Abstract
Background
Individuals with pathogenic germline variants in DNA mismatch repair (MMR) genes are at increased risk of developing colorectal, endometrial and other cancers (Lynch syndrome, LS). While previous studies have extensively described cancer risks in LS, cancer risks in individuals from families without detectable MMR gene defects despite MMR deficiency (Lynch-like syndrome, LLS), and in individuals from families fulfilling the Amsterdam-II criteria without any signs of MMR deficiency (familial colorectal cancer type X, FCCX) are less well studied. The aim of this prospective study was to characterise the risk for different cancer types in LS, LLS, and FCCX, and to compare these with the cancer risks in the general population.
Methods
Data was taken from the registry of the German Consortium for Familial Intestinal Cancer, where individuals were followed up prospectively within the framework of an intensified surveillance programme at recommended annual examination intervals. A total of 1120 LS, 594 LLS, and 116 FCCX individuals were analysed. From this total sample, eight different cohorts were defined, in which age-dependent cumulative risks and standardised incidence ratios were calculated regarding the first incident occurrence of any, colorectal, stomach, small bowel, urothelial, female breast, ovarian, and endometrial cancer, separately for LS, LLS, and FCCX.
Results
The number of individuals at risk for first incident cancer ranged from 322 to 1102 in LS, 120 to 586 in LLS, and 40 to 116 in FCCX, depending on the cancer type of interest. For most cancer types, higher risks were observed in LS compared to LLS, FCCX, and the general population. Risks for any, colorectal, stomach, urothelial, and endometrial cancer were significantly higher in LLS compared to the general population. No significantly increased risks could be detected in FCCX compared to LLS patients, and the general population. Colorectal and endometrial cancer risks tended to be higher in LLS than in FCCX.
Conclusions
The characterisation of cancer risks in patients with LLS and FCCX is important to develop appropriate surveillance programmes for these specific intermediate risk groups. Larger prospective studies are needed to obtain more precise risk estimates.
Keywords: Lynch syndrome, Lynch-like syndrome, Familial colorectal cancer type X, Cancer risk, Prospective surveillance study
Background
Lynch syndrome (LS) is an autosomal dominantly inherited disorder, which is caused by pathogenic germline variants in one of the DNA mismatch repair (MMR) genes MLH1, MSH2, MSH6, PMS2 or in the EPCAM gene [1–3]. It is estimated that one of 279 individuals in the general population carries a pathogenic MMR gene variant [4]. LS is the most common hereditary colorectal cancer syndrome and is responsible for about 2 to 4% of all colorectal cancers [5–7]. Individuals with LS are at an increased risk of developing colorectal, endometrial and other types of cancer [8–12]. Early age of onset and familial clustering of cancers are clinical indicators of LS. In order to identify families suspected of having LS, the Amsterdam criteria and Bethesda guidelines were established [13–16]. An essential characteristic of LS is MMR deficiency (dMMR) of the tumours, as shown by reduced or lost immunohistochemical staining and/or microsatellite instability (MSI). A previous study by our group showed that in families meeting the Amsterdam or Bethesda criteria and having microsatellite instability-high colorectal cancer, only 53% carried a pathogenic germline MMR or EPCAM gene variant [17]. It has been suggested to designate individuals from families without a pathogenic germline MMR gene defect despite signs of dMMR as having Lynch-like syndrome (LLS) [18, 19]. In our previous study, it could be shown that in 37% of Amsterdam-II positive families no signs of dMMR could be found [17]. Individuals from Amsterdam-positive families without any signs of dMMR were characterised as a distinct risk group, the so-called “familial colorectal cancer type X” (FCCTX or FCCX) [18, 20]. The different clinical aspects and molecular features of LS, LLS, and FCCX are summarized elsewhere [21].
A comprehensive characterisation of cancer risks is an important prerequisite for developing appropriate cancer surveillance and prevention programmes. To date, many studies have characterised cancer risks in LS, also using prospective data, but fewer studies have characterised cancer risks in LLS and FCCX [7–12, 19–33]. The aim of the present analysis was therefore to estimate and compare the risk for different types of cancers in individuals with LS, LLS, and FCCX based on data from a prospective surveillance study of the German Consortium for Familial Intestinal Cancer. Additionally, we aimed to compare these risk estimations to cancer risks in the general population in Germany.
Methods
Study population
The study population was taken from a prospective registry study of the “German Consortium for Familial Intestinal Cancer” (formerly termed “German HNPCC Consortium”). Six university centres collected information about families suspected of having Lynch syndrome based on the Amsterdam-II criteria and/or revised Bethesda guidelines [15, 16]. All participants gave their written informed consent at registry inclusion, and the registry was approved by the Ethics Committees of all participating institutions.
A tissue sample (tumour or adenoma) of the index patient was examined for MMR deficiency (dMMR) using immunohistochemistry (IHC) and/or microsatellite analysis (MSA). In case of dMMR (or if no tissue sample was available), a germline mutation analysis of the MMR genes MLH1, MSH2, MSH6 and PMS2, and the EPCAM gene was carried out. Details about the diagnostic procedure are described elsewhere [17]. According to the results of the tissue and subsequent germline DNA analyses, index patients were classified as having LS (i.e. with a proven class 4/5 germline variant), LLS (i.e. fulfilling the Amsterdam-II and/or revised Bethesda criteria and not having a class 4/5 germline variant despite signs of dMMR in at least one family member), and FCCX (i.e. not having any signs of dMMR in the family while fulfilling the Amsterdam-II criteria). Relatives of LS index patients, who were predictively tested for the specific class 4/5 variant found in the index patient, were also considered as having LS if they were tested positive. Relatives of LLS and FCCX index patients were also considered as having LLS and FCCX, respectively. Individuals from families with dMMR due to MLH1 methylation were not regarded as having LLS.
Individuals with LS, LLS, or FCCX according to the above definitions were invited to participate in an intensified surveillance programme comprising annual colonoscopies, esophagogastroduodenoscopies, and gynaecological examinations. These individuals comprised both index patients and at-risk relatives. They were prospectively followed up and the result of each single surveillance examination was recorded in the registry.
Individuals were included in the present analysis if they had LS, LLS, or FCCX according to the above definitions. In the LS group, only MLH1, MSH2, and MSH6 carriers were included, whereas EPCAM and PMS2 carriers were excluded due to the low sample size. Additionally, all individuals had to have at least one colonoscopy after study registration and a prospective observation time of more than half a year.
Statistical analysis
From the above study population, eight different cohorts were defined and cancer risks were determined for the following eight types of cancers according to the International Classification of Diseases (ICD-10): any cancer (all Cxx without C77-C79), colorectal (C18-C20), stomach (C16), small bowel (C17), urothelial (C65-C68), female breast (C50), ovarian (C56), and endometrial cancer (C54.1). For each cancer type, its first incident occurrence was analysed. Individuals, who already had the cancer of interest before or within half a year after the start of prospective observation (prevalent cancers) were excluded. Therefore, patient numbers and observation times were different between the eight cohorts. Patients with prevalent cancers other than the cancer type of interest were not excluded. Females who had undergone a hysterectomy prior to the start of the prospective observation were excluded from the endometrial cancer and females with an oophorectomy from the ovarian cancer analyses.
Prospective observation started at the first colonoscopy after study registration or at age 25, whichever occurred last. Observation ended at the specific cancer event of interest, the age of 80, the last documented contact before May 12, 2019, or death, whichever came first. For calculations of endometrial cancer, hysterectomy was an additional reason for the end of observation, as well as oophorectomy for ovarian cancer. The incident occurrence of cancers other than the cancer type of interest was no reason for censoring [9, 10]. Cumulative cancer risks were determined for the different cancer types stratified by the three risk groups LS, LLS and FCCX, and by subgrouping the LS group into MLH1, MSH2 and MSH6 carriers. Risk estimation was done using the Kaplan-Meier product limit estimator accounting for the age at the beginning of prospective observation (left-truncation) [34]. For comparisons between groups, the log-rank test was used. The proportional hazards assumption was tested using scaled Schoenfeld residuals [35, 36]. In addition, the log-minus-log-transformed 95% confidence intervals of the product limit estimator were determined [34, 37]. In order to compare cancer risks with the general population, the standardised incidence ratio (SIR) was calculated, which is defined as the ratio between the observed number of cancers of interest and the expected number of cancers of interest in the general population. The number of expected cancers of interest was determined by the sum of all products of the age-specific incidence rates for the general population with the corresponding person-years. The source of age-specific incidence rates in 5-year-intervals for the general population in Germany (2000–2014) was the German Centre for Cancer Registry Data of the Robert Koch-Institute (Berlin, Germany. URL: www.krebsdaten.de/abfrage). As information regarding skin malignancies except malignant melanoma was not available for the general population, individuals with such neoplasms were excluded from the SIR calculation of the cancer type “any cancer”. Ninety-five percent confidence intervals for SIRs were calculated assuming a Poisson distribution.
All reported testing was two-sided, and p-values lower than 0.05 were considered statistically significant. Statistical analyses were carried out with R 3.4.2 for Windows (R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL: https://www.R-project.org).
Results
Patient characteristics
The study population comprised a total of 1830 patients, including 594 in the LLS, 116 in the FCCX group, and 1120 in the LS group (447 MLH1, 549 MSH2, and 124 MSH6 carriers). In total, 1200 individuals were index patients. The detailed patient characteristics for the eight different cancer types are summarised in Table 1 (a sex specific summary is shown in Additional file 1: Tables S1 and S2). The number of individuals at risk for first incident cancer ranged from 322 to 1102 in LS, 120 to 586 in LLS, and 40 to 116 in FCCX, depending on the cancer type. The median age at the start of the prospective observation ranged from 35 to 49 years depending on the risk group and cancer of interest. Table S3 in Additional file 1 shows a detailed summary of patient numbers, observation times and numbers of incident cancers. The types of cancers considered for the calculation of the type “any cancer” are given in Additional file 1: Table S4.
Table 1.
Patient characteristics
| FCCX | LLSa | LS | Total | |||
|---|---|---|---|---|---|---|
| MLH1 | MSH2 | MSH6 | ||||
| n = 116 | n = 594 | n = 447 | n = 549 | n = 124 | n = 1830 | |
| [Index patients] | [79] | [451] | [279] | [324] | [67] | [1200] |
| Individuals at risk, number [index patients] | ||||||
| Any | 40 [9] | 120 [11] | 116 [6] | 158 [12] | 48 [5] | 482 [43] |
| Colorectal | 42 [10] | 140 [25] | 133 [14] | 206 [36] | 57 [6] | 578 [91] |
| Stomach | 115 [78] | 584 [442] | 439 [271] | 539 [316] | 124 [67] | 1801 [1174] |
| Small bowel | 116 [79] | 586 [443] | 429 [263] | 536 [315] | 124 [67] | 1791 [1167] |
| Urothelial | 116 [79] | 585 [443] | 445 [277] | 524 [304] | 122 [67] | 1792 [1170] |
| Female breast | 58 [40] | 307 [224] | 214 [115] | 256 [138] | 60 [28] | 895 [545] |
| Ovarian | 56 [38] | 270 [190] | 187 [98] | 202 [105] | 48 [22] | 763 [453] |
| Endometrial | 53 [36] | 254 [186] | 152 [76] | 163 [83] | 45 [19] | 667 [400] |
| Age at start of prospective observation, median (interquartile range) | ||||||
| Any | 40 (35–50) | 39 (30–46) | 35 (29–43) | 36 (30–43) | 40 (34–48) | 38 (30–45) |
| Colorectal | 40 (35–51) | 41 (31–48) | 37 (30–45) | 39 (31–48) | 42 (36–51) | 39 (31–48) |
| Stomach | 49 (41–55) | 44 (38–51) | 44 (35–54) | 44 (36–52) | 44 (37–57) | 45 (37–53) |
| Small bowel | 49 (41–55) | 44 (38–52) | 44 (35–53) | 44 (36–52) | 44 (37–57) | 45 (37–53) |
| Urothelial | 49 (41–55) | 44 (38–51) | 44 (35–54) | 44 (36–52) | 44 (37–56) | 44 (37–53) |
| Female breast | 48 (41–55) | 44 (38–52) | 44 (35–54) | 44 (36–54) | 44 (38–55) | 44 (37–53) |
| Ovarian | 48 (41–53) | 44 (38–50) | 41 (34–52) | 42 (34–51) | 40 (37–49) | 43 (36–51) |
| Endometrial | 49 (41–55) | 43 (37–49) | 38 (32–47) | 40 (33–46) | 40 (37–47) | 41 (35–49) |
| Median follow-up time, person-years | ||||||
| Any | 6.8 | 6.9 | 6.5 | 6.4 | 6.5 | 6.5 |
| Colorectal | 7.1 | 6.3 | 6.5 | 7.0 | 7.1 | 6.8 |
| Stomach | 7.1 | 6.5 | 7.3 | 7.8 | 6.7 | 7.1 |
| Small bowel | 7.1 | 6.4 | 7.2 | 7.7 | 6.7 | 7.0 |
| Urothelial | 7.1 | 6.4 | 7.2 | 7.5 | 6.7 | 6.9 |
| Female breast | 7.2 | 6.5 | 6.7 | 8.1 | 7.1 | 7.1 |
| Ovarian | 7.3 | 6.3 | 6.5 | 7.0 | 7.3 | 6.8 |
| Endometrial | 7.2 | 5.9 | 6.0 | 6.0 | 7.1 | 6.1 |
| Cumulative follow-up time, person-years | ||||||
| Any | 308 | 838 | 819 | 1105 | 326 | 3395 |
| Colorectal | 329 | 964 | 938 | 1509 | 417 | 4157 |
| Stomach | 854 | 4019 | 3300 | 4222 | 843 | 13239 |
| Small bowel | 858 | 4011 | 3212 | 4164 | 843 | 13088 |
| Urothelial | 858 | 4003 | 3314 | 4006 | 829 | 13010 |
| Female breast | 420 | 2093 | 1539 | 1963 | 451 | 6467 |
| Ovarian | 417 | 1805 | 1292 | 1397 | 368 | 5278 |
| Endometrial | 376 | 1581 | 994 | 1019 | 315 | 4285 |
| Individuals with incident cancer, number | ||||||
| Any | 2 | 8 | 13 | 27 | 3 | 53 |
| Colorectal | 0 | 6 | 7 | 19 | 2 | 34 |
| Stomach | 0 | 4 | 4 | 5 | 0 | 13 |
| Small bowel | 0 | 1 | 9 | 14 | 0 | 24 |
| Urothelial | 1 | 4 | 9 | 19 | 0 | 33 |
| Female breast | 1 | 3 | 3 | 6 | 4 | 17 |
| Ovarian | 0 | 0 | 0 | 5 | 0 | 5 |
| Endometrial | 0 | 5 | 9 | 13 | 1 | 28 |
an = 320 with deficient MMR protein expression in MLH1, n = 127 in MSH2, n = 26 in MSH6. IHC was not performed in n = 121 individuals
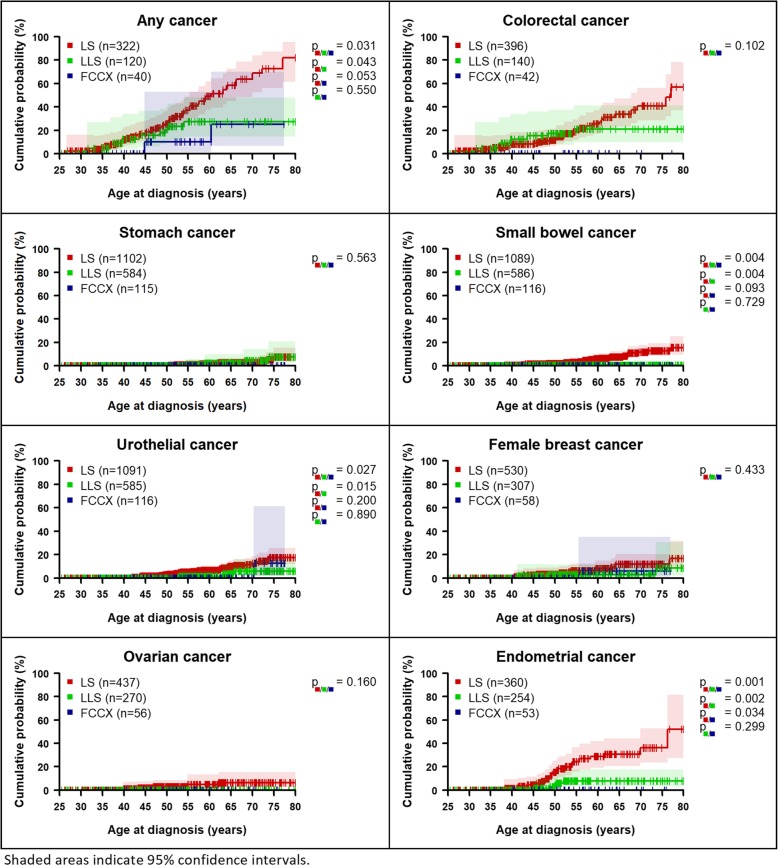
Comparison of cancer risks between LS, LLS, and FCCX
The risk for any cancer by the age of 70 years was 63.7% (95%CI 48.5–78.8%) for LS, 27.3% (95%CI 14.5–47.8%) for LLS, and 25.0% (95%CI 6.6–70.2%) for FCCX patients (Fig. 1 and Table 2). Cumulative cancer risk was higher for the LS group than for LLS or FCCX for any cancer, small bowel, urothelial, female breast, ovarian, and endometrial cancer. The risks in the FCCX group were lower than in the LLS group for all cancer types, except for female breast and ovarian cancer. The risk of any cancer, small bowel, urothelial, and endometrial cancer was statistically significantly higher in the LS group than in the LLS group. No statistically significant differences for “any cancer” were found in the sex-specific analyses, whereas significant differences were also observed in males for small bowel and urothelial cancer, but not in females. No incident colorectal cancer events were observed in the FCCX group. LLS patients showed a lower colorectal cancer risk (21.0%, 95%CI 9.9–41.3%) than LS patients (40.9%, 95%CI 28.3–56.4%) at age 70, but the difference between LS, LLS, and FCCX was not statistically significant (p = 0.102). There were no significant differences between the LLS and FCCX groups (Additional file 1: Figure S7).
Fig. 1.
Age-dependent cumulative cancer risks
Table 2.
Cumulative cancer risks (%) by age
| LS | |||||||
|---|---|---|---|---|---|---|---|
| Cancer type | Age (years) | FCCX | LLS | LS | MLH1 | MSH2 | MSH6 |
| Any | 40 | 0.0 (−) | 12.5 (4.2–34.1) | 12.2 (6.4–22.5) | 14.0 (5.5–33.1) | 13.8 (5.7–31.4) | 0.0 (−) |
| 50 | 10.0 (1.5–52.7) | 20.5 (9.7–40.4) | 25.6 (17.5–36.4) | 24.1 (12.8–42.6) | 31.6 (19.5–48.5) | 7.7 (1.1–43.4) | |
| 60 | 10.0 (1.5–52.7) | 27.3 (14.5–47.8) | 49.0 (37.5–61.9) | 44.0 (26.6–66.3) | 60.3 (44.0–77.1) | 20.9 (5.3–63.3) | |
| 70 | 25.0 (6.6–70.2) | 27.3 (14.5–47.8) | 63.7 (48.5–78.8) | 52.0 (31.9–75.3) | 72.2 (53.2–88.4) | 36.7 (12.7–78.6) | |
| Colorectal | 40 | 0.0 (−) | 12.4 (4.2–33.8) | 8.4 (3.7–18.3) | 10.0 (3.3–27.9) | 9.5 (2.9–28.3) | 0.0 (−) |
| 50 | 0.0 (−) | 17.4 (7.5–37.4) | 11.8 (6.3–21.5) | 10.0 (3.3–27.9) | 16.3 (7.7–32.7) | 0.0 (−) | |
| 60 | 0.0 (−) | 21.0 (9.9–41.3) | 25.4 (16.8–37.2) | 23.4 (10.8–46.6) | 33.7 (21.0–51.1) | 0.0 (−) | |
| 70 | 0.0 (−) | 21.0 (9.9–41.3) | 40.9 (28.3–56.4) | 30.4 (14.8–55.8) | 49.1 (32.9–68.1) | 14.3 (2.1–66.6) | |
| Stomach | 40 | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) |
| 50 | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | |
| 60 | 0.0 (−) | 2.4 (0.6–9.9) | 1.7 (0.6–4.6) | 0.9 (0.1–6.4) | 2.4 (0.8–7.4) | 0.0 (−) | |
| 70 | 0.0 (−) | 4.6 (1.4–14.5) | 2.9 (1.3–6.5) | 2.5 (0.6–9.9) | 3.6 (1.3–9.5) | 0.0 (−) | |
| Small bowel | 40 | 0.0 (−) | 0.0 (−) | 0.6 (0.1–4.1) | 1.4 (0.2–9.8) | 0.0 (−) | 0.0 (−) |
| 50 | 0.0 (−) | 0.6 (0.1–4.4) | 1.8 (0.7–4.8) | 1.4 (0.2–9.8) | 2.5 (0.8–7.7) | 0.0 (−) | |
| 60 | 0.0 (−) | 0.6 (0.1–4.4) | 5.9 (3.5–10.1) | 5.0 (1.9–12.8) | 7.6 (4.0–14.2) | 0.0 (−) | |
| 70 | 0.0 (−) | 0.6 (0.1–4.4) | 11.7 (7.6–17.6) | 11.5 (5.8–22.0) | 13.9 (8.0–23.4) | 0.0 (−) | |
| Urothelial | 40 | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) |
| 50 | 0.0 (−) | 0.0 (−) | 2.7 (1.3–5.6) | 0.9 (0.1–6.1) | 4.7 (2.1–10.3) | 0.0 (−) | |
| 60 | 0.0 (−) | 1.5 (0.4–5.9) | 6.5 (4.0–10.4) | 5.7 (2.4–13.3) | 8.4 (4.7–14.7) | 0.0 (−) | |
| 70 | 0.0 (−) | 5.7 (2.0–16.0) | 12.5 (8.3–18.5) | 11.3 (5.6–22.0) | 16.3 (9.9–26.2) | 0.0 (−) | |
| Female breast | 40 | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) | 0.0 (−) |
| 50 | 0.0 (−) | 2.9 (0.7–11.4) | 3.4 (1.3–8.7) | 2.0 (0.3–13.6) | 1.6 (0.2–10.6) | 12.0 (3.1–40.6) | |
| 60 | 5.9 (0.9–35.0) | 2.9 (0.7–11.4) | 7.9 (4.2–14.7) | 7.3 (2.4–21.2) | 6.8 (2.6–17.1) | 12.0 (3.1–40.6) | |
| 70 | 5.9 (0.9–35.0) | 2.9 (0.7–11.4) | 11.9 (6.8–20.3) | 7.3 (2.4–21.2) | 12.2 (5.5–25.8) | 20.8 (7.0–53.0) | |
| Ovarian | 40 | 0.0 (−) | 0.0 (−) | 1.0 (0.1–7.1) | 0.0 (−) | 2.4 (0.3–16.1) | 0.0 (−) |
| 50 | 0.0 (−) | 0.0 (−) | 2.9 (0.9–8.7) | 0.0 (−) | 6.8 (2.2–19.6) | 0.0 (−) | |
| 60 | 0.0 (−) | 0.0 (−) | 4.9 (1.7–13.3) | 0.0 (−) | 10.7 (4.0–26.9) | 0.0 (−) | |
| 70 | 0.0 (−) | 0.0 (−) | 6.4 (2.6–15.5) | 0.0 (−) | 14.0 (5.9–31.2) | 0.0 (−) | |
| Endometrial | 40 | 0.0 (−) | 0.0 (−) | 1.4 (0.2–9.3) | 0.0 (−) | 3.1 (0.4–20.2) | 0.0 (−) |
| 50 | 0.0 (−) | 4.3 (1.4–12.8) | 15.3 (9.1–25.0) | 14.5 (6.8–29.6) | 16.8 (7.9–33.8) | 10.0 (1.5–52.7) | |
| 60 | 0.0 (−) | 7.7 (3.2–17.6) | 28.8 (19.1–41.9) | 19.2 (9.2–37.5) | 40.1 (24.5–60.7) | 10.0 (1.5–52.7) | |
| 70 | 0.0 (−) | 7.7 (3.2–17.6) | 36.1 (23.4–52.7) | 35.4 (13.8–72.2) | 44.1 (27.8–64.5) | 10.0 (1.5–52.7) | |
Numbers in brackets are 95% confidence intervals
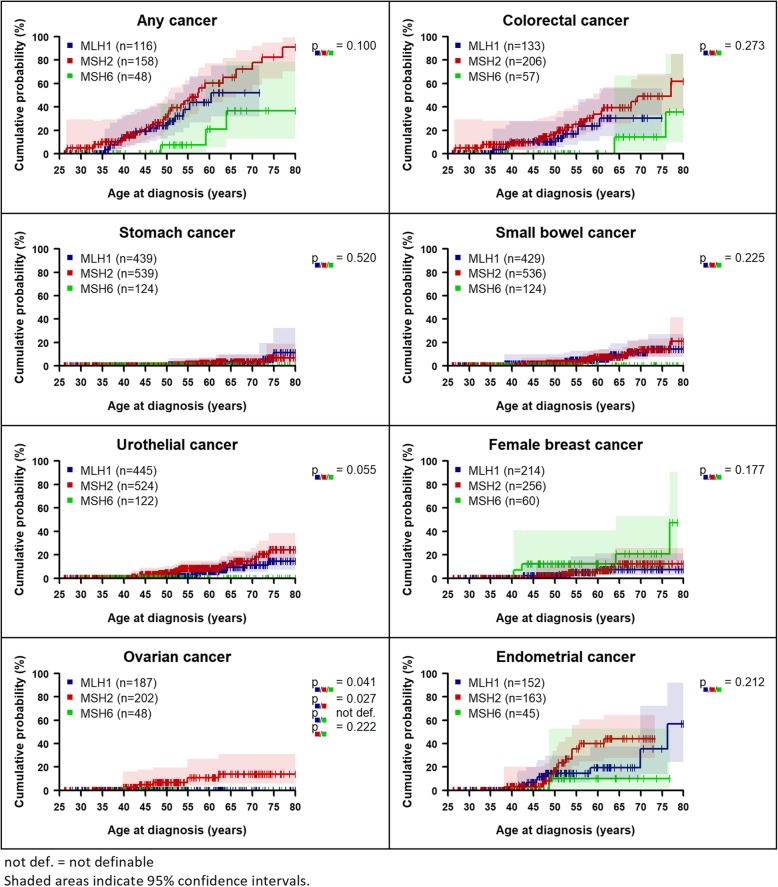
Within the LS group, higher cancer risks were found for MLH1 and MSH2 carriers than for MSH6 carriers for any cancer, colorectal, stomach, small bowel, urothelial, and endometrial cancer (Fig. 2 and Table 2, Additional file 1: Figure S8). The risk of ovarian cancer was highest in MSH2 carriers (Additional file 1: Tables S5 and S6) with statistically significant differences between the three genes (p = 0.041). For urothelial cancer, risk differences were borderline non-significant (p = 0.055).
Fig. 2.
Age-dependent cumulative cancer risks of LS patients by gene
The LLS group comprised 320 individuals from families with MMR deficiency in the MLH1 protein, 127 in MSH2, and 26 in MSH6. The remaining 121 patients could not be assigned to a specific MMR protein, because only MSA but not IHC had been performed. There were no statistically significant differences in cancer risks between MLH1, MSH2 and MSH6 in the LLS group except for urothelial cancer in women (p = 0.003). Women from LLS families with MSH2 MMR deficiency had a higher risk for urothelial cancer compared to women from families with MMR deficiency in MLH1 and MSH6.
Moreover, we found significant differences in cancer risks between index patients and the at-risk relatives for colorectal and endometrial cancer in the LLS group. Index patients had a higher risk (p = 0.027) of colorectal cancer at age 70 (50.0%, 95%CI 19.6–88.9%) compared to their relatives (13.2%, 95%CI 4.4–35.9%), but a lower risk (p = 0.010) of endometrial cancer (4.0%, 95%CI 1.0–15.3% vs. 23.1%, 95%CI 8.1–55.8%).
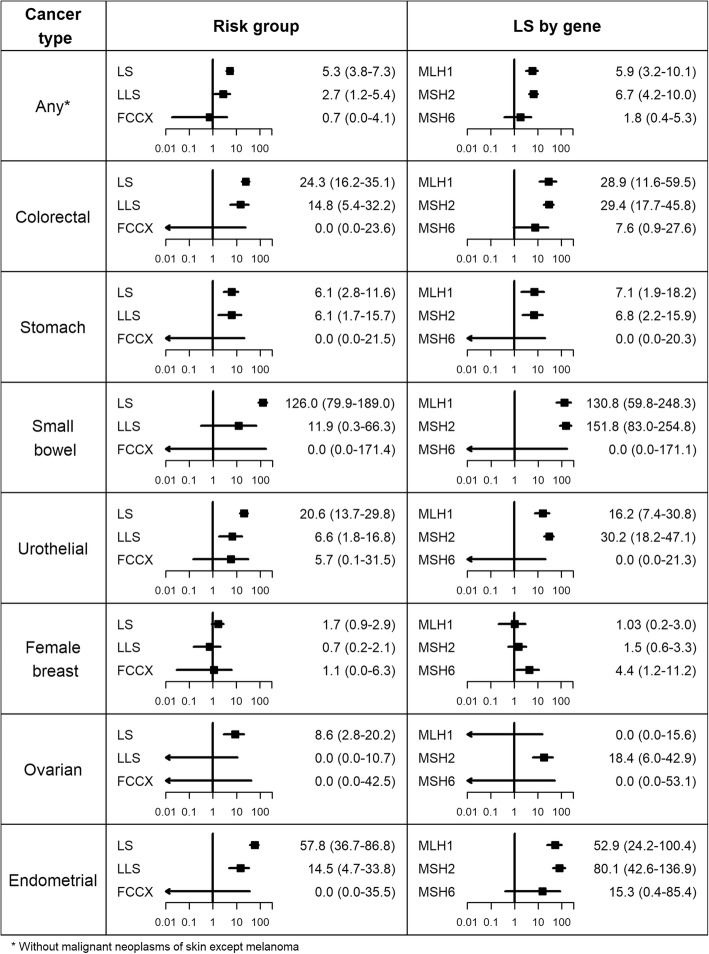
Comparison with general population risks
Compared to the general population, cancer risks in the LS group were higher for all cancer types. These results were statistically significant for all cancer types regardless of sex, with the exception of female breast cancer (Fig. 3, Additional file 1: Figures S9 and S10). Standardised incidence ratios (SIRs) ranged from 5.3 for “any cancer” to 126.0 for small bowel cancer. Increased SIRs in MLH1 and MSH2 carriers were found in male LS patients for all types of cancer. These results were also statistically significant, except for stomach cancer where only MLH1 carriers had a significantly increased risk. The SIR of colorectal cancer was also elevated in male MSH6 carriers, although not showing statistical significance. Female MLH1 and MSH2 carriers had elevated SIRs for any cancer, colorectal, stomach, small bowel, urothelial, and endometrial cancer, which were all statistically significant, with the exception of stomach cancer in MLH1 carriers. In addition, female MSH2 carriers showed a significantly increased risk of ovarian cancer. The SIRs for female breast cancer were only slightly marginally elevated for MLH1 and MSH2 carriers compared to the general population, while the SIR for MSH6 carriers was statistically significantly higher.
Fig. 3.
Comparison with general population risks: standardised incidence ratios (SIRs) with 95% confidence intervals
Larger SIRs were observed in the LLS group for any cancer, colorectal, stomach, small bowel, urothelial, and endometrial cancer, which were statistically significant except for small bowel cancer. Regarding sex, significantly increased SIRs in the LLS group were detected in females for endometrial and urothelial cancer, as well as in males for colorectal and stomach cancer. Cancer risks were not statistically significantly increased in the FCCX group compared to the general population.
Discussion
In this prospective study, we investigated different organ-specific cancer risks in Lynch syndrome, Lynch-like syndrome, and familial colorectal cancer type X. To the best of our knowledge, this is the first report comparing cumulative cancer incidences in these three risk groups based on prospective follow-up data. We found higher cancer risks for LS than for LLS and FCCX patients. Some cancer risks, such as colorectal and endometrial cancer, tended to be higher in LLS than in the FCCX group, but this did not reach statistical significance.
A large number of retro- and prospective studies have investigated cancer risks in LS patients [7–12, 19, 22–33]. The largest prospective studies to date, based on internationally pooled data gathered in the Prospective Lynch Syndrome Database (PLSD), provided risk estimates for various cancer types in LS patients stratified by age, gene, and sex [9–12]. The cumulative risks in LS patients found in our study are in agreement with those PLSD studies, which did not include the data of our present study [9–11]. We found statistically significant risk differences between MLH1, MSH2, and MSH6 carriers only for ovarian cancer, where MSH2 carriers had the highest risk. This agrees with the results from the PLSD and other studies showing that MSH2 carriers have higher ovarian cancer risks than MLH1 or MSH6 carriers [25, 26]. Compared to the general population, we found a statistically significantly increased risk of female breast cancer (SIR = 4.4, 95%CI 1.2–11.2) only in MSH6 carriers. This is in agreement with results from a retrospective study of Roberts et al. [38], but in disagreement with others studies, which have reported either no increased risks for LS patients or elevated risks in MLH1 carriers [28, 29].
Compared to LS, considerably fewer studies have investigated cancer risks in LLS and FCCX. Rodriguez-Soler and colleagues performed a population-based study with 1705 consecutively included colorectal cancer patients comparing cancer risks between LS, LLS, and sporadic cancer [19]. They found that the risk of cancer in LLS is lower compared to LS, but higher compared to sporadic cancer. In our study, we found significantly lower cancer risks in LLS compared to LS for any cancer, small bowel, urothelial, and endometrial cancer. However, compared to the general population, the risks of any cancer, colorectal, stomach, urothelial, and endometrial cancer were significantly elevated for LLS as well as for LS. This is of particular interest, as LLS patients may need specific surveillance programmes. It has been suggested that individuals with a history of cancer, as well as their first-degree relatives should undergo colonoscopic screening every 3 years [39]. Regular esophagogastroduodenoscopy might also add value, as our study showed an increased risk of stomach and small bowel cancer. However, it should be noted that the LLS group is heterogeneous as it may contains both individuals with sporadic tumours with somatic MMR variants and individuals with MMR germline variants, which were not detected.
We did not find any significant differences in cancer risks between MLH1, MSH2 and MSH6 in the LLS group with the exception of urothelial cancer in women, where women from families with a MMR deficiency in the MSH2 protein showed a higher risk. There were also no significant differences of cancer risks between index patients and the at-risk relatives in the LLS group, except for colon cancer and endometrial cancer, where index patients had a higher risk of colon cancer but a lower risk of endometrial cancer compared to the at-risk relatives. These results need to be validated in larger, ideally international collaborative studies, before specific screening recommendations can be made for this risk group.
Lindor et al. compared the incidence of different cancer types in individuals from Amsterdam-I families with and without dMMR [20]. They concluded that individuals without dMMR in their family have a lower incidence of cancer than those with dMMR. Choi et al. compared the risks of first and metachronous colorectal cancers in LS with those of members of FCCX families and found higher risks in individuals with LS compared to FCCX family members [23]. We observed lower cancer risks for FCCX compared to LS and LLS groups, although these were not statistically significant. In addition, we found no significantly higher risks for individuals of the FCCX group compared with the general population. This raises the question of whether FCCX patients require a different surveillance programme compared to LS and LLS patients, and whether screening similar to the general population would be sufficient for this group. Analyses with a larger number of FCCX individuals would be helpful in order to investigate this further.
A major strength of the present study was its prospective design, which mitigates the problem of overestimation of cancer risks due to ascertainment bias in clinic-based retrospective studies [40]. However, some limitations also need to be noted. One was the comparably low sample size and observation time in the FCCX group, resulting in large confidence intervals of the risk estimates. Secondly, observation times above the age of 60 years were comparably low. Thirdly, since all of these patients were under intensified colonoscopic surveillance, with possible colorectal cancer prevention (to an unknown extent) due to adenoma removal, the colorectal cancer risk estimates obtained in our study do not reflect the natural course of disease. Fourthly, there could be some underestimation of SIRs for endometrial cancer since general population incidences were only available for the ICD-10 group C54 and not specifically for C54.1.
Conclusions
This prospective study provides data on cancer risk estimation in patients with LS and particularly with LLS and FCCX, which is important to develop appropriate surveillance programmes for these specific intermediate risk groups. However, before specific surveillance recommendations can be given, larger prospective studies are needed to obtain more precise risk estimates. We propose international databases for LLS and FCCX, similar to the Prospective Lynch Syndrome Database (PLSD), be set up.
Supplementary information
Additional file 1 Table S1. Characteristics of female patients. Table S2. Characteristics of male patients. Table S3. Number of patients, observation times (person-years) and number of incident cancers. Table S4. Types of incident cancers considered as “any cancer”. Table S5. Cumulative cancer risks (%) by age for female patients. Table S6. Cumulative cancer risks (%) by age for male patients. Figure S7. Age-dependent cumulative cancer risks by risk group and sex. Figure S8. Age-dependent cumulative cancer risks of LS patients by gene and sex. Figure S9. Comparison with general population risks: standardised incidence ratios (SIRs) with 95% confidence interval for female patients. Figure S10. Comparison with general population risks: standardised incidence ratios (SIRs) with 95% confidence interval for male patients.
Acknowledgements
The authors are grateful to all study participants and their families, the collaborating physicians and study nurses in the clinical centres, the centre for reference pathology in Cologne, and the centre for documentation and biometry in Leipzig. We acknowledge support from the German Research Foundation (DFG) and University of Leipzig within the programme of Open Access Publishing.
Abbreviations
- CI
Confidence interval
- dMMR
Mismatch repair deficiency
- FCCX
Familial colorectal cancer type X
- ICD
International Statistical Classification of Diseases and Related Health Problems
- IHC
Immunohistochemistry
- LLS
Lynch-like syndrome
- LS
Lynch syndrome
- MMR
Mismatch repair
- MSA
Microsatellite analysis
- MSI
Microsatellite instability
- SIR
Standardised incidence ratio
Authors’ contributions
The study was designed by KB and CE. KB carried out the statistical analysis. All authors interpreted the results. KB and CE drafted the manuscript. The decision to submit the manuscript was made by all authors. All authors read and approved the final manuscript.
Funding
The study was supported by grants from the German Cancer Aid. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by all responsible ethic committees of the participating clinical centres and complies with the ethical standards of the Declaration of Helsinki. All participants gave their written informed consent at registry inclusion. The ethic committees were: Ethik-Kommission der Medizinischen Fakultät der Ruhr-Universität Bochum, Ethikkommission an der Medizinischen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn, Ethikkommission an der Technischen Universität Dresden, Ethikkommission an der Medizinischen Fakultät der Heinrich-Heine-Universität Düsseldorf, Ethikkommission der Medizinischen Fakultät Heidelberg, Ethikkommission bei der Medizinischen Fakultät der LMU München.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. Matthias Kloor is an Editorial Board Member of BMC Cancer.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12885-020-06926-x.
References
- 1.Lynch HT, de la Chapelle A. Hereditary colorectal Cancer. N Engl J Med. 2003;348:919–932. doi: 10.1056/NEJMra012242. [DOI] [PubMed] [Google Scholar]
- 2.Lynch HT, Snyder CL, Shaw TG, Heinen CD, Hitchins MP. Milestones of Lynch syndrome: 1895–2015. Nat Rev Cancer. 2015;15:181–194. doi: 10.1038/nrc3878. [DOI] [PubMed] [Google Scholar]
- 3.Ligtenberg MJ, Kuiper RP, Chan TL, Goossens M, Hebeda KM, Voorendt M, et al. Heritable somatic methylation and inactivation of MSH2 in families with Lynch syndrome due to deletion of the 3′ exons of TACSTD1. Nat Genet. 2009;41:112–117. doi: 10.1038/ng.283. [DOI] [PubMed] [Google Scholar]
- 4.Win Aung Ko, Jenkins Mark A., Dowty James G., Antoniou Antonis C., Lee Andrew, Giles Graham G., Buchanan Daniel D., Clendenning Mark, Rosty Christophe, Ahnen Dennis J., Thibodeau Stephen N., Casey Graham, Gallinger Steven, Le Marchand Loïc, Haile Robert W., Potter John D., Zheng Yingye, Lindor Noralane M., Newcomb Polly A., Hopper John L., MacInnis Robert J. Prevalence and Penetrance of Major Genes and Polygenes for Colorectal Cancer. Cancer Epidemiology Biomarkers & Prevention. 2016;26(3):404–412. doi: 10.1158/1055-9965.EPI-16-0693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamberti C, Mangold E, Pagenstecher C, Jungck M, Schwering D, Bollmann M, et al. Frequency of hereditary non-polyposis colorectal cancer among unselected patients with colorectal cancer in Germany. Digestion. 2006;74:58–67. doi: 10.1159/000096868. [DOI] [PubMed] [Google Scholar]
- 6.Hampel H, Frankel WL, Martin E, Arnold M, Khanduja K, Kuebler P, et al. Feasibility of screening for Lynch syndrome among patients with colorectal cancer. J Clin Oncol. 2008;26:5783–5788. doi: 10.1200/JCO.2008.17.5950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yurgelun MB, Kulke MH, Fuchs CS, Allen BA, Uno H, Hornick JL, et al. Cancer Susceptibility Gene Mutations in Individuals With Colorectal Cancer. J Clin Oncol. 2017;35:1086–195a. doi: 10.1200/JCO.2016.71.0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engel C, Loeffler M, Steinke V, Rahner N, Holinski-Feder E, Dietmaier W, et al. Risks of less common cancers in proven mutation carriers with Lynch syndrome. J Clin Oncol. 2012;30:4409–4415. doi: 10.1200/JCO.2012.43.2278. [DOI] [PubMed] [Google Scholar]
- 9.Møller P, Seppälä TT, Bernstein I, Holinski-Feder E, Sala P, Evans DG, et al. Cancer risk and survival in path_MMR carriers by gene and gender up to 75 years of age. A report from the Prospective Lynch Syndrome Database. Gut. 2018;67:1306–16. [DOI] [PMC free article] [PubMed]
- 10.Møller P, Seppälä T, Bernstein I, Holinski-Feder E, Sala P, Evans DG, et al. Incidence of and survival after subsequent cancers in carriers of pathogenic MMR variants with previous cancer: a report from the prospective Lynch syndrome database. Gut. 2017;66:1657–1664. doi: 10.1136/gutjnl-2016-311403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Møller P, Seppälä T, Bernstein I, Holinski-Feder E, Sala P, Evans DG, et al. Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective Lynch syndrome database. Gut. 2017;66:464–472. doi: 10.1136/gutjnl-2015-309675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dominguez-Valentin Mev, Sampson Julian R., Seppälä Toni T., ten Broeke Sanne W., Plazzer John-Paul, Nakken Sigve, Engel Christoph, Aretz Stefan, Jenkins Mark A., Sunde Lone, Bernstein Inge, Capella Gabriel, Balaguer Francesc, Thomas Huw, Evans D. Gareth, Burn John, Greenblatt Marc, Hovig Eivind, de Vos tot Nederveen Cappel Wouter H., Sijmons Rolf H., Bertario Lucio, Tibiletti Maria Grazia, Cavestro Giulia Martina, Lindblom Annika, Della Valle Adriana, Lopez-Köstner Francisco, Gluck Nathan, Katz Lior H., Heinimann Karl, Vaccaro Carlos A., Büttner Reinhard, Görgens Heike, Holinski-Feder Elke, Morak Monika, Holzapfel Stefanie, Hüneburg Robert, Knebel Doeberitz Magnus von, Loeffler Markus, Rahner Nils, Schackert Hans K., Steinke-Lange Verena, Schmiegel Wolff, Vangala Deepak, Pylvänäinen Kirsi, Renkonen-Sinisalo Laura, Hopper John L., Win Aung Ko, Haile Robert W., Lindor Noralane M., Gallinger Steven, Le Marchand Loïc, Newcomb Polly A., Figueiredo Jane C., Thibodeau Stephen N., Wadt Karin, Therkildsen Christina, Okkels Henrik, Ketabi Zohreh, Moreira Leticia, Sánchez Ariadna, Serra-Burriel Miquel, Pineda Marta, Navarro Matilde, Blanco Ignacio, Green Kate, Lalloo Fiona, Crosbie Emma J., Hill James, Denton Oliver G., Frayling Ian M., Rødland Einar Andreas, Vasen Hans, Mints Miriam, Neffa Florencia, Esperon Patricia, Alvarez Karin, Kariv Revital, Rosner Guy, Pinero Tamara Alejandra, Gonzalez María Laura, Kalfayan Pablo, Tjandra Douglas, Winship Ingrid M., Macrae Finlay, Möslein Gabriela, Mecklin Jukka-Pekka, Nielsen Maartje, Møller Pål. Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the Prospective Lynch Syndrome Database. Genetics in Medicine. 2019;22(1):15–25. doi: 10.1038/s41436-019-0596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vasen H. F. A., Mecklin J. -P., Meera Khan P., Lynch H. T. The International Collaborative Group on Hereditary Non-Polyposis Colorectal Cancer (ICG-HNPCC) Diseases of the Colon & Rectum. 1991;34(5):424–425. doi: 10.1007/BF02053699. [DOI] [PubMed] [Google Scholar]
- 14.Rodriguez-Bigas M. A., Boland C. R., Hamilton S. R., Henson D. E., Srivastava S., Jass J. R., Khan P. M., Lynch H., Smyrk T., Perucho M., Sobin L. A National Cancer Institute Workshop on Hereditary Nonpolyposis Colorectal Cancer Syndrome: Meeting Highlights and Bethesda Guidelines. JNCI Journal of the National Cancer Institute. 1997;89(23):1758–1762. doi: 10.1093/jnci/89.23.1758. [DOI] [PubMed] [Google Scholar]
- 15.VASEN H, WATSON P, MECKLIN J, LYNCH H. New clinical criteria for hereditary nonpolyposis colorectal cancer (HNPCC, Lynch syndrome) proposed by the International Collaborative Group on HNPCC☆. Gastroenterology. 1999;116(6):1453–1456. doi: 10.1016/S0016-5085(99)70510-X. [DOI] [PubMed] [Google Scholar]
- 16.Umar A., Boland C. R., Terdiman J. P., Syngal S., Chapelle A. d. l., Ruschoff J., Fishel R., Lindor N. M., Burgart L. J., Hamelin R., Hamilton S. R., Hiatt R. A., Jass J., Lindblom A., Lynch H. T., Peltomaki P., Ramsey S. D., Rodriguez-Bigas M. A., Vasen H. F. A., Hawk E. T., Barrett J. C., Freedman A. N., Srivastava S. Revised Bethesda Guidelines for Hereditary Nonpolyposis Colorectal Cancer (Lynch Syndrome) and Microsatellite Instability. JNCI Journal of the National Cancer Institute. 2004;96(4):261–268. doi: 10.1093/jnci/djh034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinke V, Holzapfel S, Loeffler M, Holinski-Feder E, Morak M, Schackert HK, et al. Evaluating the performance of clinical criteria for predicting mismatch repair gene mutations in Lynch syndrome: a comprehensive analysis of 3,671 families. Int J Cancer. 2014;135:69–77. doi: 10.1002/ijc.28650. [DOI] [PubMed] [Google Scholar]
- 18.Da Silva FC, Wernhoff P, Dominguez-Barrera C, Dominguez-Valentin M. Update on hereditary colorectal Cancer. Anticancer Res. 2016;36:4399–4405. doi: 10.21873/anticanres.10983. [DOI] [PubMed] [Google Scholar]
- 19.Rodríguez-Soler M, Pérez-Carbonell L, Guarinos C, Zapater P, Castillejo A, Barberá VM, et al. Risk of cancer in cases of suspected lynch syndrome without germline mutation. Gastroenterology. 2013;144:926–932. doi: 10.1053/j.gastro.2013.01.044. [DOI] [PubMed] [Google Scholar]
- 20.Lindor Noralane M., Rabe Kari, Petersen Gloria M., Haile Robert, Casey Graham, Baron John, Gallinger Steve, Bapat Bharati, Aronson Melyssa, Hopper John, Jass Jeremy, LeMarchand Loic, Grove John, Potter John, Newcomb Polly, Terdiman Jonathan P., Conrad Peggy, Moslein Gabriella, Goldberg Richard, Ziogas Argyrios, Anton-Culver Hoda, de Andrade Mariza, Siegmund Kim, Thibodeau Stephen N., Boardman Lisa A., Seminara Daniela. Lower Cancer Incidence in Amsterdam-I Criteria Families Without Mismatch Repair Deficiency. JAMA. 2005;293(16):1979. doi: 10.1001/jama.293.16.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Erbao, Xu Xiaojing, Liu Tianshu. Hereditary Nonpolyposis Colorectal Cancer and Cancer Syndromes: Recent Basic and Clinical Discoveries. Journal of Oncology. 2018;2018:1–11. doi: 10.1155/2018/3979135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biller LH, Syngal S, Yurgelun MB. Recent advances in Lynch syndrome. Familial Cancer. 2019;18:211–219. doi: 10.1007/s10689-018-00117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choi Yun-Hee, Lakhal-Chaieb Lajmi, Kröl Agnieszka, Yu Bing, Buchanan Daniel, Ahnen Dennis, Le Marchand Loic, Newcomb Polly A, Win Aung Ko, Jenkins Mark, Lindor Noralane M, Briollais Laurent. Risks of Colorectal Cancer and Cancer-Related Mortality in Familial Colorectal Cancer Type X and Lynch Syndrome Families. JNCI: Journal of the National Cancer Institute. 2018;111(7):675–683. doi: 10.1093/jnci/djy159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Engel Christoph, Rahner Nils, Schulmann Karsten, Holinski–Feder Elke, Goecke Timm O., Schackert Hans K., Kloor Matthias, Steinke Verena, Vogelsang Holger, Möslein Gabriela, Görgens Heike, Dechant Stefan, von Knebel Doeberitz Magnus, Rüschoff Josef, Friedrichs Nicolaus, Büttner Reinhard, Loeffler Markus, Propping Peter, Schmiegel Wolff. Efficacy of Annual Colonoscopic Surveillance in Individuals With Hereditary Nonpolyposis Colorectal Cancer. Clinical Gastroenterology and Hepatology. 2010;8(2):174–182. doi: 10.1016/j.cgh.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Watson Patrice, Vasen Hans F.A., Mecklin Jukka-Pekka, Bernstein Inge, Aarnio Markku, Järvinen Heikki J., Myrhøj Torben, Sunde Lone, Wijnen Juul T., Lynch Henry T. The risk of extra-colonic, extra-endometrial cancer in the Lynch syndrome. International Journal of Cancer. 2008;123(2):444–449. doi: 10.1002/ijc.23508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vasen HF, Stormorken A, Menko FH, Nagengast FM, Kleibeuker JH, Griffioen G, et al. MSH2 mutation carriers are at higher risk of cancer than MLH1 mutation carriers: a study of hereditary nonpolyposis colorectal cancer families. J Clin Oncol. 2001;19:4074–4080. doi: 10.1200/JCO.2001.19.20.4074. [DOI] [PubMed] [Google Scholar]
- 27.Therkildsen C, Ladelund S, Smith-Hansen L, Lindberg LJ, Nilbert M. Towards gene- and gender-based risk estimates in Lynch syndrome; age-specific incidences for 13 extra-colorectal cancer types. Br J Cancer. 2017;117:1702–1710. doi: 10.1038/bjc.2017.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aarnio M, Sankila R, Pukkala E, Salovaara R, Aaltonen LA, de La Chapelle A, et al. Cancer risk in mutation carriers of DNA-mismatch-repair genes. Int J Cancer. 1999;81:214–218. doi: 10.1002/(SICI)1097-0215(19990412)81:2<214::AID-IJC8>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 29.Scott Rodney J., McPhillips Mary, Meldrum Cliff J., Fitzgerald Patrick E., Adams Kirsten, Spigelman Allan D., du Sart Desiree, Tucker Kathy, Kirk Judy. Hereditary Nonpolyposis Colorectal Cancer in 95 Families: Differences and Similarities between Mutation-Positive and Mutation-Negative Kindreds. The American Journal of Human Genetics. 2001;68(1):118–127. doi: 10.1086/316942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harkness EF, Barrow E, Newton K, Green K, Clancy T, Lalloo F, et al. Lynch syndrome caused by MLH1 mutations is associated with an increased risk of breast cancer: a cohort study. J Med Genet. 2015;52:553–556. doi: 10.1136/jmedgenet-2015-103216. [DOI] [PubMed] [Google Scholar]
- 31.van der Post RS, Kiemeney LA, Ligtenberg MJL, Witjes JA. Hulsbergen-van de Kaa CA, Bodmer D, et al. Risk of urothelial bladder cancer in Lynch syndrome is increased, in particular among MSH2 mutation carriers. J Med Genet. 2010;47:464–470. doi: 10.1136/jmg.2010.076992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barrow E, Robinson L, Alduaij W, Shenton A, Clancy T, Lalloo F, et al. Cumulative lifetime incidence of extracolonic cancers in Lynch syndrome: a report of 121 families with proven mutations. Clin Genet. 2009;75:141–149. doi: 10.1111/j.1399-0004.2008.01125.x. [DOI] [PubMed] [Google Scholar]
- 33.Bonadona V, Bonaïti B, Olschwang S, Grandjouan S, Huiart L, Longy M, et al. Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA. 2011;305:2304–2310. doi: 10.1001/jama.2011.743. [DOI] [PubMed] [Google Scholar]
- 34.Klein J, Moeschberger M. Survival Analysis. Techniques for Censored and Truncated Data. New York: Springer; 1997. [Google Scholar]
- 35.Grambsch P, Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:512–526. [Google Scholar]
- 36.Therneau T. R documentation: Package survival version 2.44–1.1, function cox.zph: Test the proportional hazards assumption of a cox regression [Internet, cited 2019 June 13]. Available from: https://stat.ethz.ch/R-manual/R-devel/library/survival/html/cox.zph.html.
- 37.Borgan Ø, Liestøl K. A Note on Confidence Intervals and Bands for the Survival Function Based on Transformations. Scand J Stat. 1990;17:35–41.
- 38.Roberts ME, Jackson SA, Susswein LR, Zeinomar N, Ma X, Marshall ML, et al. MSH6 and PMS2 germ-line pathogenic variants implicated in Lynch syndrome are associated with breast cancer. Genet Med. 2018;20:1167–1174. doi: 10.1038/gim.2017.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Picó María Dolores, Castillejo Adela, Murcia Óscar, Giner-Calabuig Mar, Alustiza Miren, Sánchez Ariadna, Moreira Leticia, Pellise María, Castells Antoni, Carrillo-Palau Marta, Ramon y Cajal Teresa, Gisbert-Beamud Alexandra, Llort Gemma, Yagüe Carmen, López-Fernández Adriá, Alvarez-Urturi Cristina, Cubiella Joaquin, Rivas Laura, Rodríguez-Alcalde Daniel, Herraiz Maite, Garau Catalina, Dolz Carlos, Bujanda Luis, Cid Lucia, Povés Carmen, Garzon Marta, Salces Inmaculada, Ponce Marta, Hernández-Villalba Luís, Alenda Cristina, Balaguer Francesc, Soto Jose-Luis, Jover Rodrigo. Clinical and Pathological Characterization of Lynch-Like Syndrome. Clinical Gastroenterology and Hepatology. 2020;18(2):368-374.e1. doi: 10.1016/j.cgh.2019.06.012. [DOI] [PubMed] [Google Scholar]
- 40.Carayol J, Khlat M, Maccario J, Bonaïti-Pellié C. Hereditary non-polyposis colorectal cancer: current risks of colorectal cancer largely overestimated. J Med Genet. 2002;39:335–339. doi: 10.1136/jmg.39.5.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1 Table S1. Characteristics of female patients. Table S2. Characteristics of male patients. Table S3. Number of patients, observation times (person-years) and number of incident cancers. Table S4. Types of incident cancers considered as “any cancer”. Table S5. Cumulative cancer risks (%) by age for female patients. Table S6. Cumulative cancer risks (%) by age for male patients. Figure S7. Age-dependent cumulative cancer risks by risk group and sex. Figure S8. Age-dependent cumulative cancer risks of LS patients by gene and sex. Figure S9. Comparison with general population risks: standardised incidence ratios (SIRs) with 95% confidence interval for female patients. Figure S10. Comparison with general population risks: standardised incidence ratios (SIRs) with 95% confidence interval for male patients.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.