Since the coronavirus disease of 2019 (COVID-19) was first identified in December 2019 in Wuhan, China, and declared a pandemic, it has harvested thousands of lives across the globe.1 Aside from respiratory disease, COVID-19 has been shown to increase risk of thromboembolism.2 Multiple hemostatic abnormalities, including increased D-dimer and fibrin degradation product levels, prolonged thrombin and prothrombin times and international normalized ratio, shortened activated partial thromboplastin time, and thrombocytopenia, indicating possible disseminated intravascular coagulation, have been reported.1, 2, 3, 4, 5 In addition, other implicated causes include positive antiphospholipid antibodies and sepsis.4
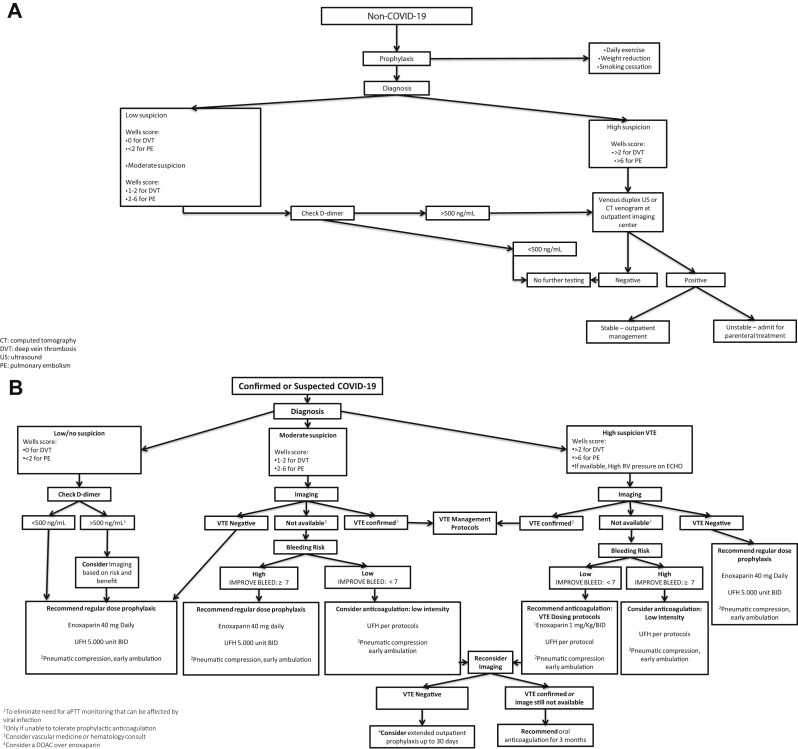
With the current recommendations of social distancing and “stay-at-home” orders, most clinical appointments have been changed into virtual visits. Furthermore, patients with potentially serious conditions, such as venous thromboembolism (VTE), might be avoiding hospital visits, which may lead to increased morbidity and mortality. Sedentary lifestyle is expected to increase risk of VTE, especially in patients with underlying risk factors. Consequently, consistent with current evidence,5 our institution has created management recommendations for VTE (Fig ).
Fig.
Management recommendations for venous thromboembolism (VTE) of non-COVID patients (A) and patients with confirmed or suspected COVID-19 (B). aPTT, Activated partial thromboplastin time; BID, twice daily; CT, computed tomography; DOAC, direct-acting oral anticoagulant; DVT, deep venous thrombosis; PE, pulmonary embolism; RV, right ventricle; UFH, unfractionated heparin; US, ultrasound.
Non-COVID patients
Prophylaxis
We recommend daily exercise activities, weight reduction, and smoking cessation.
Diagnosis
For outpatients with low risk (Wells score of 0 for deep venous thrombosis [DVT] and <2 for pulmonary embolism [PE]) or moderate risk (Wells score of 1-2 for DVT and 2-6 for PE) and D-dimer level of <500 ng/mL, we recommend no further testing. For moderate-risk patients and D-dimer level of ≥500 ng/mL or high-risk patients (Wells score of >2 for DVT and >6 for PE), we recommend venous duplex ultrasound or computed tomography at an outpatient imaging center.
Management
For stable patients, we recommend outpatient management with direct oral anticoagulants, and inpatient management with parenteral anticoagulation for unstable cases.
COVID-19 patients
Prophylaxis
In addition to early ambulation, we recommend prophylaxis for all patients, favoring enoxaparin over unfractionated heparin.
Diagnosis
Based on clinical suspicion, and D-dimer level in patients with low risk, we cautiously suggest imaging studies in order to reduce viral transmission and interruption of intensive care.
Management
We recommend prophylaxis, low- or regular-intensity full anticoagulation based on imaging availability and bleeding risk. We favor enoxaparin over unfractionated heparin to reduce the need for monitoring of activated partial thromboplastin time, which can be affected by the viral infection. Direct oral anticoagulants may be considered in patients who do not require a procedure.
Extended prophylaxis
Extended prophylaxis is considered in patients with moderate clinical suspicion and low bleeding risk.
Further research is needed for standardized management recommendations for VTE in the era of COVID-19.
References
- 1.World Health Organization Director-General's remarks at the media briefing on 2019-nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 Available at:
- 2.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gao Y., Li T., Han M., Li X., Wu D., Xu Y. Diagnostic utility of clinical laboratory data determinations for patients with the severe COVID-19. J Med Virol. 2020;92:791–796. doi: 10.1002/jmv.25770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Y., Xiao M., Zhang S., Xia P., Cao W., Jiang W. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med. 2020;82:e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]