regression for our models was to examine whether changes over the five years are significant among urban and rural counties. Thus, even though the maximum number of joinpoints is zero as a default, joinpoint regression was appropriate to address our research questions.
3. Theory
The goal of the present study was to capture the nuances of the opioid epidemic by examining how well-established relationships between urban-rural county classification, opioid prescribing, and opioid-overdose deaths may differ within a specific region (Michigan). Furthermore, these data sought to capture the rapidly changing nature of trends by examining how the relationships change over time.
In this respect, our analysis followed the guidelines outlined by the Centers for Disease Control and Prevention’s “Four Domains of Chronic Disease Prevention” (CDC, 2015). The model is commonly used for tobacco use, a substance use disorder referred to as a chronic disease, similar to how the American Society on Addiction Medicine conceptualizes opioid use disorder (ASAM, 2014). We specifically anchored our analyses in Domain 1 (Epidemiology and Surveillance), since we monitored trends and provide information that can be useful to guide policy recommendations. Information like ours can be utilized to improve facilitation of prevention and treatment efforts outlined in Domain 3 (Health Care Systems Intervention), serving to reduce and manage risks for opioid-overdose deaths. While the present study is certainly not the first to examine trends over time in a particular region, we believe this investigation will build upon previous work and lay the foundation for future research to more precisely examine correlates of opioid-overdose death.
4. Results
4.1. Sample characteristics
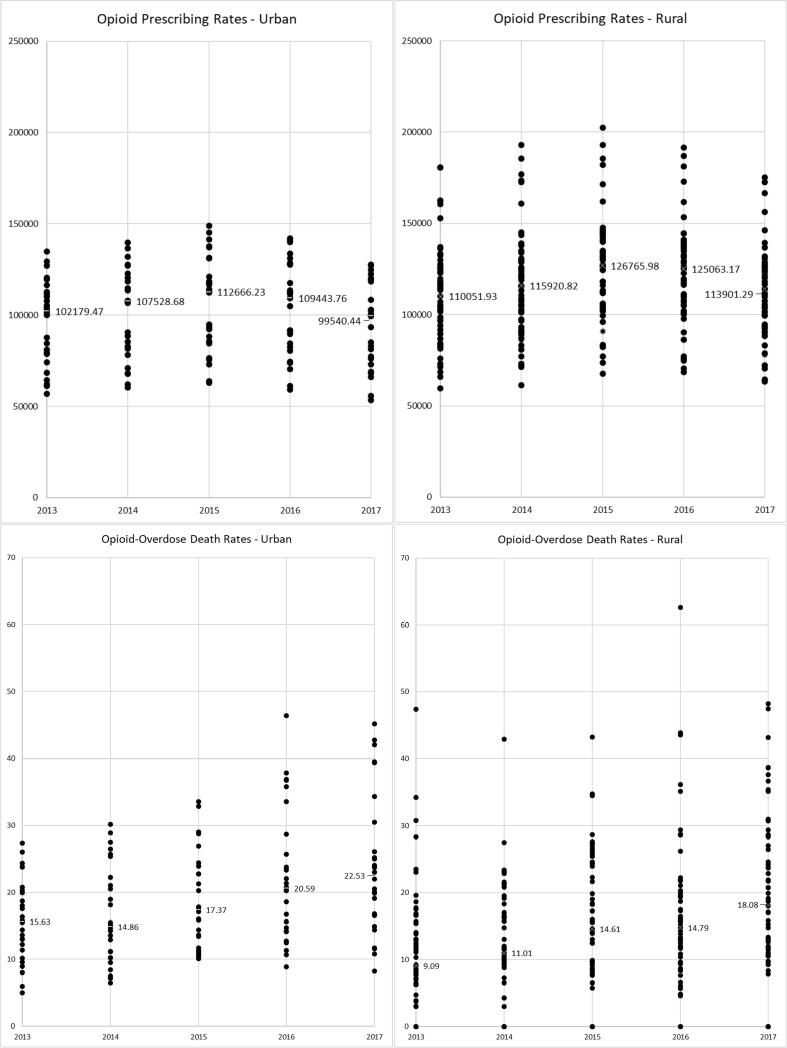
Among all Michigan counties, 31.3% (n = 26) were urban and 68.7% (n = 57) were rural. The overall crude rates for both opioid-related outcomes for all counties, all urban counties, and all rural counties are presented for each of the five years in Table 1. The median opioid-prescribing rates and opioid-overdose death rates for each year, as well as interquartile ranges, are presented in Table 2. To display the dispersion of opioid prescribing rates and opioid-overdose death rates, we also provide a scatterplot that shows the distribution of both opioid-related outcomes for each of the five years (see Fig. 1).
Table 1.
Crude opioid prescribing rates and crude opioid-overdose death rates, Michigan, 2013–2017.
| Year | All counties Crude rate |
All rural counties Crude rate |
All urban counties Crude rate |
|---|---|---|---|
| Opioid prescribing rates | |||
| 2013 | 98,708 | 103,326 | 97,682 |
| 2014 | 102,409 | 109,135 | 100,918 |
| 2015 | 107,689 | 117,062 | 105,616 |
| 2016 | 104,039 | 113,679 | 101,913 |
| 2017 | 95,284 | 104,419 | 93,272 |
| Opioid-overdose death rates | |||
| 2013 | 8.95 | 5.22 | 9.78 |
| 2014 | 10.49 | 7.23 | 11.21 |
| 2015 | 13.27 | 8.63 | 14.29 |
| 2016 | 17.92 | 9.58 | 19.76 |
| 2017 | 20.60 | 12.13 | 22.46 |
Note. Counties defined as urban (RUCC = 1–3) and rural (RUCC = 4–9). Opioid prescribing data reflects the number of opioid agonists and partial agonist prescriptions dispensed, per 100,000 people. Opioid-overdose death rates reflect the number of deaths in which an opioid was identified as a contributing cause, per 100,000 people. Bivariate differences are presented in Table 2 using non-parametric tests to minimize the influence of outlier values (i.e., among counties with small populations and/or a small number of cases for either outcome). We could not make urban-rural comparisons in bivariate analyses using crude urban and crude rural rates with only two points of data for each year.
Table 2.
Median opioid prescribing rates, median opioid-overdose death rates, and differences by urban-rural county classification, Michigan, 2013–2017.
| Year | All counties (N = 83) Median (IQR) |
Rural counties (n = 57) Median (IQR) |
Urban counties (n = 26) Median (IQR) |
Test statistic | p value |
|---|---|---|---|---|---|
| Opioid prescribing rates | |||||
| 2013 | 105,040 (39,151) | 110,052 (37,507) | 102,179 (35,949) | U = 530.0 | .038 |
| 2014 | 113,262 (38,463) | 115,921 (35,581) | 107,529 (40,398) | U = 526.0 | .035 |
| 2015 | 118,348 (35,063) | 126,766 (37,961) | 112,666 (45,600) | U = 503.0 | .019 |
| 2016 | 116,270 (34,606) | 125,063 (34,299) | 109,444 (45,696) | U = 493.0 | .015 |
| 2017 | 105,446 (34,176) | 113,901 (32,640) | 99,540 (43,470) | U = 459.0 | .006 |
| Opioid-overdose death rates | |||||
| 2013 | 5.71 (8.54) | 4.18 (7.38) | 8.64 (8.12) | U = 418.0 | .001 |
| 2014 | 5.91 (11.40) | 4.25 (9.19) | 9.16 (11.21) | U = 411.0 | .001 |
| 2015 | 9.75 (11.88) | 6.14 (13.26) | 12.27 (12.08) | U = 485.0 | .012 |
| 2016 | 10.61 (11.43) | 8.18 (8.56) | 15.48 (13.15) | U = 317.0 | <.001 |
| 2017 | 12.97 (11.62) | 11.37 (13.8) | 17.09 (13.22) | U = 451.0 | .004 |
Note. Counties defined as urban (RUCC = 1–3) and rural (RUCC = 4–9). Interquartile Range (IQR). Mann-Whitey (U) tests conducted to address non-normality. Opioid prescribing data reflects the number of opioid agonists and partial agonist prescriptions dispensed in each county, per 100,000 people. Opioid-overdose death rates reflect the number of deaths in which an opioid was identified as a contributing cause in each county, per 100,000 people.
Note. Preliminary analyses (using Kruskal-Wallis tests) demonstrated similar geographic patterns for both opioid-related outcomes if categorizing counties as urban (RUCC = 1–3, n = 26), rural/micropolitan (RUCC = 4–7, n = 43), and rural/remote (RUCC = 8–9, n = 14). Specifically, lower opioid prescribing rates were consistently observed for urban compared to both rural county categories, whereas higher opioid-overdose deaths rates were consistently observed for urban compared to both rural county categories. The overlap of these findings with comparisons using the dichotomous urban-rural county classification status, alongside the potential for Type II error due to the limited number of rural/remote counties (Jaccard & Becker, 2009), made using the validated urban-rural county classification scheme (USDA, 2019b) the most appropriate approach for these data.
Fig. 1.
Distributions of mean opioid prescribing rates and mean opioid-overdose death rates among all urban and rural counties. Note. Counties defined as urban (RUCC = 1–3) and rural (RUCC = 4–9). Opioid prescribing data reflects the number of opioid agonists and partial agonist prescriptions dispensed in each county, per 100,000 people. Opioid-overdose death rates reflect the number of deaths in which an opioid was identified as a contributing cause in each county, per 100,000 people. Numbers in the graphs indicate medians.
4.2. Bivariate analyses
Urban-rural differences for opioid prescribing rates. Bivariate analyses demonstrated that rural counties (vs. urban) had higher opioid prescribing rates in each of the five years examined. See Table 2 for detailed statistics.
Urban-rural differences for opioid-overdose death rates. Bivariate analyses demonstrated that urban counties (vs. rural) had higher opioid-overdose death rates in each of the five years examined. See Table 2 for detailed statistics.
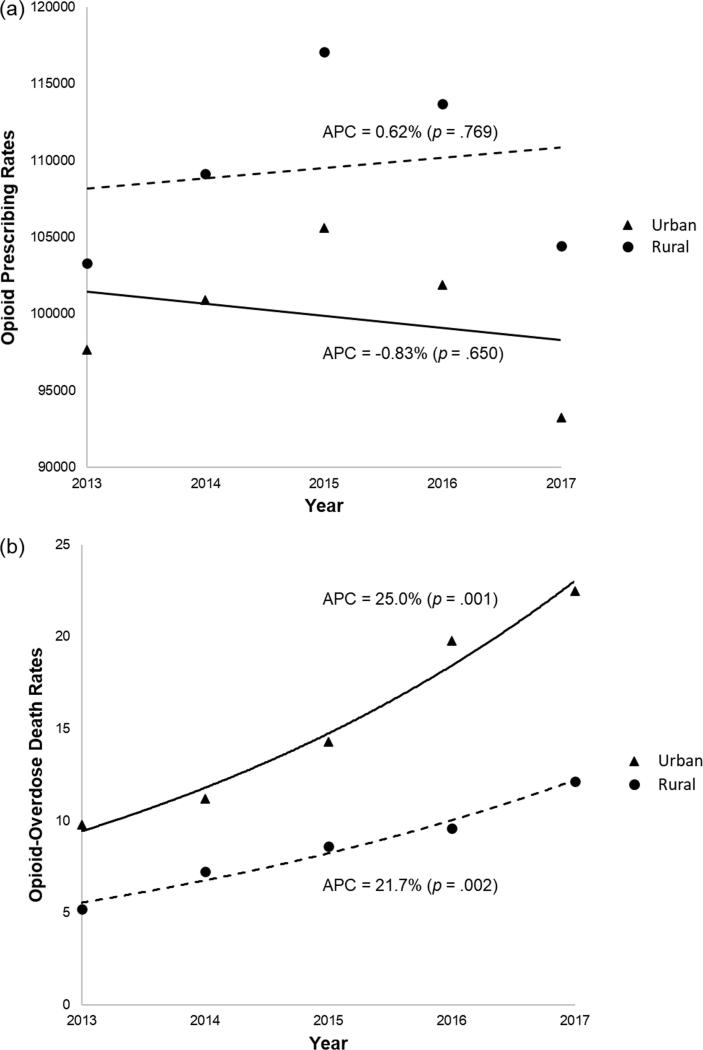
4.3. Joinpoint regression analyses
Joinpoint regression analyses (see Fig. 2) revealed that there were no changes across 2013–2017 for crude opioid prescribing rates among urban (APC = −0.83%, p = .650) or rural (APC = 0.62%, p = .769) counties. By contrast, crude opioid-overdose death rates significantly increased across 2013–2017 in both urban (APC = 25.0%, p = .001) and rural (APC = 21.7%, p = .002) counties. For the opioid prescribing trend, we considered that the Annual Percentage Change (APC) might not be statistically significant because of its inverted V shape. Therefore, we split the five-year model into two separate three year-models (2013–2015 and 2015–2017), and re-ran joinpoint regression for each three-year model. The results showed that the changes for each model (the increase from 2013 to 2015 and the decrease from 2015 to 2017) were not statistically significant, except for the crude rate increase from 2013 to 2015 among rural counties (APC = 6.44%, p = .045). Therefore, we concluded that changes (the whole trend, the split half from 2013 to 2015, and the split half from 2015 to 2017) in the model were generally not significant.
Fig. 2.
Changes over time in crude opioid prescribing rates and crude opioid-overdose death rates by Michigan county type. Note. (a) Opioid prescribing rates and (b) opioid-overdose death rates from 2013 to 2017. Counties defined as urban (RUCC = 1–3) and rural (RUCC = 4–9). APC = Annual Percent Change. Opioid prescribing data reflects the number of opioid agonists and partial agonist prescriptions dispensed in each county, per 100,000 people. Opioid-overdose death rates reflect the number of deaths in which an opioid was identified as a contributing cause in each county, per 100,000 people. The default maximum number of joinpoints is zero.
5. Discussion
Opioid-overdose deaths have continued to increase over the last several years. Generally, drug-overdose deaths have occurred more steeply in rural since the onset of the opioid epidemic (Hedegaard et al., 2019, Mack et al., 2017) and high opioid-prescribing regions (King et al., 2014). However, there have been limited investigations into these trends in the Midwestern U.S., especially in recent years (2013–2017) when urban-rural differences in overdose-death rates have begun to highlight steeper rises in urban areas (Hedegaard et al., 2019). Furthermore, Michigan represents a region with high opioid prescribing and opioid-overdose death rates (NIDA, 2019), but consistently understudied in the opioid-related literature (Lister, Weaver, Ellis, Himle, & Ledgerwood, 2019a). To address this gap, this study examined whether general trends for opioid prescribing and opioid-overdose deaths are consistent with regional trends in a large Midwestern state (Michigan) across a five-year period (2013–2017). These state-level data provide findings that can guide regional implications for health service policy.
Similar to general trends, Michigan counties, independent of urban-rural county classification, experienced an increase in opioid-overdose deaths. The annual percentage change was significant for both urban and rural Michigan counties. Also consistent with general trends (García et al., 2019, Keyes et al., 2014), rural counties were more likely to experience higher opioid prescribing rates in each year examined. We did not observe significant changes in opioid prescribing rates for either urban or rural Michigan counties. Given the persistently high levels of opioid prescribing, both nationally (Guy et al., 2017) and in these data, this finding was not entirely surprising. The consistently greater likelihood for rural counties to have higher opioid prescribing rates aligns with prior research identifying that rural residents are more likely to be provided opioid pharmacotherapy for the treatment of pain compared to their urban counterparts (Prunuske et al., 2014), likely driven by the lack of capacity to provide psychosocial treatments (Dubin et al., 2015). Additionally, because rural residents are more likely to be prescribed opioids but are often underrepresented in human subjects research (Tanner, Kim, Friedman, Foster, & Bergeron, 2015), future work may also want to examine whether particular characteristics (e.g., greater isolation, psychosocial characteristics) are associated with an increased likelihood of opioid misuse in rural populations.
In contrast to data from a few years ago (Mack et al., 2017), but similar to an analysis from 2014 to 2017 (Hedegaard et al., 2019), urban counties experienced higher rates of opioid-overdose deaths. This finding was surprising when viewed in context of the greater supply of opioids prescribed in rural Michigan counties. Furthermore, divergent from recent (2014–2017) trend analyses at the national level (Hedegaard et al., 2019), urban counties in Michigan experienced a slightly flatter rise (albeit non-significant) in opioid-overdose deaths than rural counties. Our findings highlight that state-level findings might have nuanced urban-rural patterns when viewed alongside national data. While these data did not provide insight into the cause of higher opioid-overdose death rates in urban counties, we suspect that the relatively larger urban supply of illicit and potent opioids may overpower the influence of prescription opioid supply in rural counties. Previous studies have demonstrated greater rates of heroin- and fentanyl-related overdose-deaths in urban areas, in contrast to higher rates of prescription opioid-overdose deaths in non-urban areas (Green et al., 2011). Furthermore, recent data in the largest urban county of Michigan demonstrated a spike in synthetic opioid-overdose deaths (King et al., 2019).
Our study findings provide a few directions for future research. First, these data highlight the importance of regional research, where trends may diverge or align with general patterns. As a result, region-specific investigations (Green et al., 2011) that assess urban-rural differences have the potential to provide important public health information, in line with Domain 1 of the CDC’s Four Domains of Chronic Disease Prevention (CDC, 2015) regarding epidemiological and surveillance data for opioid-related outcomes. We suggest future research investigates additional county-level factors (e.g., racial composition, age, income, and healthcare access) that may account for urban-rural variations in opioid prescribing and opioid-overdose deaths. We also recommend future studies investigate opioid-overdose death predictors using stratified analyses within urban and rural counties to extend upon comparative data. These findings can help guide prevention and intervention efforts designed for the specific antecedents determining opioid-related outcomes within each county type.
These data also provide implications that contribute to knowledge development for public health, while simultaneously offering findings that are useful in guiding healthcare policy recommendations, in line with Domain 3 of the CDC’s Four Domains of Chronic Disease Prevention (CDC, 2015). Our findings suggest that policymakers in Michigan and other Midwestern states further expand community access to known mortality buffers, including medication and psychosocial treatment, overdose-reversal medications, and syringe exchange programs (Pitt, Humphreys, & Brandeau, 2018) in both urban and rural communities. Our data suggest that these buffers, while essential for all communities, are even more urgent in urban communities than in prior years. Some possible ways to influence healthcare in urban areas include the use of emergency department-based programs offering naloxone and referrals to medication treatment (D’Onofrio et al., 2015), as well as continuing to monitor factors predictive of treatment dropout among patients already engaged in treatment (Lister, Brown, Greenwald, & Ledgerwood, 2019b). By comparison, screening rural residents for disordered use of prescription opioids at community pharmacies (Cochran, Engel, Hruschak, & Tarter, 2017) may be a particularly promising approach when pharmacies offer naloxone (Bachyrycz, Shrestha, Bleske, Tinker, & Bakhireva, 2017), especially if they facilitate access to addiction treatment (Look, Kile, Morgan, & Roberts, 2019). Independent of urban-rural county classification, we recommend jurisdictions like Michigan consider a variety of policy changes to expand access to evidence-based medication treatments. A few examples include reimbursement for telehealth-delivered treatment among publicly insured populations (Lister, 2017), policies targeting long-term financial sustainability for new buprenorphine-expansion models in hard-hit regions (Winstanley et al., 2019), and greater supports for substance use treatment facilities receiving public funds to deliver evidence-based treatment (Kepple, Parker, Whitmore, & Comtois, 2019).
This study has limitations. We did not assess the influence of other county-level variables on our opioid-related outcomes due to statistical power considerations, and did not examine whether the average dose of prescriptions dispensed varied across region. Additionally, the data set we used did not provide county-level information on whether other drug(s) were associated with opioid-overdose deaths. Given that certain substances (e.g., benzodiazepines) may increase the likelihood of overdose when combined with opioids (Sun et al., 2017), this may be important to examine in future studies. While age-adjusted opioid-overdose death rate data was available at the state level, we did not have access to the same data to make urban-rural comparisons. We recommend that public health departments provide age-adjusted rates at both the state and county levels. As such, we used “crude” rates, in line with other overdose-death rate investigations (Paulozzi et al., 2011, Wheeler et al., 2012). Finally, one limitation of any county-level analysis is that it groups all commuting areas (or cities) within the county at the same urban-rural county classification. Future research is recommended to examine these patterns using more specific (i.e., rural-urban commuting areas) or further stratified (urban, rural/micropolitan, rural/remote) measures of geographic regions, when data is both available and powered for statistical analyses.
6. Conclusions
In summary, this study used county-level public data on opioid prescribing and opioid-overdose death rates across a five-year timeframe. These data were analyzed in Michigan, a state with rates higher than the national average for both outcomes (NIDA, 2019). This study identified ongoing upward trends in opioid-overdose deaths across county types, with consistently higher death rates in urban counties and higher prescribing rates in rural Michigan counties. This investigation highlights directions for future research in Michigan and other hard-hit regions, while also illustrating that hard-hit regions may experience nuanced differences compared to national trends. Furthermore, this study synthesizes epidemiological information in Michigan, which we used to develop knowledge for public health, and generate implications for prevention, intervention, and healthcare policy in Michigan and similar regions.
Author contributions
The first author led write-up and bivariate analyses and oversaw data extraction and joinpoint regression analyses. The second author assisted with write-up and all data analyses and extracted all data. The third author conducted joinpoint regression analyses and assisted with write-up related to those analyses. All authors read and approved of the final version of this manuscript.
Declaration of Competing Interest
The first and second author received funding from the State Targeted Response to the Opioid Crisis and State Opioid Response Grants from the State of Michigan (spend-through funding to the Michigan Department of Health and Human Services from the Substance Abuse and Mental Health Services Administration). Both authors declare no conflict of interest.
Acknowledgements
We thank Su Min Oh, Michigan Department of Health and Human Services, for assistance with navigating data sets used in this analysis.
Footnotes
Overdose refers to fatal and non-fatal overdoses; overdose death(s) refers to fatal overdose.
Crude rates use raw totals for opioid-overdose deaths and opioid prescriptions, respectively, at the state, rural county, and urban county levels. Raw totals are then used to calculate rates relative to the overall population, population of all rural counties, and population of all urban counties.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.abrep.2019.100234.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- American Society of Addiction Medicine (2014). Treating opioid addiction as a chronic disease. https://www.asam.org/docs/default-source/advocacy/cmm-fact-sheet---11-07-14.pdf (accessed May 10, 2019).
- Bachyrycz A., Shrestha S., Bleske B.E., Tinker D., Bakhireva L.N. Opioid overdose prevention through pharmacy-based naloxone prescription program: Innovations in health care delivery. Substance Abuse. 2017;38(1):55–60. doi: 10.1080/08897077.2016.1184739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The four domains of chronic disease prevention: Working toward healthy people in healthy communities. https://stacks.cdc.gov/view/cdc/27508/cdc_27508_DS1.pdf (accessed May 10, 2019).
- Cochran G.T., Engel R.J., Hruschak V.J., Tarter R.E. Prescription opioid misuse among rural community pharmacy patients: Pilot study for screening and implications for future practice and research. Journal of Pharmacy Practice. 2017;30(5):498–505. doi: 10.1177/0897190016656673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N., Creppage K., Austin A., Ringwalt C., Sanford C., Proescholdbell S.K. Observed transition from opioid analgesic deaths toward heroin. Drug and Alcohol Dependence. 2014;145:238–241. doi: 10.1016/j.drugalcdep.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Daubresse M., Alexander G.C., Crews D.C., Segev D.L., McAdams-DeMarco M.A. Trends in opioid prescribing among hemodialysis patients, 2007–2014. American Journal of Nephrology. 2019;49(1):20–31. doi: 10.1159/000495353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Licensing and Regulatory Affairs (2017). Michigan automated prescription system (MAPS): Annual drug utilization reports. Retrieved from https://www.michigan.gov/lara/0,4601,7-154-89334_72600_72603_55478_55479---,00.html (accessed February 16, 2019).
- Dick A.W., Pacula R.L., Gordon A.J., Sorbero M., Burns R.M., Leslie D.L., Stein B.D. Increasing potential access to opioid agonist treatment in US treatment shortage areas. Health Affairs (Project Hope) 2015;34(6):1028–1034. doi: 10.1377/hlthaff.2014.1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Division for Vital Records and Health Statistics, Michigan Department of Health and Human Services (2018). Total population estimates by county. http://www.mdch.state.mi.us/osr/CHI/POP/MAIN/PO17CO1.htm (accessed February 16, 2019).
- D’Onofrio G., O’Connor P.G., Pantalon M.V., Chawarski M.C., Busch S.H., Owens P.H.…Fiellin D.A. Emergency department–initiated buprenorphine/naloxone treatment for opioid dependence: A randomized clinical trial. JAMA. 2015;313(16):1636–1644. doi: 10.1001/jama.2015.3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubin R.E., Flannery J., Taenzer P., Smith A., Smith K., Fabico R.…Carlin L. ECHO Ontario chronic pain & opioid stewardship: Providing access and building capacity for primary care providers in underserviced, rural, and remote communities. Studies in Health Technologies and Informatics. 2015;209:15–22. [PubMed] [Google Scholar]
- Frank J.W., Levy C., Calcaterra S.L., Hoppe J.A., Binswanger I.A. Naloxone administration in US emergency departments, 2000–2011. Journal of Medical Toxicology. 2016;12(2):148–156. doi: 10.1007/s13181-015-0525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García M.C., Heilig C.M., Lee S.H., Faul M., Guy G., Iademarco M.F.…Gray J. Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system – United States, 2014–2017. Morbidity and Mortality Weekly Report. 2019;68(2):25–30. doi: 10.15585/mmwr.mm6802a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Rudenstine S., Vlahov D. Drug use, misuse, and the urban environment. Drug and Alcohol Review. 2005;24(2):127–136. doi: 10.1080/09595230500102509. [DOI] [PubMed] [Google Scholar]
- Green T.C., Grau L.E., Carver H.W., Kinzly M., Heimer R. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug and Alcohol Dependence. 2011;115(3):221–228. doi: 10.1016/j.drugalcdep.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guy G.P., Jr, Zhang K., Bohm M.K., Losby J., Lewis B., Young R.…Dowell D. Vital signs: Changes in opioid prescribing in the United States, 2006–2015. MMWR. Morbidity and Mortality Weekly Report. 2017;66(26):697. doi: 10.15585/mmwr.mm6626a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H., Miniño A.M., Warner M. National Center for Health Statistics; Hyattsville, MD: 2019. Urban–rural differences in drug overdose death rates, by sex, age, and type of drugs involved, 2017. NCHS Data Brief, no 345. [PubMed] [Google Scholar]
- Jaccard J., Becker M.A. 5th ed. Wadsworth; Belmont, WA: 2009. Statistics for the behavioral sciences. [Google Scholar]
- Jackson A., Shannon L. Barriers to receiving substance abuse treatment among rural pregnant women in Kentucky. Maternal and Child Health Journal. 2012;16(9):1762–1770. doi: 10.1007/s10995-011-0923-5. [DOI] [PubMed] [Google Scholar]
- Jannetto P.J., Helander A., Garg U., Janis G.C., Goldberger B., Ketha H. The fentanyl epidemic and evolution of fentanyl analogs in the United States and the European Union. Clinical Chemistry. 2019;65(2):242–253. doi: 10.1373/clinchem.2017.281626. [DOI] [PubMed] [Google Scholar]
- Kepple N.J., Parker A., Whitmore S., Comtois M. Nowhere to go? Examining facility acceptance levels for serving individuals using medications for opioid used disorder. Journal of Substance Abuse Treatment. 2019;104:42–50. doi: 10.1016/j.jsat.2019.06.004. [DOI] [PubMed] [Google Scholar]
- Keyes K.M., Cerdá M., Brady J.E., Havens J.R., Galea S. Understanding the rural–urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health. 2014;104(2):e52–e59. doi: 10.2105/AJPH.2013.301709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King A., Foley D., Arfken C., Aaron C., Sung L., Hlavaty L. Carfentanil-associated mortality in Wayne County, Michigan, 2015–2017. American Journal of Public Health. 2019;109(2):300–302. doi: 10.2105/AJPH.2018.304814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King N.B., Fraser V., Boikos C., Richardson R., Harper S. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: A systematic review. American Journal of Public Health. 2014;104(8):e32–e42. doi: 10.2105/AJPH.2014.301966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvamme E., Catlin M., Banta-Green C., Roll J., Rosenblatt R. Who prescribes buprenorphine for rural patients? The impact of specialty, location and practice type in Washington State. Journal of Substance Abuse Treatment. 2013;44(3):355–360. doi: 10.1016/j.jsat.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lister J.J., Brown S., Greenwald M.K., Ledgerwood D.M. Gender-specific predictors of methadone treatment outcomes among African Americans at an urban clinic. Substance Abuse. 2019;40(2):185–193. doi: 10.1080/08897077.2018.1547810. [DOI] [PubMed] [Google Scholar]
- Lister J.J., Weaver A., Ellis J.D., Ledgerwood D.M., Himle J.A. A Systematic Review of Rural-Specific Barriers to Medication Treatment for Opioid Use Disorder in the United States. The American Journal of Drug and Alcohol Abuse. 2019 doi: 10.1080/00952990.2019.1694536. In press. [DOI] [PubMed] [Google Scholar]
- Lister, J.J., (2017). The opioid crisis is at its worst in rural areas: Can telemedicine help? The Conversation US. Retrieved from: https://theconversation.com/the-opioid-crisis-is-at-its-worst-in-rural-areas-can-telemedicine-help-86598 (accessed May 10, 2019).
- Look K.A., Kile M., Morgan K., Roberts A. Community pharmacies as access points for addiction treatment. Research in Social and Administrative Pharmacy. 2019;15(4):404–409. doi: 10.1016/j.sapharm.2018.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mack K.A., Jones C.M., Ballesteros M.F. Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan Areas—United States. MMWR Surveillance Summaries. 2017;66(19):1–12. doi: 10.15585/mmwr.ss6619a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall B.D., Krieger M.S., Yedinak J.L., Ogera P., Banerjee P., Alexander-Scott N.E.…Green T.C. Epidemiology of fentanyl-involved drug overdose deaths: A geospatial retrospective study in Rhode Island, USA. International Journal of Drug Policy. 2017;46:130–135. doi: 10.1016/j.drugpo.2017.05.029. [DOI] [PubMed] [Google Scholar]
- Michigan Substance Use Disorder Data Repository (2018). The opioid epidemic in Michigan. Michigan Department of Health & Human Services. https://mi-suddr.com/blog/2018/09/26/opioid-prescriptions-written/ (accessed February 16, 2019).
- Michigan Substance Use Disorder Data Repository (2018). The opioid epidemic in Michigan: Opioid Prescriptions Dispensed. Michigan Department of Health & Human Services. https://mi-suddr.com/blog/2018/09/26/opioid-prescriptions-written/ (accessed February 16th, 2019).
- Michigan Substance Use Disorder Data Repository (2018). The opioid epidemic in Michigan: Drug Overdose Deaths. Michigan Department of Health & Human Services. https://mi-suddr.com/blog/2018/09/26/opioid-heroin-poisonings/ (accessed February 16, 2019).
- Monnat S.M. The contributions of socioeconomic and opioid supply factors to US drug mortality rates: Urban-rural and within-rural differences. Journal of Rural Studies. 2019;68:319–335. [Google Scholar]
- National Institute on Drug Abuse (2019). Opioid summaries by state. https://www.drugabuse.gov/drugs-abuse/opioids/opioid-summaries-by-state (accessed May 7, 2019).
- Nobel T.B., Zaveri S., Khetan P., Divino C.M. Temporal trends in opioid prescribing for common general surgical procedures in the opioid crisis era. The American Journal of Surgery. 2019;217(4):613–617. doi: 10.1016/j.amjsurg.2018.11.047. [DOI] [PubMed] [Google Scholar]
- Okie S. A flood of opioids, a rising tide of deaths. New England Journal of Medicine. 2010;363(21):1981–1985. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- Paulozzi L.J., Kilbourne E.M., Desai H.A. Prescription drug monitoring programs and death rates from drug overdose. Pain Medicine. 2011;12(5):747–754. doi: 10.1111/j.1526-4637.2011.01062.x. [DOI] [PubMed] [Google Scholar]
- Pitt A.L., Humphreys K., Brandeau M.L. Modeling health benefits and harms of public policy responses to the US opioid epidemic. American Journal of Public Health. 2018;108(10):1394–1400. doi: 10.2105/AJPH.2018.304590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prunuske J.P., St Hill C.A., Hager K.D., Lemieux A.M., Swanoski M.T., Anderson G.W., Lutfiyya M.N. Opioid prescribing patterns for non-malignant chronic pain for rural versus non-rural US adults: A population-based study using 2010 NAMCS data. BMC Health Services Research. 2014;14(563):1–8. doi: 10.1186/s12913-014-0563-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossen L.M., Khan D., Warner M. Hot spots in mortality from drug poisoning in the United States, 2007–2009. Health & Place. 2014;26:14–20. doi: 10.1016/j.healthplace.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl L., Seth P., Kariisa M., Wilson N., Baldwin G. Drug and opioid-involved overdose deaths—United States, 2013–2017. Morbidity and Mortality Weekly Report. 2019;67(5152):1419–1427. doi: 10.15585/mmwr.mm675152e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein B.D., Mendelsohn J., Gordon A.J., Dick A.W., Burns R.M., Sorbero M.…Liccardo Pacula R. Opioid analgesic and benzodiazepine prescribing among Medicaid-enrollees with opioid use disorders: The influence of provider communities. Journal of Addictive Diseases. 2017;36(1):14–22. doi: 10.1080/10550887.2016.1211784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun E.C., Dixit A., Humphreys K., Darnall B.D., Baker L.C., Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356:j760–j767. doi: 10.1136/bmj.j760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner A., Kim S.H., Friedman D.B., Foster C., Bergeron C.D. Barriers to medical research participation as perceived by clinical trial investigators: Communicating with rural and African American communities. Journal of Health Communication. 2015;20(1):88–96. doi: 10.1080/10810730.2014.908985. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Agriculture Economic Research Service (2019). Documentation: Rural-Urban Continuum Codes. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx#.U9-B-4Vbw7C (accessed May 7, 2019).
- U.S. Department of Agriculture Economic Research Service (2019). Documentation: What is rural? https://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/what-is-rural/ (accessed August 26, 2019).
- U.S. National Cancer Institute . Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute; Bethesda, MD: 2019. Joinpoint Regression Program, Version 4.7.0.0. [Google Scholar]
- U.S. National Cancer Institute (2019). Joinpoint Help Manual 4.7.0.0. Retrieved from https://surveillance.cancer.gov/joinpoint/Joinpoint_Help_4.7.0.0.pdf.
- Wang K.H., Becker W.C., Fiellin D.A. Prevalence and correlates for nonmedical use of prescription opioids among urban and rural residents. Drug and Alcohol Dependence. 2013;127(1–3):156–162. doi: 10.1016/j.drugalcdep.2012.06.027. [DOI] [PubMed] [Google Scholar]
- Wheeler E., Davidson P.J., Jones T.S., Irwin K.S. Community-based opioid overdose prevention programs providing naloxone—United States, 2010. MMWR. Morbidity and Mortality Weekly Report. 2012;61(6):101–105. [PMC free article] [PubMed] [Google Scholar]
- Wingrove P., Park B., Bazemore A. Rural opioid use disorder treatment depends on family physicians. American Family Physician. 2016;94(7):546. [PubMed] [Google Scholar]
- Winstanley E.L., Lander L.R., Berry J.H., Mahoney J.J., III, Zheng W., Herschler J., Haut M.W. West Virginia's model of buprenorphine expansion: Preliminary results. Journal of Substance Abuse Treatment. 2019 doi: 10.1016/j.jsat.2019.05.005. (manuscript published online May 8, 2019) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.