Abstract
Coronavirus disease 19 (COVID-19) is an emerging infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In this scenario, managing acute medical conditions, such as stroke, requires a timely treatment together with proper strategies that minimize the risk of infection spreading to health care workers and other patients. We report the case of a 79-year-old woman, who was admitted for a wake-up stroke due to occlusion of the left middle cerebral artery. She was treated outside the COVID-19-dedicated track of the hospital because she had no concomitant signs or symptoms suggestive of SARS-CoV-2 infection nor recent contact with other infected individuals. Post-mortem nasal and pharyngeal swab was positive for SARS-CoV-2 infection.
We propose that hyperacute stroke patients should be tested for SARS-CoV-2 infection at admission and then managed as having COVID-19 until cleared by a negative result. We are aware that such measure results in some delay of the acute treatment of stroke, which could be minimal using well-exercised containment protocols.
Keywords: Stroke, COVID-19, severe acute respiratory syndrome coronavirus 2, Sars-CoV-2, stroke management
Case report
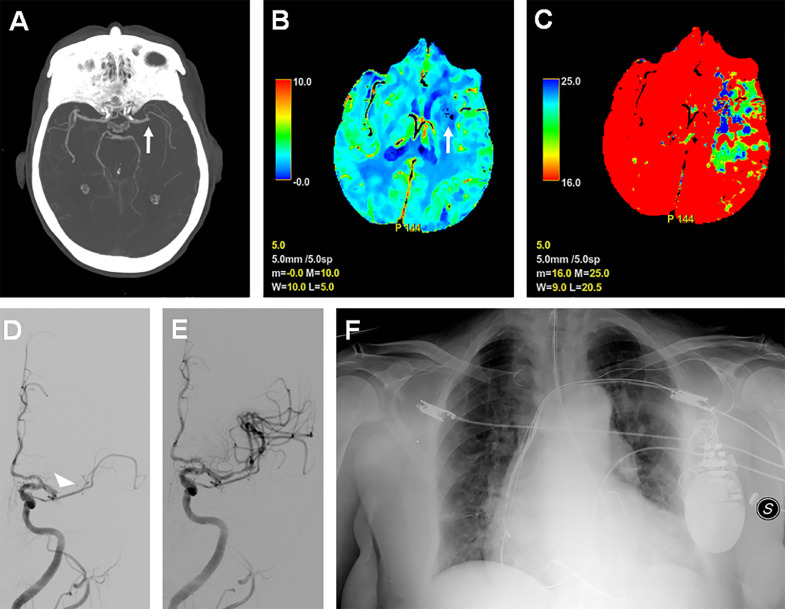
A 79-year-old woman, with a history of atrial fibrillation, hypertension, ischemic heart disease and type 2 diabetes, was admitted in the emergency room for a wake-up stroke. The NIH Stroke Scale score was 24. She had no concomitant clinical symptoms or epidemiological links suggestive of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and therefore she was managed outside of the Coronavirus disease 19 (COVID-19) dedicated track. The brain CT protocol for acute stroke, performed within 20 minutes from arrival, showed left middle cerebral artery occlusion (Fig. 1 A) and a large area of ischemic penumbra (Figs. 1B-C). The patient underwent successful thrombectomy 90 minutes after admittance (Figs. 1D-E). During the following days she received oxygen supplementation to correct slight hypoxemia but she never had fever or tachipnoea. A frontal chest radiography showed bilateral and predominantly basal interstitial lung disease (Fig. 1F). Laboratory tests were unremarkable. Transthoracic echocardiography documented reduced ejection fraction and left ventricular apical akinesia. Four days after hospitalization the patient died of cardiac arrest. Post-mortem nasal and pharyngeal swab revealed SARS-CoV-2 infection. All the health care workers who had come in contact with the patient were tested for SARS-CoV-2 infection and the Stroke Unit continued to operate after sanitation.
Fig. 1.
A) Axial maximum intensity projection reconstruction of brain CT-angiography showing left middle cerebral artery occlusion (white arrow). B-C) Axial brain CT perfusion study showing a small area of reduced cerebral blood volume in left basal ganglia (B), representing a small ischemic core volume (B, arrow), and a large area of prolonged mean transit time involving the left areas of temporal, frontal and parietal lobes (Tmax 16:25) (C); overall, this suggests the presence of a large area of ischemic penumbra. D-E) Cerebral angiography performed before (D) and after mechanical thrombectomy (E), showing at first left middle cerebral artery occlusion (D, white arrowhead) and complete vessel recanalization following the endovascular procedure (E), respectively. F) Frontal chest radiography showing lung bilateral interstitial involvement, predominantly in the lower lobes, and cardiac silhouette enlargement.
Discussion
COVID-19 is an emerging infectious disease caused by SARS-CoV-2, whose clinical spectrum ranges from asymptomatic cases to severe distress respiratory syndrome.1 , 2 Acute stroke has been reported in COVID-19 patients,3 , 4 although rarely as presenting feature.5 A managing algorithm called “Protected Code Stroke”, based on epidemiological links and the presence of signs and symptoms of COVID-19, has been proposed for stroke patients to define efficient containment measures.6 However, as seen in our patient, this strategy may fail. This can happen in asymptomatic COVID-19 cases or in older patients whose comorbidities may camouflage clinical and radiological findings of COVID-19. Our patient lacked epidemiologic, clinical and laboratory data of an ongoing SARS-CoV-2 infection. Chest radiography showed only signs of interstitial lung involvement but not ground-glass opacities that are common in SARS-CoV-2 pneumonia.7
Overall, we are witnessing a raising challenge in SARS-CoV-2 containment while managing time-dependent disorders such as stroke. In areas with high COVID-19 prevalence, it is reasonable to test stroke patients for SARS-CoV-2 at admission and manage them as suspected until cleared by a negative result. Also, chest CT scan has been shown valuable to detect asymptomatic and milder cases and is now routinely performed, immediately before brain scan, in our hospital as well as in others.8 We are aware that such measures result in delays between recognition, diagnosis and treatment that could be minimized with well-exercised containment protocols.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Jama. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Tawfiq J.A. Asymptomatic coronavirus infection: MERS-CoV and SARS-CoV-2 (COVID-19) Travel Med Inf Dis. 2020;35 doi: 10.1016/j.tmaid.2020.101608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 infection. New Eng J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oxley T.J., Mocco J., Majidi S. Large-vessel stroke as a presenting feature of covid-19 in the Young. New Eng J Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Avula A., Nalleballe K., Narula N. COVID-19 presenting as stroke. Brain Behav Immunity. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khosravani H., Rajendram P., Notario L., Chapman M.G., Menon B.K. Protected code stroke: hyperacute stroke management during the coronavirus disease 2019 (COVID-19) pandemic. Stroke. 2020;51:1891–1895. doi: 10.1161/STROKEAHA.120.029838. Strokeaha120029838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong H.Y.F., Lam H.Y.S., Fong A.H. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019 doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodriguez-Pardo J., Fuentes B., Alonso de Lecinana M. Acute stroke care during the COVID-19 pandemic. Ictus madrid program recommendations. Neurologia (Barcelona, Spain) 2020;35:258–263. doi: 10.1016/j.nrl.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]