Abstract
Coronavirus disease 2019 (COVID-19), which is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has caused great public concern worldwide due to its high rates of infectivity and pathogenicity. The Chinese government responded in a timely manner, alleviated the dilemma, achieved a huge victory and lockdown has now been lifted in Wuhan. However, the outbreak has occurred in more than 200 other countries. Globally, as of 9:56 am CEST on 19 May 2020, there have been 4,696,849 confirmed cases of COVID-19, including 315,131 deaths, reported to Word Health Organization (WHO). The spread of COVID-19 overwhelmed the healthcare systems of many countries and even crashed the fragile healthcare systems of some. Although the situation in each country is different, health workers play a critical role in the fight against COVID-19. In this review, we highlight the status of health worker infections in China and other countries, especially the causes of infection in China and the standardised protocol to protect health workers from the perspective of an anaesthesiologist, in the hope of providing references to reduce medical infections and contain the COVID-19 epidemic.
Keywords: COVID-19, SARS-CoV-2, Health worker infection, Personal protective equipment, Asymptomatic infection
Highlights
-
•
To analyze the causes of Chinese health worker infections at 3 stages of the epidemic.
-
•
It's pivotal to improve the ability to respond to public safety emergencies.
-
•
It's crucial to judge the epidemic situation timely and correctly.
-
•
It's imperative to minimise contact and apply artificial intelligence for medics.
-
•
Adequate personal protection is essential to protect health workers.
1. An overview of health worker infections of COVID-19 in China
COVID-19, which was first discovered in Wuhan, Hubei Province, China, has now led to a severe worldwide public health emergency. By 19 May 2020, the outbreak of COVID-19 had caused 84,500 confirmed cases in China, including 4,645 deaths [1]. At the same time, a large number of health workers were infected. As of 11 February 2020, a total of 3,019 health workers had been infected with SARS-CoV-2, accompanied by 1,716 confirmed cases, of which 6 died [2]. Most of the hospitals with severe medical infections were located in densely populated areas, and most of them were in non-infectious departments.
At present, there are no specific antiviral drugs or vaccines for use in humans against the SARS-CoV-2 infection. Therefore, the aim is instead to control the source of infection, to cut off routes of transmission and to do our best to treat the patients. Health workers are a valuable resource and an important part of the war against COVID-19. In the following, we will analyse the causes of Chinese health worker infections in order to provide learning points for other countries. The entire process of the Chinese fight against the COVID-19 epidemic can be roughly divided into three stages:
1.1. The first stage: From December 2019 to 20 January 2020
At this stage, the public had no information or knowledge of the nature, virulence, lethality and infectivity of the new virus, and very few paid attention to it. Due to a lack of awareness and an inaccessibility of information, frontline health workers in non-fever departments did not take any protective measures, which led to a greatly increased risk of medical infection. A large portion of health worker infections occurred through contact between health workers and asymptomatic patients or mildly symptomatic patients of COVID-19 during the early phase of the outbreak. Many infected medical personnel were located in departments that are considered low-risk, such as ophthalmology, neurology and gastroenterology and so on. This was due to insufficient cognition, inadequate protection and inaccessible information [3]. There was an anaesthesiologist infected by an orthopaedic patient who was in the incubation period in the authors’ hospital on 19 January 2020. The encounters of these Chinese health workers should warn health workers all over the world; COVID-19 is more contagious than severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), whether symptomatic or asymptomatic/latent [4,5]. Differing from SARS, the viral load of asymptomatic and latent COVID-19 patients is high and comparable to that of symptomatic patients [6]. Some asymptomatic patients, mildly infectious and latent patients became very important sources of infection during this period of time [7,8].
1.2. The second stage: From 20 January 2020 to 13 February 2020
On 20 January 2020, Dr Zhong Nan-Shan, a renowned respiratory expert and the head of a high-level expert team in the National Health Commission (NHC), confirmed the interpersonal transmission of SARS-CoV-2 and called on people to wear masks and avoid population movement [9]. However, many people in Wuhan had not yet realised the severity of the outbreak and were continued to hold all kinds of gatherings. The situation was worsening, and along with a dramatic increase in cases of COVID-19, the number of health worker infections had also increased significantly. Due to the poor control of the epidemic in the early stage and a severely insufficient of the supply of nucleic acid test kits, patients were not detected in a timely manner. All of the wards in the hospital became intensive care units, accompanied with inadequate rescue ventilators, monitors and other instruments and equipment, as well as professional doctors and nurses. This overwhelmed the healthcare system and resulted in a serious run-up of medical resources. Cross infections occurred between COVID-19 patients and ordinary patients or normal people. Many health workers were unable to achieve comprehensive protection, and even needed downgraded protection. At this stage, health workers suffered from multiple infections due to a lack of personal protective equipment (PPE) and medical apparatus, inadequate or even degraded protection and an overload of work.
1.3. The third stage: From 13 February 2020 to present
More than 40,000 healthcare workers were dispatched from all over China to Hubei Province and two hospitals were temporarily established in 10 days for the treatment severely ill patients [10]. Meanwhile, medical supplies from all over the world had also arrived. Medical device manufacturers in China had cancelled annual leave and resumed production. This alleviated the emergency situation with regard to medical supplies, and following this, the government constructed 16 Fang Cang makeshift hospitals with a capacity of more than 13,000 beds [10,11]. During this period, the “four categories of people” included were confirmed cases, suspected cases, fever patients and close contacts, all of which had been screened, treated and isolated in different places according to infection control principles. The implementation of these series of measures slowed down the spread of the pandemic and achieved a phased victory. Now, all COVID-19 patients have been cured, lockdown has been lifted in Wuhan, normal work and production order are gradually recovering.
At this stage, very few of health workers suffered from infection due to an emphasis on physical isolation and a neglect on behavioural isolation.
2. An overview of the COVID-19 pandemic worldwide
The outbreak has occurred in more than 200 other countries, areas or territories. As of 9:56 am CEST on 19 May 2020, there have been 4,696,849 confirmed cases of COVID-19, including 315,131 deaths globally, with total numbers of confirmed cases as follows: 1,477,516 in the United States of America, 231,350 in Spain, 225,435 in Italy, 174,697 in Germany, 140,036 in France and 243,699 in The United Kingdom [1]. The total number of deaths was 89,272 in the United States of America and 31,908 deaths in Italy [1]. International Council of Nurses announced that there were at least 90,000 confirmed health workers cases globally, 260 of which died by 6 May 2020 [12]. As of 13 May 2020, at least 11,369 health workers had been infected, 17 of which died in Germany and 25,446 health workers had been infected in Italy [13,14]. A total of 38,064 health workers had been infected with SARS-CoV-2 in Spain as of 11 May 2020 [15]. According to updated data from the Centre for Disease Control and Prevention on 14 April 2020, there were at least 9,282 health workers who had been identified as having COVID-19 from 12 February to 9 April 2020 in the United States, 27 of which died [16]. According to incomplete statistics, Italy had the largest number of doctors from among the European countries, at 141 per 100,000 people, and Germany had the largest number of hospital beds in Europe, at 800 per 100,000 people. Alternatively, in Wuhan, there were 287 doctors per 100,000 people and 703 hospital beds per 100,000 [17,18]. Without the assistance of medical workers from other cities and provinces in China, the healthcare system in Wuhan would have collapsed during the peak of the epidemic. Health workers in America have also encountered a shortage of protective equipment [19], and they and those in other countries are going through the same experiences as China, and therefore there are some lessons to share with health workers all over the world.
3. Future directions of health worker protection
3.1. Double triage, double buffer, double mode and double insurance
Hospitals should be divided into two categories, one for patients with COVID-19 and others for non-COVID-19 patients, also named ordinary patients. The management of elective surgery processes should be as follows: all patients should attend a designated place for SARS-CoV-2 testing (CT, SARS-CoV-2 antibody and nucleic acid test) before admission. If the test result returns as positive, the patient will need be treated at a designated hospital for COVID-19. Whereas, if the result is negative, an appointment should be made at an ordinary hospital for treatment. Upon admission to a general hospital, there should be strict buffering and isolation measures: the patient must first stay in a single room on a first-level buffer ward, after completing a second antibody and nucleic acid test for SARS-CoV-2 screening, they should be transferred to a secondary buffer ward, without symptoms. Surgery could be performed on patients who are asymptomatic for 7 days after admission and who had received two negative nucleic acid and antibody tests for SARS-CoV-2, with no exposure to the environment outside of the hospital, according to standard protection procedures.
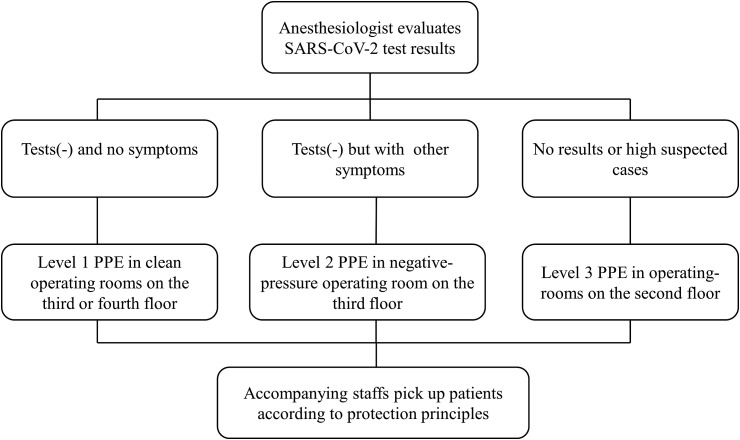
Emergency surgery management processes should be strictly performed following Fig. 1 . This principle of triage can effectively reduce cross-infection between patients, along with nosocomial infections between patients and health workers.
Fig. 1.
Emergency surgery management process in our hospital [note: tests (−) include sputum and nasopharyngeal swabs and other respiratory tract specimens tested negative in two consecutive nucleic acid tests and blood SARS-CoV-2 antibody tested negative in two antibody tests, with the sampling time at least 24 h apart, it means normal chest computed tomography simultaneously; Symptoms include fever (body temperature≥37.3 °C) and other respiratory symptoms; The operating rooms on the second floor are also clean operating rooms. As a contrast, laminar flow was turned off and an independent disinfection system such as ozone disinfection machine and ultraviolet air disinfection machine was used to disinfect the air and object surface during the COVID-19 epidemic].
Standard precautions include hand and respiration hygiene, the use of appropriate PPE according to a risk assessment, injection safety practices, safe waste management, proper linens, environmental cleaning and the sterilisation of patient-care equipment [20]. All health workers must receive training online before commencing their posts. Mutual help and supervision help to reduce infections.
WHO recommends that patients with respiratory symptoms wear masks, and for those patients without respiratory symptoms, no PPE is required [21]. In my opinion, this is only suitable in an ideal state. First of all, the patient must be identified quickly, when in fact, the detection capabilities of different countries are inconsistent. Many countries may not receive timely and effective testing, and moreover, there is the potential for interpersonal transmission during the incubation period [5]. This period of time could cause unconscious large-scale spread. Secondly, this relies on all patients being willing to wear masks, when wearing a mask effectively informs everyone that he/she is a patient, and some patients may be unwilling to wear a mask based on this. If they are not effectively isolated, these people would also become a huge source of infection, and cross-infection would happen between a patient and a normal person. Therefore, everyone should wear a mask to protect themselves and others.
Also, health workers should wear PPE. All health workers should carry out different levels of PPE if the risk level of the city where they are located has not been reduced to a low-risk level (Table 1 ).
Table 1.
Classification of protection principles to health workers (note: +Means necessary, −Means unnecessary, ±Means according to work needs, ±*Means alternative during Level 2).
| Protection level | General protection |
Level 1 |
Level 2 |
Level 3 |
|
|---|---|---|---|---|---|
| Non-fever clinic & non-infectious ward | Fever clinic & infectious ward | General diagnostic action to confirmed and suspected cases | Aerosol operation to confirmed cases and suspected cases | ||
| PPE | surgical mask | + | + | – | – |
| Medical protective mask | – | – | + | + | |
| protective goggles/headshield | – | – | ± | + | |
| scrubs | + | + | + | + | |
| disposable latex gloves | ± | + | + | + | |
| Work cloths | + | + | + | + | |
| isolation gown | – | + | ±* | – | |
| Medical protective gown | – | – | ±* | + | |
| surgical cap | – | + | + | + | |
| disposable shoe covers | – | – | + | + | |
3.2. Improve the awareness of self-protection and minimise contact with patients
Secondly, all health workers must strengthen the awareness of self-protection. According to the WHO, everybody needs to undertake regular hand hygiene but only the patient should wear a mask [21]. Controversially, some researchers found that universal masking in the community may mitigate the extent of transmission of SARS-CoV-2 and may be a necessary adjunctive public health measure in a densely populated city like Hong Kong Special Administrative Region (HKSAR) [22]. Masking is a continuous form of protection to stop the spreading of saliva and respiratory droplets to others or from others, and to the environment or from the environment to the susceptible by hands through touching of nose, mouth and eye. Therefore, it should be necessary for surgical masks to be worn at least in all medical staff. At the same time, we should not emphasize physical isolation and neglect behavioural isolation. Hand hygiene is a pivotal self-protection measure. According to the WHO, SARS-CoV-2 is transmitted between people through close contact and droplets, not by airborne transmission [21]. Therefore, minimising contact with patients or suspected patients, maintaining distance and performing regular hand hygiene may be more effective than PPE in isolation. As such, we should try our best to complete works by telephone, video conference, WeChat and other applications. For example, we have opened online consultations, contactless medication and electronic medical records and prescriptions, including wireless remote monitoring of analgesia systems for postoperative analgesia management, etc. In addition to electronic and paperless technologies, artificial intelligence technology should be more fully utilized. On the one hand, it can reduce the contact between health workers and patients. On the other hand, it can decrease the heavy workload of health workers, thereby better protecting health workers. At the same time, society must be prepared to fight the virus for a long time, and even if a hospital location has been reduced to a low-risk area, doctors should still perform hand hygiene regularly and wear masks, as well as be prepared to co-exist with the virus.
3.3. Ensure adequate medical supplies
Thirdly, ensure adequate medical supplies, including PPE and medical apparatus. Similar to the flight attendants, medical personnel must protect themselves before they can protect others. In the early phase of the virus there was an insufficient awareness and inadequate medical supplies that led to too many health workers becoming infected with SARS-CoV-2. Although the WHO recommended rational use PPE, Zhong's study found that one (2.7%) of 37 anaesthetists who wore Level 3 PPE developed PCR-confirmed COVID-19 as compared with 4/7 (57.1%) anaesthetists who had Level 1 protection in the operating theatre. The study suggests that using Level 3 PPE is more likely to reduce the risk of anaesthetic staff acquiring COVID-19, even from patients with mild symptoms [23]. We know that PPE is still in short supply, and with the progress of the epidemic, there may be further shortages. With the gradual control of the epidemic, some countries may reduce the amount of PPE to medical personnel due considerations regarding medical costs. All of this will put medical personnel into situations where they are exposed to SARS-CoV-2, which is not a responsible or humane action. In order to ensure the safety of health workers and patients, hospitals and governments must fully coordinate and make an effort to prevent health worker infections with COVID-19.
3.4. Pay attention to asymptomatic infections
What we have to be aware of is that some infected people “can be highly contagious when they are asymptomatic or mild cases combined represent about 40–50% of all infections” [[24], [25], [26]]. In non-infectious departments, it is important to be extremely vigilant in terms of infection prevention and control strategies. Protective measures need to be strengthened for medical personnel in non-infectious departments. For countries and regions with severe epidemics, if conditions permit, universal testing should be carried out as soon as possible, and patients admitted to hospital should undergo strict screening and early diversion and isolation. In my opinion, all protection levels should be increased by one level according to the classification of protection principles to health workers, because of the existence of asymptomatic and latent patients.
4. Conclusions
In actuality, each country must formulate its own infection prevention and control strategies according to its own national conditions. The experience of the Chinese may not be suitable to the situation in other countries, but the most essential things we need keep working on are: First of all, the state or region should establish a national emergency centre for major public safety emergencies with provinces, cities or states as the unit, which is used in normal time ready for the epidemic outbreak. Furthermore, the timely and accurate disclosure of epidemic information from various countries, centre for disease control (CDC) and health departments are critical to contain the epidemic and protect health workers. Last but not least, sufficient storage of PPE is necessary, meanwhile the introduction of electronic and paperless operations in medical system is imperative. Finally, medical staff should improve their awareness of protection and be proficient in infection control related knowledge.
Provenance and peer review
Not commissioned, externally peer-reviewed
Author contribution
Ling-hua Tang, Shan Tang, Xiao-liang Chen contributed equally to writing, Shi Zhang, Yong Xiong, Rong Chen contributed equally to design figures and tables, Wei Li, Hui-min Liu,Zhong-yuan Xia, Qing-tao Meng equally to modify.
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 81671948].
Ethical approval
No, the type of manuscript is review.
Research Registration Unique Identifying Number (UIN)
1Name of the registry.
2Unique Identifying number or registration ID.
3Hyperlink to your specific registration (must be publicly accessible and will be checked).
Guarantor
Qing-tao Meng.
Ling-hua Tang.
Declaration of competing interest
The authors declare no competing interests.
References
- 1.World Health Organization WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/ Available at.
- 2.Petersen E., Hui D., Hamer D.H., Blumberg L., Madoff L.C., Pollack M. Li Wenliang, a face to the frontline healthcare worker. The first doctor to notify the emergence of the SARS-CoV-2, (COVID-19), outbreak. Int. J. Infect. Dis. 2020;93:205–207. doi: 10.1016/j.ijid.2020.02.052. [Editorial] 2020-03-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30129-8. [Journal Article; Review] 2020-03-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Tawfiq J.A. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19) Trav. Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101608. [Journal Article] 2020-02-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li P., Fu J.B., Li K.F., Chen Y., Wang H.L., Liu L.J. Transmission of COVID-19 in the terminal stage of incubation period: a familial cluster. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.027. [Journal Article] 2020-03-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen T.Y., Lai H.W., Hou I.L., Lin C.H., Chen M.K., Chou C.C. Buffer areas in emergency department to handle potential COVID-19 community infection in Taiwan. Trav. Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101635. [Letter] 2020-03-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou X., Li Y., Li T., Zhang W. Follow-up of the asymptomatic patients with SARS-CoV-2 infection. Clin. Microbiol. Infect. 2020 doi: 10.1016/j.cmi.2020.03.024. [Letter] 2020-03-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ling Z., Xu X., Gan Q., Zhang L., Luo L., Tang X. Asymptomatic SARS-CoV-2 infected patients with persistent negative CT findings. Eur. J. Radiol. 2020:126. doi: 10.1016/j.ejrad.2020.108956. [Letter] 2020-03-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J.F. China at "crucial stage" to control novel coronavirus, experts say. http://english.cctv.com/2020/01/22/ARTIUwB4aawKly16HkIWPa3U200122.shtml Available at. 19 May 2020.
- 10.National Health Commission of the People’s Republic of China Wuhan to provide over 10,000 hospital beds for viral pneumonia patients: official. http://www.xinhuanet.com/english/2020-01/28/c_138739273.htm Available at.
- 11.Zhang H.F., Bo L., Lin Y., Li F.X., Sun S., Lin H.B. Response of Chinese anesthesiologists to the COVID-19 outbreak. Anesthesiology. 2020 doi: 10.1097/ALN.0000000000003300. [Journal Article] 2020-03-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Council of Nurses ICN calls for data on healthcare worker infection rates and deaths. https://www.icn.ch/news/icn-calls-data-healthcare-worker-infection-rates-and-deaths Available at.
- 13.Robert Koch institute Aktueller Lage-/Situations bericht des RKI zu COVID-19. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-05-13-de.pdf?__blob=publicationFile Available at.
- 14.Epidemiology for public health Integrated surveillance of COVID-19 in Italy. https://www.epicentro.iss.it/en/coronavirus/bollettino/Infografica_13maggio%20ENG.pdf Available at.
- 15.Ministerio de Sanidad, Consumo y Bienestar Social Informe sobre la situación de COVID-19 en España. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/Informe%20n%C2%BA%2030.%20Situaci%C3%B3n%20de%20COVID-19%20en%20Espa%C3%B1a%20a%2011%20de%20mayo%20de%202020.pdf Available at.
- 16.Centre for Disease Control and Prevention Protecting health care personnel is an urgent focus of the nation's response to COVID-19. https://www.cdc.gov/mmwr/volumes/69/wr/mm6915e6.htm?%20s_cid=mm6915e6_x Available at.
- 17.OECD. Hospital beds. https://data.oecd.org/healtheqt/hospital-beds.htm Available at.
- 18.Li B.H., Liu Z.Y., Li Y.C., Chun L., Xu J.N., Li M. Classification of regional health resources in Hubei Province. Chinese Health Resour. 2019;22:106–110. 2019-09-16. 02. [Google Scholar]
- 19.Zhang J.F. Mass graves, doctors unemployed amid bungled U.S. response to COVID-19. http://english.cctv.com/2020/04/13/ARTIVKORcsdPGLFJafZfOPBm200413.shtml Available at. 19 May 2020.
- 20.World Health Organization Infection prevention and control during health care when COVID-19 is suspected. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 Available at.
- 21.World Health Organization Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19) https://apps.who.int/iris/bitstream/handle/10665/331498/WHO-2019-nCoV-IPCPPE_use-2020.2-eng.pdf Available at.
- 22.Cheng V., Wong S.C., Chuang V., So S., Chen J., Sridhar S. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020 doi: 10.1016/j.jinf.2020.04.024. [Journal Article] 2020-04-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhong Q., Liu Y.Y., Luo Q., Zou Y.F., Jiang H.X, Li H. Spinal anaesthesia for patients with coronavirus disease 2019 and possible transmission rates in anaesthetists: retrospective, single-centre, observational cohort study. Br J Anaesth. 2020 doi: 10.1016/j.bja.2020.03.007. [Journal Article] 2020-03-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qi R., Huang Y.T., Liu J.W., Sun Y., Sun X.F., Han H.J. Global prevalence of asymptomatic norovirus infection: a meta-analysis. Clin. Med. 2018;2–3:50–58. doi: 10.1016/j.eclinm.2018.09.005. [Journal Article] 2018-08-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yu X., Yang R. 2020. COVID-19 Transmission through Asymptomatic Carriers Is a Challenge to Containment. Influenza Other Respir Viruses. [Letter] 2020-04-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qian G., Yang N., Ma A., Wang L., Li G., Chen X. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa316. [Journal Article] 2020-03-23. [DOI] [PMC free article] [PubMed] [Google Scholar]