Coronavirus disease 2019 (COVID-19) has rapidly spread around the world in the past 3 months and has now become a global public health crisis. The mortality of COVID-19 in some European cities exceeds 11%, and the fatality rate is up to 61.5% in critical patients, especially in mechanically ventilated patients [1]. Once mild to moderate patients progress to critical illness, the incidence of septic shock, intubation, and myocardial injury increases significantly. Mechanical ventilation patients need more sedative, analgesic, and neuromuscular blocker drugs, which will affect the patient’s hemodynamic status and airway expectoration ability [2]. Previous studies have confirmed that high-flow nasal cannula (HFNC) can reduce the endotracheal intubation rate and mortality in patients with respiratory failure [3]. However, this therapy of COVID-19 cannot improve the pathophysiology of ventilation-perfusion defects and atelectasis, which can be proved by autopsies, i.e., small airways are blocked by mucus plugs [4]. Awake prone position could improve the mismatch of ventilation-perfusion and open the atelectatic lungs by adequate sputum drainage. So far, the role of early awake prone position (PP) combined with HFNC therapy in the treatment of severe COVID-19 has not been reported. So, we conducted a retrospective observation study in three hospitals in Wuhu and Maanshan cities in Anhui Province.
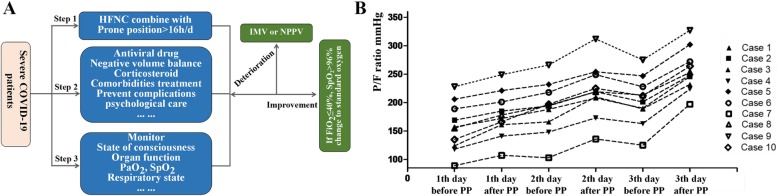
From January 1 to April 2, 2020, 79 patients with coronavirus infection were screened. Ten was severe and all of them received early awake PP combined with HFNC treatment (Table 1). COVID-19 was diagnosed using sputum or throat swab determined by real-time reverse transcription polymerase chain reaction (RT-PCR) assay. The severity of disease was graded according to the Guidelines for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infection by the National Health Commission (trial version 5). The target time of prone positioning is more than 16 h per day and can be appropriately shortened according to the patient’s tolerance. Target SpO2 was more than 90% of adult non-pregnant patients (Fig. 1a).
Table 1.
Clinical characteristics and outcomes of COVID patients treated by prone position combine with HFNC
| Case no. | Gender | Age (years) | Comorbidity | Imagine features | Time from illness onset to hospitalization | Baseline PF (onset of HFNC) (mmHg) | WBC (× 109/L) | L (× 109/L) | PCT (ng/ml) | CRP (mg/L) | D-dimer (mg/L) | Intubation | Length of stay (days) | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 54 | Bilateral lobes, GGO and consolidation | 10 | 156.8 | 5.2 | 0.8 | 0.1 | 111.2 | 2.4 | No | 18 | Survivor | |
| 2 | Female | 56 | DM | Bilateral lobes, GGO | 5 | 169.2 | 5.4 | 1.0 | 0.3 | 8.2 | 1.0 | No | 19 | Survivor |
| 3 | Male | 47 | DM, HBP | Bilateral pulmonary infiltration | 10 | 123.6 | 9.6 | 1.0 | 0.2 | 84.0 | 0.2 | No | 11 | Survivor |
| 4 | Female | 65 | Bilateral lobes, GGO | 6 | 117.7 | 6.6 | 0.4 | 0.2 | 97.3 | 3.0 | No | 11 | Survivor | |
| 5 | Female | 51 | HBP | Bilateral pulmonary infiltration | 10 | 205.8 | 6.2 | 0.6 | 0.1 | 110.2 | 0.6 | No | 11 | Survivor |
| 6 | Male | 43 | Bilateral lobes, GGO and consolidation | 6 | 188.8 | 2.2 | 0.8 | < 0.1 | 27.7 | 1.2 | No | 15 | Survivor | |
| 7 | Female | 48 | HBP | Bilateral lobes, GGO and consolidation | 9 | 89.1 | 4.7 | 0.5 | < 0.1 | 47.4 | 0.9 | No | 30 | Survivor |
| 8 | Female | 51 | Bilateral lobes, GGO and consolidation | 5 | 155.5 | 9.5 | 2.0 | < 0.1 | 68.3 | 0.4 | No | 22 | Survivor | |
| 9 | Male | 56 | HBP | Bilateral lobes, GGO and consolidation | 6 | 227.8 | 3.6 | 1.1 | < 0.1 | 15.3 | 2.3 | No | 19 | Survivor |
| 10 | Male | 31 | Bilateral lobes, GGO and consolidation | 1 | 134.7 | 4.2 | 1.4 | 0.2 | 9.5 | 1.9 | No | 21 | Survivor |
Fig. 1.
a The protocol treatment of severe COVID-19 patients. b The change of PaO2/FiO2 in the first 3 days between onset of HFNC and 4–6 h after PP therapy in severe COVID-19 patients
All the severe patients, with PF < 300 mmHg, developed mild respiratory alkalosis and no alkalemia at the beginning of HFNC treatment. After PP, compared with the baseline, the median PaCO2 increases slightly [32.3 (29.3–34.0) vs. 29.7 (28.0–32.0), p < 0.001]. The median PaO2/FiO2 (PF) was elevated significantly after PP (Fig. 1b). None of the patients progressed to critical condition or needed endotracheal intubation.
When the condition of patients with severe coronavirus deteriorated rapidly and the mortality rate was unacceptably high [1], we then put forward a concept “reduce the proportion of severe COVID-19 conversion to critical illness,” based on the experience summarized during the treatment of COVID-19 in Anhui, China. Early awake PP combined with HFNC therapy was one of the most important strategies to avoid intubation and reduce the requirement for medical staff. A previous study reported that early application of PP with HFNC therapy, especially in patients with moderate ARDS, may help avoid intubation but not in the several ARDS group [5]. However, in non-infected severe ARDS patients with a PF < 100 mmHg, 5 of 6 patients avoided intubation. In our research, the lowest P/F ratio was 89 mmHg, and the patient was successfully discharged without invasive mechanical ventilation. The main reason for the patients’ intolerance of PP is discomfort, anxiety [6], and the inability to change position. Our strategy was psychological care and a slight change of position every 2 h.
Compared to non-invasive ventilation (NIV), patients felt more comfortable when using HFNC therapy, and the demand for medical staff was reduced. Awake PP combined with HFNC therapy could be used safely and effectively in severe COVID-19 patients, and it may reduce the conversion to critical illness and the need for tracheal intubation.
Acknowledgements
Not applicable.
Abbreviations
- COVID-19
Coronavirus disease 2019
- HFNC
High-flow nasal cannula
- PP
Prone position
- PF
PaO2/FiO2
- NIV
Non-invasive ventilation
Authors’ contributions
Lu, the corresponding author, was responsible for the conceptualization of the study and the revision and approval of this manuscript. Xu, Qin, and Wang participated in the design, drafted the manuscript, and collected the data and were responsible for its accuracy. Zha helped to revise the manuscript. All authors contributed to the data analysis and interpretation. All authors read and approved the final manuscript.
Funding
This work was supported, in part, by the Anhui Provincial Special Project of Central Government Guiding Local Science and Technology Development of China (201907d07050001) and the special fund for coronavirus disease 2019 of Wuhu (no. 2020dx2-1 and 2020dx2-2).
Availability of data and materials
Data are available on request.
Ethics approval and consent to participate
The study was approved by the First Affiliated Hospital of Wannan Medical College and participating institution ethics committees (approval number 2019-97). Written consent was obtained from each patient or his/her authorized representatives.
Consent for publication
All authors have approved the manuscript and its publication.
Competing interests
The authors have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qiancheng Xu, Tao Wang and Xuemei Qin contributed equally to this work.
References
- 1.Yang Xiaobo, Yu Yuan, Xu Jiqian, Shu Huaqing, Xia Jia'an, Liu Hong, Wu Yongran, Zhang Lu, Yu Zhui, Fang Minghao, Yu Ting, Wang Yaxin, Pan Shangwen, Zou Xiaojing, Yuan Shiying, Shang You. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. The Lancet Respiratory Medicine. 2020;8(5):475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 3.Thille AW, Muller G, Gacouin A, Coudroy R, Decavele M, Sonneville R, Beloncle F, Girault C, Dangers L, Lautrette A, et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: a randomized clinical trial. JAMA. 2019;322(15):1465–1475. doi: 10.1001/jama.2019.14901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Q, Wang RS, Qu GQ, Wang YY, Liu P, Zhu YZ, Fei G, Ren L, Zhou YW, Liu L. Gross examination report of a COVID-19 death autopsy. Fa Yi Xue Za Zhi. 2020;36(1):21–23. doi: 10.12116/j.issn.1004-5619.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit Care. 2020;24(1):28. doi: 10.1186/s13054-020-2738-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiSilvio B, Young M, Gordon A, Malik K, Singh A, Cheema T. Complications and outcomes of acute respiratory distress syndrome. Crit Care Nurs Q. 2019;42(4):349–361. doi: 10.1097/CNQ.0000000000000275. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available on request.