Abstract
Background
The COVID-19 pandemic has placed an extraordinary strain on healthcare systems across North America. Defining the optimal approach for managing a critically ill COVID-19 patient is rapidly changing. Goal-directed transesophageal echocardiography (TEE) is frequently used by physicians caring for intubated critically ill patients as a reliable imaging modality that is well suited to answer questions at bedside.
Methods
A multidisciplinary (intensive care, critical care cardiology, and emergency medicine) group of experts in point-of-care echocardiography and TEE from the United States and Canada convened to review the available evidence, share experiences, and produce a consensus statement aiming to provide clinicians with a framework to maximize the safety of patients and healthcare providers when considering focused point-of-care TEE in critically ill patients during the COVID-19 pandemic.
Results
Although transthoracic echocardiography can provide the information needed in most patients, there are specific scenarios in which TEE represents the modality of choice. TEE provides acute care clinicians with a goal-directed framework to guide clinical care and represents an ideal modality to evaluate hemodynamic instability during prone ventilation, perform serial evaluations of the lungs, support cardiac arrest resuscitation, and guide veno-venous ECMO cannulation. To aid other clinicians in performing TEE during the COVID-19 pandemic, we describe a set of principles and practical aspects for performing examinations with a focus on the logistics, personnel, and equipment required before, during, and after an examination.
Conclusions
In the right clinical scenario, TEE is a tool that can provide the information needed to deliver the best and safest possible care for the critically ill patients.
Keywords: COVID-19, Novel coronavirus, SARS-CoV-2, Acute respiratory syndrome associated with COVID-19, Transesophageal echocardiography, Point-of-care ultrasound
Abbreviations: AGP, Aerosol-generating procedure; ARDS, Acute respiratory distress syndrome; COVID-19, Coronavirus disease 2019; ECMO, Extracorporeal membrane oxygenation; ICU, Intensive care unit; PE, Pulmonary embolism; SARS-CoV-2, Severe acute respiratory syndrome coronavirus-2; SVC, Superior vena cava; TEE, Transesophageal echocardiography; TELUS, Transesophageal lung ultrasound; TTE, Transthoracic echocardiography
Highlights
-
•
TEE as an invaluable tool for managing the critically ill patient with COVID-19.
-
•
TEE can be useful when adequate TTE windows cannot be obtained.
-
•
TEE can be useful to address hemodynamic instability during prone ventilation.
-
•
TEE allows to perform serial evaluations of the lungs.
-
•
TEE is useful to guide critical care procedures such veno-venous ECMO cannulation.
In December 2019, a novel coronavirus (severe acute respiratory syndrome coronavirus-2 [SARS-CoV-2]) causing novel coronavirus disease 2019 (COVID-19) first appeared in Wuhan, China.1 By April 2020, there were >2.7 million cases worldwide, with nearly 190,000 deaths2 and up to 12% of patients requiring intensive care.3 , 4 Patients with COVID-19 can present with a spectrum of critical illness, including shock, acute respiratory failure, and acute respiratory distress syndrome (ARDS).1 , 5, 6, 7, 8, 9 Given the lack of disease-specific therapy, management of critically ill patients with COVID-19 remains largely supportive. Point-of-care cardiopulmonary ultrasound is a fundamental tool in the evaluation of shock and respiratory failure10 , 11 and has been proposed as an ideal diagnostic modality for patients with COVID-19.12 Although in most patients, transthoracic echocardiography (TTE) can provide the information needed, there are situations in which goal-directed transesophageal echocardiography (TEE) provides superior diagnostic value. In contrast to comprehensive echocardiography, TEE provides acute care clinicians with a goal-directed framework to guide clinical care at the point of care in various clinical scenarios. Common applications of TEE in critically ill patients include assessment of circulatory failure, hemodynamic monitoring, evaluation of unexplained hypoxemia, and cardiac arrest.13, 14, 15 Early data suggest that SARS-CoV-2 is associated with multiple cardiovascular complications, including myocardial dysfunction as well as the presence of a hypercoagulable state, leading to an increased risk for venous thromboembolic events such as pulmonary embolism (PE).16, 17, 18 Although TEE can offer valuable information in the assessment and management of patients with these complications, this modality may carry a heightened risk for viral transmission and should be therefore considered carefully.
The American Society of Echocardiography has published a supplemental consensus statement specifically regarding the use of TEE in the perioperative setting during the COVID-19 pandemic.19 This comprehensive statement provides guidance regarding examination indications, practice protocols, and recommendations for maintaining the safety of clinicians and equipment. The authors emphasize the risk for viral transmission during this procedure and conclude that the benefits must be weighed against the risks. Despite these guidelines, there remains a lack of published guidance for acute care physicians trained in critical care TEE. Unlike the diagnostic work flow, the work flow of the point-of-care echocardiographer is driven entirely by urgent or emergent questions to be answered in real time. We hope our report addresses this information gap, as we use this opportunity to discuss the particularities of critical care TEE during COVID-19.
As a multidisciplinary group of experts in point-of-care echocardiography from the United States and Canada, we convened to review the available evidence, share experiences, and produce a consensus statement aiming to provide clinicians with a framework to maximize the safety of patients and health care providers when considering point-of-care TEE in critically ill patients during the COVID-19 pandemic. We reflect on specific clinical scenarios clinicians across care settings may encounter during this pandemic and discuss strategies for managing patient care. The aim of this article is to inform physicians working in critical care environments who are already trained and competent users of TEE. It is not meant to be a comprehensive review of the use of TEE in critically ill patients but rather a practical framework that can be used by clinicians who are competent in this modality during the management of critically ill patients with COVID-19. This article is not a call to action among acute care physicians to use TEE during the pandemic but rather an effort to assert the ongoing value of this procedure during these times.
Our recommendations focus on principles and practical aspects for clinicians performing examinations during COVID-19, including logistics, personnel, equipment preparation, and safe handling before, during, and after an examination. This article reflects our opinions and has not been commissioned by any professional society.
General Considerations for TEE in Critically Ill Patients
When considering TEE in critically ill patients it is important to note the uniqueness of this population, which requires specific discussion beyond recently published American Society of Echocardiography guidelines for imaging in patients with COVID-19.12 Frequently during the initial evaluation of critically ill patients in the emergency department and intensive care settings, clinical and historical data are limited. In these settings, TEE is performed exclusively on intubated patients when transthoracic echocardiographic images are inadequate or cannot provide needed clinical data. Imaging in this patient population is time sensitive, never elective, and always goal directed to provide information that will influence immediate clinical decision-making.
Given the need for scientific information to guide the safety of clinical practice in this unprecedented situation and the scarcity of procedure-specific data pertaining to the risk for viral transmission with TEE, it makes sense to consider the data available in other similar endoscopic procedures, as some of the same safety principles can be used. Numerous gastroenterology and endoscopy societies have published position statements regarding endoscopic examinations during the COVID-19 pandemic,20 , 21 with upper gastrointestinal endoscopy considered a procedure with a high risk for viral transmission. General recommendations include donning appropriate personal protective equipment, including an N-95 respirator or a powered air-purifying respiratory device and a fluid-resistant gown, limiting staff presence in procedure areas, and assigning senior personnel to perform examinations.22
Aerosolization risks are highest during endoscopy of nonintubated patients. Because TEE is being performed only in intubated patients, the risk is assumed to be much lower. Contact and droplet transmission of the virus remains a concern, given the close physical proximity of patient and provider at the head of the bed. Blood and bodily fluid splash events can occur,23 and secretions from the endotracheal tube and transesophageal probe may be transferred from the provider's hands to local surfaces. For this reason, appropriate personal protective equipment is a priority when performing TEE.
In contrast with comprehensive TEE, goal-directed TEE during resuscitation is performed by a single provider who executes all aspects of the examination, including probe insertion, manipulation, image acquisition, and probe removal. This provider is often the same physician who completed the endotracheal intubation (e.g., an emergency or intensive care physician), thus limiting provider and staff exposure.
Considerations in Specific Applications of Goal-Directed TEE
Cardiac Arrest and Periarrest
Cardiac arrest resuscitation represents a particular challenge in patients with suspected or confirmed COVID-19. Current resuscitation guidelines emphasize the importance of delivering high-quality chest compressions and minimizing interruptions to improve survival and neurological outcomes.24 , 25 However, in the context of the current pandemic, the International Liaison Committee on Resuscitation has provided specific recommendations regarding the infection risk to providers delivering resuscitation and stated the need to carefully balance the benefit of resuscitation interventions with the potential harm from infection to providers.26
TEE has been described as an ideal imaging modality in the management of patients with cardiac arrest. In addition to the same diagnostic and prognostic role provided by TTE (e.g., identification of reversible causes such as cardiac tamponade or PE), TEE also provides several unique advantages that should be considered. During resuscitation, TEE has the potential to optimize the quality of chest compressions by identifying compression of the left ventricular outflow tract,15 , 27 shorten chest compression interruptions,28 and guide resuscitative procedures such as extracorporeal membrane oxygenation (ECMO).29 , 30
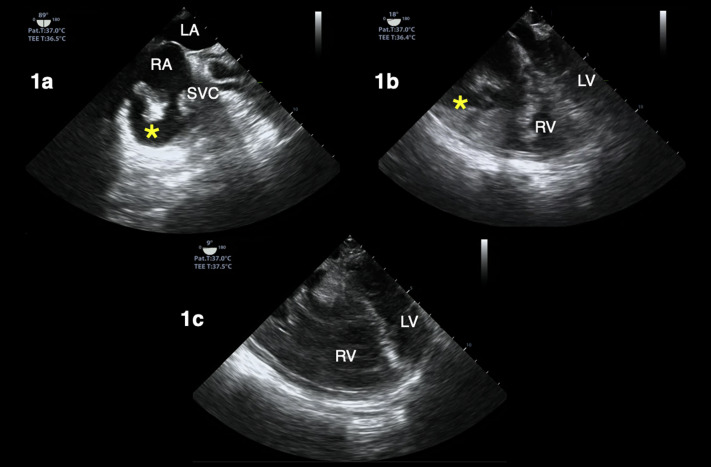
In the case of patients with suspected or confirmed COVID-19, clinicians should carefully consider the potential benefits of this procedure against the risks, specifically to health care providers. The World Health Organization has listed cardiopulmonary resuscitation as an aerosol-generating procedure (AGP). Additionally, endotracheal intubation is a known AGP, and COVID-19 viral particles have been shown to remain viable and infectious for multiple hours in aerosolized form.31 In response, the International Liaison Committee on Resuscitation has advised that providers use personal protective equipment for any AGP during cardiac arrest resuscitation.32 One beneficial aspect of TEE during cardiac arrest is that the transesophageal probe can be left in place throughout the resuscitation, displaying a continuous image of the heart, as opposed to TTE, which requires the provider to remain at the bedside for constant manipulation of the transducer. Figure 1 (see also Supplemental Videos 1 and 2) shows transesophageal echocardiographic images from a goal-directed examination performed by the emergency physician during resuscitation of a patient with COVID-19 who presented in cardiac arrest and was found to have a right atrial thrombus and right ventricular dilation consistent with massive PE as likely cause of the arrest.
Figure 1.
TEE during cardiac arrest resuscitation in a patient with COVID-19. Right atrial thrombus (asterisk) visualized in an off-axis bicaval (A) and a midesophageal four-chamber (B) view, both obtained during ongoing cardiopulmonary resuscitation (CPR). Another midesophageal four-chamber view (C) of same patient shows a dilated right ventricle (RV) and septal deviation during CPR pause, suggesting pulmonary embolism. LA, Left atrium; LV, left ventricle; RA, right atrium.
Evaluation of Shock and Hemodynamic Monitoring
A significant proportion of patients with COVID-19 may develop shock and multiorgan failure.1 , 5 Because there are several shock etiologies in this patient population, it is essential to characterize the primary mechanism of shock, and ultrasound is a key tool to accomplish this goal. Although TTE remains the first-line modality for this assessment in the emergency and intensive care settings, TEE offers a reliable, safe, and powerful alternative for patients in whom transthoracic echocardiographic windows are inadequate or unavailable. In patients with COVID-19 in particular, the high-compliance breathing commonly seen in these patients represents in our experience an additional complicating factor limiting the success acquiring cardiac windows with TTE.
Furthermore, TEE provides an ideal imaging modality to perform serial assessments that are often required in patients with shock or during acute circulatory failure, as it shares most of the properties of an “ideal” hemodynamic monitoring system.33 That is, the indwelling nature of the transducer affords a passive, continuous image for the clinician at the bedside, evaluating anatomic and/or Doppler responses to various hemodynamic interventions.
Specific applications of TEE in the management of critically ill patients include the identification of shock etiology,34 determination of preload sensitivity, and monitoring of hemodynamic interventions.14 The evaluation of patients in shock with TEE has been well described elsewhere, and although it is not necessarily different in the context of patients with COVID-19, there are a few considerations worth noting. On the basis of our experience and in line with the wide spectrum of practice and scalability of critical care echocardiography, the scope of TEE in these patients varies depending on operator skill set and the clinical question(s) at hand. Common applications for which we have used TEE while managing critically ill patients with COVID-19 include characterizing the predominant mechanism of shock, evaluating preload sensitivity using respirophasic variation of superior vena cava (SVC) diameter, and estimating stroke volume and stroke volume variation to assess the effectiveness of interventions (e.g., initiating or titrating vasopressor therapy).
Severe acute respiratory syndrome associated with COVID-19 infection has been found to be more severe in those with obesity,1 , 5 which is precisely the population of patients in whom adequate transthoracic echocardiography images are often limited. patients with COVID-19 in the intensive care unit (ICU) are frequently deeply sedated and paralyzed as part of their ventilation needs. Consequently, the anesthetic considerations with regard to both the consumption of medications in the pandemic as well as the risk of these medications are obviated during the decision-making process to perform TEE.
With respect to the cardiac particularities of COVID-19, an acute COVID-19 cardiovascular syndrome has been reported in some hospitalized patients. This syndrome can manifest with a variety of clinical presentations that include an acute cardiac injury with cardiomyopathy, ventricular arrhythmias, and hemodynamic instability in the absence of obstructive coronary artery disease.35 Despite the great amount of literature speculating on cardiac features of this disease, our experience working in the frontline acute care settings caring for patients with shock and COVID-19 most commonly unveils echocardiographic findings we typically see in other infectious causes of respiratory failure. Namely, these patients are frequently hyperdynamic and have elevated cardiac output. As well as in pre-COVID-19 era descriptions of ARDS,36 right ventricular dilation is seen commonly, especially in those who have been ventilated for ≥1 week, in whom lung compliance changes, leading to increased right heart afterload.
Procedural Guidance
Aside from its powerful value as a diagnostic and hemodynamic monitoring tool, point-of-care TEE also plays a key role during several critical care procedures. In our experience and as extensively described in the literature, echocardiographic assistance is commonly used in a number of emergency procedures, such as initiation and monitoring of ECMO,37 assistance in placement of pulmonary artery catheters,38 placement of intravenous pacemaker wires,39 placement of intra-aortic balloon counterpulsation,40 , 41 and during catheter-directed thrombolytic therapy.42
Recent international guidelines recommend consideration of ECMO in patients with severe respiratory failure from SARS-CoV-2 infection when conventional management fails, if resources and expertise are available.43 As of April 25, 2020, 563 patients with confirmed or suspected COVID-19 have undergone initiation of ECMO and are reported in the Extracorporeal Life Support Organization registry.44 Goal-directed TEE plays an important role in the management of these critically ill patients.37 Before initiating venovenous ECMO support in patients with refractory hypoxemia, an echocardiographic assessment should be performed. Echocardiography may identify unexpected and reversible findings (e.g., cardiac tamponade, PE) or demonstrate severe left ventricular dysfunction, which should prompt consideration of venoarterial ECMO. Severe valvular pathology affecting the success of venovenous or venoarterial ECMO should also be excluded (e.g., severe aortic insufficiency, mitral regurgitation, tricuspid stenosis). Although not relevant for cannulation and ECMO management, detection of patent foramen ovale may affect weaning consideration. Vascular assessment is essential to exclude preexisting complications, such as thrombosis, stenosis, or dissection, and for appropriate selection of type and size of cannulas.37 , 45 Normal variants or embryologic remnants of right heart structures might also affect the appropriate and safe placement of venous cannulas. For example, a prominent Chiari network may impede proper cannula positioning and increase the thrombotic risk. A dilated coronary sinus, as observed in persistent left SVC, may be accidentally cannulated and compromise oxygenation. The presence of pacemaker or defibrillator leads should also be documented.45
During the cannulation process, TEE allows the evaluation of proper guidewire and cannula positioning at the bedside in the ICU. Transesophageal echocardiographic guidance confirms the course of the guidewire to exclude coiling in the right atrium, displacement across the tricuspid valve, crossing the interatrial septum, or entering the carotid sinus.45, 46, 47 Transesophageal echocardiographic guidance can ensure that the return cannula is positioned clear of the tricuspid valve or interatrial septum, ensuring that the access and return cannulas are placed with sufficient distance between them to decrease the risk for recirculation. A dual-lumen bicaval cannula may be used and is placed in the right internal jugular traversing from the SVC to inferior vena cava along the posterior aspect of the right atrium.46, 47, 48
Following cannulation and during support with ECMO, TEE may be required to exclude complications related to venovenous ECMO, as TTE is more limited in its spatial resolution. Such complications include cannula thrombosis, chamber compression from tamponade, or cannula displacement.37 , 45 , 46 During this period TEE can also be used to troubleshoot the development of hypoxemia, including the identification of recirculation, when the tips of the cannulae are located too close together, inadequate ECMO flows due to hypovolemia, and thrombus formation within the cannula.37
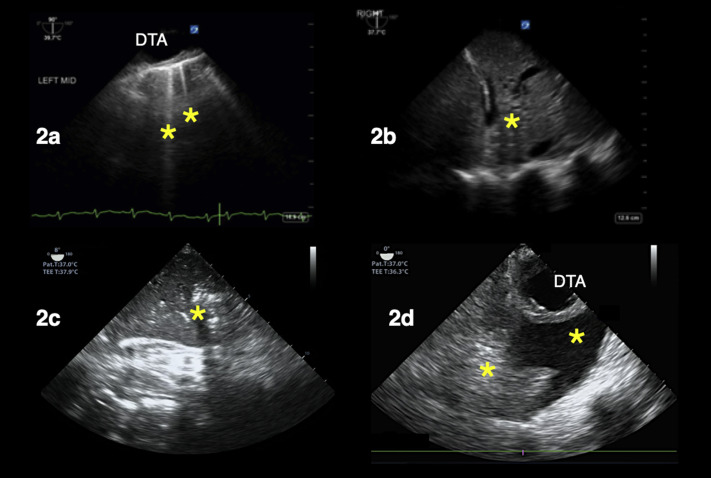
Transesophageal Lung Ultrasound
With increasing use of both TEE in the resuscitative setting as well as lung ultrasound, it has become apparent that these approaches may be effectively combined. In particular, the use of TEE to image the lungs, so-called transesophageal lung ultrasound (TELUS), has been increasingly used in the ICU environment after being initially described in the operative environment.49 This application is rarely if ever indicated on its own in the critical care environment but rather as an extension of the TEE examination providing a complete cardiopulmonary assessment, hence increasing the value of this modality. One of the benefits of imaging the lungs from within the esophagus, a relatively posterior location compared with transthoracic lung ultrasound technique, is its effectiveness at visualizing the more dependent regions of the lung. These regions are typically very difficult to visualize in a supine critically ill patient using a surface approach yet, if densely occupied with alveolar disease or atelectasis (manifest as consolidation pattern), may contribute to life-threatening respiratory failure. Furthermore, just as with TEE, TELUS affords lung imaging in those with difficult transthoracic windows: obese patients, those with surgical dressings, and those with subcutaneous emphysema in particular. Although recruitment maneuvers to open a collapsed lung are not routinely recommended in patients with ARDS,50 in our practice targeted recruitment maneuvers still have a role, specifically when atelectatic or consolidated lung is identified. Although it should be noted that the artifacts that form the basis of lung ultrasonography have not been validated in TEE but rather extrapolated from transthoracic ultrasound,49 the use TELUS in some of these selected cases has allowed us to have immediate and real-time feedback on recruitability of the lung. Figure 2 shows examples of TELUS examinations performed by the intensivist during the evaluation of patients with hypoxemia in the ICU during the COVID-19 pandemic.
Figure 2.
TELUS of patients with hypoxemia in the intensive care unit (A,B) and emergency department (C,D). (A) Sagittal plane view of the left lung shows B-lines (asterisk) suggesting increased extravascular lung water. Panels (B) and (C) correspond to sagittal-plane views of the right costophrenic angle showing consolidation pattern (asterisk) suggestive of atelectasis versus pneumonia. In (D), an axial-plane view of the left lung shows an atelectatic lung (left asterisk) and pleural effusion (right asterisk). DTA, Descending thoracic aorta.
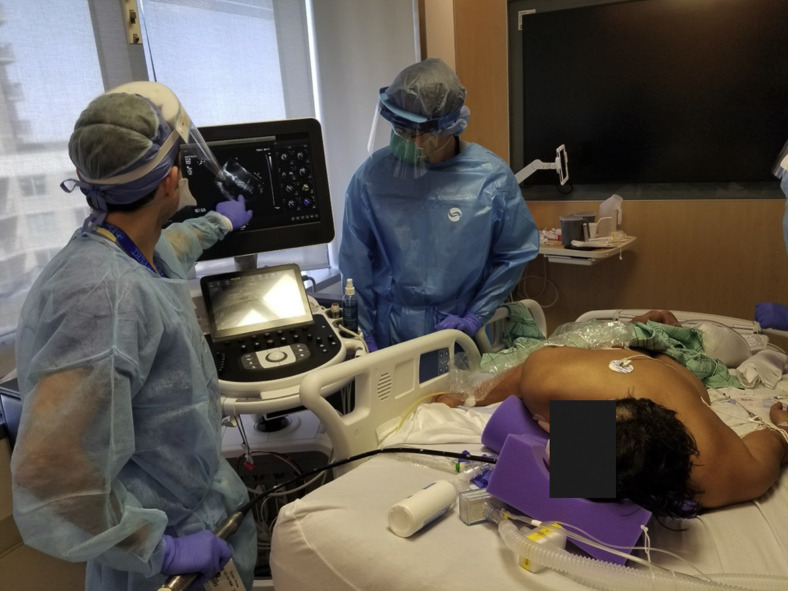
Use of TEE in Prone Patients
Prone positioning ventilation is known to improve ventilation-perfusion matching and dorsal alveolar recruitment and has been associated with improved survival in some patients with ARDS.51 Recent international guidelines for the management of critically ill patients with COVID-19 have recommended the use of prone ventilation for 12 to 16 hours in mechanically ventilated adults with moderate to severe ARDS.52 A distinguishing advantage of TEE is that it is well suited to be performed in patients during prone ventilation.53 , 54 We have performed TEE on prone patients on several occasions. The indication is usually that the patient is too hypoxemic and unstable to unprone. There is usually an urgent need for TEE to evaluate left ventricular function, for instance, when titrating up positive end-expiratory pressure or when there is concern about the size and function of the right ventricle to tolerate recruitment maneuvers when there is evidence of atelectasis. This is also the case as part of the evaluation for ECMO in patients who remain hypoxemic in prone ventilation, and the decision for venovenous or venoarterial ECMO is being considered. The logistical concern is obvious, but the real issue is only with the actual insertion of the probe into the esophagus; once that is achieved, the rest of the examination is the same as the usual transesophageal echocardiographic examination. To successfully accomplish transesophageal probe insertion on a prone patient, we have found helpful to turn the patient partially on his or her side and introduce the probe while maintaining alignment of the head and chest. The patient is then returned to the prone position, with the exception of the head and neck, which will remain facing the examiner while the probe is in place. In our group's experience, it is fairly easy to perform TEE in these patients with the proper technique, as they can remain prone throughout the course of the examination. We have found that TEE in prone patients has been particularly helpful during the COVID-19 pandemic, given the degree of hypoxemia seen in these patients and the many urgent ECMO evaluations we have had to perform. With that said, it should be noted that TEE will always be easier in the supine position and should therefore be performed in the prone position only when the information required is needed urgently enough, as in the situations just described, that the examination cannot wait until the patient is back to the supine position. Figure 3 shows two of the authors performing a point-of-care transesophageal echocardiographic examination during hemodynamic decompensation of a patient in prone ventilation.
Figure 3.
Performance of point-of-care TEE with patient in the prone position.
Principles Recommended for Clinicians Performing Goal-Directed TEE during COVID-19
On the basis of the available evidence and our group's multi-institutional and interdisciplinary collective experience working in the frontlines of the pandemic, we have generated a set of principles and practical aspects for clinicians performing examinations during COVID-19 with focus on the logistics, personnel, and equipment before, during, and after an examination. These practical recommendations are summarized in Table 1 . We recommend that the use of TEE in this setting be planned at the system level rather than the provider or department level, with a multidisciplinary approach that involves not only those performing the studies at the bedside but also those involved in all related tasks necessary for the examinations to be performed (e.g., central processing department, transport, technicians). Similar to other high-risk procedures performed routinely (e.g., endotracheal intubation), we also recommend that clinical teams have preestablished protocols in place and consider the use of in situ simulation to familiarize pertinent staff with the steps needed to maximize safety during this procedure. Additionally, to minimize risk during the procedure, the length should be limited to the minimum required to acquire the images needed in the goal-directed examination. During the examination, images and loops should be recorded and stored for further review after the examination is completed.
Table 1.
Summary of recommendations for clinicians performing goal-directed TEE during the COVID-19 pandemic
Preparation (before procedure)
|
During the procedure
|
After the procedure
|
AIIR, Airborne infection isolation room; PAPR, powered air-purifying respirator.
We are aware that the echocardiographic evaluation of dynamic hemodynamic parameters such as respirophasic variation of the SVC and velocity-time integral has not been validated in patients with ARDS in the context of COVID-19. Nevertheless, on the basis of our experience, if these are required as part of the goals of TEE, we recommend that the patient be paralyzed for a short duration to optimize the conditions of the examination and the reliability of these parameters. Although providers should be aware of the potential hazards associated with paralysis and deep sedation, in the context of COVID-19 infection, paralytics given before insertion of the transesophageal probe have the potential minimize the chance of viral aerosolization if the intubated patient gags or moves.
Similar to other endoscopic devices, high-level disinfection must be performed on all transesophageal echocardiographic transducers between each use.55 A hospital-based protocol should be in place to ensure that transesophageal probes are disinfected in a standard manner. The ultrasound system must also be cleaned, as emerging data suggest that SARS-CoV-2 can be present on surfaces for a number of days.31 Clinicians should refer to the current US Environmental Protection Agency list of recommended cleansing products and wipe down the entire ultrasound system in between each patient use.56 This includes the ultrasound screen, keyboard, cart, and so on.
Should Point-of-Care TEE Be Used in Critically Ill Patients during the COVID-19 Outbreak?
In our group's opinion, decisions regarding the use of TEE in critically ill patients should be made by individual clinicians and their hospitals and/or clinical units, while also considering the factors mentioned earlier, local resource availability, and experience. Rather than establishing one-size-fits-all regulations or policies, we recommend assessing the use of TEE on a case-by-case basis; if TEE is the tool that can provide the information needed to deliver the best and safest possible care for the patient for any of the applications described here, then TEE should be considered.
Conclusion
As resources are stretched in a pandemic scenario, the use of procedures and tools that promote efficiency and accuracy must be maximized. As such, despite plausibility as an AGP, our group of experts from across North America strongly endorses TEE as an invaluable tool for managing critically ill patients with COVID-19. The value of TEE in this pandemic is seen in familiar domains, such as patients in whom adequate transthoracic echocardiographic windows cannot be generated, as well as specific scenarios that we have encountered frequently in the context of the COVID-19. This includes the increased need to address hemodynamic instability during prone ventilation, to perform serial evaluations of the lungs, during cardiac arrest resuscitation, and to guide venovenous ECMO cannulation.
Footnotes
Dr. Teran has received consulting honoraria payments from Fujifilm Sonosite and Philips Healthcare for participation in educational events and expert panels related to point-of-care ultrasound, including transesophageal echocardiography, and he is the owner of ResusMedX. Dr. Koenig has received consulting honoraria from Fujifilm Sonosite for an educational lecture on transesophageal echocardiography in critical care during the 2019 annual meeting of the American College of Chest Physicians. Dr. Arntfield has received consulting honoraria payments from Philips Healthcare and Fujifilm Sonosite and is a member of the medical advisory boards for EchoNous and Vave Health. The views expressed in this document are those of the author (s) and do not reflect the official policy of the US Department of the Army, the US Department of Defense, or the US government.
Conflicts of Interest: None.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.echo.2020.05.022.
Supplementary Data
TEE during cardiac arrest resuscitation in a patient with COVID-19. A right atrial thrombus is visualized in an off-axis bicaval view obtained during ongoing cardiopulmonary resuscitation.
TEE during cardiac arrest resuscitation in a patient with COVID-19. A right atrial thrombus is visualized in the midesophageal four-chamber view obtained during ongoing cardiopulmonary resuscitation.
References
- 1.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization Coronavirus disease 2019 (COVID-19): situation report—69. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200329-sitrep-69-covid-19.pdf?sfvrsn=8d6620fa_8 Available at:
- 3.Grasselli G., Pesenti A., Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. https://jamanetwork.com/journals/jama/fullarticle/2763188 Available at: [DOI] [PubMed]
- 4.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:P475–P481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arentz M., Eric Y., Lindy K., Lokhandwala S., Riedo F., Chong M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spencer K.T., Kimura B.J., Korcarz C.E., Pellikka P.A., Rahko P.S., Siegel R.J. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26:567–581. doi: 10.1016/j.echo.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Narasimhan M., Koenig S.J., Mayo P.H. Advanced echocardiography for the critical care physician: part 2. Chest. 2014;145:135–142. doi: 10.1378/chest.12-2442. [DOI] [PubMed] [Google Scholar]
- 12.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Soc Echocardiogr. 2020;00 doi: 10.1016/j.echo.2020.04.001. 000-000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mayo P.H., Narasimhan M., Koenig S. Critical care transesophageal echocardiography. Chest. 2015;148:1323–1332. doi: 10.1378/chest.15-0260. [DOI] [PubMed] [Google Scholar]
- 14.Arntfield R., Lau V., Landry Y., Priestap F., Ball I. Impact of critical care transesophageal echocardiography in medical–surgical ICU patients: characteristics and results from 274 consecutive examinations. J Intensive Care Med. 2020 doi: 10.1177/0885066618797271. In press. [DOI] [PubMed] [Google Scholar]
- 15.Teran F., Dean A.J., Centeno C., Panebianco N.L., Zeidan A.J., Chan W. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140–147. doi: 10.1016/j.resuscitation.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 16.Long B., Brady W.J., Koyfman A., Gottlieb M. Cardiovascular complications in COVID-19. Am J Emerg Med. https://www.ajemjournal.com/article/S0735-6757(20)30277-1/pdf Available at: [DOI] [PMC free article] [PubMed]
- 17.Xie Y., Wang X., Yang P., Zhang S. COVID-19 complicated by acute pulmonary embolism. Radiol Cardiothorac Imaging. 2020;2:e200067. doi: 10.1148/ryct.2020200067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Danzi G.B., Loffi M., Galeazzi G., Gherbesi E. Acute pulmonary embolism and COVID-19 pneumonia: a random association? Eur Heart J. 2020;41:1858. doi: 10.1093/eurheartj/ehaa254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nicoara A., Maldonado Y., Kort S., Swaminathan M., Mackensen G.B. Specific considerations for the protection of patients and echocardiography service providers when performing perioperative or periprocedural transesophageal echocardiography during the 2019 novel coronavirus outbreak: Council on Perioperative Echocardiography supplement to the statement of the American Society of Echocardiography. J Am Soc Echocardiogr. 2020;00 doi: 10.1016/j.echo.2020.04.008. 000-000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gralnek I.M., Hassan C., Beilenhoff U., Antonelli G., Ebigbo A., Pellisè M. ESGE and ESGENA position statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020. https://www.esge.com/esge-and-esgena-position-statement-on-gastrointestinal-endoscopy-and-the-covid-19-pandemic/ 52. 2020. Available at: [DOI] [PMC free article] [PubMed]
- 21.Soetikno R., Teoh A.Y., Kaltenbach T., Lau J.Y., Asokkumar R., Cabral-Prodigalidad P. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. https://www.giejournal.org/article/S0016-5107(20)34033-5/fulltext Available at: [DOI] [PMC free article] [PubMed]
- 22.Lui R.N., Wong S.H., Sánchez-Luna S.A., Pellino G., Bollipo S., Wong M.-Y. Overview of guidance for endoscopy during the coronavirus disease 2019 pandemic. J Gastroenterol Hepatol. 2020;35:749–759. doi: 10.1111/jgh.15053. [DOI] [PubMed] [Google Scholar]
- 23.Johnston E.R., Habib-Bein N., Dueker J.M., Quiroz B., Corsaro E., Ambrogio M. Risk of bacterial exposure to the endoscopist’s face during endoscopy. Gastrointest Endosc. 2019;89:818–824. doi: 10.1016/j.gie.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 24.Nolan J., Ornato J., Parr M., Perkins G., Soar J. Resuscitation highlights in 2014. Resuscitation. 2015;89:A1–A6. doi: 10.1016/j.resuscitation.2015.01.027. [DOI] [PubMed] [Google Scholar]
- 25.Kleinman M.E., Goldberger Z.D., Rea T., Swor R.A., Bobrow B.J., Brennan E.E. 2017 American Heart Association focused update on adult basic life support and cardiopulmonary resuscitation quality: an update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2018;137:e7–e13. doi: 10.1161/CIR.0000000000000539. [DOI] [PubMed] [Google Scholar]
- 26.Couper K., Taylor-Phillips S., Grove A., Freeman K., Osokogu O., Court R. International Liaison Committee on Resuscitation; Brussels, Belgium: 2020. COVID-19 infection risk to rescuers from patients in cardiac arrest. Consensus on science with treatment recommendations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Catena E., Ottolina D., Fossali T., Rech R., Borghi B., Perotti A. Association between left ventricular outflow tract opening and successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8–14. doi: 10.1016/j.resuscitation.2019.02.027. [DOI] [PubMed] [Google Scholar]
- 28.Fair J., Mallin M.P., Adler A., Ockerse P., Steenblick J., Tonna J. Transesophageal echocardiography during cardiopulmonary resuscitation is associated with shorter compression pauses compared with transthoracic echocardiography. Ann Emerg Med. 2019;73:610–616. doi: 10.1016/j.annemergmed.2019.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arntfield R., Pace J., McLeod S., Granton J., Hegazy A., Lingard L. Focused transesophageal echocardiography for emergency physicians-description and results from simulation training of a structured four-view examination. Crit Ultrasound J. 2015;7:27. doi: 10.1186/s13089-015-0027-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fair J., Tonna J., Ockerse P., Galovic B., Youngquist S., McKellar S. Emergency physician-performed transesophageal echocardiography for extracorporeal life support vascular cannula placement. Am J Emerg Med. 2016;34:1637–1639. doi: 10.1016/j.ajem.2016.06.038. [DOI] [PubMed] [Google Scholar]
- 31.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization WHO interim guidelines. Vol. 6, infection prevention and control of epidemic- and pandemic-prone acute respiratory diseases in health care. http://www.who.int/csr/resources/publications/WHO_CDS_EPR_2007_6c.pdf Available at: [PubMed]
- 33.Vignon P., Merz T.M., Vieillard-Baron A. Ten reasons for performing hemodynamic monitoring using transesophageal echocardiography. Intensive Care Med. 2017;43:1048–1051. doi: 10.1007/s00134-017-4716-1. [DOI] [PubMed] [Google Scholar]
- 34.Vignon P., Mentec H., Terre S., Gastinne H., Gueret P., Lemaire F. Diagnostic accuracy and therapeutic impact of transthoracic and transesophageal echocardiography in mechanically ventilated patients in the ICU. Chest. 1994;106:1829–1834. doi: 10.1378/chest.106.6.1829. [DOI] [PubMed] [Google Scholar]
- 35.Hendren N.S., Drazner M.H., Bozkurt B., Cooper L.T., Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.047349 Available at: [DOI] [PMC free article] [PubMed]
- 36.Vieillard-Baron A., Price L.C., Matthay M.A. Acute cor pulmonale in ARDS. Intensive Care Med. 2013;39:1836–1838. doi: 10.1007/s00134-013-3045-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Douflé G., Roscoe A., Billia F., Fan E. Echocardiography for adult patients supported with extracorporeal membrane oxygenation. Crit Care. 2015;19:1–10. doi: 10.1186/s13054-015-1042-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cronin B., Robbins R., Maus T. Pulmonary artery catheter placement using transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2017;31:178–183. doi: 10.1053/j.jvca.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 39.Lerner R.P., Haaland A., Lin J. Temporary transvenous pacer placement under transesophageal echocardiogram guidance in the emergency department. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2019.12.027. In press. [DOI] [PubMed] [Google Scholar]
- 40.Nishioka T., Friedman A., Cercek B., Chaux A., Luo H., Berglund H. Usefulness of transesophageal echocardiography for positioning the intraaortic balloon pump in the operating room. Am J Cardiol. 1996;77:105–106. doi: 10.1016/s0002-9149(97)89148-5. [DOI] [PubMed] [Google Scholar]
- 41.Klopman M.A., Chen E.P., Sniecinski R.M. Positioning an intraaortic balloon pump using intraoperative transesophageal echocardiogram guidance. Anesth Analg. 2011;113:40–43. doi: 10.1213/ANE.0b013e3182140b9a. [DOI] [PubMed] [Google Scholar]
- 42.Miller S.D., Lee D.C., Dollar B.T., Schepel S.R., Shestopalov A., Culp W.C. Transesophageal echocardiography guidance for atrial-caval thrombus removal with the AngioVac system. Baylor Univ Med Cent Proc. 2020;33:85–86. doi: 10.1080/08998280.2019.1673920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Extracorporeal Life Support Organization ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. https://www.elso.org/COVID19.aspx Available at:
- 44.Extracorporeal Life Support Organization COVID-19 cases on ECMO in the ELSO registry. https://www.elso.org/Default.aspx?TabID=576 Available at:
- 45.Platts D.G., Sedgwick J.F., Burstow D.J., Mullany D.V., Fraser J.F. The role of echocardiography in the management of patients supported by extracorporeal membrane oxygenation. J Am Soc Echocardiogr. 2012;25:131–141. doi: 10.1016/j.echo.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 46.Griffee M.J., Zimmerman J.M., McKellar S.H., Tonna J.E. Echocardiography-guided dual-lumen venovenous extracorporeal membrane oxygenation cannula placement in the ICU—a retrospective review. J Cardiothorac Vasc Anesth. 2020;34:698–705. doi: 10.1053/j.jvca.2019.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cianchi G., Lazzeri C., Bonizzoli M., Batacchi S., Peris A. Echo-guided insertion of a dual-lumen cannula for venovenous extracorporeal membrane oxygenation. ASAIO J. 2019;65:414–416. doi: 10.1097/MAT.0000000000000826. [DOI] [PubMed] [Google Scholar]
- 48.Banfi C., Pozzi M., Siegenthaler N., Brunner M.E., Tassaux D., Obadia J.F. Veno-venous extracorporeal membrane oxygenation: cannulation techniques. J Thorac Dis. 2016;8:3762–3773. doi: 10.21037/jtd.2016.12.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cavayas Y.A., Girard M., Desjardins G., Denault A.Y. Transesophageal lung ultrasonography: a novel technique for investigating hypoxemia. Can J Anesth. 2016;63:1266–1276. doi: 10.1007/s12630-016-0702-2. [DOI] [PubMed] [Google Scholar]
- 50.Cavalcanti A.B., Suzumura É.A., Laranjeira L.N., de Moraes Paisani D., Damiani L.P., Guimaraes H.P. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA. 2017;318:1335–1345. doi: 10.1001/jama.2017.14171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guérin C., Reignier J., Richard J.C., Beuret P., Gacouin A., Boulain T. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 52.Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19) Intensive Care Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mekontso Dessap A., Proost O., Boissier F., Louis B., Roche Campo F., Brochard L. Transesophageal echocardiography in prone position during severe acute respiratory distress syndrome. Intensive Care Med. 2011;37:430–434. doi: 10.1007/s00134-010-2114-z. [DOI] [PubMed] [Google Scholar]
- 54.Guarracino F. Transoesophageal echocardiography during prone positioning for ARDS: watching the heart to care for the lung. Intensive Care Med. 2011;37:380–381. doi: 10.1007/s00134-010-2119-7. [DOI] [PubMed] [Google Scholar]
- 55.Rutala W.A., Weber D.J. Guideline for disinfection and sterilization in healthcare facilities. https://www.cdc.gov/infectioncontrol/guidelines/disinfection/ Available at:
- 56.US Environmental Protection Agency List N: disinfectants for use against SARS-CoV-2. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2 Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TEE during cardiac arrest resuscitation in a patient with COVID-19. A right atrial thrombus is visualized in an off-axis bicaval view obtained during ongoing cardiopulmonary resuscitation.
TEE during cardiac arrest resuscitation in a patient with COVID-19. A right atrial thrombus is visualized in the midesophageal four-chamber view obtained during ongoing cardiopulmonary resuscitation.