Abstract
Background
To describe the infection control strategy to achieve zero nosocomial transmission of symptomatic coronavirus disease (COVID-19) due to SARS-CoV-2 during the prepandemic phase (the first 72 days after announcement of pneumonia cases in Wuhan) in Hong Kong.
Methods
Administrative support with the aim of zero nosocomial transmission by reducing elective clinical services, decanting wards, mobilizing isolation facilities, providing adequate personal protective equipment, coordinating laboratory network for rapid molecular diagnosis under 4-tier active surveillance for hospitalized patients and outpatients, and organizing staff forum and training was implemented under the framework of preparedness plan in Hospital Authority. The trend of SARS-CoV-2 in the first 72 days was compared with that of SARS-CoV 2003.
Results
Up to day 72 of the epidemic, 130 (0.40%) of 32,443 patients being screened confirmed to have SARS-CoV-2 by reverse transcription polymerase chain reaction. Compared with SARS outbreak in 2003, the SARS-CoV-2 case load constituted 8.9% (130 SARS-CoV-2/1458 SARS-CoV) of SARS-CoV infected cases at day 72 of the outbreak. The incidences of nosocomial acquisition of SARS-CoV per 1,000 SARS-patient-day and per 100 SARS-patient-admission were 7.9 and 16.9, respectively, which were significantly higher than the corresponding incidences of SARS-CoV-2 (zero infection, P <.001).
Conclusions
Administrative support to infection control could minimize the risk of nosocomial transmission of SARS-CoV-2.
Key Words: Coronavirus, Health care workers, Outbreak
Introduction
Pandemic infection of coronavirus disease 2019 (COVID-19) due to severe acute respiratory syndrome-associated coronavirus-2 (SARS-CoV-2) was declared by World Health Organization (WHO) on March 11, 2020, which is 72 days after announcement of a cluster of patients with community acquired pneumonia in Wuhan, Hubei Province by National Health Commission of the People's Republic of China (NHCPRC) on December 31, 2019 (day 1).1 On day 72, the COVID-19 had already spread to 113 countries or territories in 5 continents, resulting in 118,319 confirmed cases all over the world.2 While the epidemic of COVID-19 is slowing down in China, there is active community transmission in Europe and North America, resulting in 30% of disease burden outside China.2 Overwhelming number of COVID-19 infections could not only paralyze the health care system, but more importantly, result in nosocomial outbreaks, associated with increased morbidity and mortality of the hospitalized patients and health care workers (HCWs). Up to February 24, 2020 (day 56), NHCPRC reported that 3,387 HCWs were infected with COVID-19, resulting in 22 (0.6%) deaths.3 This had exceeded the number of HCWs death due to SARS in mainland China in 2003.4 In Hong Kong, 8 HCWs succumbed as a result of nosocomial acquisition of SARS-CoV.5 The top priority of our pandemic preparedness is to achieve zero COVID-19 infection among HCWs in Hong Kong.
Here, we report our infection control strategy and epidemiology of SARS-CoV-2 in the first 72 days (from the official announcement of pneumonia by NHCPRC to the declaration of pandemic infection by WHO), using the historical data on the epidemiology of SARS-CoV in Hong Kong for comparison.
Methods
Comparative epidemiology of SARS-CoV and SARS-CoV-2
After the outbreak of SARS-CoV in 2003, a total of 1,755 persons were infected and 299 persons (17.0%) died.6 Of 386 HCWs infected with SARS-CoV in Hong Kong, 8 of them (2.2%) succumbed. Six HCWs (2 doctors, 1 nurse, and 3 health care assistants) of 8 were the employee of Hospital Authority, the governing body of all 43 public hospitals, divided into 7 cluster-networks, responsible for 90% of inpatient service in Hong Kong. A “Select Committee to inquire into the handling of the Severe Acute Respiratory Syndrome outbreak by the Government and the Hospital Authority” was established by the Legislative Council of the Hong Kong Special Administrative Region, China in order to examine the performance and accountability of the Government and Hospital Authority and their officers at policy-making and management levels.7 The report includes temporal sequence of events and daily statistics on SARS patients with breakdown by HCWs and patients. The information was retrieved for analyzing the epidemiology of SARS in 2003.8 When a novel coronavirus disease, known as COVID-19 due to SARS-CoV-2 emerged 17 years later, Hospital Authority immediately activated our response plan to combat the epidemic and to prevent nosocomial transmission and outbreaks of SARS-CoV-2. The clinical perspective of infection control measures was reported recently.9 The epidemiology of SARS-CoV-2 until March 11, 2020 (at day 72 after the official announcement of a cluster of pneumonia of unknown etiology in Wuhan, Hubei Province, by NHCPRC) in Hong Kong was analyzed. This was also the date when WHO declared the COVID-19 pandemic. Our results were compared with the epidemiological data of SARS-CoV at day 72 (April 11, 2003) after the official announcement of atypical pneumonia in Guangdong Province, China on February 11, 2003. In addition, we also compared the epidemiology of SARS-CoV-2 in Hong Kong with Hubei Province, China, which was the most severe affected region by SARS-CoV-2, and the other countries or areas with uncontrolled local transmission at day 72, including Republic of Korea, Singapore, Islamic Republic of Iran, and Italy, using the publicly accessible information from the WHO website.10
Preparedness plan of Hospital Authority to combat against SARS-CoV-2 in Hong Kong
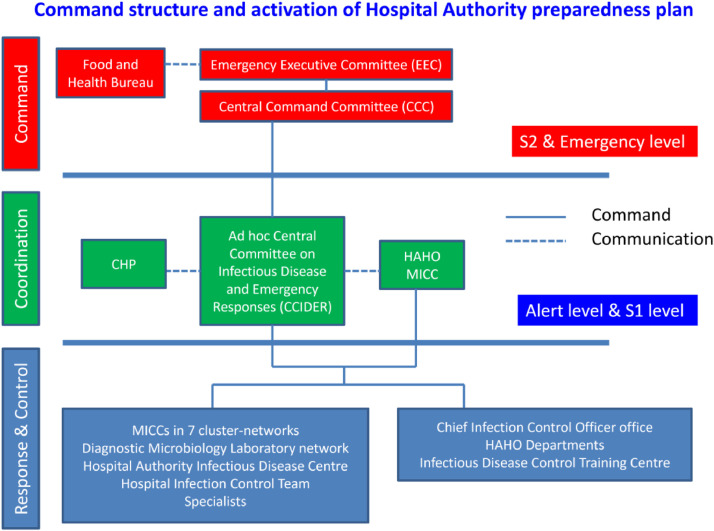
After the SARS outbreak in 2003, a preparedness plan for emerging infectious diseases, including pandemic influenza and Middle East Respiratory Syndrome-associated coronavirus, was formulated under the governance of Hospital Authority. The preparedness plan to combat against SARS-CoV-2 is basically referring to the framework of these plans. According to the risk assessment, the response levels are categorized into alert level, serious response level 1 (S1), serious response level 2 (S2), and emergency response level.11 The command structure depends on the different response levels (Fig 1 ). In the alert and S1 level, the response plan is coordinated by ad hoc Central Committee on Infectious Disease and Emergency Responses (ad hoc CCIDER). In the S2 and emergency response level, the governance is under the command of Central Command Committee, which is chaired by Chief Executive of Hospital Authority, or Emergency Executive Committee, which is chaired by Chairman of Hospital Authority. The response measures at each response level comprise of a series of actions, including active surveillance and electronic notification, laboratory network for rapid molecular diagnostic, infection control measures, provision of essential medical services, facility management in the hospitals, human resources and staff deployment, staff training, research, and communication. Contact tracing for potential secondary cases was performed to investigate for any possible nosocomial infection as reported previously.12 , 13
Fig 1.
Command structure and activation of Hospital Authority preparedness plan. Note. CHP, Centre for Health Protection under the governance of Department of Health; HAHO, Hospital Authority Head Office; MICC, major incident control center, S1, serious response level 1; S2, serious response level 2. Central Command Committee is chaired by the Chief Executive of Hospital Authority. Emergency Executive Committee is chaired by the Chairman of Hospital Authority.
Laboratory diagnosis of SARS-CoV-2
Clinical specimens including nasopharyngeal aspirate, nasopharyngeal swab, throat swab, saliva, sputum, endotracheal aspirate, or bronchoalveolar lavage were subjected to nucleic acid extraction by the eMAG extraction system (bioMérieux, Marcy-l’Étoile France) as previously described.9 , 11The presence of the SARS-CoV-2 ribonucleic acid (RNA) in the specimens was first determined by the LightMix Modular SebeccoV E-gene commercial kit (TIB Molbiol, Berlin, Germany) and further confirmed by another in-house real-time reverse transcription polymerase chain reaction assay targeting the SARS-CoV-2 RNA-dependent RNA polymerase/helicase gene.14
Statistical analysis
The Fisher's exact test was used to compare independent categorical variables between groups. All reported P values were 2-sided. A P value of <.05 was considered statistically significant. Computation was performed using the SPSS Version 15.0 for Windows.
Results
Comparative epidemiology of SARS-CoV and SARS-CoV-2
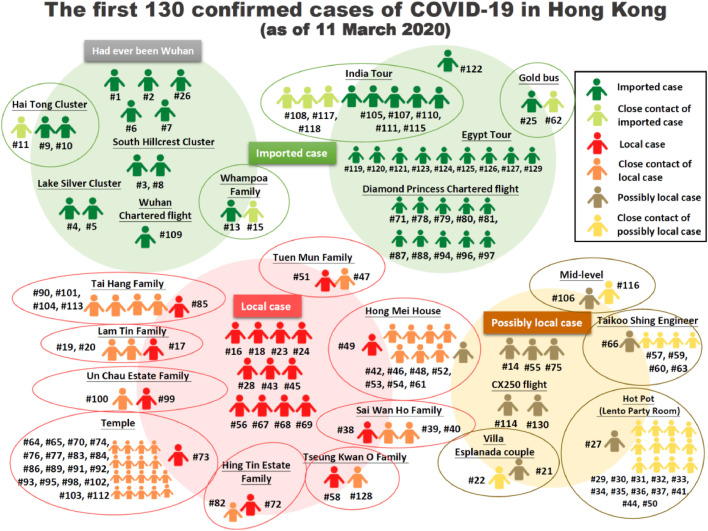
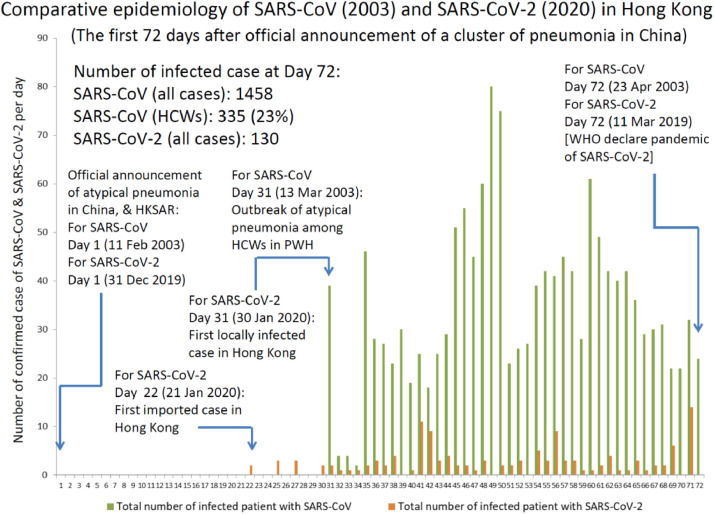
Up to March 11, 2020 (day 72 after the official announcement of a cluster of pneumonia of unknown etiology in Wuhan, Hubei Province), a total of 130 cases of SARS-CoV-2 infection were confirmed in Hong Kong, while the first 42 cases were reported previously.9 With these additional cases, there were 63 males and 67 females with a median age of 60 years (range 16-96 years). The 130 confirmed cases belonged to 22 clusters, of which 8 clusters could be traced from an index patients who had travel history within 14 days of symptoms onset (Fig 2 ). The first local case of SARS-CoV-2 occurred on day 31, while the onset of 2003 SARS-CoV was also detected on day 31, which occurred as a nosocomial outbreak affecting 39 HCWs in Hong Kong (Fig 3 ). In the first 72 days, the number of infected patients (n = 130) with SARS-CoV-2 was 11 times lower than that of SARS-CoV (n = 1,458) according to the day-by-day comparison (Fig 3). While the number of infected HCWs for SARS-CoV-2 remained zero on day 72 in 2020, 335 HCWs were infected with SARS-CoV on day 72 in 2003. At the end of the SARS outbreak, 386 HCWs were infected with SARS-CoV. Two hundred and ninety-three (75.9%) of them were investigated for nosocomial acquisition of SARS-CoV in 8 acute hospitals.15 The incidences of nosocomial acquisition of SARS-CoV per 1,000 SARS-patient-day and per 100 SARS-patient-admission were 7.9 and 16.9 respectively, which were significantly higher than the corresponding incidences of nosocomial acquisition of SARS-CoV-2 (P <.001).
Fig 2.
Epidemiological relationship of the first 130 confirmed case of coronavirus disease 2019 (COVID-19) in Hong Kong. Note. The cumulative number of case as of March 11, 2020 (day 72 after the official announcement of a cluster of pneumonia of unknown etiology in Wuhan, Hubei Province, China); Imported case is defined as patient developed symptoms suggestive of COVID-19 upon arrival to Hong Kong; Local case is defined as patient who had no history of travel during incubation period; Possibly local case is defined as patient who had local movement both outside and inside Hong Kong during the incubation period; Close contact in the community refers to household member or any person with face to face communication of more than 15 minutes in a confined area.
Fig 3.
Comparative epidemiology of SARS-CoV (2003) and SARS-CoV-2 (2020) in Hong Kong. Note. The daily statistic of SARS-CoV was retrieved from the report of the Select Committee to inquire into the handling of the Severe Acute Respiratory Syndrome outbreak by the Government and the Hospital Authority July 2004 [https://www.legco.gov.hk/yr03-04/english/sc/sc_sars/reports/sars_rpt.htm ] (Accessed March 24, 2020). The imported case (65-year-old medical doctor who came from Guangdong Province, China and stayed in hotel M) was not included in the official statistical data in Hong Kong.
In the first 72 days, the incidence of SARS-CoV-2 in Hong Kong was 0.16 per 10,000 populations, which was lower than China (Hubei province), Europe (Italy), Asia (Republic of Korea, and Singapore), and Middle East (Iran) (Table 1 ).
Table 1.
Incidence of acute respiratory syndrome associated coronavirus 2 (SARS-CoV-2) infection in Hong Kong as compared with the selected country, province, or city as of March 11, 2020 (WHO declared the COVID-19 pandemic)*
| Country, province, or city | Population (10,000s)‡ | Cumulative confirmed case§ | Cumulative death§ | Incidence of infection per 10,000 population | Date of first imported case / date of over 100th confirmed cases (day of first case to over 100th confirmed cases) |
|---|---|---|---|---|---|
| Hubei† | 5,917 | 67,773 | 3,046 | 11.45 | Not applicable |
| Italy | 6,024 | 10,149 | 631 | 1.68 | 31-Jan-20 / 24-Feb-20 (24) |
| Republic of Korea | 5,178 | 7,755 | 60 | 1.50 | 20-Jan-20 / 20-Feb-20 (31) |
| Iran | 8,328 | 8,042 | 291 | 0.97 | 20-Feb-20 / 27-Feb-20 (7) |
| Bahrain | 154 | 110 | 0 | 0.71 | 25-Feb-20 / 10-Mar-20 (14) |
| Switzerland | 859 | 491 | 3 | 0.57 | 26-Feb-20 / 7-Mar-20 (10) |
| Norway | 537 | 277 | 0 | 0.52 | 27-Feb-20 / 7 Mar-20 (9) |
| Denmark | 582 | 262 | 0 | 0.45 | 27-Feb-20 / 11 Mar-20 (13) |
| Spain | 4,710 | 1639 | 36 | 0.35 | 1-Feb-20 / 3-Mar-20 (31) |
| Sweden | 1,033 | 326 | 0 | 0.32 | 1-Feb-20 / 7 Mar-20 (35) |
| Singapore | 570 | 166 | 0 | 0.29 | 24-Jan-20 / 1 Mar-20 (37) |
| France | 6,706 | 1,774 | 33 | 0.26 | 25-Jan-20 / 1-Mar-20 (36) |
| Belgium | 1,152 | 267 | 0 | 0.23 | 5-Feb-20 / 7 Mar-20 (31) |
| Netherlands | 1,744 | 382 | 4 | 0.22 | 28-Feb-20 / 7 Mar-20 (8) |
| Austria | 890 | 182 | 0 | 0.20 | 26-Feb-20 / 8 Mar-20 (11) |
| Germany | 8,315 | 1,296 | 2 | 0.16 | 28-Jan-20 / 2-Mar-20 (34) |
| Hong Kong SAR# | 745 | 120 | 3 | 0.16 | 23-Jan-20 / 3-Mar-20 (40) |
| The United Kingdom | 6,644 | 373 | 6 | 0.06 | 1-Feb-20 / 6-Mar-20 (34) |
| Japan | 12,601 | 568 | 12 | 0.05 | 16-Jan-20 / 22-Feb-20 (37) |
| Australia | 2,565 | 112 | 3 | 0.04 | 25-Jan-20 / 11-Mar-20 (46) |
| Malaysia | 3,272 | 129 | 0 | 0.04 | 26-Jan-20 / 10-Mar-20 (44) |
| United States of America | 32,945 | 696 | 25 | 0.02 | 23-Jan-20 / 4-Mar-20 (41) |
Country, province, or city with more than 100 reported case of SARS-CoV-2 were selected for comparison.
Hubei province, as the most severely affected area in China, was selected for comparison.
The population of country, province, or city were retrieved from the website of World Health Organization.
Infection retrieved from situation report – 51 of World Health Organization issued on March 11, 2020 (day 72 after the official announcement of a cluster of pneumonia of unknown etiology in Wuhan, Hubei Province, China).
Hong Kong SAR, Hong Kong Special Administrative Region, China, although the number of confirmed case in Hong Kong reached 130 on March 11, 2020, data from WHO situation report-51 was used for comparison.
Preparedness plan of Hospital Authority to combat SARS-CoV-2 in Hong Kong
Upon receiving the official announcement of a cluster of pneumonia of unknown etiology in Wuhan, Hubei Province, on December 31, 2020 (day 1), the infection control responses were stepped up by Hospital Authority according to the rapidly evolving epidemiology of SARS-CoV-2 in Hong Kong.9 The level of response towards emerging infectious disease was directly elevated from alert to S2 on day 5. Ad hoc CCIDER was regularly held among infection control professionals in 7 cluster-networks and senior management team in the head office of Hospital Authority (HAHO) to review and update the infection control responses so as to disseminate the information to the frontline staff via open staff forum, department visit, right-on-time training of donning and doffiing of personal protective equipment (PPE). Upon receiving the first imported case of SARS-CoV-2 in Hong Kong on day 22, the response level was further elevated to the emergency level on day 26. The Central Command Committee composed of the top management team of 7 cluster-networks and HAHO is responsible for the decision for various administrative supports in consultation with ad hoc CCIDER which is responsible for the professional advice. Up to day 72, a total of 16 meetings of ad hoc CCIDER were held , especially focusing on the evolution of infection control recommendations issued by WHO and Centers for Disease Control and Prevention of the United States, as well as the scientific evidences published during the evolution of epidemic. Central Command Committee was held daily since the activation of emergency level. Hospital Authority has set the priority of service to support the infection control and clinical management against SARS-CoV-2. The elective and nonessential clinical services were trimmed down to reduce the bed occupancy in the hospitals. Visitors were prohibited to the hospitals except for compassionate reasons. The utilization of airborne infection isolation room (AIIRs) of 1,400 beds in the Hong Kong was closely monitored. The first 20 confirmed cases of SARS-CoV-2 were admitted to a designated hospital. Subsequently, each cluster-network required to take care of the next 20 confirmed cases. The major incident control center of HAHO was responsible for cross cluster-network transfer of confirmed cases. Procurement, distribution, and monitoring the utilization of PPE and laboratory reagents for rapid molecular diagnostic among 7 cluster-networks were performed by HAHO and hospital management teams. Accommodation was provided to staffs working in high risk areas and isolation facilities during the period of emergency response level.
A 4-tier active surveillance for patients infected with SARS-CoV-2 was implemented for patients upon admission (tier 1 to 3),9 while the tier 4 surveillance was initiated for patients attending outpatient clinics as well as accident and emergency department since February 20, 2020 (day 52) (Table 2 ). From day 1 to day 72, 119 (0.47%) of 25,097 patients fulfilling tier 1 to 3 were confirmed, while between day 52 and 72, eleven (0.15%) of 7,346 outpatients were found to be positive for SARS-CoV-2.
Table 2.
Tiers of enhanced laboratory surveillance for coronavirus disease 2019 (COVID-19) in both inpatients and outpatients in Hong Kong*
| Tier | Inclusion criteria | Type of specimen collection | Patient placement and use of personal protective equipment |
|---|---|---|---|
| In-patients | |||
| 1 | Patient with clinical criteria (fever or acute respiratory illness or pneumonia) AND with epidemiological criteria (with travel history to a place with active community transmission of COVID-19 or had close contact with a confirmed case of COVID-19) within 14 days before onset of symptoms | Nasopharyngeal flocked swab (NPFS), or nasopharyngeal aspirate (NPA) [in viral transport medium (VTM)] | AIIR (single room) N95 respirator, eye protection by goggles or face shield, gloves, and isolation gown (AAMI level 1)† |
| 2 | Irrespective of history of travel, patient with pneumonia requiring ICU care; or occurring in clusters; or who is a health care worker. | NPFS, or NPA in VTM; lower respiratory tract such as sputum, tracheal aspirate (TA) (if intubated), and bronchoalveolar lavage (BAL) (if bronchoscopy) | AIIR (single room as far as possible); otherwise cohort nursing in AIIR |
| 3 | Any patient with pneumonia other than Tier 2 | NPFS, or NPA in VTM; lower respiratory tract such as sputum, TA (if intubated), and BAL (if bronchoscopy) | Surveillance ward (one metre spacing between patients; increase air change per hour by mobile HEPA filter) |
| Outpatients in clinics and AEDs | |||
| 4‡ | Fever or respiratory symptoms subject to clinical assessment of physician in charge | Patients should be smart enough to understand the technique to collect “Deep Throat Saliva” in early morning for adult and pediatric cases | Hospitalization is not required; patients is called back for admission if the specimen is positive for SARS-CoV-2 |
Note. AAMI, Association for the Advancement of Medical Instrumentation PB70:2003 is to define the liquid barrier performance and classification of protective apparel and drapes intended for use in health care facilities (https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/medical-gowns); AED, accidental and emergency departments; AIIR, airborne infection isolation room; HEPA, high efficiency particulate air; ICU, intensive care unit.
The evolving criteria of active surveillance was reported.9
AAMI level 1 isolation gown is used when small amounts of fluid exposure is anticipated. AAMI level 3 isolation gown can be considered when splashing is anticipated. Alternatively, a waterproof apron on top of the AAMI level 1 isolation gown is also acceptable (with effect from February 19, 2020, day 51).
The fourth tier enhanced laboratory surveillance was updated since February 20, 2020 (day 52).
Discussion
Infection of HCWs due to occupational exposure to infectious diseases is always a great challenge to hospital administration and infection control professionals. Sporadic cases of occupation related infection among HCWs due to various infectious diseases such as Mycobacterium tuberculosis, hepatitis B virus, and hepatitis C virus were occasionally reported.16 However, the impact of SARS transmission among HCWs was unprecedentedly high. According to WHO, HCWs accounted for 1,707 (21%) of 8,098 cases of SARS patients in 2003.6 It produced a significant psychosocial effects and long-term psychological effects on HCWs.17 Therefore, when the COVD-19 emerged, it is important to maximize our administrative resources and infection control measures to protect our HCWs, which is particularly relevant in Hong Kong as we had 8 HCWs died in 2003 as a result of nosocomial acquisition of SARS-CoV.5 , 18
Administrative support to infection control is important to prevent nosocomial outbreak but it is not well-studied in recent years.19 However, suboptimal administrative support was attributed to the prolonged outbreak of carbapenemase-producing Enterobacteriaceae in a tertiary care hospital in France,20 as well as the major outbreak of SARS in Hong Kong.7 Therefore, the command structure for preparedness of emerging infectious diseases was established in Hospital Authority in Hong Kong after outbreak of SARS. Through the regular meetings between the hospital representative of infection control professionals and senior hospital administrators, infection control policy could be timely revised and endorsed by all hospitals under the governance of Hospital Authority. For instance, the clinical and epidemiological criteria for active surveillance of suspected case of COVID-19 was serially updated along with the evolving epidemic of COVID-19.9
With the support of hospital administration, the infrastructure of hospitals was improved from the period of SARS-CoV to SARS-CoV-2 by the provision of 1,400 AIIRs in Hong Kong. Early isolation of patients with SARS-CoV and their close contacts was found to be effective measure to terminate the chain of transmission5 , 18 when the viral load of SARS-CoV was peaked at day 10 after symptoms onset.5 For SARS-CoV-2, high viral load was detected soon after onset of symptoms.21 Therefore, 109 of 130 confirmed cases in our series belong to 22 households or social gathering clusters. It is even more important to perform rapid molecular diagnostic test and isolate patients with SARS-CoV-2 as early as possible. It is the reason why we further extended the scope of active surveillance from hospitalized patients to outpatients who have relatively mild respiratory symptoms, and continue contact tracing for potential secondary cases in order to identify any transmission in hospital and community. Business service department of Hospital Authority plays a key role to secure the timely procurement of diagnostic platforms and reagents, as well as PPE for HCWs because supply of PPE becomes strategically important in the pandemic of COVID-19.
Major incident control center of Hospital Authority coordinates the utilization of isolation facilities by transferring confirmed cases of SARS-CoV-2 across different public hospitals in order to avoid an individual hospital being overwhelmed by confirmed cases. Temporal conversion of general wards to AIIRs was conducted to accommodate the increasing number of COVID-19 patients. In addition, non-emergency clinical services were trimmed down in order to reduce the bed occupancy and improve the manpower ratio of HCWs to patients, which may facilitate the control of outbreak. No visiting policy during emergency response level in Hospital Authority may further reduce the risk of importation of patients with SARS-CoV-2 from the community. Decanting of wards and deployment of HCWs to care for patients with SARS-CoV-2 were planned in advance. As working in an unfamiliar environment and lapses in infection control were attributed to the nosocomial outbreak of SARS,22 the deployed HCWs other than the discipline of internal medicine would be oriented for the logistic of patients’ management in the isolation wards and trained for the use of PPE well before managing suspected and confirmed case of SARS-CoV-2. It is because inappropriate removal of PPE may increase the risk of acquisition of SARS-CoV.23
Ongoing staff forum and training sessions for PPE are regularly conducted to enhance the alertness of HCWs. During the community outbreak of pandemic influenza A, provision of timely education to the staff was one of the important parameters to achieve zero nosocomial outbreak of pandemic influenza A H1N1 virus in 2009.12 The training materials were compiled into a communication kit which was uploaded to the electronic platform of Hospital Authority with free access to all staff. The health promotion messages to HCWs were further promulgated via social media such as Facebook, YouTube, and WhatsApp group.
From the declaration of pandemic (day 72) to the time of manuscript submission on March 24, 2020 (day 85), the number of global confirmed cases of SARS-CoV-2 has nearly tripled (from 118,000 to 332,000). Almost 5,000 HCWs infected with 24 deaths in Italy.24 In mainland China, it was shown that 29% (40 of 138) of admitted SARS-CoV-2 patients in Zhongnan hospital, Wuhan were HCWs.25 This proves the high risk of nosocomial transmission of SARS-CoV-2. On day 85, the number of confirmed cases of SARS-CoV-2 was over 300 in Hong Kong while zero transmission of SARS-CoV-2 among HCWs and hospitalized patients could be achieved, suggestive of a significant improvement in the health care infrastructure to combat against emerging infectious diseases in Hong Kong.
Footnotes
This work was supported in part by the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Diseases of the Department of Health, Hong Kong Special Administrative Region; and the Collaborative Innovation Center for Diagnosis and Treatment of Infectious Diseases, the Ministry of Education of China.
Conflicts of interest: All authors report no conflicts of interest relevant to this article.
References
- 1.The Centre for Health Protection closely monitors cluster of pneumonia cases on Mainland. Press release of the Department of Health, Hong Kong Special Administrative Region. Available at: https://www.info.gov.hk/gia/general/201912/31/P2019123100667.htm. Accessed March 16, 2020.
- 2.World Health Organization. Coronavirus disease 2019 (COVID-19) Situation Report-51. Available at:https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. Accessed March 16, 2020.
- 3.Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100–101. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.List of medical professionals who died during the SARS outbreak. Available at: https://en.wikipedia.org/wiki/List_of_medical_professionals_who_died_during_the_SARS_outbreak. Accessed March 16, 2020.
- 5.Cheng VC, Lau SK, Woo PC, Yuen KY. Severe acute respiratory syndrome coronavirus as an agent of emerging and reemerging infection. Clin Microbiol Rev. 2007;20:660–694. doi: 10.1128/CMR.00023-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Summary of probable SARS cases with onset of illness from 1 November 2002 to 31 July 2003 (Based on data as of the 31 December 2003). World Health Organization. Available at:https://www.who.int/csr/sars/country/table2004_04_21/en/ . Accessed March 22, 2020.
- 7.Report of the select committee to inquire into the handling of the severe acute respiratory syndrome outbreak by the government and the hospital authority July 2004. Available at:https://www.legco.gov.hk/yr03-04/english/sc/sc_sars/reports/sars_rpt.htm. Accessed March 16, 2020.
- 8.Daily statistics on SARS patients with breakdown by healthcare workers, Amoy Gardens residents and others. Available at:https://www.legco.gov.hk/yr03-04/chinese/sc/sc_sars/reports/tbl/a35.pdf. Accessed March 8, 2020.
- 9.Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi: 10.1017/ice.2020.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coronavirus disease (COVID-2019) situation reports. Available at:https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed March 16, 2020.
- 11.Cheng VCC, Wong SC, To KKW, Ho PL, Yuen KY. Preparedness and proactive infection control measures against the emerging novel coronavirus in China. J Hosp Infect. 2020;104:254–255. doi: 10.1016/j.jhin.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cheng VC, Tai JW, Wong LM, et al. Prevention of nosocomial transmission of swine-origin pandemic influenza virus A/H1N1 by infection control bundle. J Hosp Infect. 2010;74:271–277. doi: 10.1016/j.jhin.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng VC, Tai JW, Lee WM, et al. Infection control preparedness for human infection with influenza A H7N9 in Hong Kong. Infect Control Hosp Epidemiol. 2015;36:87–92. doi: 10.1017/ice.2014.2. [DOI] [PubMed] [Google Scholar]
- 14.Chan JF, Yip CC, To KK, et al. Improved molecular diagnosis of COVID-19 by the novel, highly sensitive and specific COVID-19-RdRp/Hel real-time reverse transcription-polymerase chain reaction assay validated in vitro and with clinical specimens. J Clin Microbiol. 2020;58:e00310–e00320. doi: 10.1128/JCM.00310-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Evidence/documents provided by the administration and related persons for the select committee to inquire into the handling of the severe acute respiratory syndrome outbreak by the government and the hospital authority July 2004. Available at:https://www.legco.gov.hk/yr03-04/chinese/sc/sc_sars/reports/tbl/a98.pdf. Accessed March 16, 2020.
- 16.Nienhaus A, Kesavachandran C, Wendeler D, Haamann F, Dulon M. Infectious diseases in healthcare workers - an analysis of the standardised data set of a German compensation board. J Occup Med Toxicol. 2012;7:8. doi: 10.1186/1745-6673-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12:1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng VC, Chan JF, To KK, Yuen KY. Clinical management and infection control of SARS: lessons learned. Antiviral Res. 2013;100:407–419. doi: 10.1016/j.antiviral.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein L. The role of the hospital administrator in the control of nosocomial infections. Rev Infect Dis. 1981;3:785–789. doi: 10.1093/clinids/3.4.785. [DOI] [PubMed] [Google Scholar]
- 20.Delory T, Seringe E, Antoniotti G, et al. Prolonged delay for controlling KPC-2-producing Klebsiella pneumoniae outbreak: the role of clinical management. Am J Infect Control. 2015;43:1070–1075. doi: 10.1016/j.ajic.2015.05.021. [DOI] [PubMed] [Google Scholar]
- 21.To KKW, Tsang OTY, Leung WS, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis. 2020;20:565–574. doi: 10.1016/S1473-3099(20)30196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai TS, Yu WC. The lessons of SARS in Hong Kong. Clin Med (Lond) 2010;10:50–53. doi: 10.7861/clinmedicine.10-1-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Puro V, Nicastri E. SARS and the removal of personal protective equipment. CMAJ. 2004;170:930. doi: 10.1503/cmaj.1031700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Available at: https://www.sbs.com.au/news/these-are-the-names-of-the-24-italian-health-care-workers-who-have-died-during-the-coronavirus-pandemic. Accessed March 24, 2020.
- 25.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel Coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]