Abstract
Purpose
COVID-19 pandemic represents a novel challenge for healthcare systems, and it affects even the daily urological practice. Italy was the first country after China to experience a lock-down period. Our objective is to determine whether, during the COVID-19 period, there has been any modification in urological emergencies.
Methods
we retrospectively reviewed urgent urological consultations requested by the Emergency Department (ED) of Padua University Hospital in the 36-day period between February 22nd and March 30th, 2020 and compared them to the prior year cases within a similar time frame (February 24th to March 31st, 2019). Pediatric population (age < 15 years); surgical complications and traumas were excluded to avoid confounding from the reduction of activities during the lockdown. The number of daily consultations, the number of invasive procedures performed and admissions were evaluated, together with the predictors of admission were identified through multivariate logistic regression models.
Results
The final sample resulted in 107 consultations performed in 2020 and 266 in 2019. A higher number of daily consultations was performed during 2019 (7.33 vs 2.97, p < 0.001). Similarly, the number of daily-invasive procedures was higher in 2019 (p = 0.006), while there was no difference in the number of daily admissions (15 vs 12, p = 0.80). On multivariate analysis, the year (2020 vs 2019, OR 2.714, 95% CI 1.096–6.757, p = 0.0297) was a significant predictor of admission.
Conclusions
Urgent urology practice was affected during COVID-19 pandemic with a remarkable reduction in urgent urological consultations; furthermore, a higher risk of admissions was observed in 2020. The consequences of a potentially delayed diagnosis remain to be determined.
Electronic supplementary material
The online version of this article (10.1007/s00345-020-03264-2) contains supplementary material, which is available to authorized users.
Keywords: COVID-19, Pandemic, Urological emergencies, Urology
Introduction
The recent outbreak and diffusion of a respiratory disease (COVID-19) caused by a newly discovered coronavirus (Sars-CoV-2) [1] led to a worldwide pandemic, as declared by WHO on March 11th, 2020 [2]. After spreading in the Hubei region in China, the SARS-CoV-2 reached several different countries. Northern Italy was among the first areas to be hit, with the first cases reported on February 21st, 2020, causing the Government to declare a “red-zone” in the townships of these cases. Although no restrictions were put on the movements of citizens yet, people were asked to avoid unnecessary movements and hospital accesses. The official “lock-down” was declared initially (for the Padua province) on March 8th and extended to all of Italy the following day.
Padua University Hospital was identified as one of the Regional COVID-19 referral centers, with the creation of new COVID-dedicated medical wards and Intensive Care Units (ICUs). The Urology Department is an academic referral center and, according to Regional and Hospital Administration regulations [3], it strongly reduced elective urological activities, to shift some personnel to departments in need, similarly to what Naspro already reported in other Italian regions [4].
During the COVID-19 lock-down period, the Urology Department experienced an unexpected noticeable reduction in urgent urological consultations requested by the central Emergency Department (ED), that theoretically should not have decreased.
We thus hypothesized that during the COVID-19 outbreak daily consultations requested by the ED were reduced compared to the same period in 2019, possibly because of more “appropriate” access to the service during the pandemic, intended as patients presenting to the ED for real urgent needs.
Materials and methods
Study design and data collection
A retrospective chart review of urgent urological consultations requested by the ED of Padua University Hospital between February 22nd and March 30th, 2020 was performed. Urological consultations are registered through institutional software and each single urological report was reviewed by the Authors to assess the fulfillment of inclusion criteria. To maintain a comparable time window, including the same number of holidays and weekdays, we reviewed also urological consultations performed between February 24th and March 31st, 2019. Pediatric patients (age < 15 years) that refer to the Pediatric ED of Padua University Hospital, were excluded from the final analysis. Data collected were age, sex, day and time of the consultation performed, requesting ED physician, triage color, province of residence of the patient, diagnosis of discharge/admission, diagnostic tests requested, and invasive procedure performed by the urologist.
To avoid potential bias from the reduction of elective surgical activities and the lifestyle changes in the general population, consultations related to complications of surgical procedures performed within 30-days and every type of trauma were excluded from the analysis.
At Padua University Hospital, the triage classification is based on a four-level system, ranging from red (life-threatening condition) to white (non-critical, non-urgent care) [5]. Our Urology Department provides a 24-h urology service with the presence of dedicated staff, thus patients arriving to the ED and requiring urological consultation are promptly evaluated. The time of the consultation was dichotomized based on the staff shifts, in day (08:00–20:00) and night periods (20:00–08:00). During the period of time analyzed, ordinary elective urologic outpatient follow-up procedures and visits were reduced and maintained for oncological patients, but evaluations requested with a non-deferrable priority (less than 30 days, according to national classification) were guaranteed with no delay, since no tele-health service was provided as alternative.
The procedures performed by the urology staff during the consultations, such as bladder catheterization, evaluation of non-functioning indwelling urological devices (catheters, nephrostomy tubes, etc.) and minor surgical procedures performed in outpatient setting were considered as invasive procedures, however these procedures were not counted as such in the cases where the patient eventually needed in-hospital admission for any other urological cause.
To provide an overview of total number of non-COVID ED accesses, the raw number of patients evaluated at our ED were collected from the Management and Control Department database of the Hospital.
The outcomes analyzed were the number of daily invasive procedures or admission, the proportion of consults requiring either one, together with the predictors of admission.
Statistical analysis
Distributions were summarized using frequencies, medians and interquartile ranges. Independent sample t test, Mann–Whitney U test and Pearson Chi-squared test were used to model the association between continuous and categorical variables as appropriate. Logistic regression models were used to evaluate on multivariate analysis the predictors of admission. Any p value less than 0.05 was considered statistically significant. All analyses were performed using R Statistical Software (Foundation for Statistical Computing, Vienna, Austria).
Results
On a 36-day period we identified 287 and 109 urologic consultations performed, respectively, in 2019 and 2020. As per the study design, some cases had to be excluded from the final sample, which totaled 107 consultations performed in 2020 and 266 consultations performed in 2019 given that 2 surgical complications were identified during the COVID-19 outbreak period, and in the prior year there had been 8 traumatic events and 13 surgical complications.
Similarly, in the same timeframe the total number of ED accesses for any cause excluding COVID-19 was reduced from 14,964 in 2019 to 10,278 in 2020. Precisely, the reduction was 30.2% for those classified as “white code”, 49.2% for the “green”, 31.1% for the “yellow” and 8.8% for the “red” ones.
Table 1 summarizes the characteristics of the consultations performed, based on each time frame. During the COVID-19 period, the patients seeking urgent urological consult were older compared to the past year (median age 72 vs 64, p = 0.035) and there were different diagnoses of admission/discharge (p = 0.002), with almost one third (29%) presenting for urinary retention, compared to the 14.3% of the last year. There were 76 (28.6%) invasive procedures performed in 2019 and 36 (33.6%) in 2020, as well as 15 admissions in 2019-period (5.6%) and 12 in the 2020-period (11.2%).
Table 1.
Characteristics of consultations performed
| Variablea | Period | p valueb | |
|---|---|---|---|
| Non-COVID (total 266) | COVID (total 107) | ||
| Age | 64 (44–79) | 72 (53–83) | *0.035 |
| Sex | 0.489 | ||
| Male | 213 (80.1) | 89 (83.2) | |
| Female | 53 (19.9) | 18 (16.8) | |
| Consult time | 0.428 | ||
| Night | 96 (36.1) | 34 (31.8) | |
| Day | 170 (63.9) | 73 (68.2) | |
| Triage code | 0.805 | ||
| White | 117 (44.0) | 49 (45.8) | |
| Green | 95 (35.7) | 41 (38.3) | |
| Yellow | 21 (19.2) | 16 (15.0) | |
| Red | 3 (1.1) | 1 (0.9) | |
| Province | 0.272 | ||
| Padua | 236 (88.7) | 99 (92.5) | |
| Other | 30 (11.3) | 8 (7.5) | |
| Dx admission/discharge | *0.002 | ||
| Urinary retention | 38 (14.3) | 31 (29.0) | |
| Device malfunction | 27 (10.2) | 8 (7.5) | |
| Renal colic | 50 (18.8) | 20 (18.7) | |
| UTI | 24 (9.0) | 11 (10.3) | |
| Acute testicular pain | 27 (10.2) | 13 (12.1) | |
| Gross hematuria | 38 (14.3) | 12 (11.2) | |
| LUTS | 17 (6.4) | 9 (8.4) | |
| Other | 45 (16.9) | 9 (8.4) | |
| Invasive procedure and discharge | 76 (28.6) | 36 (33.6) | 0.336 |
| Admissions | 15 (5.6) | 12 (11.2) | 0.06 |
aMedian (25th–75th percentile) for continuous variables, number (%) for categorical variables
bMann–Whitney U Test for continuous variables, Pearson chi-squared test for categorical variables
The mean number of daily consultations performed was higher during the non-COVID-19 period (7.33 vs 2.97, mean difference 4.36, 95% CI 3.28–5.44, p < 0.001), as the number of daily-invasive procedures (p = 0.006), while there was no difference in the number of daily admissions (p = 0.80) (Fig. 1). When considering the percentage of consultations requiring urological intervention, intended as either an invasive procedure or admission, no difference was seen between the two periods: 33.26% vs 42.6% in 2019 and 2020, respectively, (mean difference − 9.344, 95% CI for the mean difference 21.446; 2.758; p = 0.128).
Fig. 1.
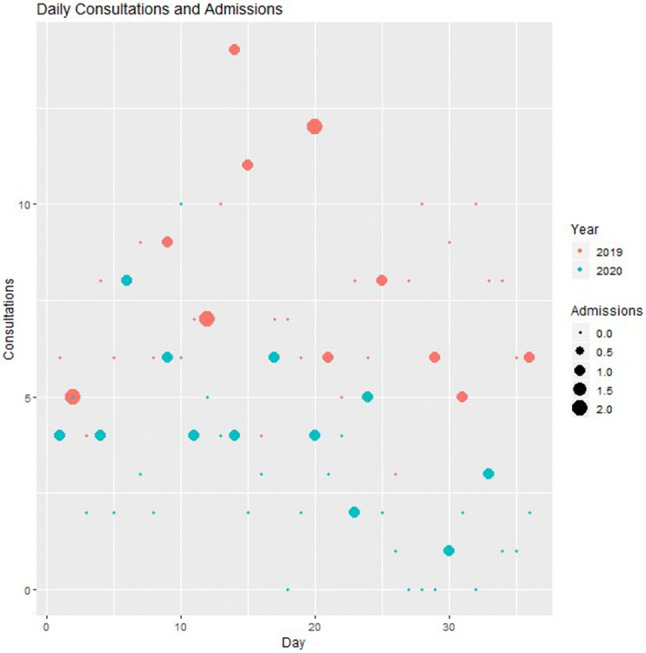
Plot of daily consultations and admissions
In-hospital admissions were 15 in 2019 and 12 in 2020, with similar characteristics and higher median age in 2020 (76 vs 59, p = 0.028) (Supplementary Table 1). The multivariate logistic regression model found that the period (COVID vs non-COVID, OR 2.714, 95% CI 1.096–6.757, p = 0.0297), the province of residency of the patients (outside Padua vs Padua, OR 5.812, 95% CI 1.99–16.643, p = 0.001) and the diagnosis of UTI (OR 5.386, 95% CI 1.304 – 25.314, p = 0.0229) were the only significant predictors of in-hospital admission (Supplementary Table 2). When analyzing the data from invasive procedures without admission, on multivariate analysis only age (p = 0.0284) resulted to be a significant predictor, while the period was not (p = 0.238) (Supplementary Table 3).
Discussion
Italy still is one of the most involved countries in 2020 SARS-CoV-2 spread, with the first cases diagnosed at the end of February [6]. With the contagion reaching a pandemic impact, a number of experts suggested the opportunity of a marked reduction of urological surgical activity, eventually leaving space only for urgent or oncological non-deferrable surgery during this COVID-19 emergency and recommending deferral of all the other activities [7–10]
Herein is provided the first outlook of how the urologic urgent practice has been affected, compared to last year, over a 5-week period. As already described in other medical fields, such as stroke and myocardial infarction [11, 12], the COVID-19 emergence caused a dramatic change in daily clinical practice, also involving urgencies. Within the period analyzed in our study, there was a reduction of ED accesses for any non-COVID-19 diagnosis (− 4686). In the same period, elective surgical activity performed in our Department experienced an 18.1% reduction, compared to last year (unpublished data), while urological consultations were approximately three times lower.
Since the beginning of COVID-19 outbreak in the country, there have been 8 days where none or just one urgent consultations were requested. During the coronavirus outbreak, the risk of admission resulted to be higher compared to last year (OR 2.714), despite a comparable raw number and rate of daily admissions, highlighting the fact that those conditions considered urgent are not missed. One plausible explanation of the higher proportion of admission during the COVID-19 period is that, the “fear” of the virus might have reduced the number of “improper” ED-accesses. Interestingly, despite the need for invasive procedures is usually intended as surrogate for appropriate urological consultation, the daily number of these procedures was reduced during the COVID-19 period.
These findings may have different interpretations. During the pandemic period patients might be reluctant to seek ED evaluation even when requiring prompt consultation by a specialist; as pointed out by others in this setting [4, 9]. The consequences of this scenario are difficult to estimate at this time, since more time is required to show the long-term effects of a delayed diagnosis. Common clinical scenarios presenting for urgent consultations are, for example, gross hematuria and urinary retention that often do not require admission, but prompt evaluation may prevent delay in the diagnosis of serious underlying conditions such as cancer. On the other hand, there is a common understanding that, at least in Italy, ED access may be frequently “abused” by the patients, that might take advantage of the service to speed up their diagnostic pathways through the public health system in case of non-urgent needs. Therefore, this number of patients is likely to be reduced during the pandemic. The importance of this aspect should not be underestimated as it demonstrates that the high proportion of unnecessary procedures performed in ordinary times, may overload the system jeopardizing healthcare management, consuming time and resources dedicated to the real needs. In our experience we found a significant difference in the diagnosis for patients presenting in the two periods of time, reflecting the aforementioned aspects: patients presenting for renal colic and testicular pain were more than halved in this year; probably a significant proportion of this reduction is represented by those patients presenting to the ED with mild and non-urgent conditions no more presenting to the ED, but even a small number of “missed” diagnosis for the more serious case could have significant clinical impact that is still to be determined [13].
Our study presents some limitations, the first is related to the small sample size; the second is that a single-center design might affect its universal validity, in particular regarding the criteria and triggers for urologic consultations and admission. However, this is the first reported experience in the urological emergency setting since the diffusion of the virus outside of China. Every country in the world is dealing with the pandemic in different ways because of its novelty and there is lack of unanimous consent on the best healthcare management strategies. It will be interesting to extend our observations to include a longer timeframe and other experiences on a regional, national and international basis. Another limitation is that Padua Hospital represents a tertiary center, which is subject to the risk of referral bias. Despite regulations limiting the movements of citizens in Italy (which do not apply to medical care), the higher risk of admission found for patients coming from other provinces confirms that our Department attracts more serious cases from outside the province. For this reason, the province of residence was included in the multivariate analysis. There might be also a number of potential unmeasured confounders limiting the comparison between the 2 years analyzed, however the exclusion in the study design of traumas and surgical complications aimed at avoiding potential confounding related to differences in lifestyle and reduction of the surgical activity caused by the “lock-down”. We found that during the COVID-19 period, consultations performed for surgical complications were more than six times lower and no traumatic event was identified, compared to eight during the same period of time in last year.
Conclusion
This novel healthcare scenario that the world is facing interests even the urology practice. Urgent care should theoretically remain barely untouched; surprisingly, we demonstrated that there was a considerable reduction of urgent urological consultations performed in the first 5 weeks of the COVID-19 pandemic. Probably a combination of postponed diagnoses and more proper access to the ED can explain this phenomenon; the consequences of this event are yet to be defined. This information will serve as a starting point for further research and healthcare management.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
GM: conception and design, acquisition of data, analysis and interpretation of data, statistical analysis, manuscript writing/editing. AM: conception and design; analysis and interpretation of data; manuscript writing/editing. MI: analysis and interpretation of data; manuscript writing/editing. MB: acquisition of data; manuscript writing/editing. GF: acquisition of data; manuscript writing/editing. OX: acquisition of data; manuscript writing/editing. FZ: conception and design; manuscript writing/editing; supervision. TPG: conception and design; manuscript writing/editing.
Funding
None.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This research study was conducted retrospectively from data obtained for clinical purposes.
Informed consent
Not applicable for this study.
Availability of data and material (data transparency)
Not applicable.
Code availability (software application or custom code)
R Statistical code available.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet (London, England) 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO (2020) Novel Coronavirus. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed 01 Apr 2020
- 3.Regione Veneto (2020) Coronavirus. Il Veneto riorganizza attività sanitarie per preservare posti di letto di terapia intensiva. https://www.regione.veneto.it/article-detail?articleId=4377038. Accessed 01 Apr 2020
- 4.Naspro R, Da Pozzo LF. Urology in the time of corona. Nat Rev Urol. 2020 doi: 10.1038/s41585-020-0312-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ministero della Salute (2012) Linee di Indirizzo Nazionali sul Triage Intraospedaliero. http://www.salute.gov.it/imgs/C_17_notizie_3849_listaFile_itemName_1_file.pdf. Accessed 01 Apr 2020
- 6.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet (London, England) 2020 doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribal MJ, Cornford P, Briganti A, et al. EAU Guidelines Office Rapid Reaction Group: an organisation-wide collaborative effort to adapt the EAU guidelines recommendations to the COVID-19 era. Eur Urol. 2020;S0302–2838(20):30324–30329. doi: 10.1016/j.eururo.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stensland KD, et al. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simonato A, et al. Pathways for urology patients during the COVID-19 pandemic. Minerva Urol Nefrol. 2020 doi: 10.23736/S0393-2249.20.03861-8. [DOI] [PubMed] [Google Scholar]
- 10.Ficarra V, et al. Urology practice during COVID-19 pandemic. Minerva Urol Nefrol. 2020 doi: 10.23736/S0393-2249.20.03846-1. [DOI] [PubMed] [Google Scholar]
- 11.Quotidiano Sanità (2020) Ictus, con il Coronavirus ricoveri più che dimezzati. Un dato che preoccupa. https://www.quotidianosanita.it/lettere-aldirettore/articolo.php?articolo_id=83098. Accessed 01 Apr 2020
- 12.Ictus, con il Coronavirus ricoveri più che dimezzati. Un dato che preoccupa, Quotidiano Sanità, 2020. https://www.quotidianosanita.it/lettere-al-direttore/articolo.php?articolo_id=83098. Accessed 01 Apr 2020
- 13.Proietti S, Gaboardi F, Giusti G. Endourological stone management in the era of the COVID-19. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


