Abstract
Skilled nursing facilities (SNFs) have emerged as an integral component of care for older adults with heart failure (HF). Despite their prominent role, poor clinical outcomes for the medically complex patients with HF managed in SNFs are common. Barriers to providing quality care include poor transitional care during hospital-to-SNF and SNF-to-community discharges, lack of HF training among SNF staff, and a lack of a standardized care process among SNF facilities. Although no evidence-based practice standards have been established, various measures and tools designed to improve HF management in SNFs are being investigated. In this review, we discuss the challenges of HF care in SNFs as well as potential targets and recommendations that can help improve care with respect to transitions, HF management within SNFs, and modifiable factors within facilities. Policy considerations that might help catalyze improvements in SNF-based HF management are also discussed.
Keywords: Skilled nursing facility, post-acute care, heart failure, transitions, systems of care, policy
Of the more than 1 million hospital discharges for heart failure (HF) each year in the United States,1 approximately 20% result in discharge to skilled nursing facilities (SNFs).2,3 Hospitalized patients with HF discharged to SNFs are usually older, frailer, and have significantly more complexity (greater comorbidity and higher mortality risk) than patients with HF discharged home.3 Nonetheless, many patients with HF referred to SNFs have the expectation they will return to home after attaining physical therapy goals or stabilization of their medical issues. Given this challenge, it seems SNF care could/would already be honed to best ensure success, but instead practice patterns vary widely between facilities and differences in quality and efficiency are significant.4 Medicare spending on SNF services is increasing and totaled $28.6 billion in 2014.4 The annual cost of HF care among all SNF patients has not been described, but 1 study suggested that Medicare spent $3.39 billion in 2006 on potentially avoidable skilled nursing facility rehospitalizations,5 of which HF was a significant component.6 This evolution and punitive repercussions of rehospitalization have transformed SNF HF management into a major policy priority.
The numerous challenges of providing care to patients with HF in SNFs stem from 3 broad categories: (1) the complexity of the patients3,7; (2) lack of standardized systems of care to facilitate smooth patient transfer and management; and 3) variability in individual SNF’s capacity to provide quality care. Although attention to problems related to HF management in SNFs has been growing, evidence for improvement strategies has lagged. Two recent reviews have been informative about HF care in SNFs.8,9 One is a comprehensive review of the recent literature on the current state of knowledge of patients with HF in SNFs. Of 37 publications reviewed, 2 evaluation projects provide insights regarding patient clinical outcomes10,11 and 1 intervention study discusses challenges and strategies to improve staff preparedness to deliver HF care.12 The other review details best practices for transitional care and management of SNF patients with HF, and highlights the importance of patient-centered clinical HF management. It also explains that in the absence of HF-specific data-driven recommendations, SNF providers extrapolate evidence collected in non-SNF settings.9 This paper expands upon those reviews with an extended commentary accentuating expert insights regarding strategies to improve transitional and systems-based HF care in SNFs. Recommendations for responding to challenges in SNF based HF care as well as proposals for future policy considerations to address gaps in care are provided. While patient factors contributing to poor outcomes and priorities for targeted care of this population are also relevant, broad principles are briefly introduced in Table 1, but further details are beyond the scope of this manuscript and are described elsewhere.3,7–9,13,14
Table 1.
Problems, Barriers, Targets, and Recommendations for Improving Heart Failure Care in Skilled Nursing Facilities
| Factors Associated with Poor Outcomes for SNF Patients with HF | Problem Specifics | Barriers to Quality Improvement | Targets for Intervention | Recommendations |
|---|---|---|---|---|
| Patients | • Older • Multiple co-morbidities, • Functional and cognitive impairment |
• Administrative pressure for timely hospital discharge • Lack of attention to patient goals of care and end of life preferences • Lack of evidence based treatment strategies |
• Improved evaluation of readiness for hospital discharge • Patient centered care; Attention to geriatric and cardiology care issues • Underutilization of palliative care |
• Coordinated multidisciplinary pre-discharge assessments • Investigation into geriatric based management options, consultation with cardiologist • Consultation to palliative care and hospice services |
| Transitions of Care | • Documentation deficits | • Lack of standardization • Unclear which components of care are most pertinent to SNF admission • Lack of HF specific information |
• Identification of pertinent HF specific information • Standardization of discharge documentation • Addressing patient goals of care • Addressing social support structure |
• Inclusion of physiologic targets, and changes and responses to medication regimen • Recommending laboratory monitoring, and weight management • Inclusion of advanced directives, health literacy • Designation of primary caregiver/decision maker • Required discharge summary from SNF providers to community providers • Document functional gains and NYHA class, HF symptoms at SNF discharge • Provision of HF specific discharge information to cardiologist/HF specialist |
| • Communication deficits | • High clinical complexity • Inadequate HF training among SNF staff • Time constraints and volume of transfers limit participation in hand-offs • Lack of designated community PCP • Inability for frail cognitively impaired patients to participate in their own care. |
• Inter-professional team communication of HF details • Establish designated communications personnel • Enhance mid-level or physician to physician hand-offs |
• Include HF specific information in multidisciplinary transitional communications • Develop Inter-professional care plan • Designate select staff to communicate comprehensive discharge instructions role to select staff • Utilize a transitional coach for patients • Enhance caregiver involvement |
|
| • Transitional Care Coordination |
• Lack of SNF staff organizational structures • Lack of staff training in transitional care |
• Develop of HF sensitive transitional care programs | • Incorporate HF specific clinical targets and patient goals into communications • Involving HF specialty provider in communication chain |
|
| Systems of Care | • Risk Prediction | • Lack of validated HF risk prediction models for SNF patients | • Develop and validate current risk prediction models for patients with HF in SNFs | • Include caregivers in HF transitional care • Use of one or all currently available risk prediction tools to guide general risk estimates until more specific risk models are available: -HOSPITAL score45 – identifies risk of potentially avoidable 30-day readmissions in SNF patients, but not specific for HF patients -Registry based risk prediction tool44 – identifies indicators of HF rehospitalization in one SNF, but not validated -CORE risk calculator43 -predicts readmission risk of hospitalized HF patients, but not validated in SNF cohort |
| • Disease Management Programs |
• Lack of standardized protocols • Culture of SNF care not aligned with goals of post-acute patients with HF • Lack of outcomes data proving benefit of HF DMPs in SNFs |
• Staff education to improve recognition and monitoring of at-risk patients • Development of DMPs tailored to SNF patient demographic • Further research and outcomes data on effects of SNF based HF DMPs |
• Use of HF order sets to monitor clinical status and apply basic principles of HF management (i.e. dietary compliance and diuretic use) • Incorporate management for non-HF patients at risk for developing HF • Assess and manage comorbidities • Focus on HFpEF • Incorporation of geriatric principles into HF management strategies • Use the 2015 Scientific Statement on HF Management in SNFs13 |
|
| • Patient Monitoring | • Lack of standardized monitoring processes • Nuanced and unfamiliar triggers of HF exacerbation • Lack of control over patient choices and compliance • Nursing and nutrition service culture accustomed to improving hydration/ failure to thrive • Cognitive limitations in patients impairs symptom reporting |
• Staff education specifically to monitor nuanced factors contributing to exacerbations in SNF patients with HF (i.e. atrial arrhythmias, infection, high sodium meals/snacks) | • Collective nursing effort to monitor at risk patients • Close monitoring of weights, diuretic needs, dietary choices, symptoms • Improved training on triggers for HF exacerbation in SNF HFpEF patients Notification to physician of changes in physiologic status • Monitoring status of comorbid illnesses |
|
| • Timely interventions | • Lack of standardization of protocols for timely intervention specific to HF patients • Lack of staff training to administer interventions and/or IV medications |
• Increased use of quality improvement interventions • Train on HF specific interventions, including IV medication administration • Compliance with CMS proposal for physician bedside encounter prior to hospital transfer |
• Use of Interact II52 to assess clinical changes • Broaden assessment and interventions to incorporate HF issues • Redirect management strategy when interventions are not effective • Improve bedside availability of SNF based physicians • Use of specialty consultation when needed |
|
| Skilled Nursing Facility Characteristics | • Non-Modifiable | • Facility size • Profit status • Free standing vs. hospital based •Geographic location |
• Improved awareness of outcomes and achievement of quality metrics associated with non-modifiable facility factors | • Mindful recommendation of SNFs with non-modifiable factors for high risk patients • Cautious selection of SNFs with higher quality ratings based on non-modifiable factors, (i.e. smaller, hospital based not for profit facilities) |
| • Modifiable | • Lack of resources to improve SNF staffing availability and staff to • Cultures resistant to changing administrative or admitting practices • Misaligned incentives to admit healthy patients |
• Improved NP/MD, RN, and PT/OT staffing availability • Increased preparedness for admission of high risk patients • Promoting a culture of change and com- mitment to excellence among staff • Improved administrative policies on staff education and team building • Building collaborative networks with hospitals and community providers |
• Selection of SNFs for high risk patients with emphasis on quality of care • Administrative leadership investment in quality improvement • Motivate to establish partnerships with referral networks. |
SNF, Skilled Nursing Facility; HF, Heart Failure; NYHA, New York Heart Association; PCP, Primary care provider; DMP, disease management program; HFpEF, Heart failure with preserved EF; IV, intravenous; CMS, Center for Medicare and Medicaid Services; NP, nurse practitioner; MD, Doctor of medicine; RN, registered nurse; PT, physical therapy; OT, occupational therapy.
HF Hospital Admissions and Readmissions From SNFs Are Central to Policy Changes
Hospital readmissions have become a widely used metric by which suboptimal care is measured, and, as such, rehospitalization is now a key target of legislative efforts.15,16 Although causes of readmissions from SNFs are often difficult to deconstruct, HF and/or HF symptoms are frequent triggers.17–20 In the context of current measured quality metrics, HF is 1 of 13 conditions recognized by The Center for Medicare and Medicaid Services (CMS) as potentially preventable; in other words, rehospitalization could potentially be avoided with improved monitoring and management in the SNF setting.21 In an analysis of Medicare claims, HF was identified as 1 of the 3 most frequent “avoidable” reasons for rehospitalizations among residents within 100 days of SNF admission.21
With the goal to improve quality and value of care in SNFs, and reduce rehospitalization, Congress initiated several legislative changes: (1) the Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) requires submission of standardized data from post-acute care settings15 and (2) the Protecting Access to Medicare Act of 201416 authorized CMS to create an SNF value-based purchasing program, a reimbursement model tied to performance and quality, rather than the traditional “fee-for-service” model. The value-based purchasing program performance is based on a specific “resource use” measure, the SNF 30-Day Potentially Preventable Readmission Measure, which assesses rates of preventable readmissions, including HF, within the first 30 days of the SNF stay. SNFs that achieve high performance measures by October 1, 2018, will receive incentive payments; SNFs that lag behind (eg, bottom decile) will be subject to penalties.22 The first adjustments to SNF payments will occur in 2019. Since 2012, rates of hospital admission in the 30 days after SNF discharge have also been tracked.23 Data suggest that more than 20% of patients discharged from SNFs seek acute care within the subsequent 30 days.24 CMS has since been developing a Potentially Preventable 30-Day Post-Discharge Readmission Measure for SNFs that aligns with standards of the IMPACT Act of 2014, which is intended to discern how well SNFs are transitioning patients to the next health care setting.
Several key complexities confound interpretation of these metrics. SNF patients with HF are frequently readmitted for reasons unrelated to their primary diagnosis, and development of HF is also common among SNF patients with other diagnoses. One study shows that SNF patients with a primary diagnosis of HF during their index hospitalization are among the most frequently readmitted patients within 30 days, but they are readmitted for HF in only 38% of cases. Other causes of rehospitalizations included pneumonia (14%); sepsis (8%); ischemic heart disease (6%); atrial fibrillation and other respiratory, renal, cardiovascular, and infectious diseases (21%); and all other diagnoses (13%). Furthermore, patients with a primary diagnosis admission of renal failure, ischemic heart disease, pneumonia, or other respiratory disorders were readmitted with a diagnosis of HF in 12%, 22%, 9%, and 14%, of cases, respectively.25 Such data highlight the vulnerability of SNF patients with HF to developing or succumbing to their comorbid illnesses as well as the importance of monitoring all SNF patients for the development of HF, regardless of their primary admitting diagnosis.
Improving performance on HF quality metrics in SNFs will require comprehensive interventions and focus on enhancing transitions and care for circumstances that are inherently complex. To address these issues, we review practical targets and recommendations for improving transitions as well as systems factors and facility factors to enhance quality of care (Table 1). Specific priority targets and recommendations are highlighted, and knowledge gaps that should be addressed in future research and policy efforts are identified.
Transitional Care for Patients With HF Admitted to and Discharged From SNFs
Transitions of care (ie, transitional care) occur when patients are transferred between health care settings (ie, from hospital to SNF or from SNF to home) and actions (ie, medical reconciliation, discharge documentation, communication, co-ordinating patient follow-up, and postdischarge services) are taken to ensure coordination and continuity of care.26 Gaps in transitions contribute to poor outcomes,27,28 and poor documentation, lack of attention to patient goals and geriatric conditions (eg, cognitive impairment, health literacy, frailty), and poor communication between providers29 may contribute to suboptimal transitional care for SNF patients. Transitional care is further encumbered by lack of ownership of the responsibility in SNFs, insufficient time available for SNF staff to engage in these complex processes, and/or uncertainty of who/what/how to achieve the most effective transitional care for patients with HF. In 1 study, organizational structures and interactions related to transitional care among SNF staff were found to be fragmented, uncoordinated, lacking interdisciplinary approaches, and did not address patient goals.30 Limited physical and cognitive functional capacities among SNF patients with HF add to cumulative challenge. Effective transitional care interventions for both older hospitalized patients with HF and SNF patients discharged to home have been described, and 1 review nicely describes their applicability to SNF patients with HF in the absence of HF-specific, evidence-based SNF strategies, with emphasis on the need for coordinated, comprehensive care.9
Transitions: Opportunities for Improvement
HF-Specific Documentation and Communication.
Improved documentation and communication are targets to enhance transition to and from SNFs. Hospital discharge summaries often lack disease-specific content and broader patient goals.31–33 Although impact of improved discharge summaries on outcomes has not been specifically proven,34,35 utility seems self-evident. HF-specific documentation can clarify physiologic targets (eg, discharge weight, ideal weight and recent trends, blood pressure goals), heart failure type (ie, HF with preserved ejection fraction [HFpEF] vs HF with reduced EF [HFrEF]), New York Heart Association (NYHA) classification, recommended follow-up laboratory tests, and patient-specific management recommendations, and can better direct and educate SNF providers. Expectations and goals for clinical and functional improvement are especially important for frail SNF patients with HF who often fall short of rehabilitation objectives.
Providing clinical summaries is not yet routine process, but was included among the new rules for long-term care facilities released by CMS effective as of November 28, 2016.36 Inclusion of HF-specific content in SNF discharge documentation is a priority recommendation for enhancing care. This is especially important for patients either without a designated cardiologist or who logistically can only follow-up with a general community practitioner who might not easily interpret changes in a patient’s HF regimen or status. Adjustments to goals of care that occurred during the SNF stay and the level of function or NYHA symptom class after completion of physical rehabilitation should also be documented upon SNF discharge to better convey benchmarks for the next provider.
Improved communications between providers are also important,29 and may enhance care for patients with HF. A study evaluating the impact of phone calls from a hospital case manager to SNF nurses within 48 hours of hospital discharge to review specific aspects of HF care (weights, sodium restrictions, diuretic use, and discharge plans) demonstrated a reduction in average rate of hospital readmissions from 30% to 11.3% and a net cost savings of $16,748 over a 6-month period.11 Direct communications between mid-level providers or physicians regarding complex HF management and goals of subacute care at the time of transfer are often abandoned amidst constraints of time, practitioner unavailability, volume of patient transfers, and shift-based coverage, but are logical priorities.
Multiple environmental, medical, social, and organizational issues confound communication goals,29 especially in transitions from SNF to home. It is also frequently difficult to identify a community primary care physician (PCP) and a community cardiovascular disease specialist and to arrange follow-up appointments. Designating personnel in the community to confirm receipt of communication and relay SNF HF discharge documentation to a designated community PCP or specialist would theoretically improve the process and should be considered. Enhanced communications between SNF providers and patients and caregivers, use of a transitional coach (a provider who directs communication between the patient/caregiver and PCP, and maintains patient contact through postdischarge site visits and phone calls),37 and direct provider-to-provider communication in the case of particularly complex patients, are additional considerations.
Multidisciplinary Transitional Care Programs.
Strategies of multidisciplinary transitional care teams providing patient education, emphasis on self-care, optimizing medication adherence, and ensuring evidence-based HF pharmacotherapy have been shown to be effective in decreasing admissions and mortality in patients with HF discharged from the hospital to the community.9,38 Although it seems logical to apply similar processes to SNF patients, added complexity often arises from cognitive and functional limitations that are more likely among SNF patients and that can detract from education, self-care, and/or adherence goals. CMS has recently required development of a comprehensive, patient-centered baseline care plan by an interdisciplinary team (including a nurse aide and dietary staff member) for residents within 48 hours of admission.36 Incorporating HF-specific management into these care plans is an important first-step consideration for transitioning hospitalized patients with HF to SNFs.
Small intervention studies have demonstrated improvements in SNF-to-home transitional care by adding a pharmacistled intervention to medication reconciliation39,40; using personalized care planning, patient-centered discharged instructions, timely communications with PCPs, utilization of electronic medical record tools;41 and arranging appointments in a postdischarge clinic 72 hours before or on the same day of SNF discharge.42 Two targets stand out from these studies: well-organized interprofessional team-based care models and timely/earlier use of transitional care interventions.30,37,41,42 The benefit of similar multidisciplinary transitional care programs to facilitate transitions for complex SNF patients with HF should be a priority of future research. Until data are available, a multidisciplinary discharge planning approach (including pharmacists, social work, dietary and nursing staff) to begin early in the SNF course seems a logical step to enable generation of coordinated plans (ie, medication reconciliation, patient education, and establishing adequate follow-up and/or home health care).
HF Disease Management Approach
Processes to improve assessment and management of patients with HF during their SNF stay are critical determinants of quality and efficacy, but are inherently challenging. An undertrained and unstable SNF workforce, lack of standardized SNF disease management programs (DMP), and limited physician access all contribute to this challenge. Risk prediction tools, monitoring protocols, and DMPs have evolved, but still need to be adapted for SNF patients with HF (Table 1). Designation of disease management responsibilities need to be adapted to individual SNFs, which vary widely in their staffing practices. Importantly, management decisions made by physicians in other healthcare systems may fall to mid-level providers (ie, nurse practitioners or physician assistants) or nursing supervisors, who may be more readily available in the SNF setting.
Improving Risk Prediction
Risk prediction calculators to estimate HF readmission risk for hospitalized patients have been developed,43 but validated risk prediction models for SNF patients do not exist. Understanding HF hospitalization risk upon admission and throughout the SNF stay could guide the intensity of clinical monitoring, frequency of reassessments, and the extent of clinical intervention needed. One risk score model categorized patients with HF as high risk for readmission based upon: (1) a hospitalization in the last 6 months for HF; (2) a primary hospital discharge diagnosis of HF or an active secondary diagnosis (signs and symptoms of HF); (3) NYHA III or IV symptoms; and (4) hypertension. In contrast, patients were considered low risk with (1) ≥ 6 months since last hospitalization and (2) NYHA I or II symptoms,44 but this model has not yet been validated. Until validated models for SNF patients with HF become available, use of 1 or more available models by physician, nursing, or administrative staff may be a reasonable approach (Table 1).43–45
Enhanced Monitoring for Patients at Risk
Close monitoring of HF can contribute to improved outcomes, and patients should be regularly assessed for signs and symptoms of HF.9,13,14 Use of HF admission orders to ensure regular assessment of weights (with instructions to contact providers for weight gain), dietary sodium restriction (2 g), and to gauge diuretic use in SNF patients with HF was associated with a reduction of average monthly readmission rate (from 30% to 11%).11 However, for most SNFs, these goals can be surprisingly difficult to achieve. Key impediments include the following. (1) Dietary challenges. Despite the controlled SNF environment, low-sodium diets are infrequently available, dietary restrictions are opposed to the SNF culture where patient choice has been highly valued, and dietary recommendations can be undermined as patients are free to accept snacks and meals from visitors. (2) Urinary confounders. Patients prone to incontinence often request to hold diuretics before therapy or outpatient appointments, and SNF staff tend to encourage hydration and regard weight gain as a marker of improved nutrition rather than imminent HF decompensation. (3) Infections. SNF patients are at risk of infectious exposure, a common HF trigger. (4) Multimorbidity. SNF patients are prone to atrial arrhythmias, labile hypertension, and other triggers of HF exacerbation. Moreover, SNF staff may lack sophistication (eg, inappropriately holding diuretics for bradycardia) to administer algorithm-based care effectively. (5) Cognitive limitations. High prevalence of cognitive limitations makes it difficult to rely on patients’ report of HF symptoms.46 The 2015 American Heart Association/Heart Failure Society of America Scientific Statement on HF management in SNFs suggests that monitoring patients with HF be a collective nursing staff effort and be tailored to the patient’s individual risk.13 Staff training to achieve adequate monitoring is essential. Some important considerations to improve monitoring of patients with HF include assessments of daily weights by certified nursing assistants or licensed practical nurses, if possible, for at least the first 7 days of SNF admission, notifying the covering physician or mid-level provider of weight gain according to prespecified parameters, monitoring serum chemistries in appropriate patients within 1–2 weeks after admission, increasing the frequency of weight and volume assessments of patients with HF who develop an infection or other potential exacerbation trigger (eg, poorly controlled hypertension, atrial fibrillation), avoiding excess fluid intake, and monitoring fluid balance with the goal of reducing diuretics when possible.47
Implementing Disease Management Programs
A standardized SNF-based HF DMP to provide education, protocols, and interventions based on quality standards has yet to be established. Barriers to development and implementation of HF DMPs may stem in part from the complexity of the patient population as well as a culture of care in SNF setting in which stringencies of HF management seem foreign.
An important clinical consideration is that SNFs treat predominantly older patients with HFpEF, rather than younger patients with HFrEF.3 DMPs thus need to respond to the clinical needs of both HFpEF and the comorbid illnesses/geriatric syndromes with which HFpEF is particularly associated. Because readmission is often precipitated by comorbidity rather than incident HF,25,48 regular evaluation and optimization of care for active comorbidities by physicians or mid-level providers in the context of patient-centered goals of care is essential. Management considerations were well-summarized in the 2015 American Heart Association/Heart Failure Society of America Scientific Statement on HF Management in SNFs.13 Salient considerations include judicious use of diuretics and antihypertensive agents to mitigate risks of falls, orthostasis, and prerenal azotemia; and use of agents demonstrated to reduce hospitalizations in older HFpEF patients such as the angiotensin-converting enzyme inhibitor perindopril, the angiotensin-receptor blocker candesartan, and/or the β-blocker nebivolol. Likewise, daily physical activity facilitated either by therapy or nursing staff is promoted.
Multiple small trials have demonstrated the utility of aerobic and strength training to improve functional and qualitative outcomes in old, frail, and complex HFpEF patients.49 Typical outcomes include improved functional capacity, enhanced physical activity, better self-efficacy, and potential for increased independence, reduced falls, and improved quality of life. With the unique advantage of having onsite therapy and exercise programs, HF DMPs could incorporate standard monitoring of progress with physical therapy into HF assessments, and titrate therapy to patients with HF goals of care. Similarly, incorporating frailty as a modifier of SNF-based HF management is another important consideration for SNF clinicians and a compelling area for research. Even as those standards evolve, routine assessments to reduce sedating and/or hemodynamically compromising medications, improve nutrition, and reduce use of medications that could exacerbate HF, are important practices to integrate into management protocols, especially when dietary, pharmacy, and social services are available in SNFs to facilitate those practices.
Robust staff education and strong leadership are critical to implementing a HF DMP in SNFs. One project implementing an educational based DMP in 4 academically affiliated SNFs found that at baseline SNF staff had limited foundational knowledge of HF, and no guidelines to monitor, treat, or track patients with HF. During the project, staff enthusiasm quickly waned; attendance at didactics decreased; staff turnover was high; and, at best, only 65% of participants completed the training tests. Nonetheless improvements from pre-to posttest scores of HF knowledge and confidence were demonstrated, highlighting the importance of quality didactic training but the need to further refine its delivery.12 The use of HF champions, physician coaches who facilitate and guide teams and attend weekly interdisciplinary HF rounds, has been shown to improve adherence to HF DMP components within SNFs.50 Similar models should be considered among administrative staff currently developing HF protocols. Ongoing research is essential to develop a standardized organizational structure.
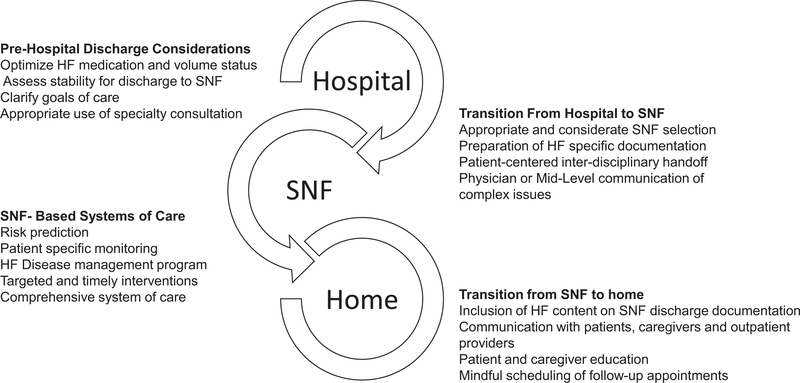
Implementing an Integrative Approach to SNF HF Care
Modification of transitional care, risk assessment, DMPs, monitoring, and intervention protocols for SNF patients with HF may be more easily achieved if integrated into a comprehensive systems of care model. One small study evaluated development of a skilled heart unit, a model designed by an SNF medical director, nurse, and cardiologist, which used best practices in communication, nursing assessments, advanced care planning, thorough initial assessments, daily weight monitoring, daily nurse practitioner rounds, maintaining scheduled cardiology appointments, family and patient education, weekly interdisciplinary rounds, and root cause analysis of hospital transfers. Although this 6-month evaluation involved only 15 SNF patients and was not designed to assess the effect of the program on outcomes, the staff response to the intervention was positive and hospital readmissions and mortality were below reported averages.51 Use of a similar comprehensive program, combined with practices to better determine clinical stability before hospital discharge, assessing ongoing readmission risks, providing timely interventions,52 and improving HF-specific staff training, would seem to significantly enhance care (Fig. 1). Research is needed to assess if such intensive efforts would improve efficiency and clinical outcomes.
Fig. 1.
Conceptual model of an integrated approach to improving the systems of care and transitions.
Facility Factors
A unique challenge in discharging patients to SNFs is that the facilities themselves lag behind hospitals in experience relevant to achieving quality improvement in HF. Navigating though complexities in care provision within individual facilities can be difficult for providers and families. More than 90% of Medicare beneficiaries live in a county with 3 or more SNFs; fewer than 1% live in a county without one.4 SNF placement is often based on geographic preferences, insurance coverage, or facility acceptance, but understanding facility factors that contribute to quality may enhance discernment of which SNFs are best suited for patients with HF when a choice is available. Data specific to HF-related outcomes and SNF characteristics are very limited, but associations between SNF characteristics and quality metrics that incorporate HF outcomes (ie, preventable readmissions) are loosely informative until more specific data become available.
Facility Quality Ratings and HF Outcomes
In 2002, CMS launched The Nursing Home Compare website so that health inspections, staffing levels, and clinical quality measures could be publicly reported for the more than 15,000 Medicare-certified SNFs in the United States.53 In 2008, CMS began scoring individual SNFs using a 5-star rating system (on health inspections, staffing, clinical quality measures, and an overall quality rating) to help patrons better select facilities based on quality. A small retrospective study examining patients with acute decompensated HF showed that SNFs with lower overall quality ratings (<2 stars), had 15% to 20% higher 30-day risk-adjusted readmission rates, but the differences were not statistically significant.54 Another retrospective study found that lower overall quality, health inspection, and registered nurse staffing ratings were associated with greater 90-day mortality for patients with a primary diagnosis of HF after adjustment for facility characteristics. Lower quality ratings were associated with a greater hazard of 90-day readmission, but that association was attenuated when adjusted for facility size and ownership status.55 From these data, one might cautiously conclude that patients with HF may have a lower risk of dying in SNFs with some higher quality ratings. Quality ratings are inconsistently informative about readmission risks, however, and data are generally too weak to draw firm conclusions.
Facility Characteristics and Outcomes
The Medicare Advisory Payment Committee, distinct from CMS, does not use the 5-star quality rating system to track facility quality, but tracks rates of discharge back to the community, change in functional status during the SNF stay, and risk-adjusted rates of potentially avoidable readmissions (PARs) during both the SNF stay and within 30 days after SNF discharge.4 The direct contribution of HF to preventable readmission rates has not been clearly described, but studies have shown that HF is a significant contribution to PAR.56 Trends in HF readmission rates might then be cautiously extrapolated from PAR readmission data. Between 2011 and 2014, improvements were made for the first time in a decade in both risk-adjusted PAR rates during the SNF stay (decreased from 12.4% to 10.9%) and in community discharge rates (increased from 33.1 to 37.6%).4 Facilities that were hospital-based, not-for-profit, and smaller performed better than larger facilities on both readmission and community discharge rates; urban SNFs performed better than rural SNFs with regard to community discharge rates only.20 Providers might interpret these data as a signal that discharging patients with HF to smaller, not-for-profit, hospital-based SNFs may yield slightly better 30-day readmission rates during the SNF stay, but definitive conclusions are still uncertain. Notably, improvements in readmission rates during the SNF stay follow the recent legislative initiatives to reduce hospital readmissions, and may reflect hospital incentives to establish preferred provider networks with higher quality SNFs.
Potentially avoidable readmission rates within 30 days of SNF discharge increased slightly from 5.5% in 2013 to 5.6% 2014, and there was significant variation between the worst-performing quartile (7.9%) and best-performing quartile (3.6%) of SNFs. These data suggest there remains considerable room for improvement in this quality measure.4 No facility characteristics have been found to be predictive of 30-day post-SNF discharge PAR rate20; however, PAR rates during SNF stays are associated with readmissions within 30 days after SNF discharge, which suggests that SNFs with adequate quality to prevent readmissions during the SNF stay have better quality in the postdischarge transition.57 Still, until individual SNFs can be identified as being better prepared to manage and transition patients with HF, providers and patients should cautiously consider quality ratings and facility characteristics when selecting SNFs, if a choice is available.
Modifiable Facility Characteristics
Perhaps more practical considerations for SNF selection would be assessments of their allocation of resources to staffing and/or admitting practices. Availability of a medical director, primary care provider, nurse practitioner, or physician assistant, and more nursing hours per resident-day are associated with lower all cause hospitalization rates19,20; higher physical therapy staff hours per resident-day is associated with higher rates of community discharge.20 It seems plausible that SNFs with investment in greater staff availability might be better suited for complex elderly patients with HF, but more data are needed to assess the effect of SNF staffing patterns on outcomes specific to patients with HF. Patients admitted to SNFs with higher patient volume (annual number of admissions in the top tertile) had lower all-cause 30-and 90-day rehospitalization rates58; whether sending patients with HF to SNFs where the staff are accustomed to higher clinical volumes is associated with improved outcomes should be considered in future research efforts. Discharges from hospitals with higher nurse staffing levels and higher scores on accountability processes (eg, prescription of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers for left ventricular systolic dysfunction) to SNFs with higher nurse staffing levels and lower deficiency scores are associated with lower 30-day hospitalization rates.59 Although hospitals are often focused on the quality of the SNF to which they are sending patients, perhaps a consideration for SNFs might be assessing the quality of the hospitals sending them their patients with HF.
Variability in quality among SNFs4 may lie in yet underinvestigated factors such as cultural and attitudinal characteristics of facility staff and administration. As an example, SNFs with a culture resistant to quality improvement efforts or little emphasis on staff education might provide lower quality of care than facilities that emphasize staff development and ambitiously seek preferred provider status among referring hospitals. Investigation into the effect of SNF administrative characteristics and other cultural variables on outcomes of patients with HF is needed. For providers, gaining an understanding of SNFs on levels beyond their published ratings is encouraged.
Future Policy Considerations
Adding regulations on the federal level is a complex challenge; however, we advocate that federal policies are needed to both better assist SNFs in meeting their impending quality mandates, and improve the overall quality of care SNFs provide to the increasing number of patients with HF.
Classification of SNFs as “HF Ready:” Under newer bundled payment models, hospitals will bear the burden of postacute care costs. Many hospitals currently have broad but weak relationships with postacute care providers,60 with little impact on the care that is administered. Selecting “HF-Ready” SNFs, those that demonstrate preparedness for HF care and/or above average HF outcomes for hospitalized patients with HF, may lead to cost savings and improved patient care, and could narrow the selection process for case management and families of patients with HF when choice is available. Components of such “HF readiness” might include standardized physician and nursing training with 100% compliance in meeting HF core competencies, nursing staff trained in administration of IV diuretics, established HF disease management protocol, operating within a developed system of care that addresses the needs of patients with HF as outlined previously, and an on-staff physician with additional training in HF. Alternatively, SNFs that voluntarily obtain HF certification through The Joint Commission could be designated as “HF Ready.”
Core competencies in HF training for medical directors, nurse practitioners, and nursing staff: Completion of core competencies in HF training and annual performance assessments should be required for all clinical nursing staff, even in SNFs not opting to be “HF ready,” given the prevalence of HF in SNFs.7,13 Medical directors obtain certification for their role through the American Board of Post-Acute and Long-Term Care Medicine, and incorporation of modules into the American Medical Directors Association’s training program to assist medical directors in implementing HF management protocols should be considered. Continuing interprofessional education for SNF staff that addresses not only care provision but team-based improvement strategies can be offered nationally.
Collecting data specific to SNF patients with HF: Current data do not quantify the economic burden of HF care in SNFs, and data are very limited on outcomes specific to SNF patients with HF. Reported rates of preventable readmissions incorporate 12 other conditions in addition to HF.4 Medicare data should be examined to better describe the economic burden/annual cost of HF care provided for patients requiring SNF-based care as well as the specific contribution of HF to measured SNF quality metrics. These data could better direct resource allocation and guide future HF-specific intervention efforts of physicians and staff.
Incentivizing cardiologists to staff SNFs using loan forgiveness: Better SNF staffing is associated with improved outcomes.19,20 The presence of specialty physicians in SNFs is growing, but still remains underproportioned to address the needs of complex SNF patients with heart disease. Because SNF-based work is inherently inefficient and may result in relative revenue loss for practicing cardiologists, implementation of a federal loan forgiveness program for cardiovascular disease specialists who staff SNFs with advanced cardiac care needs should be considered.
Encouraging selective use of evidence-based HF therapy in SNFs, including cardiac rehabilitation: Evidence-based management strategies for the complex SNF HF population are lacking, but utilization of selectively applicable guideline recommended therapies should be encouraged, with the understanding that many geriatric cardiology patients may not be appropriate candidates for all therapies. The most recent guidelines recommend cardiac rehabilitation (CR) as a class IIa indication61 and CR has been shown to improve quality of life62 and exercise capacity,63 yet components of CR are not offered in SNFs.64 Furthermore, in 2014, Medicare expanded coverage for CR eligibility, and recent work shows that this has significantly increased the size of the Medicare population with HFrEF potentially eligible for CR.65 SNF staff should be required to discuss and encourage qualified patients with HF to enroll in CR upon discharge from SNF (if such a program is available) to further augment wellness and strengthening/functional training achieved after standard SNF physical and occupational therapy services.
Conclusions
SNFs are moving to the forefront of care as a key component in the transitional pathway from acute care hospitalization to the community for older patients with HF; however, quality standards to optimize care are still lagging. Better understanding of factors that contribute to optimal care for older patients with HF, who tend to be inherently more complex than younger patients, is an area that requires ongoing investigation and management enhancements. The cardiology community has been garnering support to optimize the care of geriatric cardiology patients,66 and interests in evidence-based recommendations for diagnosis and treatment of older patients with HF is developing.67 As this matures, we advocate for pragmatic strategies that enhance the quality of SNF-based HF care and we emphasize the value of research and policy changes (both in respect to medical standards and federal laws) that are helping to foster insights and incentives to overcome the many gaps in care that still persist for this vulnerable population.
Acknowledgment
Supported by NIH grant R01 HL 113387.
Dr. Forman is supported in part by NIA grants P30 AG024827 and 1R56AG051637–01A1, PCORI grant IH-1304678, and VA Office of Rehabilitation Research and Development grant F0834-R
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 update. Circulation 2015;26:447–54. [DOI] [PubMed] [Google Scholar]
- 2.Dolansky MA, Xu F, Zullo M, Shishehbor M, Moore SM, Rimm AA. Post-acute care services received by older adults following a cardiac event: a population-based analysis. J Cardiovasc Nurs 2010;25:342–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, Masoudi FA, et al. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Hear Fail 2011;4:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Medicare Payment Advisory Commision. Medicare payment policy. Rep to Congr 2016;175–205. [Google Scholar]
- 5.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff 2010;29:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donelan-McCall N, Eilertsen T, Fish R, Kramer A. Small patient population and low frequency event effects on the stability of SNF quality measures. 2006. A report submitted to Medicare Payment Advisory Commission. Available at: http://www.mobileendoscopix.com/assets/pdf/Small%20Patient%20Pop%20and%20Low%20Frequency%20Event%20Effects%20on%20the%20Stability%20of%20SNF%20Quality%20Measures.pdf. [Google Scholar]
- 7.Orr NM, Forman DE, De Matteis G, Gambassi G. Heart failure among older adults in skilled nursing facilities: more of a dilemma than many now realize. Curr Geriatr Reports 2015;4:318–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jung M, Yeh A-Y, Pressler SJ. Heart failure and skilled nursing facilities: review of the literature. J Card Fail 2012;18:854–71. [DOI] [PubMed] [Google Scholar]
- 9.Nazir A, Smucker WD. Heart failure in post-acute and long-term care: evidence and strategies to improve transitions, clinical care, and quality of life. J Am Med Dir Assoc 2015;16:825–31. [DOI] [PubMed] [Google Scholar]
- 10.Valle R, Chinellato M, Milani L. Impact of a guideline-based management on outcomes of very old persons with heart failure living in nursing homes. Arch Intern Med 2001;161:2264–5. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs B. Reducing heart failure hospital readmissions from skilled nursing facilities. Prof Case Manag 2011;16:18–24. [DOI] [PubMed] [Google Scholar]
- 12.Boxer RS, Dolansky MA, Frantz MA, Prosser R, Hitch JA, Pina IL. The bridge project: Improving heart failure care in skilled nursing facilities. J Am Med Dir Assoc 2012;13:83–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jurgens CY, Goodlin S, Dolansky M, Ahmed A, Fonarow GC, Boxer R, et al. Heart failure management in skilled nursing facilities: a scientific statement from the American Heart Association and the Heart Failure Society of America. J Card Fail 2015;21:263–99. [DOI] [PubMed] [Google Scholar]
- 14.AMDA. Heart failure in the long-term care setting: clinical practice guidelines. Columbia. MD: AMDA: Society of Post-acute and Long-term care Medicine; 2015. [Google Scholar]
- 15.Improving Medicare Post-Acute Transformation Act of 2014, Pub. L. 113–185, 128 Stat. 1952 (1801 U.S.C. 6001 et seq.). Available at: http://www.gpo.gov/fdsys/pkg/BILLS-113hr4994enr/pdf/BILLS-113hr4994enr.pdf.
- 16.United States Congress. HR 4302. 2014. Protecting access to medicare act of 2014. Available at: https://www.gpo.gov/fdsys/pkg/PLAW-113publ93/pdf/PLAW-113publ93.pdf.
- 17.Hutt E, Ecord M, Eilertsen TB, Frederickson E, Kramer AM. Precipitants of emergency room visits and acute hospitalization in short-stay medicare nursing home residents. J Am Geriatr Soc 2002;50:223–9. [DOI] [PubMed] [Google Scholar]
- 18.Burke RE, Whitfield EA, Hittle D, Min SJ, Levy C, Prochazka AV, et al. Hospital readmission from post-acute care facilities: risk factors, timing, and outcomes. J Am Med Dir Assoc 2016;17:249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ouslander JG, Naharci I, Engstrom G, Shutes J, Wolf DG, Rojido M, et al. Hospital transfers of skilled nursing facility (SNF) patients within 48 hours and 30 days after SNF admission. J Am Med Dir Assoc 2016;17:839–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, et al. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J Am Geriatr Soc 2010;58:627–35. [DOI] [PubMed] [Google Scholar]
- 21.Kramer A, Lin M, Fish R, Min S. Development of potentially avoidable readmission and functional outcome SNF quality measures. p1–75 A Report for the Medicare Payment Advisory Commission. 2014. Available at: https://www.providigm.com/wp-content/uploads/2013/08/Mar14_2014_SNFQualityMeasures_CONTRACTOR.pdf.
- 22.U.S. Department of Health and Human Services. Report to Congress. Plan to implement a medicare skilled nursing facility value-based purchasing program. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/SNFPPS/Downloads/SNF-VBP-RTC.pdf. 2014.
- 23.Medicare Payment Advisory Comission. Medicare payment policy. Rep to Congr 2014;333–59. [Google Scholar]
- 24.Toles M, Anderson RA, Massing M, Naylor MD, Jackson E, Peacock-Hinton S, et al. Restarting the cycle: incidence and predictors of first acute care use after nursing home discharge. J Am Geriatr Soc 2014;62:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ouslander JG, Diaz S, Hain D, Tappen R. Frequency and diagnoses associated with 7-and 30-day readmission of skilled nursing facility patients to a nonteaching community hospital. J Am Med Dir Assoc 2011;12:195–203. [DOI] [PubMed] [Google Scholar]
- 26.American Medical Directors Association. Transitions of care in the long-term care continuum clinical practice guideline. Columbia, MD: AMDA; 2010, p. 1–80. [Google Scholar]
- 27.Sofaer S. Navigating poorly charted territory: patient dilemmas in health care “nonsystems. Med Care Res Rev 2009;66(1 Suppl):75S–93S. [DOI] [PubMed] [Google Scholar]
- 28.Coleman EA. Falling through the cracks: challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549–55. [DOI] [PubMed] [Google Scholar]
- 29.King BJ, Gilmore-Bykovskyi AL, Roiland RA, Polnaszek BE, Bowers BJ, Kind AJH. The consequences of poor communication during transitions from hospital to skilled nursing facility: a qualitative study. J Am Geriatr Soc 2013;61:1095–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Toles M, Colón-Emeric C, Naylor MD, Barroso J, Anderson RA. Transitional care in skilled nursing facilities: a multiple case study. BMC Health Serv Res 2016;16:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horwitz LI, Jenq GY, Brewster UC, Chen C, Kanade S, Van Ness PH, et al. Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med 2013;8:436–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neuman MD, Wirtalla C, Werner RM. Association between skilled nursing facility quality indicators and hospital readmissions. JAMA 2014;312:1542–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Damluji MS, Dzara K, Hodshon B, Punnanithinont N, Krumholz HM, Chaudhry SI, et al. Hospital variation in quality of discharge summaries for patients hospitalized with heart failure exacerbation. Circ Cardiovasc Qual Outcomes 2015;8:77–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl J Med 2009;361:2637–45. [DOI] [PubMed] [Google Scholar]
- 35.Hansen LO, Strater A, Smith L, Lee J, Press R, Ward N, et al. Hospital discharge documentation and risk of rehospitalisation. BMJ Qual Saf 2011;20:773–8. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Medicare and Medicaid Services. Capitalized: Medicare and medicaid programs; reform of requirements for long-term care facilities. Rules and Regulations 2016; Available at: https://federalregister.gov/d/2016-23503 [PubMed]
- 37.Coleman EA, Jodi Smith ÃD, Janet Frank ÃC, Min S-J, Carla Parry Ã, Kramer AM. Preparing patients and caregivers to participate in care delivered across settings: the care transitions intervention. J Am Geriatr Soc 2004;52:1817–25. [DOI] [PubMed] [Google Scholar]
- 38.Feltner C, Jones CD, Cene CW, Zheng ZJ, Sueta CA, Coker-Schwimmer EJ, et al. Transitional care interventions to prevent readmissions for persons with heart failure: a systematic review and meta-analysis. Ann Intern Med 2014;160:774–84. [DOI] [PubMed] [Google Scholar]
- 39.Delate T, Chester EA, Stubbings TW, Barnes CA. Clinical outcomes of a home-based medication reconciliation program after discharge from a skilled nursing facility. Pharmacotherapy 2008;28:444–52. [DOI] [PubMed] [Google Scholar]
- 40.Reidt SL, Holtan HS, Larson TA, Thompson B, Kerzner LJ, Salvatore TM, et al. Interprofessional collaboration to improve discharge from skilled nursing facility to home: preliminary data on postdischarge hospitalizations and emergency department visits. J Am Geriatr Soc 2016;64:1895–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berkowitz RE, Fang Z, Helfand BKI, Jones RN, Schreiber R, Paasche-Orlow MK. Project reengineered discharge (red) lowers hospital readmissions of patients discharged from a skilled nursing facility. J Am Med Dir Assoc 2013;14:736–40. [DOI] [PubMed] [Google Scholar]
- 42.Park HK, Branch LG, Bulat T, Vyas BB, Roever CP. Influence of a transitional care clinic on subsequent 30-day hospitalizations and emergency department visits in individuals discharged from a skilled nursing facility. J Am Geriatr Soc 2013;61:137–42. [DOI] [PubMed] [Google Scholar]
- 43.Keenan PS, Normand S-LT, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes 2008;1:29–37. [DOI] [PubMed] [Google Scholar]
- 44.Dolansky MA, Capone L, Leister E, Boxer RS. Targeting heart failure rehospitalizations in a skilled nursing facility: a case report. Hear Lung J Acute Crit Care 2016;45:392–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kim LD, Kou L, Messinger-Rapport BJ, Rothberg MB. Validation of the HOSPITAL score for 30-day all-cause readmissions of patients discharged to skilled nursing facilities. J Am Med Dir Assoc 2016;17:863. e15–8. [DOI] [PubMed] [Google Scholar]
- 46.Heckman GA, Patterson CJ, Demers C, St.Onge J, Turpie ID, McKelvie RS. Heart failure and cognitive impairment: Challenges and opportunities. Clin Interv Aging 2007;2(2):209–218. [PMC free article] [PubMed] [Google Scholar]
- 47.Ahmed A, Young JB, Love TE, Levesque R, Pitt B. A propensity-matched study of the effects of chronic diuretic therapy on mortality and hospitalization in older adults with heart failure. Int J Cardiol 2008;125:246–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013;309:355–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pandey A, Parashar A, Kumbhani D, Agarwal S, Garg J, Kitzman D, et al. Exercise training in patients with heart failure and preserved ejection fraction: a meta-analysis of randomized control trials. Circ Hear Fail 2015;8:33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dolansky MA, Hitch JA, Piña IL, Boxer RS, Payne Bolton F. Improving heart failure disease management in skilled nursing facilities: lessons learned. Clin Nurs Res 2013;22:432–47. [DOI] [PubMed] [Google Scholar]
- 51.Nazir A, Dennis ME, Unroe KT. Implementation of a heart failure quality initiative in a skilled nursing facility: lessons learned. J Gerontol Nurs 2014;41:26–33. [DOI] [PubMed] [Google Scholar]
- 52.Ouslander JG, Lamb G, Tappen R, Herndon L, Diaz S, Roos BA, et al. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J Am Geriatr Soc 2011;59:745–53. [DOI] [PubMed] [Google Scholar]
- 53.Center for Medicare and Medicaid Services. Nusing Home Compare. Available at: https://www.medicare.gov/nursinghomecompare. 2016. [Google Scholar]
- 54.Ogunneye O, Rothberg MB, Friderici J, Slawsky MT, Gadiraju VT, Stefan MS. The association between skilled nursing facility care quality and 30-day readmission rates after hospitalization for heart failure. Am J Med Qual 2015;30:205–13. [DOI] [PubMed] [Google Scholar]
- 55.Unroe KT, Greiner MA, Colón-Emeric C, Peterson ED, Curtis LH. Associations between published quality ratings of skilled nursing facilities and outcomes of medicare beneficiaries with heart failure. J Am Med Dir Assoc 2012;13:188 e1–188.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kramer A, Lin M, Fish R, Sung-Joon Min M. Refinement of community discharge, potentially avoidable readmission, and functional outcome snf quality measures, for fiscal years 2011, 2012, and 2013 final report. 2015. p 1–57. Available at: http://www.medpac.gov/docs/default-source/contractor-reports/refinement-of-community-discharge-potentially-avoidable-readmission-and-functional-outcome-snf-quali.pdf?sfvrsn=0. 2016.
- 57.Kramer A, Fish R, Min S-J. Community discharge and rehospitalization outcome measures (Fiscal Year 2011) final report. 2013. Available at: http://ww1.prweb.com/prfiles/2014/03/04/11640554/Apr2013_Community_Discharge_CONTRACTOR_report.pdf. 2016.
- 58.Li Y, Cai X, Yin J, Glance LG, Mukamel DB. Is higher volume of postacute care patients associated with a lower rehospitalization rate in skilled nursing facilities? Med Care Res Rev 2012;69:103–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thomas KS, Rahman M, Mor V, Intrator O. Influence of hospital and nursing home quality on hospital readmissions. Am J Manag Care 2014;20:e523–31. [PMC free article] [PubMed] [Google Scholar]
- 60.Lau C, Alpert A, Huckfeldt P, Hussey P, Auerbach D, Liu H, et al. Post-acute referral patterns for hospitals and implications for bundled payment initiatives. Healthcare 2014;2:190–5. [DOI] [PubMed] [Google Scholar]
- 61.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation 2013;128:1810–52. [DOI] [PubMed] [Google Scholar]
- 62.Flynn KE, Piña IL, Whellan DJ, Lin L, Blumenthal JA, Ellis SJ, et al. Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009;301: 1451–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.O’Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009;301:1439–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dolansky MA, Zullo MD, Hassanein S, Schaefer JT, Murray P, Boxer R. Cardiac rehabilitation in skilled nursing facilities: a missed opportunity. Heart Lung 2012;41:115–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kelly JP, Hammill BG, Doll JA, Felker GM, Heidenreich PA, Bhatt DL, et al. The potential impact of expanding cardiac rehabilitation in heart failure. J Am Coll Cardiol 2016;68:977–8. [DOI] [PubMed] [Google Scholar]
- 66.Bell SP, Orr NM, Dodson JA, et al. What to expect from the evolving field of geriatric cardiology. J Am Coll Cardiol 2015;66(11):1286–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rich MW, Chyun DA, Skolnick AH, et al. Knowledge gaps in cardiovascular care of the older adult population. Circulation 2016;67(20):2419–2440. [DOI] [PMC free article] [PubMed] [Google Scholar]