Abstract
Objective
Coronavirus disease 2019 (COVID-19) is a disruptive pandemic that has continued to test the limits of health care system capacities. It is important to highlight the specific challenges facing US neurosurgery during these difficult circumstances. In the present study, we have described our neurosurgery department’s unique experience during the COVID-19 pandemic.
Methods
We analyzed the following data points both before and during the first months of the COVID-19 pandemic: the number of patients infected with COVID-19 at our institution, changes in neurosurgical operative workflow, changes in neurosurgical outpatient and inpatient clinic workflows, resident redeployment statistics and changes in call schedules, and changes in neurosurgical education.
Results
At our institution, the adult surgery numbers decreased from 120 during the week of March 4–11, 2020 (before the World Health Organization had classified the COVID-19 outbreak as a pandemic) to 17 during the week of April 13–17, 2020. The number of pediatric surgeries decreased from 15 to 3 during the same period. Significantly more surgeries were cancelled than were delayed (P < 0.0001). A drastic decline occurred in the number of in-person neurosurgery clinic visits (97.12%) between March and April 2020 (P = 0.0020). The inpatient census declined from mid-March to mid-April 2020 by 44.68% compared with a 4.26% decline during the same period in 2019 (P < 0.0001). Finally, neurosurgery education has largely shifted toward video-conferencing sessions rather than in-person sessions.
Conclusion
By detailing our experience during the COVID-19 pandemic, we hope to have provided a detailed picture of the challenges facing neurosurgery within an academic medical center.
Key words: Coronavirus, COVID-19, Education, Neurosurgery
Abbreviations and Acronyms: COVID-19, Coronavirus disease 2019; NAT, Nucleic acid amplification test; NCCU, Neurocritical care unit
Introduction
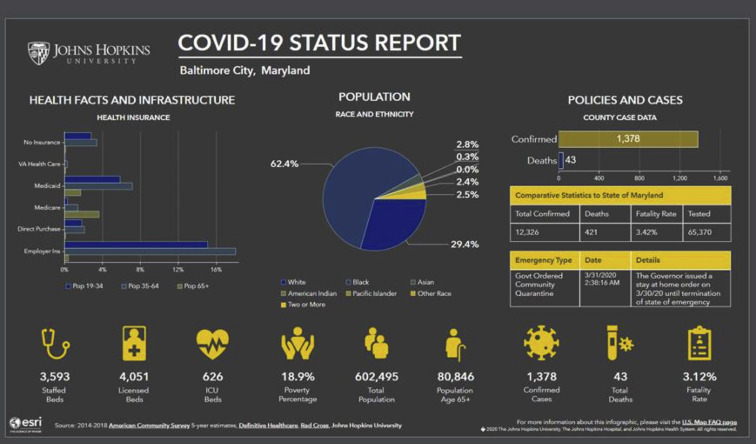
At the time of this writing (April 18, 2020), 2.3 million cases of coronavirus disease 2019 (COVID-19) have been confirmed worldwide, with ~740,500 cases in the United States and 12,300 cases within the state of Maryland (Supplementary Figure 1). At our institution, we are currently providing care for 251 patients with COVID-19.1 At all Johns Hopkins hospitals, the following patients will undergo COVID-19 testing in the absence of any specific coronavirus disease symptoms: admitted inpatients and patients undergoing a surgical procedure, electroconvulsive therapy, organ or stem cell transplantation procedures, and radiotherapy procedures within the radiation oncology department. To protect patients and hospital staff during the ongoing pandemic, various guidelines restricting hospital visitation have been implemented. In brief, no visitors are permitted into the hospital except under specific, extenuating circumstances (and with previous approval) such as end-of-life care, labor and delivery, certain pediatric cases, and emergency surgery. Elective and nonelective procedures have been cancelled on a rolling basis 3 weeks in advance to ensure essential resources and staff are available for the care of patients with COVID-19 and those requiring urgent care.
Supplementary Figure 1.
The Johns Hopkins University coronavirus disease 2019 (COVID-19) US tracking map, accessed April 18, 2020 (available at: coronavirus.jhu.edu/map.html). ICU, intensive care unit.
The Johns Hopkins University School of Medicine neurosurgery department includes 24 attending neurosurgeons and 27 residents, performing an average of 4500–5000 operative cases annually. Our faculty include the only 4 pediatric neurosurgeons within the state of Maryland. Physicians at our institution who had tested positive for COVID-19 toward the start of the crisis have now recovered and have returned to work. Within our neurosurgery department, 1 faculty member and 1 resident have tested positive for COVID-19. Within the city of Baltimore, our clinical services are performed across 2 campuses (The Johns Hopkins Hospital and The Johns Hopkins Bayview Medical Center), which collectively include 16 operating rooms, 32 intensive care unit beds, and 87 intermediate care or floor beds.
Impact on Operative Workflow
Overall, our entire institution experienced a total of 7600 cancelled surgical cases and other procedures between March 18, 2020 and April 17, 2020. In the neurosurgery department, the cancellation of operative cases varied by subspecialty, with the greatest number of cancellations affecting spine (n = 71), followed by tumor (n = 39), vascular (n = 20), functional (n = 19), and pediatric (n = 9) surgeries. Overall, the neurosurgical operative volumes decreased from 360 total cases in April 2019 to 112 projected total cases for April 2020, representing reduction of 68.89% (P = 0.012, Mann-Whitney U test with a normal approximation). A sharp decline occurred in the surgeries performed between March 4–11, 2020 and April 13–17, 2020. The adult surgery numbers decreased from 120 during March 4–11 to 17 during April 13–17. The number of pediatric surgeries decreased from 15 during March 4–11 to 3 during April 13–17. We chose the week of March 4–11 as a reference period because this was before the World Health Organization had classified the COVID-19 outbreak as a pandemic. The average operative room charges ± standard deviation and total hospital charges ± standard deviation for 2617 brain tumor surgeries conducted at The Johns Hopkins hospitals from 2016 to 2019 were calculated as $13,133.64 ± $7711.45 and $45,555.94 ± $35,858.18, respectively. Multiplying these averages by the 158 cancelled neurosurgical operations to estimate the lost clinical revenue resulted in an estimated $2,075,115.12 in lost operating room revenue and $7,197,838.52 in lost total hospital revenue.
Starting on March 15, 2020, weekly surveys were internally sent via e-mail to all neurosurgery attendings within our department. The surveys aimed to gauge physician perceptions of COVID-19's impact on neurosurgical workflow. The survey results are summarized in Table 1 . Overall, 158 elective surgeries were cancelled and 43 surgeries were delayed as per surgeon self-report. Cancellations were defined as elective operations that had been cancelled without any scheduled replacement date, and delays were defined as cancellations with a scheduled replacement date. The vast majority (71.5%) of surgeries were cancelled to follow national guidelines regarding the cancellation of elective surgeries issued by the Centers for Disease Control and Prevention. Only a small minority (1.9%) were cancelled because of a patient or provider testing positive for COVID-19.2 Significantly more surgeries were cancelled than delayed (P < 0.0001, Mann-Whitney U test). This finding likely represents the difficulty in rescheduling elective cases amid the uncertainty regarding the future workforce and resource availability and the lack of a consensus regarding when nationwide travel restrictions will be eased. Responses to the question “In the past week, how many of your cases were negatively affected intraoperatively for reasons related to COVID-19?” described challenges such as a relative lack of support staff and reflected the delays associated with the need for additional operating room setup time.
Table 1.
Coronavirus Disease 2019 Impact on Neurosurgical Practice Survey∗
| Question | Total Cases (n) |
|---|---|
| 1. In the past week, how many elective operations were cancelled in your practice for reasons related to COVID-19? (WITHOUT any scheduled replacement date) | 158 |
| How many cases were cancelled because of | |
| Patient following national guidelines for cancelling elective surgery | 113 |
| Patient concern about contracting COVID-19 during hospitalization | 23 |
| Lack of hospital beds | 18 |
| Travel restrictions (inability to travel to Johns Hopkins) | 5 |
| Surgeon quarantine | 2 |
| Patient testing positive for COVID-19 | 1 |
| 2. In the past week, how many elective operation cases were delayed in your practice for reasons related to COVID-19? (WITH a scheduled replacement date) | 43 |
| How many cases were delayed because of | |
| Patient following national guidelines for delaying elective surgery | 34 |
| Patient concern about contracting COVID-19 during hospitalization | 13 |
| Patient tested positive for COVID-19 | 0 |
| Travel restrictions (inability to travel to Johns Hopkins) | 0 |
| Surgeon quarantine | 0 |
| Lack of hospital beds | 0 |
| 3. In the past week, how many of your cases were negatively affected intraoperatively for reasons related to COVID-19? | 17 |
| How many of these cases were negatively affected because of | |
| Loss of co-surgeon | 0 |
| Loss of an anesthesiologist | 0 |
| Loss of resident/trainee | 1 |
| Loss of other intraoperative staff | 1 |
| Loss of vendor/medical device representative | 1 |
| 4. In the past week, how many scheduled clinic video visits in your practice were converted to telephone visits in real time? | 176 |
| How many clinic visits were converted to telephone visits because of | |
| Patient's inability to log into the video portal | 32 |
| Your inability to log into the video portal | 4 |
| Poor connection for the patient once you had logged into the video portal | 6 |
| Poor connection for you once you had logged into the video portal | 8 |
| 5. How many in-person clinical visits were cancelled for reasons related to COVID-19? | 147 |
| How many clinic patients' appointments were cancelled with | |
| No further follow-up scheduled | 66 |
| A change to a telephone call | 40 |
| A deferred visit until after the COVID-19 outbreak | 50 |
COVID-19, coronavirus disease 2019.
Data gathered from March 15 to April 18, 2020.
At our institution, the COVID-19 testing protocol for patients requiring a surgical procedure includes a COVID-19 screening test performed, ideally, within the 48 hours before the scheduled surgery but not >72 hours before the surgery. Asymptomatic hospital inpatients recovering from their surgical procedures and awaiting their COVID-19 nucleic acid amplification test (NAT) screening result have been treated similar to other non–COVID-19 patients in the hospital. Specifically, providers are expected to wear a face shield and surgical mask, and the patient stays in a standard, non-negative pressure room and are not required to wear a mask in their room. For urgent surgical procedures, if a NAT test was ordered but the results were not yet available, the procedure would either proceed in accordance with the COVID-19–negative patient protocol or be delayed, if possible. Finally, if a NAT test had not been ordered, patients would be treated similar to non–COVID-19 hospital patients.
Impact on Outpatient Clinic Workflow
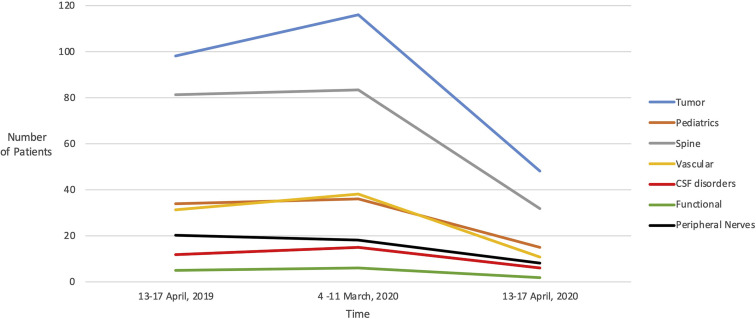
Through a retrospective analysis of our departmental outpatient clinic log via the electronic medical records (Epic Systems Corp., Madison, Wisconsin, USA), we tracked the number of in-person clinic visits within our department at specific points leading up to and during the COVID-19 pandemic (Table 2 ). In April 2019, the largest number of clinic patients was seen within the tumor service line (n = 98), followed by the spine service line (n = 81). The total in-person clinical visits increased across all specialties between April 13–17, 2019 (n = 281) and March 4–11, 2020 (n = 312), an 11.03% increase. In the next month (April 2020), a dramatic decline occurred in the in-person clinic visits across the department (n = 9), a reduction of 97.12%. Significantly fewer in-person clinic visits occurred during the first portion of April 2020 compared with March 2020 (P = 0.0020; Mann-Whitney U test) and during the first portion of April 2020 compared with April 2019 (P = 0.0020; Mann-Whitney U test). The distribution of in-person clinic visits, with April 2019 visits serving as a reference for March and April 2020, is shown in Figure 1 . Additionally, we noted a dramatic decrease in the number of non–COVID-19 patients with neurological complaints presenting to the emergency department. We also noted a decrease in the number of people undergoing evaluations for stroke. This specific issue of a decline in non–COVID-19 patients presenting to hospitals has been described in other reports,3 , 4 and we have planned to better characterize these data in the upcoming weeks.
Table 2.
In-Person Neurosurgery Clinic Visits Over Time
| Neurosurgeon Practice | Total In-Person Visits (n) |
||
|---|---|---|---|
| In April 2019 | In March 2020 | In April 2020 | |
| Tumor | 98 | 116 | 4 |
| Pediatrics | 34 | 36 | 1 |
| Spine | 81 | 83 | 3 |
| Vascular | 31 | 38 | 0 |
| CSF disorders | 12 | 15 | 1 |
| Functional | 5 | 6 | 0 |
| Peripheral nerves | 20 | 18 | 0 |
| Total | 281 | 312 | 9 |
| Mean ± SD | 40.14 ± 35.52 | 44.57 ± 40.34 | 1.29 ± 1.60 |
CSF, cerebrospinal fluid; SD, standard deviation.
Figure 1.
Average distribution of neurosurgery clinic visits before and during the coronavirus disease 2019 pandemic. CSF, cerebrospinal fluid.
Despite the marked reduction in the in-person visits over time, the adoption of telehealth in the clinic setting has been increasing, especially after the Centers for Medicare and Medicaid Services waived or relaxed the parameters required for performing telehealth visits on March 30, 2020.5 A total of 65 telehealth or video clinic visits occurred during April 13–17, 2020, comprising 92.62% of all clinic visits. Our survey of departmental staff demonstrated technical difficulties for both patients and providers that might have hindered even more widespread use of video technology for telemedicine. Of the 572 total video clinic visits during the entire survey period, 176 (30.7%) were forced to convert to telephone visits, most often because of patients' inability to properly log into the video portal system (Table 1). Of the 147 cancelled in-person visits during the study period, 40 (27.2%) had been changed upfront to telephone appointments, further reinforcing the importance of keeping alternative, low-resource methods of patient–provider communication available. Finally, 66 in-person clinic visits (44.9%) were cancelled without further follow-up appointments scheduled; thus, these patients remain at risk of being lost to follow-up (Table 1).
Impact on Inpatient Workflow
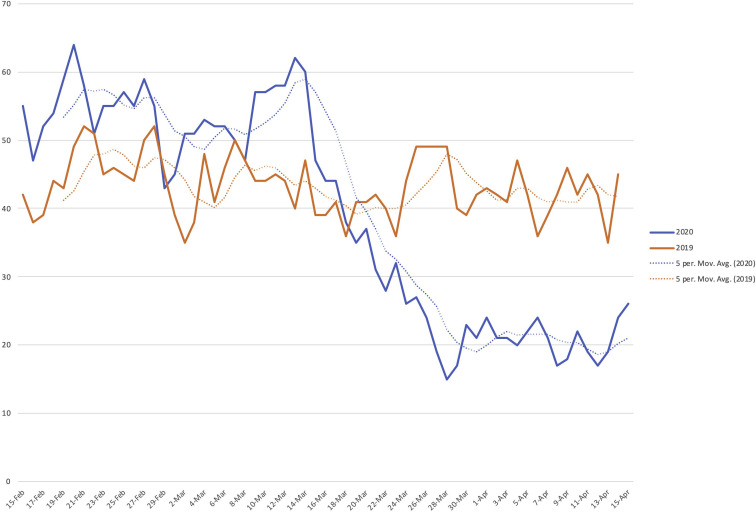
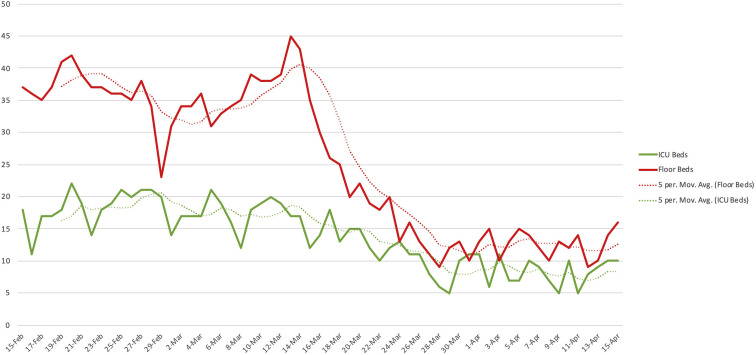
Regarding COVID-19's effect on neurosurgical hospital inpatients, a precipitous decline in the inpatient census occurred from mid-March 2020 to the end of the month, with 62 inpatients on March 13 compared with only 19 inpatients on March 27 (Supplementary Figure 2). The overall inpatient census declined from mid-March to mid-April 2020 by 44.68% compared with a 4.26% decline during the same period in 2019 (P < 0.0001; Mann-Whitney U test). These data emphasize the effect of cancelled elective cases on our inpatient census. The absence of a further precipitous decline toward the end of our study period might foreshadow a slow return to normalcy. The primary driver of the reduced census was a reduced floor bed census, which had decreased from a peak of 45 inpatients on March 13, 2020 to a trough of 9 patients on April 12, 2020, an 80% decrease in volume (Supplementary Figure 3).
Supplementary Figure 2.
Inpatient census data from February 15, 2020 to April 15, 2020.
Supplementary Figure 3.
Intensive care unit (ICU) and floor bed census data from February 15, 2020 to April 15, 2020.
Resident Redeployment and Change in Call Schedule
Medical and surgical residents around the United States have been experiencing drastic changes in their normal clinical schedules and academic curricula as hospitals attempt to manage large influxes of patients with COVID-19.6, 7, 8, 9 At our institution, 13 residents and 2 attendings volunteered to help care for patients with COVID-19 within a newly designated COVID-19 section within the neurocritical care unit (NCCU). To date, 2 residents have worked in the COVID-19 NCCU and 3 additional residents have pending shifts in the NCCU. A total of 2 residents and 2 physician assistants have covered non–COVID-19 NCCU shifts, and 2 additional residents and 5 additional physician assistants have been scheduled to work in the non–COVID-19 NCCU in the upcoming days. Additionally, nurses who were working in the NCCU before the pandemic have been redeployed to medicine departments to care for patients with COVID-19. Also, neurosurgical advanced practice providers (i.e., physician assistants and nurse practitioners) have been deployed to care for patients with COVID-19 to have adequately trained and prepared clinical staff available in the event of a second wave of COVID-19. Overall, an extensive redeployment of neurosurgical residents toward providing care for patients with COVID-19 has not yet been implemented at our institution, and our residents have primarily focused their clinical efforts on caring for patients within the non–COVID-19 NCCU.
Although the resident call schedule did not significantly change at The Johns Hopkins Bayview Medical Center, immediate changes were implemented to the resident call schedule as soon as COVID-19 cases began appearing at The Johns Hopkins Hospital in mid-March 2020. The faculty call schedule did not significantly change at either The Johns Hopkins Bayview Medical Center or The Johns Hopkins Hospital. In the pre–COVID-19 era, the inpatient team at The Johns Hopkins Bayview Medical Center included 1 chief resident, 1 junior resident, and a team of advanced practice providers. During the COVID-19 era, this team has continued to include 1 chief resident and 1 junior resident, with only 1 advanced practice provider, on service daily. The resident call schedule has remained grossly unchanged during the COVID-19 era at The Johns Hopkins Bayview Medical Center, with a “daytime” chief resident alternating with a home-call–based “nighttime” chief during weekdays. At The Johns Hopkins Hospital, previous 24-hour shifts have been replaced with 12-hours shifts to help reduce the physiologic stress among the residents. Our inpatient service was additionally downsized. Rather than 4 chief residents running 4 independent services, at present, 1 chief resident supervises the entire, downsized inpatient services. The remaining 3 chief residents only come to the hospital to cover operative duties. The 4 graduating chief residents had met their operative case minimum requirements in all categories before the COVID-19–associated schedule changes. No operative cases are double-scrubbed with a second resident. Two junior residents come into the hospital daily, with each caring for one half of the current inpatients for 7 days at a time. One junior resident answers the trauma and consultation pagers, performs rounds for all inpatients, operates alongside attendings, and returns home at the end of each day. A second junior resident similarly manages the pediatric neurosurgery service. The new resident schedule remains compliant with Accreditation Council for Graduate Medical Education work hour restrictions. All remaining junior residents work remotely from home on research projects and remain available as backup in the event that too many operative cases are present for the chief residents to cover alone. These backup junior residents have not yet been called in to assist with any surgical cases to date. Residents in their research and elective years are also working from home and available as backup, although residents currently completing enfolded clinical fellowships will occasionally come to the hospital to operate alongside their enfolded fellowship director.
Impact on Neurosurgical Education
Within our department, grand rounds have been held using online video-conferencing services (Zoom Video Communications, Inc., San Jose, California, USA) since March 19, 2020. The first grand rounds session had 53 participants compared with 115 participants at the most recent grand rounds session on April 16, 2020. Educational sessions have been conducted via video-conferencing services since March 24, 2020 and have consisted of neurosurgical faculty, residents, postdoctoral fellows, and fourth-year medical students presenting sessions that have varied from 30 to 90 minutes in length on a variety of education topics, including neuroanatomy, case conferences, and journal club. Such sessions occur 3 times daily, 5 days each week. With fewer operative cases, educational session attendance has markedly increased, having approximately doubled from 15 attendees at the first sessions on March 24 to 30 attendees during the most recent sessions on April 17. Additional virtual sessions have consisted of biweekly morbidity and mortality conferences and twice weekly faculty planning meetings. Additionally, a 3-hour lecture series on the fundamentals of critical care was created and made available to faculty, residents, and medical students during the first week of April 2020 in preparation for possible faculty and resident redeployment to COVID-19 units. Finally, our annual mock oral board session was converted to an online, Zoom-based format. The mock oral board sessions included the evaluation of 26 residents by 19 faculty over 3 hours, for a total of >45 hours of collective, interactive time between faculty and residents reviewing core clinical cases. We offered residents the option of having their mock oral board sessions recorded for self-review, which has been found in other surgical specialties to be associated with improved resident organization and decision-making on subsequent examinations.10
Discussion
We have presented our neurosurgery department's early experience during the COVID-19 pandemic by documenting how and to what extent hospital workflow and education have been altered. Overall, our report has highlighted the considerable difficulty in rescheduling elective neurosurgical operations amid efforts to ensure resource availability for patients with COVID-19. We also noted a significant decrease in the number of in-person clinic visits within our department with concomitant increased usage of telemedicine in an effort to preserve patient–provider communication as we have continued navigating the physical distancing restrictions. Our inpatient census has significantly decreased, and our residents have been partially redeployed to help care for patients with COVID-19 within the NCCU. Regular video-conferencing sessions have been implemented to ensure departmental meetings and educational activities continue; participation in these virtual meetings has increased during the duration of the pandemic. Our early estimates have demonstrated no notable increased rates of morbidity or mortality within our patient population during the pandemic, along with no known transmission of COVID-19 between patients and providers. We plan to continue closely monitoring outpatient clinic workflows, operative workflows, and the inpatient census daily during the coming months to help identify subtle spikes in COVID-19 positivity that might portend a future surge. Our current response has been informed by the available scientific data and expert consensus on COVID-19, and we believe that such scientific and expert consensus, partly informed by reports such as our present study, will help guide the response to a future pandemic surge.
A recent editorial by Arnaout et al.11 detailed the response of the neurosurgery departments at Brigham and Women's Hospital and Massachusetts General Hospital. Similar to our experience in preparing for the pandemic in a non–hot spot tertiary and quaternary care academic medical center, they described a reduction in elective operative volume, increased adoption of telemedicine in the outpatient setting, and a shift toward the use of teleconferencing services for neurosurgical educational activities since the onset of the pandemic.11 Arnaout et al.11 also discussed the predicted negative financial effects that the pandemic will have on hospitals generally, predicting that mergers and acquisitions, government bailouts, and the reduction of certain expenditures such as travel for meetings and residents dinners will be necessary to expedite the recovery of large healthcare systems in the wake of the pandemic. Eichberg et al.12 similarly described the University of Miami/Jackson Memorial Hospital response to the COVID-19 pandemic, discussing elective surgery cancellations, increased outpatient telemedicine usage, changes in resident and attending call schedules to ensure safety and limit exposure, and virtual models for neurosurgical resident education. Theofanis et al.,13 describing the experience at the Thomas Jefferson University Hospital, have further emphasized the importance of changes in neurosurgery resident clinical responsibilities and education to ensure physician safety. Our experience at a large, academic medical center is similar to the experiences described in these editorials, especially regarding the changes in operative volumes, outpatient services, call schedules, and resident education. We believe that our quantitative analysis of such changes is a novel contribution to the reports examining departmental responses to COVID-19 and hope that providing this data-driven description of our experience during the early first wave of the pandemic will be instructive to other departments during potential future waves.
Conclusions
By detailing our experience during the ongoing COVID-19 pandemic, we hope to paint a more detailed picture of the severe impact and challenges facing neurosurgery within an urban, academic, tertiary, and quaternary care medical center. We are confident that through collaboration, innovation, and perseverance, the practice of neurosurgery in the United States will remain able to adapt to the everchanging circumstances to ensure the best care for all our patients.
CRediT authorship contribution statement
Adham M. Khalafallah: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - review & editing. Adrian E. Jimenez: Conceptualization, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Ryan P. Lee: Formal analysis, Investigation, Writing - review & editing. Jon D. Weingart: Writing - review & editing. Nicholas Theodore: Writing - review & editing. Alan R. Cohen: Writing - review & editing. Rafael J. Tamargo: Writing - review & editing. Judy Huang: Writing - review & editing. Henry Brem: Writing - review & editing. Debraj Mukherjee: Supervision, Writing - review & editing.
Acknowledgments
The authors would like to acknowledge neurosurgery resident Ann Liu, MD, neurosurgery residency program coordinator Jamie Hoffberger, and Departments of Neurology and Neurosurgery assistant administrator Wendy Fang for their contributions to our report. We additionally would like to acknowledge the entire Johns Hopkins University School of Medicine Department of Neurosurgery faculty for completion of the weekly surveys described within our report.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Data
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;3099:1–2. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Healthcare Facilities: Preparing for Community Transmission. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html Available at:
- 3.Krumholz H.M. Where have all the heart attacks gone? The New York Times. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html?action=click&module=Top Stories&pgtype=Homepage Available at: Accessed May 16, 2020.
- 4.Kittleson M.M. The invisible hand—medical care during the pandemic. N Engl J Med. 2020;382:1586–1587. doi: 10.1056/NEJMp2006607. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services Physicians and Other Clinicians: CMS Flexibilities to Fight COVID-19. https://www.cms.gov/files/document/covid-19-physicians-and-practitioners.pdf Available at:
- 6.Bambakidis N.C., Tomei K.L. Impact of COVID-19 on neurosurgery resident training and education. https://doi.org/10.3171/2020.3.JNS20965 [e-pub ahead of print]. J Neurosurg. accessed April 18, 2020. [DOI] [PMC free article] [PubMed]
- 7.Choi B.D. A neurosurgery resident’s response to COVID-19: anything but routine. https://doi.org/10.3171/2020.4.JNS201028 [e-pub ahead of print]. J Neurosurg. accessed April 21, 2020. [DOI] [PMC free article] [PubMed]
- 8.Vargo E., Ali M., Henry F., Kmetz D., Krishnan J., Bologna R. Cleveland Clinic Akron general urology residency program’s COVID-19 experience. https://doi.org/10.1016/j.urology.2020.04.001 [e-pub ahead of print]. Urology. accessed April 21, 2020. [DOI] [PMC free article] [PubMed]
- 9.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;53:1689–1699. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kozol R.A., Giles M., Voytovich A. The value of videotape in mock oral board examinations. Curr Surg. 2004;61:511–514. doi: 10.1016/j.cursur.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Arnaout O., Patel A., Carter B., Chiocca E.A. Letter: adaptation under fire: two Harvard neurosurgical services during the COVID-19 pandemic. https://doi.org/10.1093/neuros/nyaa146 [e-pub ahead of print]. Neurosurgery. accessed April 18, 2020. [DOI] [PMC free article] [PubMed]
- 12.Eichberg D.G., Shah A.H., Luther E.M. Letter: academic neurosurgery department response to COVID-19 pandemic: the University of Miami/Jackson Memorial Hospital model. https://doi.org/10.1093/neuros/nyaa118 [e-pub ahead of print]. Neurosurgery. accessed May 16, 2020. [DOI] [PMC free article] [PubMed]
- 13.Theofanis T.N., Khanna O., Stefanelli A. Letter: neurosurgery residency in the COVID-19 era: experiences and insights from Thomas Jefferson University Hospital, Philadelphia, Pennsylvania. https://doi.org/10.1093/neuros/nyaa211 [e-pub ahead of print]. Neurosurgery. accessed May 16, 2020. [DOI] [PMC free article] [PubMed]