Abstract
Though Hispanics live long lives, whether a “Hispanic paradox” extends to older-age health remains unclear, as do the social processes underlying racial-ethnic and immigrant-native health disparities. Using data from the Health and Retirement Study (2004–2012) (N=6,581), we assess the health of US- and foreign-born Hispanics, relative to US-born Whites and Blacks, and examine the socioeconomic, stress, and behavioral pathways contributing to health disparities. Findings indicate higher disability, depressive, metabolic, and inflammatory risk for Hispanics relative to Whites and similar health profiles among Hispanics and Blacks. We find limited evidence of a healthy immigrant pattern among foreign-born Hispanics. While socioeconomic factors account for Hispanic-White gaps in inflammation, disparities in other outcomes persist after adjustment for SES, due in part to group differences in stress exposure. Hispanics may live long lives, but their lives are characterized by more socioeconomic hardship, stress, and health risk than Whites and similar health risks as Blacks.
Keywords: aging, health disparities, Hispanic paradox
A substantial body of research examines racial-ethnic and immigrant-native disparities in US adult health and mortality. On the one hand, studies indicate that Blacks and, to some extent, Hispanics experience worse health than Whites (Brown 2018; Hummer and Gutin 2018). On the other hand, research documents an immigrant health advantage, with studies indicating that immigrants have better health and live longer lives than their native peers (Dupre, Gu, and Vaupel 2012; Hummer and Gutin 2018). In particular, Hispanic mortality rates among adults aged 50 and above are lower than the non-Hispanic White population; this advantage, termed the Hispanic paradox, is particularly pronounced among Hispanic immigrants (Elo et al. 2004; Lariscy et al. 2015).
Despite a vast literature in this area, several critical questions regarding the health of the diverse aging population remain unanswered. First, while much research assesses the magnitude and direction of racial-ethnic and immigrant-native health disparities, the social processes and exposures that contribute to these disparities are less clear. Further, despite clear documentation of the Hispanic mortality paradox, less is known about whether the paradox extends to health (Hayward et al. 2014). Finally, most studies of population health disparities use cross-sectional data, which leaves questions about the life course patterning of health inequalities unanswered. Together, these gaps suggest that the relative health and well-being of native- and foreign-born Hispanics remains to be better understood, particularly as these groups fare across diverse measures of morbidity as they age.
Using nationally representative, longitudinal data, this study examines the physical, psychological, and physiological well-being of older age native- and foreign-born Hispanics, relative to U.S.-born Whites and Blacks, and further assesses the socioeconomic, stress-related, and behavioral explanations for population health disparities. This study advances scholarship on racial-ethnic and immigrant-native health disparities, generally, and Hispanic health, specifically, in three key ways. First, while most research on Hispanic health utilizes disease or mortality outcomes, we include a range of pre-disease markers of physical health, psychological well-being, and physiological functioning with documented links to morbidity and mortality. As such, this study provides a comprehensive assessment of the health of the aging population and sheds new light on the factors producing disparities in disease emergence and progression. Second, this study assesses the role of multiple social factors contributing to population health gaps and is among the first to examine stress exposure as a mechanism underlying Hispanic-White and Hispanic-Black disparities in health. Finally, this study uses nationally representative, longitudinal data, which improves understanding of the state and determinants of the health of older US adults. Together, our findings contribute new knowledge of the health profiles of the diverse aging population; document racial-ethnic and nativity-status disparities in social exposures; and provide new evidence on the role of social factors in producing population disparities in disease emergence and progression from mid- through late-life.
BACKGROUND
Racial-Ethnic Health Disparities
Despite reductions in morbidity and mortality over the past century, stark racial and ethnic health gaps persist. In studies of racial-ethnic health inequality, race and ethnicity are often treated as proxies for the underlying determinant of health gaps: racism (Schnittker and McLeod 2005). A system of domination that ranks the value of groups as superior or inferior (Bonilla-Silva 1997), racism contributes to population health gaps at the institutional, interpersonal, and individual levels through the propagation of attitudes, beliefs, and differential treatment of group members by both individuals and institutions (Gee, Walsemann, and Brondolo 2012). Thus, racial and ethnic health disparities stem from this broader system of stratification that structures access to resources, opportunities, and risks by race and ethnicity (Phelan and Link 2015).
Much of the research on racial-ethnic health inequality focuses on Black-White health gaps, with studies showing that, compared to US-born non-Hispanic Whites (hereafter, Whites), US-born Blacks (hereafter, Blacks) experience earlier disease, disability, and death from a range of causes, including diabetes, cardiovascular disease, and cancer (Hummer and Gutin 2018). While Blacks experience similar or lower rates of psychiatric disorders than Whites, the evidence on the magnitude and direction of Black-White gaps in measures of psychological distress and well-being is mixed (Williams 2018).
Health disparities between Hispanics and Whites also exist, though the patterning is less consistent than Black-White health gaps. Research suggests that Hispanics have lower or comparable rates of cancer and cardiovascular disease (Crimmins et al. 2004), similar or better psychological well-being (Williams 2018), and longer life expectancies (Elo et al. 2004; Lariscy et al. 2015) than Whites but higher rates of diabetes (Crimmins et al. 2004) and disability (Hayward et al. 2014; Sheftel and Heiland 2018). The factors underlying the equivocal findings on the relative health of Hispanics are complex and multifaceted. For one, the magnitude and direction of racial-ethnic health gaps depends on nativity status and outcome (Brown 2018; Hummer and Gutin 2018), so failure to differentiate native and foreign-born Hispanics and/or including only one or two health outcomes in empirical studies risks masking substantial heterogeneity within and across groups. The mixed findings also reflect the relative positioning of Hispanics within the US racial order. Racism in the US has largely been predicated on a Black/White binary, and how Hispanics fare within this context is situational and evolving (Frank, Akresh, and Lu 2010). Hispanics are phenotypically diverse with varied racial identities (Chinn and Hummer 2016), and studies vary in their treatment of “Hispanic” as a racial or ethnic origin category, which further complicates understanding of the relative well-being of this group. For these reasons, a more complete understanding of the health of the aging Hispanic population requires an assessment of how systems of racial and nativity status inequality intersect across the life course to produce differential trajectories of health across a variety of outcomes (Brown 2018).
The Immigrant Health Advantage
Immigrants experience fewer chronic conditions (Brown 2018; Gorman, Read, and Krueger 2010), less depression (Harker 2001), and lower mortality rates (Dupre, Gu, and Vaupel 2012) than US-born individuals. Research on the immigrant health advantage has shown that Hispanic mortality rates are not only lower than the non-Hispanic White population but that foreign-born Hispanics have mortality rates 15–20% lower than US-born Hispanics (Lariscy et al. 2015). Further, studies indicate that Hispanic immigrants have fewer bed disability days, lower obesity rates, lower levels psychological distress, and lower rates of hypertension and cardiovascular disease than US-born Hispanics (Hummer and Gutin 2018).
The Life Course Patterning of Health Inequality
A core principle from the life course perspective is that aging is a life-long process (Pavalko and Willson 2011). Individual health changes across the life span in response to social exposures; as such, subpopulation differences in life course social exposures can produce differential timing and accumulation of health problems. Consistent with this notion, studies indicate Blacks and Hispanics may experience accelerated aging in mid-to late-life—a process often referred to as “weathering” (Geronimus et al. 2010)—in response to cumulative exposure to hardship across the life course. As a result, Black and Hispanic individuals experience earlier onset of physiological dysregulation and disease risk than Whites (Boen 2019; Brown, O’Rand, and Adkins 2012). Though few studies assess the life course patterning of immigrant-native health gaps, insights from previous work on the healthy immigrant effect suggest that US-born groups may experience earlier health decline than their foreign-born counterparts, but that such a pattern depends on race-ethnicity (Brown 2018).
Given that individual and group trajectories of health respond to social exposures, it follows that the magnitude and direction of population health disparities may vary across the life course. Existing empirical work focuses on three hypotheses about the age patterning of population health disparities, with studies finding that support for the hypotheses varies by outcome, race-ethnicity, and age (Boen 2016; Brown, O’Rand, and Adkins 2011). Studies finding support for the “cumulative advantage hypothesis” show that population health gaps grow through mid- and late-life, as advantaged groups accumulate more health resources over time relative to their less advantaged counterparts (Boen 2016; Brown, O’Rand, and Adkins 2012). Evidence for the “age-as-leveler” hypothesis shows that disparities converge—and even cross-over—in late life as both advantaged and disadvantaged groups experience the biological frailty and senescence associated with aging (Haas and Rohlfsen 2010). Finally, the “persistent inequality hypothesis” suggests that the magnitude of population health gaps remains stable with age (Haas and Rohlfsen 2010; Warner and Brown 2011). Still, because so few studies use longitudinal data to study the life course patterning of population health gaps across multiple outcomes, questions about how these inequalities unfold with age remain largely unanswered.
The Social Determinants of Population Health Gaps
Studies typically focus on three sets of social factors contributing to racial-ethnic and nativity status variations in health. First, socioeconomic disparities are key drivers of subpopulation differences in health (Boen 2016). Lower SES individuals have higher risk of disease, death, and disability across the life course than their higher SES counterparts. There are numerous pathways through which higher SES shapes health, including factors related to status, power, prestige, and personal autonomy; improved access to healthy foods and safe living environments; better health care; lower exposure to violence; and greater access to health-enhancing social networks (Link and Phelan 1995; Marmot 2004).
Blacks and Hispanics have markedly fewer socioeconomic resources than Whites, including substantially less wealth (Kochnar and Cilluffo 2017) and lower levels of education (Everett et al. 2013). Because SES is both a “fundamental” determinant of health (Link and Phelan 1995) and strongly patterned by race and ethnicity, a number of studies find that racial and ethnic health disparities are at least partially attributable to SES, including both Black-White (Boen 2016; Haas and Rohlfsen 2010) and Hispanic-White gaps (Crimmins 2007). Still, research on the Hispanic mortality paradox indicates that the relative socioeconomic disadvantage of Hispanics, while deleteriously affecting health and longevity, actually compresses the Hispanic mortality advantage, suggesting that Hispanic health would be more favorable and mortality would be lower if Hispanics had comparable levels of SES as Whites (Lariscy et al. 2015).
Second, differential exposure to stressors also plays a role in population health gaps. Studies in this area draw on the stress process model (Pearlin et al. 1981) to assess the pathways through which stress exposure “gets under the skin” to affect disease risk. In response to stress, the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system (SNS) secrete hormones to up-regulate physiological functioning, including in the immune, metabolic, and cardiovascular systems (Cohen et al. 2012). In the short term, these physiological changes are necessary to protect health from acute threats and infections, but repeated activation of the body’s stress response systems due to chronic stress exposure can promote physiological dysregulation and increase disease and mortality risk (Cohen et al. 2012).
Blacks report higher levels of stress than Whites (Turner 2013), and studies indicate that differences in stress exposure contribute to Black-White health inequality (Boen 2019; Sternthal, Slopen, and Williams 2011; Williams 2018). Research also suggests that US-born Hispanics report greater stress exposure than Whites, with reports of stress exposure among US-born Hispanics being similar to US-born Blacks. However, foreign-born Hispanics tend to report similar levels of stress exposure as US-born Whites (Sternthal, Slopen, and Williams 2011), which may be due to the conventional stress-related items being measured. Foreign-born Hispanics may be particularly vulnerable to stressors associated with acculturation to the US, such as legal status, language barriers, and living outside of one’s home country (Finch and Vega 2003; Williams 2018), which are less commonly assessed in health studies. Though stress exposure may account for a portion of health gaps between US-born Hispanics and Whites, there is little evidence that conventional measures of stress exposure explains health gaps between foreign-born Hispanics and Whites (Sternthal, Slopen, and Williams 2011).
Finally, health behaviors, particularly smoking patterns, may play a role in producing racial-ethnic and nativity status gaps in health. While Black-White differences in smoking contribute to racial differences in life expectancy (Ho and Elo 2012), life course patterns of smoking are lower among Hispanics than US-born Blacks and Whites (Lariscy et al. 2015). Estimates from Blue and Fenelon (2011) suggest that more than half of the mortality advantage among US immigrants relative to native-born adults is attributable to differences in smoking.
Gaps in the Literature
Despite a large body of research on racial-ethnic and nativity status disparities in health, three critical gaps remain. First, studies of the relative well-being of Hispanics focus predominantly on mortality, so less is known about whether the Hispanic mortality paradox extends to health (Hayward et al. 2014). Further, many studies of health outcomes utilize self-reported measures of disease or diagnosis, which risk misclassification error, whereby individuals who do not yet have a disease or diagnosis are classified as “well” (Turner 2013). Concerns about misclassification are particularly salient in studies of racial-ethnic health disparities, given documented disparities in health care access and diagnosis (Fiscella, Franks, and Gold 2000). The misclassification of individuals with high levels of physiological dysregulation or psychological distress as “healthy” could result in underestimating the magnitude of population health disparities, as well as mask the social processes contributing to health disparities. Further, the racial-ethnic and nativity-status patterning of biophysiological well-being among middle and older age adults remains to be better understood; the literature offers especially conflicting evidence regarding the relative biological well-being of Hispanics. Some studies document that Hispanics have higher levels of biological risk than Whites (Crimmins et al. 2007), while others find that Hispanics display similar levels of biological risk as Whites (Peek et al. 2010; Zhang et al. 2012). Taken together, past research suggests that morbidity, disability, and biophysiological functioning may not be as tightly tied to mortality for Hispanics as for Whites and Blacks (Hayward et al. 2014; Sheftel and Heiland 2018). Moreover, questions regarding the magnitude and direction of racial-ethnic and nativity-status disparities in physical, psychological, and physiological functioning remain open.
Second, the social processes and exposures contributing to population patterning of health need greater understanding. Studies of racial-ethnic health gaps have typically focused on the role of SES in producing disparities. Less research has focused on the social factors contributing to observed patterns of Hispanic health, particularly as these factors shape nativity-status variation in outcomes. While studies suggest that the relatively favorable Hispanic mortality rates may not extend to some health conditions, there is little empirical evidence of the mechanisms producing disparities in non-mortality outcomes, such as biological and physical functioning. Despite a wide body of literature documenting the role of stress exposure in contributing to Black-White health disparities (Boen 2019), few studies assess the role of stress in shaping the health of older age Hispanics and differentiating their outcomes from Blacks and Whites.
Finally, while a number of studies document racial-ethnic and nativity-status disparities using cross-sectional data or community-based samples, less is known about how population health disparities unfold across the life course using nationally-representative, longitudinal data. Insights from the life course perspective suggest that individual health changes across the life span in response to social exposures, but few studies empirically examine these processes. Still, understanding how exposures across the life span shape trajectories of health is essential to identifying the role of social factors in producing health at any particular time. Research suggests that the magnitude and direction of population health disparities vary across the life course (Brown, O’Rand, and Adkins 2012; Brown 2018), but because so few studies use longitudinal data to study the life course patterning of population health gaps across multiple outcomes, questions about how these inequalities unfold with age remain unanswered.
Research Aims
Using nationally representative, longitudinal data, the present study fills these critical gaps by examining the physical, psychological, and biological well-being of older age US- and foreign-born Hispanics, relative to US-born Whites and Blacks, and further assessing the socioeconomic, stress-related, and behavioral pathways underlying racial-ethnic and immigrant-native disparities in health. In particular, this study has three aims:
1) Determine and compare the physical, psychological, and biological functioning profiles of older age US- and foreign-born Hispanics, US-born Blacks, and US-born Whites;
2) Assess the racial-ethnic and nativity-status patterning of socioeconomic resources, stress exposures, and health behaviors among older age adults; and
3) Examine how disparities in socioeconomic factors, stress, and health behaviors contribute to racial-ethnic and immigrant-native disparities in physical, psychological, and biological well-being.
DATA AND METHODS
Data and Samples
Data come from the Health and Retirement Study (HRS), a nationally representative, longitudinal study of U.S. adults aged 50 years and older. Started in 1992, the HRS collects information about the social, economic, physical, and psychological well-being of older adults. The HRS sample was selected using a multi-stage area probability design that included oversamples of Hispanics (Heeringa and Connor 1995). The HRS collected blood-based biomarkers on a random half of the sample in 2006, and the other half of the sample provided biomarker data in 2008. These sample respondents were re-interviewed in 2010 and 2012, respectively, when they again provided blood samples. This study utilizes data from five waves of the HRS that include data on stress exposure and/or the outcomes of interest: 2004, 2006, 2008, 2010, and 2012. Analytic samples include US- and foreign-born Hispanic, US-born Black, and US-born White respondents aged 50 and older with complete data on the variables used in the analyses; longitudinal samples include respondents with at least one valid wave of observation. Sample sizes vary by outcome: functional limitations (N=6,581); depressive symptoms (N=6,436), metabolic dysregulation (N=3,412); and C-reactive protein (N=3,853). The analysis for functional limitations includes 5,472 US-born Whites, 663 US-born Blacks, 242 US-born Hispanics, and 204 foreign-born Hispanics; the racial-ethnic sub-samples are proportionally lower for other outcomes. The majority of Hispanics in the sample (approximately 57%) are of Mexican origin. On average, foreign-born Hispanics in the sample had been in the US 36 years at baseline in 2004.
Measures
Outcomes
We include four outcomes that together provide a comprehensive assessment of health across bodily systems: functional limitations, depressive symptoms, metabolic dysregulation, and C-reactive protein (CRP). Functional limitations is a composite measure indicating difficulty performing five Activities of Daily Living (ADL): dressing, walking, bathing, eating, and getting in/out of bed (range=0–5). Depressive risk is a count indicating respondent scores on the 8-item Center for Epidemiological Studies Depression (CES-D) scale. Respondents were asked whether they experienced the following symptoms in the last week: felt depressed, everything was an effort, sleep was restless, was happy (reverse coded), felt lonely, felt sad, could not get going, and enjoyed life (reverse coded). The final depressive symptoms score indicated the number of symptoms that the respondent reported feeling “much of the week” (range=0–8). Metabolic dysregulation is a composite that indicates overall levels of metabolic burden: blood pressure, waist circumference, Hba1c, total cholesterol, HDL cholesterol, and body mass index. For each individual marker, we construct a dummy variable indicating high risk according to clinical guidelines, and then sum the individual measures to construct an indicator of overall metabolic burden (range=0–6). CRP is an acute phase protein produced by the liver that is a marker of inflammation and immune function. Because of its skewed distribution, we log transform CRP. To ensure that the social exposures occurred prior to measurement of the outcomes, we use the 2010 and 2012 measurements of metabolic dysregulation and CRP. Functional limitations and depressive symptoms were measured in 2008, 2010, and 2012.
Socio-Demographic Characteristics
Race-ethnicity is self-reported and includes non-Hispanic Whites, non-Hispanic Blacks, and Hispanics. Immigrant status is measured using a variable indicating whether respondents were born in the US. We combine information on race-ethnicity and immigration status to create four categories: US-born non-Hispanic White, US-born non-Hispanic Black, US-born Hispanic, and foreign-born Hispanic. We also include measures of age (years), gender (1=female), and marital status (1=married or partnered). In longitudinal models, we include age2 to account for the curvilinear associations between age and the outcomes, as well as interactions of race-ethnicity/immigration status X age to document the age patterning of population health inequality. Finally, to account for the potential bias introduced by mortality selection, we include an indicator for death (1=died) in longitudinal models.
Key Explanatory Measures
Key explanatory variables include measures of SES, stress, and health behavior. Measures of SES include education (1=less than high school; 2=high school; 3=some college; 4=Bachelor’s degree or higher) and total household wealth. Measures of stress exposure come from leave behind questionnaires at the 2004, 2006, and 2008 waves of the HRS, though respondents did not answer questions about stress exposure at every wave. Consistent with prior research (Boen 2019; Sternthal, Slopen, and Williams 2011), we construct indices of the following widely-used stressors: lifetime traumas (Krause, Shaw, and Cairney 2004), stressful life events (Turner 2013), financial strain (Campbell, Converse, and Rodgers 1976), chronic strains (Troxel et al. 2003), everyday discrimination (Williams et al. 1997), and major lifetime discrimination (Williams et al. 1997). More detailed information on the stress measures can be found in Appendix A. For health behaviors, smoking history is included as a categorical variable (0=never smoker; 1=former smoker; 2=current smoker). Supplementary analyses adjusted for alcohol consumption, social integration, and social support, but these measures had comparatively high levels of missing data, relatively weak associations with the outcomes, and played no role in producing racial-ethnic or immigrant-native disparities in the outcomes. Thus, we excluded them from final analyses.
Analytic Strategy
We first examine racial-ethnic and immigrant-native disparities in the outcomes and covariates using weighted descriptive statistics and t-tests and chi-square statistics to formally assess subpopulation differences in the measures. For time-varying measures, means/proportions indicate the average score for each respondent over all waves for which they have valid data. We then use longitudinal mixed effects Poisson (for functional limitations) and negative binomial (for depressive symptoms) regression models to examine the associations between the exposures at baseline and changes in functional limitations and depressive risk with age. In these models, observations at level 1 are “nested” within individuals at level 2 (Raudenbush and Bryk 2002), generating trajectories of functional limitations and depressive symptoms as a function of the socioeconomic, stress, behavioral, and other measures. Likelihood ratio tests and Akaike information criterion indicated that models with quadratic slopes and random intercepts provided the best fit. Age, age2, marital status, and wealth are time-varying covariates measured in 2008–2012. All other covariates are time-constant and were measured at baseline (2004–2008), with the exception of the indicator for respondent death during the survey period, which was measured at the final observation. Given that the HRS does not provide longitudinal survey weights and because of debates about the utility of weighting longitudinal models, we do not weight the functional limitations or depressive symptoms models. Supplemental analyses using base-year and terminal-year weights produced substantively similar results.
For metabolic dysregulation and CRP, we exploit the temporal sequencing of the data by modeling the outcomes in 2010–2012 as a function of SES, stress exposure, and health behaviors in earlier waves (i.e., outcomes measured at t2 regressed on stress measured at t1) using Poisson (for metabolic dysregulation) and OLS (for CRP) regression models. These models are weighted using the HRS biomarker weights.
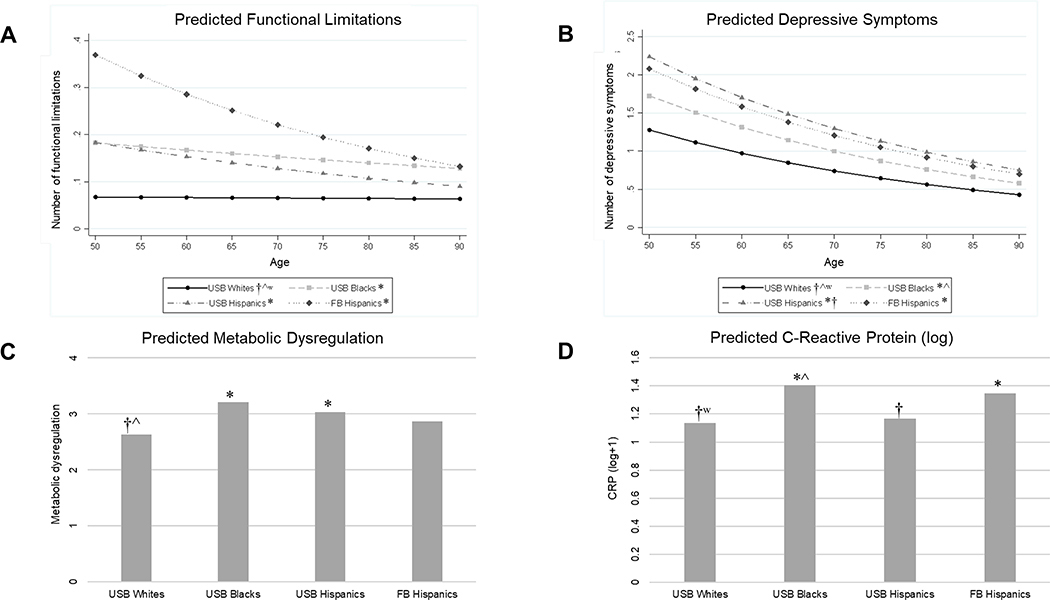
All models follow a similar covariate adjustment strategy. Model 1 documents the race-ethnic/nativity status patterning of the outcomes, adjusting for gender, marital status, age, and, in the longitudinal models, death. While Whites are the reference group in the multivariate models presented in Tables 2–5, Figure 1 visually depicts the results of Model 1 for each outcome and offers additional comparisons between racial-ethnic and immigrant-native groups. Models 2–4 build on Model 1 by including the socioeconomic, stress, and behavioral measures, respectively, in a stepwise fashion. Model 5 is the fully adjusted model and indicates how the key explanatory measures together account for the racial-ethnic patterning of the outcomes.
Table 2.
Race-Ethnicity, Nativity Status, and the Social Determinants of Trajectories of Functional Limitations (2006–2012)(N=6,581)
| Basic Adj. | M1+SES | M1+Stressors | M1+Behav. | Fully Adj. | |
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| IRR | IRR | IRR | IRR | IRR | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| For the intercept | |||||
| Racial/ethnic/immigrant disparity (US-born White is ref.) | |||||
| US-born Hispanics | 2.714** | 2.192* | 2.346* | 2.743** | 2.055 |
| (1.280 – 5.758) | (1.037 – 4.637) | (1.129 – 4.874) | (1.294 – 5.814) | (0.991 – 4.259) | |
| Foreign-born Hispanics | 5.478*** | 3.708*** | 5.073*** | 5.740*** | 3.683*** |
| (2.748 – 10.919) | (1.859 – 7.396) | (2.574 – 9.997) | (2.882 – 11.430) | (1.866 – 7.269) | |
| US-born Blacks | 2.708*** | 2.248*** | 2.520*** | 2.615*** | 2.242*** |
| (1.720 – 4.265) | (1.431 – 3.533) | (1.619 – 3.923) | (1.661 – 4.116) | (1.441 – 3.486) | |
| Socio-demographic characteristics | |||||
| Gender (1=female) | 1.040 | 0.997 | 1.019 | 1.112 | 1.034 |
| (0.896 – 1.207) | (0.860 – 1.157) | (0.880 – 1.180) | (0.954 – 1.296) | (0.889 – 1.202) | |
| Marital status (1=married or partnered) | 0.670*** | 0.719*** | 0.791*** | 0.691*** | 0.819** |
| (0.588 – 0.764) | (0.631 – 0.820) | (0.696 – 0.900) | (0.606 – 0.788) | (0.720 – 0.932) | |
| Died (1=yes) | 5.438*** | 4.820*** | 4.901*** | 5.252*** | 4.410*** |
| (4.507 – 6.562) | (3.997 – 5.812) | (4.087 – 5.878) | (4.353 – 6.336) | (3.677 – 5.290) | |
| Socioeconomic factors | |||||
| Education (HS is reference) | |||||
| <HS | 1.766*** | 1.754*** | |||
| (1.451 – 2.150) | (1.448 – 2.124) | ||||
| Some college | 1.063 | 1.012 | |||
| (0.884 – 1.279) | (0.845 – 1.212) | ||||
| BA+ | 0.600*** | 0.678*** | |||
| (0.485 – 0.742) | (0.552 – 0.834) | ||||
| Total household wealth | 1.000*** | 1.000 | |||
| (1.000 – 1.000) | (1.000 – 1.000) | ||||
| Stress exposure | |||||
| Lifetime traumas | 2.638*** | 2.298*** | |||
| (1.606 – 4.332) | (1.400 – 3.772) | ||||
| Stressful life events | 0.924 | 1.076 | |||
| (0.481 – 1.772) | (0.562 – 2.060) | ||||
| Financial strain | 1.374*** | 1.278*** | |||
| (1.263 – 1.494) | (1.172 – 1.394) | ||||
| Ongoing chronic strains | 2.655*** | 2.728*** | |||
| (2.207 – 3.193) | (2.268 – 3.281) | ||||
| Everyday discrimination | 1.069 | 1.063 | |||
| (0.969 – 1.180) | (0.964 – 1.172) | ||||
| Major discrimination | 1.610 | 1.965** | |||
| (0.979 – 2.650) | (1.194 – 3.236) | ||||
| Health behaviors | |||||
| Smoking (never smoker is reference) | |||||
| Former smoker | 1.315*** | 1.185* | |||
| (1.126 – 1.536) | (1.020 – 1.376) | ||||
| Current smoker | 1.631*** | 1.094 | |||
| (1.279 – 2.079) | (0.863 – 1.388) | ||||
| For the slope | |||||
| Age | 0.998 | 0.996 | 1.026* | 1.000 | 1.022 |
| (0.976 – 1.021) | (0.974 – 1.019) | (1.003 – 1.049) | (0.977 – 1.022) | (0.999 – 1.045) | |
| Growth rate of racial/ethnic/immigrant disparity (US-born White is ref.) | |||||
| US-born Hispanics X Age | 0.984 | 0.981 | 0.985 | 0.984 | 0.981 |
| (0.952 – 1.017) | (0.949 – 1.013) | (0.954 – 1.017) | (0.952 – 1.016) | (0.951 – 1.013) | |
| Foreign-born Hispanics X Age | 0.976 | 0.976 | 0.974* | 0.975 | 0.974* |
| (0.951 – 1.002) | (0.951 – 1.002) | (0.949 – 0.999) | (0.950 – 1.001) | (0.949 – 0.999) | |
| US-born Blacks X Age | 0.993 | 0.990 | 0.986 | 0.994 | 0.983 |
| (0.975 – 1.011) | (0.973 – 1.008) | (0.969 – 1.003) | (0.976 – 1.012) | (0.966 – 1.001) | |
| For the quadratic slope | |||||
| Age2 | 1.001*** | 1.001*** | 1.001*** | 1.001*** | 1.001*** |
| (1.001 – 1.002) | (1.001 – 1.002) | (1.001 – 1.002) | (1.001 – 1.002) | (1.001 – 1.002) | |
| Model fit statistics | |||||
| AIC | 18528.6 | 18435.0 | 18135.8 | 18513.9 | 18076.0 |
p<0.001
p<0.01
p<0.05
Notes: N=6,581; total observations=17,300. Results based on mixed effects Poisson regression models with random intercepts. Incidence rate ratios (IRR) and 95% confidence intervals reported. Only fixed effects parameters displayed. Functional limitations assessed in 2008–2012. Age, age2, marital status, and wealth are time-varying covariates measured in 2006–2012. Died indicates whether respondent died during observation period. All other covariates are time-constant and measured at baseline.
Table 5.
Race-Ethnicity, Nativity Status, and the Social Determinants of Inflammation (Log CRP)(N=3,853)
| Basic Adj. | M1+SES | M1+Stressors | M1+Behav. | Fully Adj. | |
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Coeff. | Coeff. | Coeff. | Coeff. | Coeff. | |
| (SE) | (SE) | (SE) | (SE) | (SE) | |
| Racial/ethnic/immigrant disparity (US-born White is ref.) | |||||
| US-born Hispanics | 0.032 | −0.041 | 0.013 | 0.031 | −0.042 |
| (0.082) | (0.084) | (0.082) | (0.085) | (0.086) | |
| Foreign-born Hispanics | 0.211* | 0.113 | 0.204* | 0.212* | 0.121 |
| (0.091) | (0.093) | (0.087) | (0.091) | (0.091) | |
| US-born Blacks | 0.270*** | 0.202** | 0.242*** | 0.236*** | 0.173** |
| (0.060) | (0.062) | (0.060) | (0.061) | (0.063) | |
| Socio-demographic characteristics | |||||
| Age | −0.001 | −0.003 | 0.002 | −0.000 | 0.000 |
| (0.002) | (0.002) | (0.002) | (0.002) | (0.002) | |
| Gender (1=female) | 0.087** | 0.068* | 0.091** | 0.124*** | 0.104*** |
| (0.031) | (0.030) | (0.031) | (0.030) | (0.030) | |
| Marital status (1=married or partnered) | −0.048 | −0.026 | −0.011 | −0.021 | 0.014 |
| (0.035) | (0.034) | (0.036) | (0.035) | (0.035) | |
| Socioeconomic factors | |||||
| Education (HS is reference) | |||||
| <HS | 0.089 | 0.082 | |||
| (0.051) | (0.050) | ||||
| Some college | −0.020 | −0.025 | |||
| (0.038) | (0.038) | ||||
| BA+ | −0.207*** | −0.178*** | |||
| (0.036) | (0.037) | ||||
| Total household wealth | −0.000*** | −0.000** | |||
| (0.000) | (0.000) | ||||
| Stress exposure | |||||
| Lifetime traumas | 0.248* | 0.147 | |||
| (0.122) | (0.121) | ||||
| Stressful life events | 0.033 | 0.066 | |||
| (0.142) | (0.139) | ||||
| Financial strain | 0.048* | 0.011 | |||
| (0.019) | (0.019) | ||||
| Ongoing chronic strains | 0.071 | 0.088* | |||
| (0.043) | (0.042) | ||||
| Everyday discrimination | 0.018 | 0.013 | |||
| (0.024) | (0.023) | ||||
| Major discrimination | 0.058 | 0.102 | |||
| (0.119) | (0.118) | ||||
| Health behaviors | |||||
| Smoking (never smoker is ref.) | |||||
| Former smoker | 0.131*** | 0.109*** | |||
| (0.030) | (0.029) | ||||
| Current smoker | 0.284*** | 0.212*** | |||
| (0.053) | (0.053) | ||||
| Model fit statistics | |||||
| AIC | 8759.0 | 8673.4 | 8717.2 | 8707.3 | 8622.5 |
p<0.001
p<0.01
p<0.05,
Notes: N=3,853. Results based on weighted OLS regression models. CRP assessed in 2010–2012; all other covariates measured in 2004–2008.
Figure 1.
Predicted Race/Ethnic/Nativity Disparities in Health
Note: Based on estimates from Model 1 of Tables 2–5. Symbols indicate the statistical significance of the difference between the respective group and: US-born Whites (*p<0.05), US-born Blacks (†p<0.05), US-born Hispanics (^p<0.05), and foreign-born Hispanics (wp<0.05).
RESULTS
Descriptive Statistics
Descriptive analyses in Table 1 reveal that Hispanics and Blacks have worse health profiles than Whites, but the magnitude and significance of Hispanic-White disparities depends on outcome and nativity status. Both US- and foreign-born Hispanics have more functional limitations and depressive symptoms than Whites and similar levels of functional and depressive risk as Blacks. US-born Hispanics have higher levels of metabolic risk than Whites and similar levels of metabolic risk as Blacks, but similar levels of CRP as Whites. On the other hand, foreign-born Hispanics have similar levels of metabolic risk as Whites, but higher CRP. Foreign-born Hispanics have similar levels of CRP compared to Blacks. Across all four outcomes, US- and foreign-born Hispanics have similar health profiles. Blacks fare worse than Whites across the four outcomes.
Table 1.
Descriptive Statistics by Race-Ethnicity and Nativity Status (N=6,581)
| US-born Hispanics (N=242) |
Foreign-born Hispanics (N=204) |
US-born Blacks (N=663) |
US-born Whites (N=5,472) |
p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Outcomes | |||||||||
| Functional limitations (count: 0–5) | 0.421 | * | 0.676 | * | 0.502 | * | 0.288 | †^ʷ | <0.001 |
| Depressive symptoms (count: 0–8) | 1.875 | * | 1.935 | * | 1.646 | * | 1.186 | †^ʷ | <0.001 |
| Metabolic dysregulation (count: 0–6) | 2.921 | * | 2.868 | † | 3.191 | *ʷ | 2.633 | †^ | <0.001 |
| C-reactive protein (log+1) | 1.209 | † | 1.396 | * | 1.381 | *^ | 1.142 | †ʷ | <0.001 |
| Socio-demographic characteristics | |||||||||
| Age | 68.024 | *†ʷ | 69.615 | *^ | 69.553 | *^ | 71.108 | †^ʷ | <0.001 |
| Gender (1=female) | 0.564 | 0.598 | 0.650 | * | 0.571 | † | 0.055 | ||
| Marital status (1=married or partnered) | 0.662 | † | 0.609 | *† | 0.458 | *^ʷ | 0.696 | †ʷ | <0.001 |
| Died (1=yes) | 0.123 | 0.122 | 0.127 | 0.112 | 0.725 | ||||
| Socioeconomic factors | |||||||||
| Education | |||||||||
| <HS | 0.448 | *†ʷ | 0.625 | *†^ | 0.370 | *^ʷ | 0.108 | †^ʷ | <0.001 |
| High school | 0.274 | 0.184 | 0.299 | 0.398 | |||||
| Some college | 0.190 | 0.123 | 0.219 | 0.238 | |||||
| BA+ | 0.088 | 0.067 | 0.112 | 0.255 | |||||
| Household wealth (dollars) | 247,745 | *† | 159,394 | * | 144,045 | *^ | 586,128 | †^ʷ | <0.001 |
| Domain-specific stressors | |||||||||
| Lifetime traumas (range: 0–1) | 0.175 | 0.131 | 0.154 | 0.157 | 0.334 | ||||
| Stressful events (range: 0–1) | 0.064 | * | 0.046 | 0.056 | 0.044 | ^ | 0.038 | ||
| Financial strain (range: 0–5) | 2.603 | *† | 2.646 | * | 2.823 | *^ | 2.321 | †^ʷ | <0.001 |
| Ongoing chronic strains (range: 0–4) | 1.553 | * | 1.574 | * | 1.555 | * | 1.478 | †^ʷ | <0.001 |
| Everyday discrimination (range: 0–6) | 1.783 | *ʷ | 1.479 | †^ | 1.788 | *ʷ | 1.634 | †^ | 0.007 |
| Major discrimination (range: 0–1) | 0.088 | † | 0.060 | † | 0.127 | *^ʷ | 0.068 | † | <0.001 |
| Health behaviors | |||||||||
| Smoking | |||||||||
| Never smoker | 0.431 | *ʷ | 0.538 | *†^ | 0.389 | *ʷ | 0.443 | †^ʷ | <0.001 |
| Former smoker | 0.432 | 0.354 | 0.382 | 0.455 | |||||
| Current smoker | 0.137 | 0.107 | 0.229 | 0.102 | |||||
Notes: Weighted descriptive statistics. The last column of the table indicates the p-value of overall race/ethnic/immigration status differences (chi-square test). Symbols indicate the statistical significance of the difference in means between the respective group and: US-born Whites (*p<0.05), US-born Blacks (†p<0.05), US-born Hispanics (^p<0.05), and foreign-born Hispanics (ʷp<0.05). Sample size for covariates based on analytic sample for functional limitations (N=6,581). Sample size for outcome measures reflect analytic samples for the multivariate analyses: functional limitations (N=6,581); depressive symptoms (N=6,436), metabolic dysregulation (N=3,412); and CRP (N=3,853). For time-varying measures, means/proportions indicate the average score for each respondent over all waves for which they have valid data.
Table 1 also reveals stark disparities in other measures. Hispanics and Blacks have lower levels of educational attainment and household wealth than Whites, with heterogeneity by nativity status. Hispanics have lower levels of education than Blacks, but US-born Hispanics have more wealth than Blacks. Across several domains, Hispanics and Blacks report more stress than Whites, but the magnitude of Hispanic-White differences again depends on nativity. Hispanics and Blacks report more financial strain and ongoing chronic strains than Whites. Blacks report more everyday and major discrimination than the other groups. While US-born Hispanics report more stressful life events than Whites, foreign-born Hispanics report similar numbers of events. Further, foreign-born Hispanics report similar exposure to everyday discrimination as Whites, but US-born Hispanics report more discrimination than both Whites and foreign-born Hispanics. Further, foreign-born Hispanics report the lowest levels of lifetime smoking.
Multivariate Models
Functional Limitations
Results from Model 1 of Table 2 indicate that Hispanics and Blacks have more functional limitations than Whites, with foreign-born Hispanics reporting the greatest number. The racial-ethnic and immigrant-native gaps are constant with age, providing evidence of the persistent inequality hypothesis. Figure 1a visually depicts the results of Model 1 and further reveals that Whites have fewer functional limitations than the other three groups and that US- and foreign-born Hispanics and Blacks have similar functional limitation trajectories.
Model 2 adjusts for SES, and results reveal a strong socioeconomic gradient in functional limitations, with high levels of educational attainment (IRR=.600, p<0.001) and household wealth (IRR=1.000, p<0.001) being associated with fewer limitations and low levels of education being associated with more limitations (IRR=1.766, p<0.001). Model 3 adjusts for stress exposure, and results indicate that lifetime traumas (IRR=2.638, p<0.001), financial strain (IRR=1.374, p<0.001), and ongoing chronic strains (IRR=2.665, p<0.001) are positively associated with functional limitations. In Model 3, the gap between foreign-born Hispanics and Whites decreases with age, providing evidence of the age-as-leveler hypothesis. Model 4 indicates that both current and former smokers have more limitations than non-smokers.
Model 5 is the fully adjusted model. Indicators of education and stress exposure maintain their associations with functional limitations, net of the other covariates. Major discrimination is also associated with more functional limitations. Former smokers continue to have higher levels of functional limitations, while there is no difference between current smokers and nonsmokers. The gap between US-born Hispanics and Whites is eliminated in Model 5, though foreign-born Hispanic-White and Black-White gaps persist. Moreover, the foreign-born Hispanic-White gap decreases slightly with age, providing evidence of the age-as-leveler hypothesis. Across the models presented in Table 2, Model 5 exhibits the best fit.
Depressive Risk
Table 3 presents results for depressive symptoms. In Model 1, US- and foreign-born Hispanics and US-born Blacks report more depressive symptoms than Whites (p<0.001). As shown in Figure 1B, US-born Hispanics have more depressive symptoms than Blacks, but similar levels of depressive risk as foreign-born Hispanics. Supplementary analyses also included age X race-ethnicity/nativity interactions, but the coefficient estimates for these interactions were not significant and greatly reduced model fit so are excluded from final models. Results support the persistent inequality hypothesis, whereby the magnitude of the health gaps remains constant with age.
Table 3.
Race-Ethnicity, Nativity Status, and the Social Determinants of Trajectories of Depressive Risk (2006–2012)(N=6,436)
| Basic Adj. | M1+SES | M1+Stressors | M1+Behav. | Fully Adj. | |
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| IRR | IRR | IRR | IRR | IRR | |
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | (95% CI) | |
| For the intercept | |||||
| Racial/ethnic/immigrant disparity (White is ref.) | |||||
| US-born Hispanics | 1.751*** | 1.482*** | 1.566*** | 1.750*** | 1.391*** |
| (1.474 – 2.080) | (1.250 – 1.757) | (1.340 – 1.829) | (1.475 – 2.077) | (1.192 – 1.623) | |
| Foreign-born Hispanics | 1.629*** | 1.256* | 1.520*** | 1.659*** | 1.255** |
| (1.350 – 1.964) | (1.040 – 1.518) | (1.283 – 1.802) | (1.377 – 1.999) | (1.057 – 1.491) | |
| US-born Blacks | 1.350*** | 1.157** | 1.177** | 1.322*** | 1.052 |
| (1.209 – 1.507) | (1.036 – 1.292) | (1.063 – 1.303) | (1.185 – 1.475) | (0.950 – 1.165) | |
| Socio-demographic characteristics | |||||
| Gender (1=female) | 1.254*** | 1.207*** | 1.232*** | 1.301*** | 1.227*** |
| (1.168 – 1.346) | (1.126 – 1.295) | (1.154 – 1.316) | (1.211 – 1.398) | (1.148 – 1.312) | |
| Marital status (1=married or partnered) | 0.626*** | 0.649*** | 0.710*** | 0.645*** | 0.728*** |
| (0.588 – 0.666) | (0.610 – 0.691) | (0.669 – 0.754) | (0.606 – 0.686) | (0.686 – 0.772) | |
| Died (1=yes) | 1.816*** | 1.674*** | 1.665*** | 1.743*** | 1.543*** |
| (1.621 – 2.036) | (1.496 – 1.874) | (1.500 – 1.848) | (1.556 – 1.953) | (1.392 – 1.711) | |
| Socioeconomic factors | |||||
| Education (HS is reference) | |||||
| <HS | 1.416*** | 1.373*** | |||
| (1.278 – 1.568) | (1.251 – 1.508) | ||||
| Some college | 0.964 | 0.950 | |||
| (0.884 – 1.051) | (0.877 – 1.028) | ||||
| BA+ | 0.658*** | 0.717*** | |||
| (0.599 – 0.722) | (0.658 – 0.782) | ||||
| Total household wealth | 1.000*** | 1.000 | |||
| (1.000 – 1.000) | (1.000 – 1.000) | ||||
| Stress exposure | |||||
| Lifetime traumas | 1.632*** | 1.421** | |||
| (1.296 – 2.054) | (1.131 – 1.785) | ||||
| Stressful life events | 0.743* | 0.801 | |||
| (0.556 – 0.993) | (0.602 – 1.066) | ||||
| Financial strain | 1.232*** | 1.172*** | |||
| (1.185 – 1.281) | (1.126 – 1.220) | ||||
| Ongoing chronic strains | 2.076*** | 2.115*** | |||
| (1.910 – 2.258) | (1.947 – 2.297) | ||||
| Everyday discrimination | 1.209*** | 1.203*** | |||
| (1.156 – 1.265) | (1.151 – 1.257) | ||||
| Major discrimination | 0.940 | 1.099 | |||
| (0.744 – 1.188) | (0.871 – 1.386) | ||||
| Health behaviors | |||||
| Smoking (never smoker is ref.) | |||||
| Former smoker | 1.150*** | 1.082* | |||
| (1.068 – 1.237) | (1.012 – 1.157) | ||||
| Current smoker | 1.573*** | 1.219*** | |||
| (1.406 – 1.760) | (1.101 – 1.351) | ||||
| For the slope | |||||
| Age | 0.973*** | 0.970*** | 0.989* | 0.974*** | 0.987** |
| (0.963 – 0.983) | (0.960 – 0.981) | (0.979 – 0.999) | (0.964 – 0.985) | (0.977 – 0.997) | |
| For the quadratic slope | |||||
| Age2 | 1.001*** | 1.001*** | 1.001*** | 1.001*** | 1.001*** |
| (1.000 – 1.001) | (1.000 – 1.001) | (1.000 – 1.001) | (1.000 – 1.001) | (1.000 – 1.001) | |
| Model fit statistics | |||||
| AIC | 47786.3 | 47567.8 | 46767.4 | 47727.0 | 46605.8 |
p<0.001
p<0.01
p<0.05
Notes: N=6,436; total observations=16,770. Results based on mixed effects negative binomial regression models with random intercepts. Incidence rate ratios (IRR) and 95% confidence intervals reported. Only fixed effects parameters displayed. Depressive symptoms assessed in 2008–2012. Age, age2, marital status, and wealth are time-varying covariates measured in 2006–2012. Died indicates whether respondent died during observation period. All other covariates are time-constant and measured at baseline.
Adjusting for SES in Model 2 reveals strong associations between SES and depressive risk, though racial-ethnic/immigrant disparities persist after adjusting for SES. Model 3 reveals that all of the stress measures are associated with depressive risk, with the exception of major discrimination, but population disparities in depressive symptoms persist after adjusting for stress. In Model 4, smoking history is strongly associated with depressive risk.
Model 5 adjusts for the full set of covariates. Most of the socioeconomic, stress, and health behavior measures maintain strong associations with depressive symptoms, net of one another. In the fully adjusted model, there is no depressive symptom gap between US-born Hispanics and Whites. Model 5 provides the best fit.
Metabolic Dysregulation
Table 4 presents results from the prospective metabolic dysregulation models, where the outcome in 2010–2012 was regressed on the covariates in 2004–2008. Model 1 shows that both US-born Hispanics (.144, p=0.001) and Blacks (.201, p<0.001) have higher levels of metabolic dysregulation than Whites, while foreign-born Hispanics have similar levels of metabolic risk as Whites. Consistent with findings in Table 1, Figure 1C reveals similar levels of metabolic dysregulation among US-born Hispanics and Blacks. Results from Model 2 indicate that higher levels of education and wealth are both protective against metabolic dysregulation. Adjusting for SES substantially attenuates the US-born Hispanic-White and Black-White disparities over Model 1, suggesting that these gaps in metabolic dysregulation are partially attributable to socioeconomic differences between the groups.
Table 4.
Race-Ethnicity, Nativity Status, and the Social Determinants of Metabolic Dysregulation (N=3,412)
| Basic Adj. | M1+SES | M1+Stressors | M1+Behav. | Fully Adj. | |
|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
| Coeff. | Coeff. | Coeff. | Coeff. | Coeff. | |
| (SE) | (SE) | (SE) | (SE) | (SE) | |
| Racial/ethnic/immigrant disparity (US-born White is ref.) | |||||
| US-born Hispanics | 0.144*** | 0.106* | 0.131** | 0.143*** | 0.096* |
| (0.043) | (0.041) | (0.044) | (0.042) | (0.041) | |
| Foreign-born Hispanics | 0.088 | 0.051 | 0.086 | 0.089 | 0.047 |
| (0.056) | (0.055) | (0.056) | (0.055) | (0.054) | |
| US-born Blacks | 0.201*** | 0.167*** | 0.187*** | 0.208*** | 0.173*** |
| (0.028) | (0.028) | (0.028) | (0.028) | (0.028) | |
| Socio-demographic characteristics | |||||
| Age | −0.002 | −0.002* | −0.000 | −0.002* | −0.002 |
| (0.001) | (0.001) | (0.001) | (0.001) | (0.001) | |
| Gender (1=female) | 0.033 | 0.022 | 0.039* | 0.043* | 0.032 |
| (0.019) | (0.019) | (0.019) | (0.020) | (0.020) | |
| Marital status (1=married or partnered) | −0.012 | 0.005 | 0.005 | −0.017 | 0.006 |
| (0.021) | (0.022) | (0.022) | (0.021) | (0.022) | |
| Socioeconomic factors | |||||
| Education (HS is reference) | |||||
| <HS | 0.001 | 0.011 | |||
| (0.028) | (0.028) | ||||
| Some college | −0.011 | −0.014 | |||
| (0.023) | (0.023) | ||||
| BA+ | −0.129*** | −0.130*** | |||
| (0.026) | (0.026) | ||||
| Total household wealth | −0.000** | −0.000* | |||
| (0.000) | (0.000) | ||||
| Stress exposure | |||||
| Lifetime traumas | 0.085 | 0.036 | |||
| (0.070) | (0.069) | ||||
| Stressful life events | 0.118 | 0.137 | |||
| (0.085) | (0.083) | ||||
| Financial strain | 0.030* | 0.007 | |||
| (0.012) | (0.013) | ||||
| Ongoing chronic strains | 0.009 | 0.026 | |||
| (0.027) | (0.026) | ||||
| Everyday discrimination | 0.031* | 0.026 | |||
| (0.015) | (0.014) | ||||
| Major discrimination | −0.051 | −0.019 | |||
| (0.075) | (0.074) | ||||
| Health behaviors | |||||
| Smoking (never smoker is ref.) | |||||
| Former smoker | 0.058** | 0.045* | |||
| (0.020) | (0.020) | ||||
| Current smoker | −0.058 | −0.103** | |||
| (0.034) | (0.034) | ||||
| Model fit statistics | |||||
| AIC | 1.48E+08 | 1.48E+08 | 1.48E+08 | 1.48E+08 | 1.47E+08 |
p<0.001
p<0.01
p<0.05
Notes: N=3,412. Results based on weighted OLS regression models. Metabolic dysregulation assessed in 2010–2012; all other covariates measured in 2004–2008.
Model 3 includes the stress measures. Only financial strain (.030, p=0.015) and everyday discrimination (.031, p=0.038) are associated with metabolic dysregulation. Including the stressor measures reduces the US-born Hispanic-White and Black-White gaps in metabolic risk over Model 1, indicating that differential exposure to stress contributes to these health disparities. Model 4 shows that former smokers have higher levels of metabolic dysregulation than never smokers (.058, p=0.004). The inclusion of the smoking measure in Model 4 does little to change the metabolic risk disparity between US-born Hispanics and Whites but slightly exacerbates the Black-White gap.
Model 5 is the fully adjusted model. Education, wealth, and smoking history maintain their associations with metabolic risk, while the associations between financial strain and everyday discrimination and the metabolic risk are reduced to marginal statistical significance (p<0.1). The US-born Hispanic-White gap is smallest in the fully adjusted model, which also provides the best fit.
CRP
Model 1 of Table 5 reveals that foreign-born Hispanics and Blacks have higher levels of CRP than Whites. US-born Hispanics have similar levels of CRP as Whites. Figure 1D further reveals that Blacks have higher CRP than Whites and US-born Hispanics, but similar levels of CRP compared to foreign-born Hispanics. Model 2 reveals that education and household wealth are associated with inflammation and that SES differences between foreign-born Hispanics and Whites completely account for subgroup differences in CRP. The Black-White disparity in inflammation is partially attenuated after adjusting for SES.
Models 3 shows that lifetime traumas (.248, p=0.042) and financial strain (.048, p=0.010) are positively associated with inflammation. The Black-White disparity in CRP is attenuated in Model 3 over Model 1, suggesting that Black-White differences in stress exposure may be a driver of Black-White differences in inflammation. Model 4 adjusts for smoking status, which is strongly associated with CRP. Adjusting for smoking attenuates the Black-White gap in inflammation.
In Model 5, the measures of SES, ongoing chronic strains, and smoking exhibit associations with inflammation. In the fully adjusted model, the Hispanic-White disparities are fully attenuated and the Black-White gap is the smallest in magnitude across the models presented in Table 5. Model 5 provides the best fit.
DISCUSSION
Using nationally representative, longitudinal data, the present study examines the physical, psychological, and biological well-being of individuals from mid- through late-life, paying particular attention to the health of the Hispanic population, and sheds new light on the socioeconomic, stress-related, and behavioral pathways underlying racial-ethnic and immigrant-native disparities across a variety of health markers.
In doing so, this study offers three key contributions to the scientific understanding of racial-ethnic and immigrant-native health disparities. First, findings indicated that the Hispanic mortality paradox does not extend to pre-disease markers of health risk, with results documenting stark racial-ethnic and nativity status disparities in physical, mental, and physiological well-being. Both US- and foreign-born Hispanics had higher levels of functional limitations and depressive symptoms than Whites. While foreign-born Hispanics have similar levels of metabolic dysfunction as Whites, US-born Hispanics have higher levels of metabolic risk. By contrast, foreign-born Hispanics had higher levels of CRP than Whites, while there was no significant disparity in inflammation between US-born Hispanics and Whites. Importantly, we found no evidence of a healthy immigrant effect across the four outcomes, perhaps because the foreign-born Hispanics in this study have been in the US on average 36 years. Further, across markers of health, Blacks fared worse than Whites, and there was a great level of similarity in health risk between Hispanics and Blacks. Consistent with previous studies (Brown 2018; Geronimus et al. 2010), findings showed that Hispanics and Blacks generally fare worse than Whites, indicating that racism accelerates health deterioration among Blacks and Hispanics relative to Whites by patterning exposure to resources, opportunities, and risks across the life course. While previous research provides mixed evidence on the relative health of Hispanics, findings from this study show that, along several dimensions of health, a White/non-White binary can be observed, where Whites have better health than Hispanics and Blacks, and Hispanics and Blacks have similarly high levels of health risk. In this way, our findings indicate that the health protections associated with Whiteness are not extended to Hispanics in the US racial context. Still, our findings also suggest that the racial stratification of health depends on nativity status, whereby these dimensions of stratification intersect to shape trajectories of health through old age (Brown 2018; Hummer and Gutin 2018).
Second, our results improve understanding of the life course patterning of racial-ethnic and immigrant-native disparities in health across mid- to late-life. Results from the functional limitations models documented age variation in the magnitude of population health gaps that depended on race-ethnicity and nativity status. In the fully adjusted functional limitation model, the US-born Hispanic-White and Black-White gaps provided evidence of the persistent inequality hypothesis, while the disparity between foreign-born Hispanics and Whites declined with age, offering evidence of the age-as-leveler hypothesis. Population disparities in functional limitations may decline with age due to racial-ethnic and nativity status variation in the onset and acceleration of functional limitations earlier in the life course. Relative to Whites, foreign-born Hispanics may experience physical decline at younger ages, possibly prior to age 50, when respondents entered the HRS, producing an eventual convergence of disparities at older ages as Whites experience the later-onset frailty associated with aging. Results from the depressive symptoms models in Table 3 indicated that racial-ethnic disparities in psychological well-being were constant with age, consistent with the persistent inequality hypothesis. Psychological well-being may not be subject to the same biological aging processes as disability risk. Social exposures may have similar associations with depressive risk regardless of the age at which they are experienced, which may in turn produce stable population disparities in depressive risk across the life course. Despite the differences in the age patterning of health inequity across outcomes, results suggest that intervening on population health disparities is most critical early in the life course, before these disparities emerge and, in some cases, persist unabated into old age.
Finally, our results provide new evidence of the social determinants of population disparities in health. Descriptive analyses revealed striking socioeconomic disparities between racial-ethnic/nativity groups. Across all four outcomes, results indicated that socioeconomic differences between older age Hispanics, Blacks, and Whites were key drivers of disparities. In fact, adjusting for SES completely accounted for the disparity in CRP between foreign-born Hispanics and Whites. While disparities in metabolic dysregulation were also largely attributable to SES, our findings are consistent with other studies showing that inflammatory processes may play a particularly critical role in linking disparities in social exposures to subpopulation gaps in health (Boen 2019). Together, our findings are consistent with previous studies showing that the unequal racial patterning of socioeconomic resources, opportunities, and exposures is a primary pathway through which racism harms health (Boen 2016; Phelan and Link 2015).
Our analyses also revealed the role of stress exposure in contributing to patterns of health inequality at older ages (Williams 2018). Descriptive analyses revealed stark racial-ethnic and nativity status patterning of stress exposure, and the multivariate models confirmed that subpopulation differences in stress exposure contribute to disparities in health. Importantly, we found that financial strain, ongoing chronic strains, and everyday discrimination were consistently associated with the outcomes and that adjusting for these measures resulted in the greatest reductions of subgroup disparities in the outcomes. These findings suggest that—unlike more acute events—exposure to ongoing, chronic stressors and strains may result in lasting wear and tear on physiological and psychological stress response systems. Whereas individuals may be able to “bounce back” from stressful events, repeated activation of the body’s stress response systems in response to chronic stressors results in physiological and psychological dysfunction. While previous studies have documented the role of stress in Black-White health gaps (Boen 2019), this study shows that Hispanic-White differences in stress exposure contribute to the accelerated physical, psychological, and physiological deterioration of Hispanics relative to Whites. As such, these findings suggest that social stratification—particularly along lines of race-ethnicity and nativity status—patterns the everyday lived experiences of individuals in ways that shape their exposure to a host of stressors and consequently impact their old age health. Looking ahead, population health data sets such as HRS should consider broadening the stressors measured to incorporate those that are particularly relevant to racial-ethnic minority and immigrant groups; measures of acculturation stress and racism-related stress, particularly in the current US political climate, may be especially important (Williams 2018).
Results also revealed that disparities in smoking contribute to racial-ethnic and immigrant-native health gaps. Across all four outcomes, smokers had worse health than non-smokers. Still, among older adults, racial-ethnic differences in smoking were modest, although foreign-born Hispanics exhibited the lowest smoking rates. Thus, adjusting for smoking in models either did not impact the magnitude of population health gaps or actually widened population disparities. The relatively low levels of smoking among foreign-born Hispanics proves protective for health as they age and contributes to their mortality advantage relative to Whites (Fenelon 2013; Lariscy et al. 2015). Our study shows that, while foreign-born Hispanics have greater risk of functional limitations and depression than Whites, their health risk would be even greater if their smoking patterns mirrored the older age White population.
Our study is not without limitations. First, we did not have sufficient statistical power to draw conclusions about how the racial-ethnic and nativity status disparities in health or drivers of health varied by gender or national origin. Further, analyses restricting the Hispanic sample to Mexican origin individuals yielded substantively similar results to those presented here. Still, gender and national origin are important axes of stratification that shape U.S. health disparities (Brown 2018; Hummer and Gutin 2018) and should be investigated in future studies. Second, our inclusion of stressor measures was an important contribution of the present study. Nonetheless, these measures were retrospectively collected among older aged individuals and, thus, did not assess stressors as individuals were experiencing them throughout the life course. Further, as discussed, there are additional stressors not measured here (for example, acculturation stress, hate crimes, incarceration, etc.) that likely play a role in population health gaps. Third, we find that smoking plays an important role in producing population health gaps, but future research should assess the role of other health behaviors in population health disparities. Fourth, while the socioeconomic, stress, and behavioral mechanisms included in this study attenuated health gaps, racial-ethnic and immigrant-native disparities remained even in fully adjusted models. As such, scholars should continue to develop and integrate additional life course socioeconomic and stress exposure measures into studies of population health disparities. Finally, though our longitudinal models adjust for mortality, our analyses may still be subject to survivor bias such that the least healthy individuals died before they were eligible for the survey.
In sum, our findings suggest that older age US- and foreign-born Hispanics in the United States experience higher levels of disability, depressive risk, and physiological dysregulation than Whites and similar levels of such health problems as Blacks. They also experience more socioeconomic disadvantage and stress exposure than Whites. Thus, Hispanics live longer lives than Whites and Blacks, but their lives are also characterized by greater levels of socioeconomic hardship, stress, and health risk than Whites and similar old age health risks as Blacks. Future research in this area should continue to interrogate whether and why morbidity, physiological functioning, and psychological well-being may not be as tightly tied to mortality for Hispanics as for Whites and Blacks.
Supplementary Material
Acknowledgments
Funding
The project described was supported by a Quartet Pilot Research Award and funded through the National Institute on Aging, P30 AG-012836–24. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Aging or the National Institutes of Health. We are also grateful to the Carolina Population Center and its NIH/NICHD center grant (P2C HD050924) for general support.
Biography
Courtney E. Boen is an assistant professor in the Department of Sociology and research associate in the Population Studies Center and Population Aging Research Center at the University of Pennsylvania. Dr. Boen’s research focuses on the social determinants of population health inequality, with a particular focus on the role of racism in shaping health disparities across the life course.
Robert A. Hummer is the Howard W. Odum Distinguished Professor of Sociology and Fellow of the Carolina Population Center at the University of North Carolina – Chapel Hill. Dr. Hummer’s research focuses on the accurate description and explanation of racial-ethnic, nativity status, and socioeconomic status disparities in US health and mortality patterns and trends.
Footnotes
Supplemental Material
Additional supporting information may be found in the online version of this article.
Contributor Information
Courtney E. Boen, University of Pennsylvania
Robert A. Hummer, University of North Carolina at Chapel Hill
References
- Blue L, & Fenelon A 2011. “Explaining low mortality among U.S. immigrants relative to native-born Americans: The role of smoking.” International Journal of Epidemiology 40: 786–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen Courtney. 2016. “The role of socioeconomic factors in Black-White health inequities across the life course: Point-in-time measures, long-term exposures, and differential health returns.” Social Science & Medicine 170: 63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boen Courtney. 2019. “Death by a Thousand Cuts: Stress Exposure and Black-White Disparities in Physiological Functioning in Late Life.” The Journals of Gerontology, Series B. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Silva E 1997. “Rethinking racism: Toward a structural interpretation.” American Sociological Review 465–480. [Google Scholar]
- Brown Tyson. 2018. “Racial Stratification, Immigration, and Health Inequality: A Life Course-Intersectional Approach.” Social Forces 96(4): 1507–1540. [Google Scholar]
- Brown TH, O’Rand AM, & Adkins DE 2012. “Race-ethnicity and health trajectories: Tests of three hypotheses across multiple groups and health outcomes.” Journal of Health and Social Behavior 53(3): 359–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell A, Converse PE, and Rodgers W 1976. The quality of American life: Perceptions, evaluations, and satisfactions. New York: Russell Sage Foundation. [Google Scholar]
- Chinn JJ, & Hummer RA 2016. “Racial disparities in functional limitations among Hispanic women in the United States.” Research on Aging 38(3): 399–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS and Turner RB 2012. “Chronic Stress, Glucocorticoid Receptor Resistance, Inflammation, and Disease Risk.” Proceedings of the National Academy of Sciences of the United States of America 109(16):5995–5999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins Eileen M., Kim Jung K., Alley Dawn E., Karlamangla Arun and Seeman Teresa. 2007. “Hispanic Paradox in Biological Risk Profiles.” American Journal of Public Health 97(7):1305–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Hayward MD, and Seeman T 2004. “Race/ethnicity, socioeconomic status and health” In Anderson NB, Bulatoa RA, and Cohen B (eds.) Critical perspectives on racial and ethnic differences in health in later life (pp. 310–352). Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Dupre Mathew E., Gu Danan, and Vaupel James W. 2012. “Survival Differences among Native-Born and Foreign-Born Older Adults in the United States.” PLoS One 7(5): e37177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma T., Turra Cassio M., Kestenbaum Bert and Ferguson BR 2004. “Mortality among Elderly Hispanics in the United States: Past Evidence and New Results.” Demography 41(1):109–128. [DOI] [PubMed] [Google Scholar]
- Everett Bethany G., Rogers Richard G., Krueger Patrick M., and Hummer Robert A. 2011. “Trends in Educational Attainment by Race/Ethnicity, Nativity, and Sex in the United States, 1989–2005.” Ethnic and Racial Studies 34(9): 1543–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A 2013. “Revisiting the Hispanic mortality advantage in the United States: The role of smoking.” Social Science & Medicine 82: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch Brian K., and Vega William A. 2003. “Acculturation Stress, Social Support, and Self-Rated Health among Latinos in California.” Journal of Immigrant Health 5(3): 109–117. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P, Gold MR, & Clancy CM 2000. “Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care.” JAMA 283(19): 2579–2584. [DOI] [PubMed] [Google Scholar]
- Frank R, Akresh IR, & Lu B 2010. “Latino immigrants and the US racial order: How and where do they fit in?” American Sociological Review 75(3): 378–401. [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E 2012. “A life course perspective on how racism may be related to health inequities.” American Journal of Public Health 102(5): 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus Arline T., Hicken Margaret T., Pearson Jay A., Seashols Sarah J., Brown Kelly L. and Cruz Tracey D. 2010. “Do US Black Women Experience Stress-Related Accelerated Biological Aging?” Human Nature 21(1):19–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman Bridget K., Read Jen’nan G., and Krueger Patrick M. 2010. “Gender, Acculturation, and Health among Mexican Americans.” Journal of Health and Social Behavior 51(4):440–57. [DOI] [PubMed] [Google Scholar]
- Haas Steven A., and Rohlfsen Leah 2010. “Life Course Determinants of Racial and Ethnic Disparities in Functional Health Trajectories.” Social Science & Medicine 70(2):240–50. [DOI] [PubMed] [Google Scholar]
- Harker K 2001. “Immigrant generation, assimilation, and adolescent psychological well-being.” Social Forces 79(3): 969–1004. [Google Scholar]
- Hayward Mark D., Hummer Robert A., Chiu Chi-Tsun, González-González César and Wong Rebeca 2014. “Does the Hispanic Paradox in US Adult Mortality Extend to Disability?” Population Research and Policy Review 33(1):81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa Steven G. and Connor Judith H. 1995. “Technical Description of the Health and Retirement Survey Sample Design.” Ann Arbor: University of Michigan. [Google Scholar]
- Ho JY, & Elo IT 2013. “The contribution of smoking to black-white differences in US mortality.” Demography 50(2): 545–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer Robert A. & Gutin Iliya 2018. “Racial/Ethnic and Nativity Disparities in the Health of Older US Men and Women.” Chapter 3 (pp. 31–66) in Future Directions for the Demography of Aging: Proceedings of a Workshop, edited by Hayward MD and Majmundar MK Committee on Population, Division of Behavioral and Social Sciences and Education, National Academy of Sciences, Engineering, and Medicine. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Kochnar Rakesh, and Cilluffo Anthony 2017. “How wealth inequality has changed in the U.S. since the Great Recession, by race, ethnicity and income” Fact Tank: News in the Numbers. Pew Research Center, November 1, 2017. Available at: http://www.pewresearch.org/fact-tank/2017/11/01/how-wealth-inequality-has-changed-in-the-u-s-since-the-great-recession-by-race-ethnicity-and-income/ [Google Scholar]
- Krause N, Shaw BA, and Cairney J 2004. “A descriptive epidemiology of lifetime trauma and the physical health status of older adults.” Psychology and Aging 19(4): 637–48. [DOI] [PubMed] [Google Scholar]
- Lariscy Joseph T., Hummer Robert A. and Hayward Mark D. 2015. “Hispanic Older Adult Mortality in the United States: New Estimates and an Assessment of Factors Shaping the Hispanic Paradox.” Demography 52(1):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, & Phelan J 1995. “Social conditions as fundamental causes of disease.” Journal of Health and Social Behavior, 80–94. [PubMed] [Google Scholar]
- Marmot Michael 2004. The Status Syndrome: How Social Standing Affects our Health and Longevity. NY: Henry Holt and Company. [Google Scholar]
- Pavalko EK, & Willson AE 2011. “Life course approaches to health, illness and healing” In Handbook of the sociology of health, illness, and healing (pp. 449–464). Springer, New York, NY. [Google Scholar]
- Pearlin Leonard I., Menaghan Elizabeth G., Lieberman Morton A. and Mullan Joseph T. 1981. “The Stress Process.” Journal of Health and Social Behavior 22(4):337–356. [PubMed] [Google Scholar]
- Peek MK, Cutchin Malcolm P., Salinas Jennifer J., Sheffield Kristin M., Eschbach Karl, Stowe Raymond P. and Goodwin James S. 2010. “Allostatic Load among Non-Hispanic Whites, Non-Hispanic Blacks, and People of Mexican Origin: Effects of Ethnicity, Nativity, and Acculturation.” American Journal of Public Health 100(5):940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phelan JC, & Link BG 2015. “Is racism a fundamental cause of inequalities in health?” Annual Review of Sociology 41: 311–330. [Google Scholar]
- Raudenbush SW, & Bryk AS 2002. Hierarchical linear models: Applications and data analysis methods (Vol. 1). Sage. [Google Scholar]
- Schnittker J, & McLeod JD 2005. “The social psychology of health disparities.” Annu. Rev. Sociol 31: 75–103. [Google Scholar]
- Sheftel Mara, and Heiland Frank W. 2018. “Disability Crossover: Is There a Hispanic Immigrant Health Advantage That Reverses from Working to Old Age?” Demographic Research 39: 209–250. [Google Scholar]
- Sternthal MJ, Slopen N, & Williams DR 2011. “Racial disparities in health: how much does stress really matter?” Du Bois Review: Social Science Research on Race 8(1): 95–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ 2013. “Understanding Health Disparities: the Relevance of the Stress Process Model.” Society and Mental Health 3(3): 170–186. [Google Scholar]
- Warner David F., and Brown Tyson H. 2011. “Understanding How Race/Ethnicity and Gender Impact Age-Trajectories of Disability: An Intersectionality Approach.” Social Science & Medicine 72(8):1236–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R. 2018. “Stress and the Mental Health of Populations of Color: Advancing our Understanding of Race-Related Stressors.” Journal of Health and Social Behavior 59(4): 466–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Yu Yan, Jackson James S. and Anderson Norman B. 1997. “Racial Differences in Physical and Mental Health: Socio-Economic Status, Stress and Discrimination.” Journal of Health Psychology 2(3):335–351. [DOI] [PubMed] [Google Scholar]
- Zhang Zhenmei, Hayward Mark D. and Lu Chuntian 2012. “Is there a Hispanic Epidemiologic Paradox in Later Life? A Closer Look at Chronic Morbidity.” Research on Aging 34(5):548–571. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.