On December 31, 2019, China reported the first cases of pneumonia of unknown cause that would later be identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1, 2, 3 SARS-CoV-2 rapidly spread, resulting in a pandemic, and as of April 10, 2020, there were almost 1.6 million confirmed cases reported worldwide, with approximately 97,200 deaths. The United States is currently the country with the highest number of infections, 466,396, with 16,703 deaths. Italy, with 143,626 confirmed cases since the beginning of the epidemic, has the highest number of deaths, 18,279. In particular, Lombardy (a region in northern Italy with a population of 10,000,000) has been the Italian region most affected by SARS-Cov-2: since the beginning of the epidemic 54,802 people have contracted the virus, and, of these, 10,022 people have died.4
Patients undergoing hemodialysis (HD) treatment and health care staff may be at high risk of coronavirus disease 2019 (COVID-19) both because of the difficulty in applying isolation and social distancing, and the immunosuppressed state and frailty of patients.5
There are few data available from China5,6 on the prevalence of SARS-CoV-2 infection in HD patients and no data on HD patients from other countries.
We report the experience of a large HD center in Lombardy, Italy, during the SARS-CoV-2 epidemic in March 2020.
Results
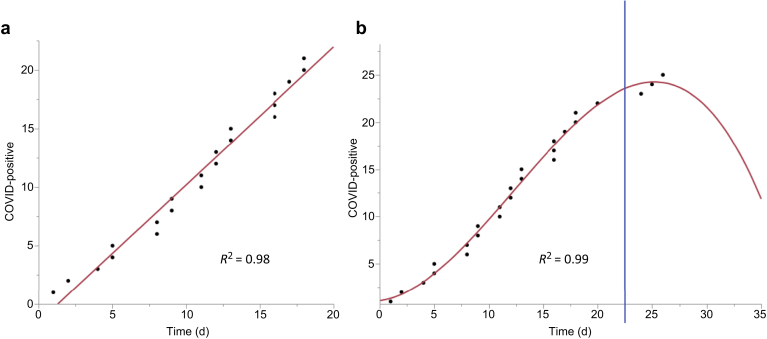
During the first 2 weeks of March, 7 HD patients (5 from the HD hospital and 2 from the HD satellite centers) died from causes unrelated to SARS-CoV-2 infection (2 from cachexia, 2 from Staphylococcus aureus sepsis, 1 from sudden death, and 2 from voluntary interruption of HD treatment). On March 9, the first HD patient was admitted to hospital for interstitial pneumonia with positive nasopharyngeal swab for SARS-CoV-2. From March 9 to March 26, a total of 26 HD patients were admitted for fever. Of these, 21 (81%) patients (7 from the satellite centers) tested positive for SARS-CoV-2 and they all had interstitial pneumonia. Thereafter, the incidence of new cases of COVID-19 in HD patients was almost linear from March 9 to 26 (Figure 1a).
Figure 1.
Coronavirus disease 2019 (COVID-19) trend in hemodialysis (HD) patients before (a) and after (b) the upgrade of personal protective equipment and nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 in all HD patients. The blue line represents the moment when these measures were put in place.
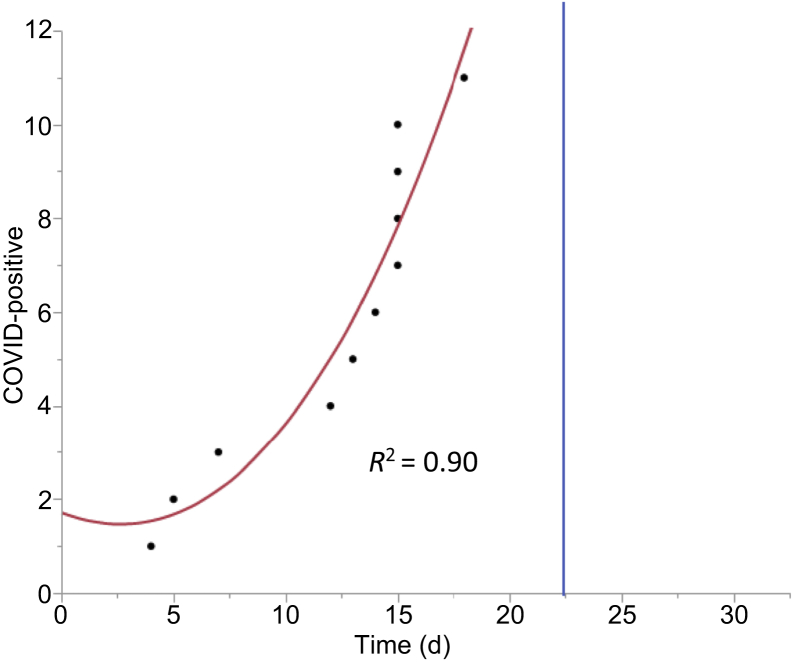
From March 12 to March 26, 10 of 30 (33%) nurses and and 1 physician, working in the hospital HD center, were diagnosed with COVID-19 infection (Figure 2).
Figure 2.
Coronavirus disease 2019 (COVID-19) trend in health care staff before and after (blue line) the upgrade of personal protective equipment and nasopharyngeal swab for severe acute respiratory syndrome coronavirus 2 in all hemodialysis patients.
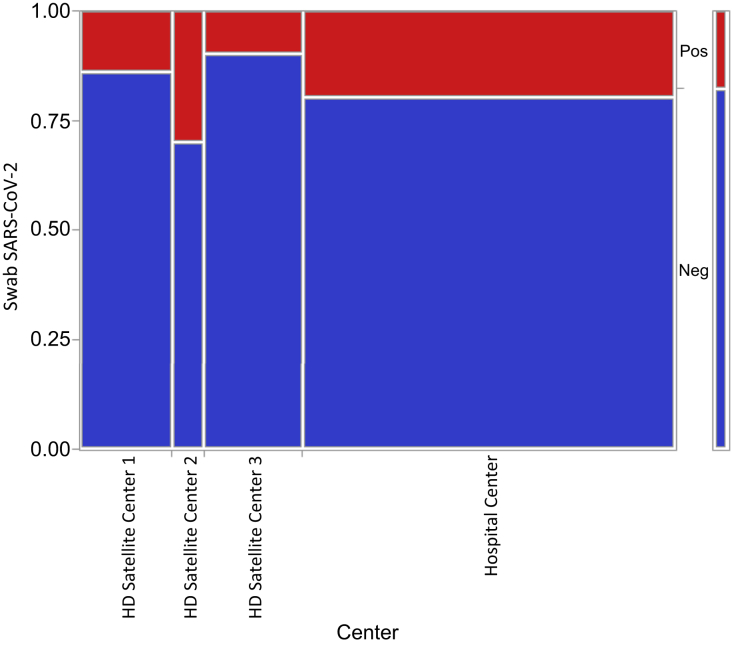
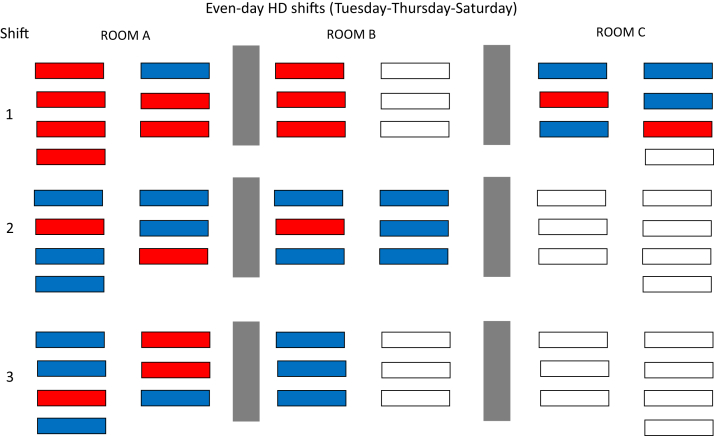
Thirty-three of 188 (18%) asymptomatic HD patients had positive nasopharyngeal swabs for SARS-CoV-2: 23 patients in the hospital HD center and 10 patients in the 3 satellite HD centers (Figure 3). These SARSCoV-2–positive patients received HD treatment in rooms together with swab-negative patients (Figure 4) until March 25. In total, 55 of 209 (26%) HD patients had a positive nasopharyngeal swab for SARS-CoV-2 with or without symptoms.
Figure 3.
Distribution of asymptomatic hemodialysis (HD) patients with nasopharyngeal swab positive (Pos) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the 4 HD centers. Neg, negative.
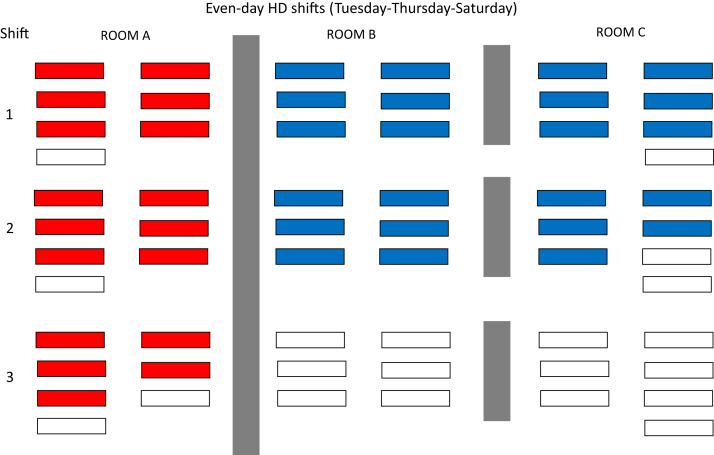
Figure 4.
Example of distribution of patients with nasopharyngeal swab positive for severe acute respiratory syndrome coronavirus 2 (red) together with negative patients (blue) in some hemodialysis (HD) rooms. White boxes represent the HD stations without patients at that time. Gray boxes represent the partition walls between one HD room and another room.
From March 26, after the implementation of preventive measures (upgrade of personal protective equipment [PPE], nasopharyngeal swab for SARS-CoV-2 in all HD patients, and cohorting HD sessions for SARS-CoV-2–positive asymptomatic patients in dedicated areas, as described in Supplementary Materials and Methods), no further symptomatic infections were noted in patients with previously negative nasopharyngeal swabs (Figure 1b) and none in the HD health care staff. Four asymptomatic HD patients, with previously positive nasopharyngeal swab SARS-CoV-2, developed symptoms of COVID-19.
In the same month, no patient on peritoneal dialysis was admitted for COVID-19 and none of these patients developed symptoms due to SARS-CoV-2 infection at home.
Outcomes
Among the 25 patients with COVID-19 who were hospitalized, 13 (52%) died, 7 (28%) improved and were discharged, and 5 (20%) are still hospitalized. The cause of death was acute respiratory failure in 8 patients and worsening neurological conditions in 5 patients. There were no statistically significant differences in age (73 ± 8 years vs. 72 ± 15 years), dialysis vintage (55 ± 15 months vs 39 ± 9 months), major comorbidities (2 ± 0 vs 1 ± 0), and therapy (all patients were treated with antiviral therapy, hydroxychloroquine, azithromycin, and low molecular weight heparin) between the patients with COVID-19 who died and the patients with COVID-19 who were discharged or are still hospitalized.
All HD patients with COVID-19 received respiratory support (oxygen therapy with nasal cannulae, masks or noninvasive positive pressure ventilation) but not mechanical ventilation. Patients died after a median of 8 days (interquartile range, 5–11 days) from admission. Patients who recovered were discharged after a median of 15 days (interquartile range, 13–16 days) from admission.
Discussion
COVID-19 presents particular challenges for patients on dialysis, in particular for those undergoing treatment in HD centers. In-center HD significantly increases the risk of transmission of infection, including to medical staff, patients themselves, and family members, due to the difficulty in applying epidemiological measures, such as isolation and social distancing.
The incidence of SARS-CoV-2 infection in patients on HD or peritoneal dialysis, and patients with renal transplantation is gradually emerging, and there are few data on the incidence of SARS-CoV-2 infection in HD patients,5, 6, 7 peritoneal dialysis patients, and renal transplant patients.8,9
Unpublished data (F. He and G. Xu, unpublished data in Li and Xu5) on SARS-CoV-2 infection at the dialysis centers in Wuhan reported COVID-19 infection of up to 10% among patients and 6.4% among medical staff.
This study reports the incidence of SARS-CoV-2 infection in the Nephrology and Dialysis Department in the Hospital of Province of Lecco in Lombardy (Italy) where there was a high incidence of infection in the general population. As of April 10, 2020, 1838 cases of COVID-19 infection were recorded in Lecco province, of a population of 337,380 (0.5%). However, nasopharyngeal swabs for SARS-CoV-2 detection were performed only on patients admitted to hospital for COVID-19 symptoms and therefore the true incidence of the infection is likely to be much higher.
In our hospital and 3 satellite HD centers there were 55 of 209 HD patients with positive nasopharyngeal swab for SARS-CoV-2 with or without symptoms. The incidence in our HD population was very high: 26% of the entire HD population. Considering only symptomatic patients with COVID-19, all hospitalized, the incidence was 12% (25 patients of 209). SARS-CoV-2 infection among health care workers was very high: 10 of 30 (33%) nurses and 1 physician (of 12), despite attempts to detect symptomatic patients early on and performing HD treatment in isolation with appropriate PPE.
It is well known that asymptomatic SARS-CoV-2 carriers can transmit the infectionS1 and this in fact is important in transmission of the virus in areas such as waiting rooms, HD rooms, and the shared transportation to and from the HD centers. In HD rooms, it is not always possible to maintain the recommended safety distance of approximately 2 m,S2 and patients cannot always tolerate the surgical mask for long periods of time. Because of the high incidence of patients and health care professionals with COVID-19 symptoms, we decided to perform a nasopharyngeal swab for SARS-CoV-2 in all asymptomatic patients of the 4 outpatient HD centers: of these, 18% (33 of 188) were found positive. Before performing nasopharyngeal swab for SARS-CoV-2, patients underwent dialysis sessions in the same rooms and health care professionals wore the appropriate PPE, but not the PPE reserved for patients known to be SARS-CoV-2 positive. On receiving swab results, we embarked on a different strategy. We transferred all patients who tested positive from the satellite centers to the hospital center and created 3 distinct areas for patients on HD treatment: 1 for positive asymptomatic, 1 for positive symptomatic, and 1 for negative (Figure 5). After having deployed these preventive measures, we had no more cases of COVID-19 among the previously negative patients and among the health care staff. Four patients with positive swab subsequently developed symptoms for COVID-19.
Figure 5.
Example of separation of patients with nasopharyngeal swab positive for severe acute respiratory syndrome coronavirus 2 (red) from negative patients (blue) and physical separation of hemodialysis (HD) rooms (gray). White boxes represent the HD stations without patients at that time.
With these measures, probably, it was possible to reduce the incidence of COVID-19 transmission among HD patients in our dialysis centers obtaining the flattening and then the inversion of the incidence curve (Figure 1b). The mortality of COVID-19 in the general population has been observed to be approximately 2.3%, with age and comorbidities such as cardiovascular diseases, diabetes, chronic respiratory diseases, hypertension, and cancer being associated with worse prognoses.S3
There are no data on COVID-19 mortality in HD patients. Unlike other limited experiences,6 mortality in our HD patients was very high: 13 of 25 (52%) patients with COVID-19 died.
All HD patients with COVID-19 were treated with antiviral therapy, hydroxychloroquine, antibiotics (azithromycin), and low molecular weight heparin and there were no statistically significant differences in age, dialysis vintage, and major comorbidities between the patients with COVID-19 who died and the patients with COVID-19 who were discharged or are still hospitalized. A factor explaining such high mortality may be the mean age of the HD patients in our HD centers; however, the high mortality among HD patients indicates a vulnerability toward a severe viral infection.
It is possible that the attenuation of the incidence of HD patients with COVID-19 is also due to the course of the epidemic in the territory of our province and not to the measures that we have put in place, as well as it is possible that we have not identified all patients positive to SARS-CoV-2 for the non absolute sensitivity of the nasopharyngeal swab.S4 However, ours is the first report of attempted containment in HD centers, in addition to general measures, of the SARS-CoV-2 epidemic in areas where there has been a very high spread of the virus, such as in our territory.
In the absence of other measures to detect asymptomatic carriers of SARS-CoV-2, performing a nasopharyngeal swab on all HD patients, separating positive and negative patients during HD transport and treatment, and upgrading the PPE for staff may represent a useful attempt to counter the spread of COVID-19. Furthermore, the absence of COVID-19 infections among our peritoneal dialysis patients, compared with the very high incidence among our HD patients, suggests that self-quarantine and social distancing are the most effective measures for the containment of the spread of the SARS-CoV-2 epidemic in patients on dialysis treatment.
Disclosure
All the authors declared no competing interests.
Footnotes
Supplementary Material
References
- 1.World Health Organization. Pneumonia of unknown cause—China. Available at: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. Published January 5, 2020. Accessed March 11, 2020.
- 2.World Health Organization Novel coronavirus—China. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/ Available at: Published January 12, 2020. Accessed March 11, 2020.
- 3.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available at: https://coronavirus.jhu.edu/map.html. Udated April 10, 2020. Accessed April 10, 2020.
- 5.Li J., Xu G. Lessons from the experience in Wuhan to reduce risk of COVID-19 infection in patients undergoing long-term hemodialysis. Clin J Am Soc Nephrol. 2020;15:717–719. doi: 10.2215/CJN.03420320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma Y., Diao B., Lv X. 2019 novel coronavirus disease in hemodialysis (HD) patients: report from one HD center in Wuhan, China. medRxiv preprint. https://www.medrxiv.org/content/10.1101/2020.02.24.20027201v2 Available at: Accessed March 13, 2020.
- 7.Watnick S., McNamara E. On the frontline of the COVID-19 outbreak keeping patients on long-term dialysis safe. Clin J Am Soc Nephrol. 2020;15:710–713. doi: 10.2215/CJN.03540320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Banerjee D., Popoola J., Shah S. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020;97:1076–1082. doi: 10.1016/j.kint.2020.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alberici F., Delbarba E., Manenti C. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020;97:1083–1088. doi: 10.1016/j.kint.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.