Abstract
The new zoonotic coronavirus (SARS-CoV-2) responsible for coronavirus disease (COVID-19) is a new strain of coronavirus not previously seen in humans and which appears to come from bat species. It originated in Wuhan, Hubei Province, China, and spread rapidly throughout the world, causing over 5,569,679 global cases and 351,866 deaths in almost every country in the world, including Europe, particularly Italy. In general, based on existing data published to date, 80.9% of patients infected with the virus develop mild infection; 13.8% severe pneumonia; 4.7% respiratory failure, septic shock or multi-organ failure; 3% of these cases are fatal. Critical patients have been shown to develop acute respiratory distress syndrome (ARDS) and hospitalization in intensive care units. The average age of patients admitted to hospital is 57–79 years, with one third half with an underlying disease. Asymptomatic infections have also been described, but their frequency is not known. SARS-CoV-2 transmission is mainly airborne from one person to another via droplets. The data available so far seem to indicate that SARS-CoV-2 is capable of producing an excessive immune reaction in the host. The virus attacks type II pneumocytes in the lower bronchi through the binding of the Spike protein (S protein) to viral receptors, of which the angiotensin 2 conversion enzyme (ACE2) receptor is the most important. ACE2 receptor is widely expressed in numerous tissues, including the oropharynx and conjunctiva, but mostly distributed in ciliated bronchial epithelial cells and type II pneumocytes in the lower bronchi. The arrival of SARS-CoV-2 in the lungs causes severe primary interstitial viral pneumonia that can lead to the “cytokine storm syndrome”, a deadly uncontrolled systemic inflammatory response triggered by the activation of interleukin 6 (IL-6), whose effect is extensive lung tissue damage and disseminated intravascular coagulation (DIC), that are life-threatening for patients with COVID-19. In the absence of a therapy of proven efficacy, current management consists of off-label or compassionate use therapies based on antivirals, antiparasitic agents in both oral and parenteral formulation, anti-inflammatory drugs, oxygen therapy and heparin support and convalescent plasma. Like most respiratory viruses can function and replicate at low temperatures (i.e. 34–35 °C) and assuming viral thermolability of SARS-CoV-2, local instillation or aerosol of antiviral (i.e. remdesivir) in humid heat vaporization (40°–41 °C) in the first phase of infection (phenotype I, before admission), both in asymptomatic but nasopharyngeal swab positive patients, together with antiseptic-antiviral oral gargles and povidone-iodine eye drops for conjunctiva (0,8–5% conjunctival congestion), would attack the virus directly through the receptors to which it binds, significantly decreasing viral replication, risk of evolution to phenotypes IV and V, reducing hospitalization and therefore death.
Keywords: SARS-CoV-2, COVID-19, Viral pneumonia, Aerosol vaporization and nebulization, Alcoholic gargle, Povidone-iodine gargle and eye drop, Remdesivir, IL-1/IL-6, Monoclonal antibody, Cytokine storm
Introduction and background
[In nulla parte naturae maiora esse miracula quam in acquis calidis. Plinius Maior (23–79 p.C.n), Naturalis Historia]
The nose and throat setting
A normal breathing means 6 lt air/minute. Air is climatized in nose cavity, and independently from external temperature is sent to lungs via trachea at 31°–34 °C and 90–95% humidity. The bronchial-alveolar temperature is 37°–38 °C. Air is cleaned from about 85% from particles >4.5 µm by mucous-ciliary clearance that transports germs from the nose through pharynx to the stomach for gastric destruction. The nasopharyngeal cavity is naturally exposed to the penetration of pathogenic bacteria that forcefully adhere to the walls and creep into the lymphatic folds maintaining a persistent bacterial load [1]. The Hemophilus Influenzae (HI) and the Streptococcus Pneumoniae (SP), which together with the Moraxella catarrhalis are considered the ‘infernal trio’; the most frequent pathogens of the URDT (upper respiratory digestive tract) are instead present in healthy individuals only in 6% of the nasal samples and in 27% of the pharyngeal samples with a clear prevalence HI (5%) compared to SP (0.5%). In healthy subjects the anaerobic nasal culture is always characterized by the presence of Propionibacterium acnes in 74.5% and Peptococcus magnus in 3.5%. Viruses cause 85% to 95% of throat infections in adults and children younger than 5 years of age; for those aged 5 to 15 years, viruses cause about 70%/ of throat infections, with the other 30% due to bacterial infections, mostly group A β-hemolytic streptococcus (GABHS) [2]. NK cells are there largely active.
The processes that take place in the lungs are basically isothermal. The air in the lungs is saturated with water vapor at the internal body temperature. The water vapor in a saturated mixture is characterized by a partial pressure which mainly depends only on the temperature. Under these conditions, the water vapor does not behave like a compressible gas and its partial pressure PH2O depends only on temperature: 47 mmHg at 37 °C. The heat transfer between a heated stationary body and a moving fluid that invests it, depends on the speed, thermal conductivity and temperature of the fluid [3], [4].
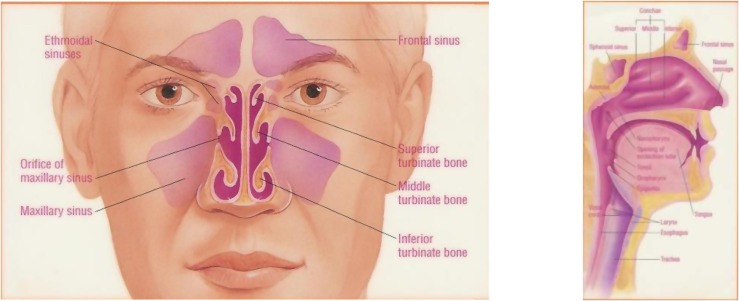
An apparent bias could be overcome separating the air volume introduced with nasal inspiration (which reaches the trachea and bronchi at an air-conditioned temperature of 34° C, whatever the outside temperature) and the volume introduced directly by mouth, which without nasal humidification and filtration, cools the oropharynx and the ring of Waldeyer and reaches service temperatures only in the trachea. In case of SARS-CoV-2 contagion, the cooling and drying of the pharynx can explain the onset with pharyngodynia; mucosal membrane infection of nose and sinuses explain rhinorrhea with anosmia and dysgeusia for viral neurotropism to olfactory and taste nerve receptors (a possible way to reach the brain), and conjunctivitis for mucosal continuity, as well as for direct insemination (droplets): the air temperature introduced via the nasal route is similar to the limbo-conjunctival temperature (Fig. 1 a–b).
Fig. 1.
a) The nasal/sinuses air conditioning. b) The oro-pharynx and trachea. Courtesy B.Y. Ghorayeb, www.ghorayeb.net.
The eye setting
The temperature of the exposed corneal surface is around 34 °C (32.8 to 35,4°C) [5], the limbus being 0,45 °C warmer than the apex. Ocular surface cooled during sustained eye opening and rate of the cooling was greater in the dry eye patient (mostly older people and video terminal operator) [6], while it increases to 36°–37 °C at the conjunctival fornix . In the logical context of this paper, this would justify the related conjunctivitis SARS-CoV-2/19. Indeed, pharyngodinia and low-temperature related conjunctivitis is a common finding in respiratory virus infections. A report in The Lancet, raised concern that ocular surfaces may be a potential target for human- SARS-CoV-2 invasion via droplets, as published by Sun and Coll [7a,b] in two consecutive papers collected in two different period: in Huazhong province from the end of December 2019 till February 7th 2020, and in Hubei province in the second week of February 2020, that had similar results. Twelve (32%) patients in the first series had conjunctivitis with signs that included conjunctival hyperemia, chemosis, epiphora, and increased secretions. Of those patients, 11 (92%) tested positive for CoV-19 by nasopharyngeal swab. In one patient, epiphora was the first symptom of COVID-19. Twenty-eight (74%) of the 38 patients in the second one was positive for CoV-19 by nasopharyngeal swabs, of whom only two (5%) patients had a positive conjunctival specimen, whilst Guan and Coll [8] on NEJM, documented ‘’conjunctival congestion’’ in 9 of 1.099 patients (0,8%) across China, with laboratory confirmed CoV-19. So, a largely approximated valuation would point out about 0,8–5% locally positive patients of those affected by conjunctivitis in evolved stages [9] (the virus possibly vanished in the meantime or by therapy). Still remaining unknown the percentage in phenotype I and in asymptomatic pre-clinical (the majority!) patients. Aged patients have higher rate of dry eye that could justify or amplify the virus conjunctival access to the body, reaching the nose via the lacrimal ductus. Environmental control should therefore take into consideration topical humidification preferably with a cross-linked hyaluronate drops and a hot vaporization (suffumigation, water hot-humid vaporization (WHV) [10]) involving also the upper airways in mucosal continuity with the conjunctiva (Fig. 2 ). It must be humid: an air dryer evaporates the tear film, drastically reduces lactoferrin, mucin trap-door effectiveness and macrophages activity; in addition to the peptidoglycan N-acetylmuramoyl hydrolase (i.e. Fleming's Lysozyme) whose catalysis rate is maximum at pH5.
Fig. 2.
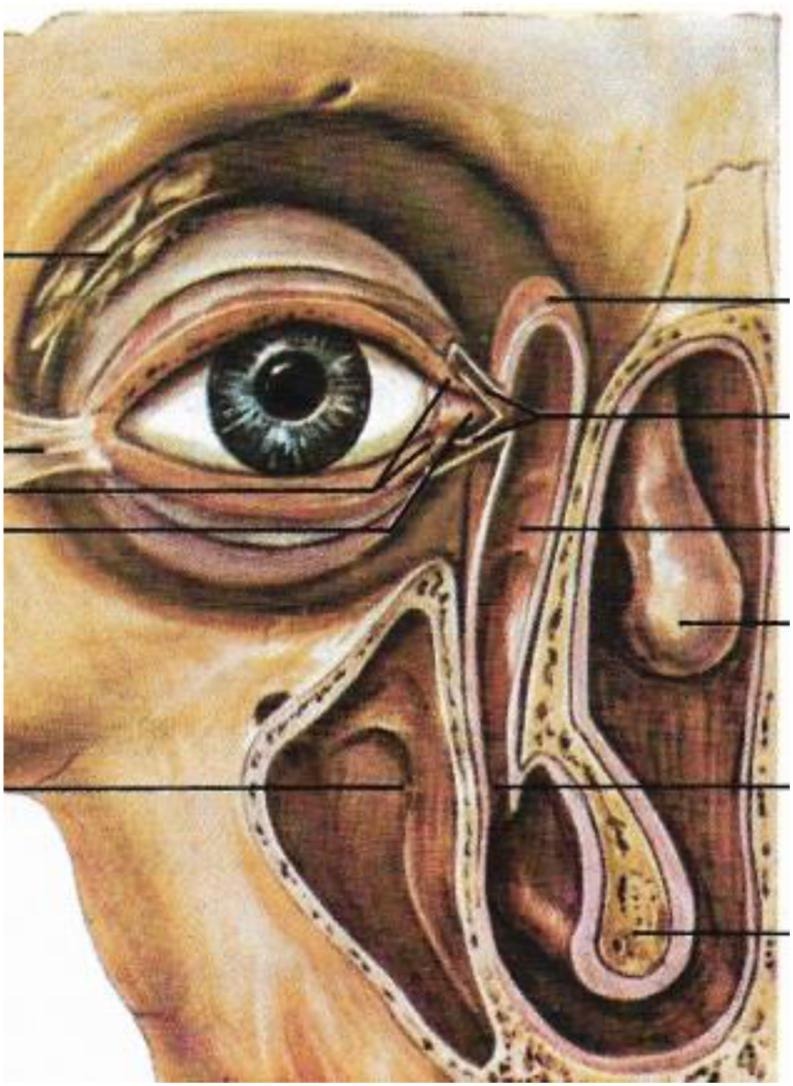
Conjunctival mucosal continuity through lacrimal sac and nasal-lachrymal ductus to inferior meatus. Courtesy Minerva Medica, Torino, 1974.
The Hypothesis/Theory
Most respiratory virus may work and replicate at lower temperatures (34°–35 °C) than the optimal range for epithelial tracheal-bronchial cells (37°–38 °C) [10], either for mucin layer fluidity: exposed to lower temperatures may less react to fight infections. This also causes vasoconstriction reducing blood flow and mucin production. Increasing the air temperature, therefore keeping the upper tract and trachea-bronchial temperature higher, may reduce the replication and diffusion of the respiratory virus. Older people have a weak and altered thermoregulatory response while children, that quickly develop a high body temperature that may halt viral replication, and more balanced immune response, /may have a better chance of fighting infections. SARS-CoV-2 binding the Toll Like Receptor (TLR) causes the release of pro-IL-1β which is cleaved by caspase-1, followed by inflammasome activation and production of active mature IL-1βwhich is a mediator of lung inflammation, fever and fibrosis [11], cardiovascular implications [12], [13] for increased troponin T (TnT), C-reactive protein and terminal fragment of type B natriuretic pro-peptide (NT-proBNP), microvascular endothelial aggression and intestinal-pulmonary cross-talk, with link to colangiocyte ACE2 receptor, interfering with intestinal microbiota [14] requiring pro-biotic adjuvant therapy. This infectious disease mostly affects men, since immune genes are more expressed on the X chromosome [11]. The two coronaviruses that preceded CoV-19 causing respectively the SARS (Severe Acute Respiratory Syndrome) pandemic of 2003 [15] and the MERS (Middle East Respiratory Syndrome) epidemic of 2012 [16], emerged during the summer and spring-summer season, thus not respecting the principle that “respiratory viruses can only function (and replicate) at lower temperatures (i.e. 34–35 °C)”, as stated [10]. The MERS, moreover, is still ongoing in endemic form since 2012, therefore disrespectful of the summer-winter binomial. These concepts, are perhaps explainable that both viruses have made the so-called species jump (Spillover), thus modifying the phenotypic and genotypic characteristics of both virus. SARS-CoV-2 probably behaves in the same way. Therefore, it cannot be accurately stated that this is thermolabile. The biological characteristics of the latter coronavirus are not yet known; SARS-CoV-2 also made the spillover, but passing directly from the bat to the man maybe without an intermediate host [17]. SARS-CoV-2, as the two recent zoonotic coronavirus, are enveloped viruses with round and sometimes pleiomorphic virions of approximately 80 to 120 nm in diameter. Coronaviruses contain positive-strand RNA, with the largest RNA genome (approximately 30 kb) reported to date. The genome RNA is complexed with the basic nucleocapsid (N) protein to form a helical capsid found within the viral membrane. The membranes of all coronaviruses contain at least three viral proteins, of which the most important is the spike (S), the type I glycoprotein that forms the peplomers on the virion surface, giving the virus its corona- or crown-like morphology in the electron microscope. The virus coating consists of a membrane that the virus “inherits” from the host cell after infecting it. As all viruses, SARS-CoV-2 needs an animal cell to survive and spread off. Out of this host, virus loses the ability to survive and infect. Degradation time depends on temperature, humidity and behavior and belongs to the capsid. For this reason, the foamy detergents are active for a contact of at least 20 ', the heat degrades the membrane lipids, as it happens for alcohol 65%, chloride in water 1/5 that directly destroys the protein, as for H2O2 at maximal concentration. It may remain stable in cold outside behavior or in the air conditioner for more than 3 h and on surfaces for days [18], needing also humidity and obscurity, being destroyed by UV, hot, dried and illuminated environments. Up to now is unknown if SARS-CoV-2 induces viremia, as happens in Feline coronavirus [19] that also cause virus systemic spread, including inflammation of the abdominal and thoracic cavities and occasionally, other organs including brain [20] with confusion and epileptic crisis till neurological reliquate needing rehabilitation, as experienced by many survivors. Anyway, even in the absence of precise data on viremia, we can with reasonable certainty state that SARS-CoV-2 runs down to the lung. The virus binds to the type II pneumocytes from lower bronchi via Spike protein (S-protein) [17] binding to virus receptors, of which the angiotensin conversion enzyme 2 (ACE2) receptor is the most important [21]. In the respiratory tract, ACE2 receptor is widely expressed on type II pneumocytes of the alveoli, trachea, bronchi, bronchial submucous membrane serous glands [22], and alveolar monocytes and macrophages. The arrival of SARS-CoV-2 to the lungs causes primary severe viral interstitial pneumonia which in about 10% of cases can degenerate into acute respiratory distress syndrome (ARDS) characterized by a cytochemical storm triggered by the activation of interleukin 6 (IL-6) [11]: the Cytokine Storm Syndrome (CSS). Blocking the initial binding of the virus to the ACE2 receptor via the S protein could be one potential treatment approach avenue. In this context, most efforts are aimed at finding pharmacological molecules to inhibit this link. Monoclonal antibodies that target vulnerable sites on viral surface proteins are an emerging approach for treating some rheumatological disease including arthritis. In a study by Wang et al. [23], a human antibody known as 47D11, targeting on communal epitope, was announced to bind to SARS-CoV-2 and SARS-CoV, and to potently inhibit the virus infection of Vero cells.
Tissue-resident alveolar macrophages (AMs) are inhabitant of lungs and are responsible for direct clearance of viruses. A new group of alveolar macrophages, dubbed NAMs (nerve and airway associated macrophages) embryonically derived and self-renewing requiring colony stimulating factor 1, that proliferated robustly following infection in the wild-type mice, where recently identified in lung mice [24]. NAMS help regulate and suppress excessive production of cytokines and immune cell infiltration into tissues. To increase their function or induce their proliferation should be a target for future studies.
Evaluation of the hypothesis/idea
In the absence of a proven effective therapy, current management consists of supportive care, including invasive and noninvasive oxygen support and treatment with antibiotics and heparin. In addition, many patients have received off-label or compassionate-use therapies, including antiretrovirals, antiparasitic agents, anti-inflammatory compounds, and convalescent plasma [25], [26], [27], [28] always in both oral and parenteral formulation.
Aim is to find new opportunity to treat SARS-CoV-2 infection both in early preclinical and in clinical phenotypes using warm humid vaporization (VHM) and oral pharmacological therapies, always looking to surrounding symptoms for holistic clinical interpretation. Pre-infection week and the 2 first weeks may be an important window for any management, according to Paglia phenotypes classification [29] (Box 1).
Box 1. Paglia phenotypes classification.
Lecture by Dr Stefano Paglia, director of the Emergency Department of Lodi, (‘red zone’), Italy, who in collaboration with Chinese colleagues, has managed to identify SARS-CoV-2 positive patients in 5 different phenotypes, which correspond to a possible different therapeutic management [29]:
Phenotype I: patient with fever who does not necessarily present respiratory symptoms, no hypoxia in arterial blood gas analysis and chest x-ray negative. The swab is carried out only if it is considered at risk of previous contact and is safely discharged if, performing a specific respiratory activity test (6′ walking test with an oximeter on the finger), he/she does not show any significant alteration. At their “follow-up” no return to ER was observed with a negative outcome. In these patients, ultrasound of the chest is not recommended, because it will probably be positive and in any case will not indicate hospitalization. These are believed to represent the majority of patients. Quarantine at home and Practitioner control.
Phenotype II: patient with fever plus pulmonary thickening on chest X-ray or in the presence of arterial blood gas hypoxia. The patient must be hospitalized in the medical area and must be observed: in the following hours he can either undergo rapid deterioration or turn towards a significant improvement. The patient cannot be discharged. These patients are approximately 20 times more frequent than those who end up in resuscitation.
Phenotype III: Hypoxia frank to arterial EGA, fever and multiple thickenings to chest x-ray. The patient responds to oxygen therapy set at 15 l / min (i.e. with SpO2 > 90 mmHg with O2), and needs hospitalization in a sub-intensive area.
Phenotype IV: pre-respiratory distress syndrome picture that requires C-PAP (continuous ventilation at positive pressure) to obtain acceptable levels of oxygen pressure / flow ratio (normal values above 350).
Phenotype V: full-blown respiratory distress syndrome, typical of males between 35 and 70 years of age arriving with oxygen pressure values of up to 35–40 mmHg, apparently in less serious conditions than the data show. Here pulmonary ultrasound can make the difference, distinguishing patients with “wet” interstitial syndrome, i.e. only B lines and a sliding conserved, by “dry” patients with an interstitial syndrome composed of multiple pleural sub consolidations but reduced sliding. In the first case, an attempt with C-PAP continuous ventilation at positive pressure is desirable, while in the second, early intubation is mandatory.
Common feature of COVID19 positive patients is leukopenia, associated with respiratory alkalosis on arterial blood gas analysis, with multiple lung consolidations on chest x-ray. CT is not essential and is risky as it requires continuous transport of patients to other departments.
A common feature observed in the hospitals most involved, is that there is a pre-epidemic phase of about a week with some daily / sporadic cases followed by the real epidemic phase in which patients arrive in two waves, one around midday and one around 8 pm.
Preventive implications: Belcaro et al. [10], postulate that humid warm air inhalation by aerosol, vaporisation, nebulization (40°- 41 °C) in the early phases may stop viral replication within hours and may prevent viral contamination, quickly killing respiratory viruses, as also suggested with weak evidence by House et al. [30] for bronchiolitis, in a metanalysis on JAMA Paediatrics. In subsequent cases, the use of warmer humid air (40–41 °C) in ventilation systems and artificial respirators (WHV) can inactivate viruses or stop their replication in the respiratory tract helping the recovery process. In fact, the correlation between lower air/environment temperatures and infections, such as acute viral infections, is one of the pillars of 'common' hygiene and medicine, since viruses die when exposed to warmer air [10].
Therefore, a hairdryer may be effective in reducing the virus pathogenicity and inhibiting its activity also on physical surfaces (handles, computer keyboards, car steering wheel, elevator keys, furnishings or common use on desk, bedside table, etc.) without the need for chemicals that may cause other problems.
Alcoholic solution for oral gargles, practiced for perceived prevention of viral infection and chemotherapeutic agents, including mouth rinses, could have role as adjuncts to daily home care, preventing and controlling supragingival plaque, gingivitis and oral malodor, as Listerine® that offers a anecdotical protection helping to defend the oropharynx and the Waldeyer ring, before the tracheal-bronchial invasion, acting against the oral biofilm which contains many microbial inhabitants including bacteria, viruses and fungi [31], whilst Chlorhexidine is ineffective.
Povidone –iodine (Pi: tested on adeno-, mumps, rota-, polio-(types 1 and 3), coxsackie-, rhino-, herpes simplex, rubella, measles, influenza and human immunodeficiency viruses) instead had a wider virocidal spectrum, covering both enveloped and nonenveloped viruses, Pi eye drops are also commercially available in different concentration, and routinely used before eye surgery [32].
Currently no label specific therapies are available for Covid-19, although many important studies are underway to identify active antiviral drugs. Of these, two in particular are in evidence.
-
-
Remdesivir® (RDV). Is a prodrug of a nucleotide analogue that is intracellularly metabolized to an analogue of adenosine triphosphate that inhibits viral RNA polymerases. RVD has broad- spectrum activity against members of several virus families, including filoviruses (e.g., Ebola) and coronaviruses (e.g., SARS-CoV and Middle East respiratory syndrome coronavirus [MERS-CoV] and has shown prophylactic and therapeutic efficacy in nonclinical models of these coronaviruses.
In vitro testing has also shown that RDV has activity against SARS-CoV-2. RDV appears to have a favorable clinical safety profile, as reported on the basis of experience in approximately 500 persons, including healthy volunteers and patients treated for acute Ebola virus infection, and supported by our data (on file and shared with the World Health Organization [WHO]).
-
-
Tocilizumab®. IL-6R blocker protease inhibitors immunosuppressor humanized monoclonal antibody: suppression of pro-inflammatory IL-1 family and IL-6 have been shown to have a therapeutic effect in many inflammatory diseases, including viral infections [11], to contrast or possibly avoid the CSS. Accumulating evidence suggests that SARS-COV-2 causes an inflammatory response in the lower airway and leads to lung injury. Collectively, virus particles invade the respiratory mucosa first and infect other cells, triggering a powerful immune response with production of a cytokine storm, i.e. a deadly uncontrolled systemic inflammatory response in the body resulting from the release of large amounts of pro-inflammatory cytokines (IFN-α, IFN-γ, IL-1β, IL-6, IL-12, IL-18, IL-33, TNF-α, TGFβ, etc.) and chemokines (CCL2, CCL3, CCL5, CXCL8, CXCL9, CXCL10, etc.) from immune-effector cells in SARS-CoV-2 infection, which may be associated with the critical condition of COVID-19 patients [33]. Besides these, other interesting active antiviral compound under evaluation are noticed; some are included in Box 2. In this setting, is already known that other Authors have also tested the inhalation of α-interferon by aerosol (5 million U at a time for adults in sterile water by injection, twice daily) with weak recommendation [37]. Even tough suggested for reinforcing action on innate immune system, there are not yet confirmative results on BCG vaccination. The transplantation of ACE2-mesenchymal stem cells is still ongoing [38]. Anticoagulants (lmw Heparin) and Antibiotics (mainly Azithromycin) as supportive therapy are widely used. A wide range of competitors have a vaccine in the pipeline, with a large fundraising (even by B&M Gates Foundation), although vaccines seem less successful in older people, because aged immune system do not respond as well to immunization. To treat those infections more infectious and harmful for the elderly, called as geophilic and gerolavic infections, Zhakoronkov [39] on Aging, suggests Rapamycin, Nicotinamide riboside, Metformin, as geroprotectors with known safety profile, for precautionary measure. A tentative to empower the innate immunity with Pentraxin 3 (PTX-n3: a humoral pattern recognition molecule, protein active against other Coronaviruses), for control of Complement activation [40] to also be used as prognostic for death [41], [42] in the CSS, is just tested in an observational protocol at the Spallanzani (COVID Hospital) in Rome; anecdoctical of faster improvement in phenotype III-IV using plasma of recovered positive patients have been reported by Mantua and Pavia Hospitals. Lastly, a trial with Ruxolitinib® selective inhibitor of Janus associate Kinase (JAK1-2) is approved in Italy by AIFA (Italian Drug Agency), for compassionate use in selected severe patients (phenotypes IV – V). Our suggestion is to test remdesivir® (RDV) in the proposed set. Among antiretrovirals, RDV a novel anti-viral drug developed by Gilead Sciences, is a prodrug of a nucleotide analogue that is intracellularly metabolized to an analogue of adenosine triphosphate that inhibits viral RNA polymerases) [43]. Remdesivir® has broad-spectrum activity against members of several virus families, including filoviruses (e.g., Ebola and Marburg virus infection) and coronaviruses (e.g., SARS-CoV and MERS-CoV] and has shown prophylactic and therapeutic efficacy in nonclinical models of these coronaviruses.
Box 2. Active antiviral compound.
-
•
47D11 [23] (if confirmed), human antibody.
-
•
EIDD-1931© / EIDD-2801© demonstrated in mouse and human lung cells in vitro that viruses that show resistance to Remdesivir® experience higher inhibition with the oral compound and viceversa, suggesting that the two drugs could be combined for greater efficacy and to prevent the emergence of resistance [34], holding promise not only to treat COVID-19, but also new coronaviruses that may emerge in the future.
-
•
APN01© is the recombinant form of the human angiotensin-converting enzyme 2 (rhACE2), based on a dual mechanism of action on pulmonary arterial hypertension (PAH), acute lung injury (ALI), acute respiratory distress syndrome (ARDS), and viral binding to soluble ACE2/APN01 avoiding cell infection [35], [36].
-
•
Chloroquine derived drugs (approved off-label by AIFA).
-
•
Colchicine (approved off-label by AIFA).
This drug has shown in vitro and in animals a high capacity to block infection and viral replication with attainable concentrations in human plasma. RDV has been demonstrated to improve pulmonary function and reduce lung viral loads in mice infected with MERS-CoV. It seems that by virological and functional analogy, RDV is one of the few antiviral drugs with proven efficacy against SARS-CoV-2. Currently, RDV is being tested in Italy in patients suffering from COVID-19 pneumonia in severe or moderate form that do not require mechanical ventilation.
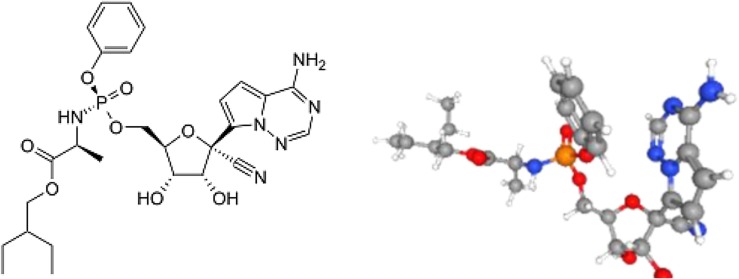
If hot nebulization of RDV (Fig. 3 ), developed to be used intravenously, is administered via aerosol as proposed, SARS-CoV-2 should be sought and monitored at 24 h intervals by RT-PCT (nasopharyngeal swab or aspirated in endotracheal tube) in patients in severe clinical conditions and in intensive care units (ICUs) immediately after aerosol of this antiviral drug, to clarify the local activity other than systemic evolution of the disease. The nucleotide analog, once phosphorylated, works as antimetabolite, being incorporated into growing DNA strands, acting as chain terminator and stops viral DNA. But being not specific to viral DNA, they also affect mithocondrial DNA, generating side effects such as bone marrow suppression. Moreover, it is not known if the RDV hot nebulization could alter the effectiveness of the drug administered by this route. There are approved clinical trial all over the world, trying to demonstrate the in vivo intravenous efficacy of this drug known for its in vitro activity [43]. Two phase III trials in hospitalized adult with mild/moderate (NCT04252664) or severe (NCT04257656) COVID-19 were halted on April 15th for lack of patient (‘’The epidemic of COVID-19 has been controlled well at present, no eligible patients can be recruited’’), whilst Grein et al. [44] in April 10th published on NEJM an interesting clinical improvement in 36 of 53 treated patients (68%). In Italy, several studies involving RDV monotherapy in patients with COVID19 infection of different severity are underway and results are expected in the next two months. The opening of two Gilead sponsored international registration studies is imminent and several Asian and European centers will participate. For the Emilia Romagna region the centers currently included in the study are: AOU of Parma and the AUSL of Piacenza. The EC authorizations of AVEC are in progress. These consist in: 1) A Phase lll RCT in open-open in which 2 different RDV-based regimens (same dose, but different duration) will be compared on a population of 400 patients suffering from COVI-19 pneumonia in severe form that at the time of entry into the study do not require mechanical ventilation; 2) A phase lll open-label RCT in which 2 different RDV-based regimens (same dose, but different duration) versus the standard of care in a population of 600 patients with mild COVI19 pneumonia will be compared. Some SARS-CoV-2 patients have received uncontrolled treatment with other investigational antivirals [45].
Fig. 3.
Remdesivir®, G-S 5734, Gilead Science. A nucleic acid analogue, a sugar and one phosphate group. Image credit: PubChem.
Consequences of the hypothesis and discussion
The hypothesis to be tested is that local instillation of the study products, i.e. RDV directly into the bronchial tree (via WHV) may be as or more effective than systemic doses and reduce patients' exposure to side effects, including increased liver enzymes, diarrhoea, rash, renal failure and hypotension [44]. It should be noted that vaporisation particles have a diameter greater than 8 µm impacting the oropharynx, while aerosol particles, therefore capable of settling at the lower airway level, are between 0,5 and 5 µm in size. So if the hypothesis is to attack the virus in the oropharynx through the binding of SARS-COV-2 with the ACE2 receptor also present in this district, vaporization would be fine (both as suffumigation); but if we have to chase it into the lung, an aerosol is mandatory. Local instillation, vaporization or aerosolization of antivirals with WHV 40°–41 °C can significantly decrease viral replication in hours or 2–3 days at most, in the early stages of respiratory disease (preclinical and phenotype I Straw I [29], (Box 1). The amount of product needed may be minimal, plausibly reducing disease evolution, patient pain and discomfort, drug consumption and social cost.
Vaporization with warmer air can also play a preventive role, and we are considering it [10]
But… On March 23/2020, Gilead suspended access to Remdesivir® for compassionate use (excepting cases of critically ill children and pregnant women), for reasons related to supply, citing the need to continue to provide agent for testing in clinical trials [46]. We summarize here some warnings (Box 3).
Box 3. Warning.
It’s important to observe that:
-
•
Public health measures – the so-called non-pharmaceutical interventions (NPIs) – aimed at reducing contact rates in the population, and thereby reducing virus transmission, could be oriented to: a) mitigation (focused on slowing but not necessarily stopping epidemic spread); or b) suppression (which aims to reverse epidemic growth, reducing case numbers to low levels and maintaining that situation indefinitely, until a vaccine becomes available) [47].
-
•
Wearing personal protection devices, maintaining a high level of personal/hands hygiene.
-
•
Smoking is the most important cause of bronchospasm and bronchial epithelial vasoconstriction. All smokers should be advised to avoid smoking in this situation (unfortunately this is an immediate subjective behaviour for cough and dyspnoea in phenotype I, but to be evaluated in the pre-clinical phase or of suspected or documented infection by swab, even in asymptomatic patient).
-
•
Vasoconstriction – as for cold – may significantly impair the reaction to a virus; mostly in polluted environment.
-
•
To use alcoholic/Pi gargle in pre-clinical subjective oropharyngeal symptoms could act as a protection against progression to tracheal-bronchial involvement.
-
•
To use hot humid aerosol could improve pre-clinical subjective symptoms.
-
•
Aerosol could act as a vector for local pharmaceutical supply.
-
•
Ingestion of nebulized drug and probiotics can positively interfere with intestinal-pulmonary cross-talk.
-
•
At present, there is no drug approved for treating CoV-19 flu, although trials are testing promising compounds; the only therapeutic remedies are those aimed at the side effects caused by the virus, such as inflammation, arterial blood gas hypoxia, myocardial involvement [12], [13] and ARDS till the pulmonary fibrosis, up to now recognized as the first cause of death [48], together with DIC.
-
•
The anatomo-pathological finding of cardio-pulmonary microvascular heavy pathology [12], [13], causing death in 69,44% between older patients with previous cardiovascular disease (CVD) and increased troponin T (TnT), higher D‐dimer and fibrin degradation product (FDP) levels, longer prothrombin time and activated partial thromboplastin time in 71,4% of non‐survivors in the overall mortality of 11.5%, met the Sofa criteria of Disseminated Intravascular Coagulation (DIC) [49]. That means that another cause of death must take in account as viral consequence, mainly in phenotype IV-V, that would impose to add to ventilation, antiviral and IL-storm blocker, the proper anticoagulant therapies.
-
•
Inhaling a mixture of gaseous hydrogen and oxygen, seems obtaining better results than with oxygen alone. It was also noted that individuals vaccinated for viral and/or bacterial infectious diseases were less likely to become infected. The germicidal UV radiation “breaks down” the oxygen O2 which then aggregate into O3 molecules creating an ozone layer, capable of inhibiting viral replication and improving lung respiration. New anti-viral therapies with new drugs should also be take into consideration. For example, microbes are known to bind TLR, inducing IL-1, a pleiotropic cytokine, highly inflammatory, mediator of fever and fibrosis. Therefore, drugs that suppress IL-1 or IL-1R, also used for the treatment of rheumatoid arthritis are to be taken into consideration to fighting COVID-19 [48].
-
•
Low-cost measures like nasal medicated hot vaporisation in preclinical swab-positive asymptomatic patient or in phenotype I, and medicated aerosol in phenotypes II could be suggested, complementary to systemic therapy.
-
•
In hospitalized phenotypes III-V aerosol in oxygen breathing mask with nucleotide analog or IL-6 blocker (acting on the interrelationship between inflammatory cytokines [50]) could be add to systemic and resuscitation therapies.
-
•
Looking for a vaccine, the actual target is to avoid the viral adhesion to ACE2 pulmonary cells receptor where the pro-inflammatory cascade. [48] induces the alveolar edema, inhibit the O2/blood exchange and can evolve in interstitial fibrosis, with microvascular and myocardial involvement. The severity of the disease depends on the efficiency of the immune system which, if weak, cannot stem the infection and its symptoms. A strategy to enhance the anti-inflammatory cytokines or suppress IL-1 or IL-1R, as suggested by Conti et al. [11], would be effective.
-
•
Blocking the IL-6 pro-inflammatory cascade with Tocilizumab® via aerosol may also be tested, having clear in mind the previous weak recommendation for α-interferon, as quoted in text.
-
•
Remdesivir® is a promising drug to act against CoV-1.
The heat and alcohol / Pi susceptibility of SARS-CoV-2 may be a vulnerable point of attack in the conjunctival or pharyngeal by relatively simple means, especially in the context of a pandemic. Early treatment with heated aerosol with antiviral drugs to avoid evolution towards more severe pictures should take into account the advantages of avoiding or improving the patient's severe clinical conditions leading to muscular thoracic respiratory weakness, rhabdomyolysis, involved pulmonary and cardiac microvasculature, hematological dyscrasia and the long subsequent rehabilitation time required when leaving the ICUs. In addition, the reduction of social costs, especially considering that the proposed method can also be used by health systems with tight budgets, especially in low-income countries, until global vaccination is available.
Therefore, the first 2 weeks (incubation - preclinical phase) can be an important window to avoid the progression towards the phases of respiratory distress: it is therefore mandatory to avoid social contact with known people at risk, and to enter quarantine in case of contact with positive people, carefully following the rules. Suggested low level auto prophylaxis (warm domestic aerosol, alcohol/pi gargles, eye drops in case of conjunctivitis [32], [51], [52]) should be started as early as possible as it is free from the risk of side effects, leaving the prescription of a second level active therapy to the physician and social doctors.
The cause of death among infected patients is the severe respiratory insufficiency also linked to severe venous thromboembolism. Critical patients with COVID often develop ARDS and require hospitalization in intensive care, although oxygen therapy and assisted intubation do not always save their lives because of the massive thrombosis that leads to CID.
Further research is needed, including the monitoring of the endemic stroke phase after the pandemic, the so-called Phase 2, mainly in developing countries, under WHO control.
Giovanni Belcaro MD, from the Darwin Lab & Irvine3 Labs and the OOLEX C-virus project, Pescara, Italy, for the opportunity to discuss and share the therapeutic approach.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
Giovanni Belcaro MD, from the Darwin Lab & Irvine3 Labs and the OOLEX C-virus project, Pescara, Italy, for the opportunity to discuss and share the therapeutic approach.
Footnotes
In memoriam: A tribute to Li Wenliang, young Chinese ophthalmologist who served as scientist at the Wuhan Central Hospital, China, who first alerted of this new disease.
Grants: FAR 2019 G D’Annunzio University, Chieti-Pescara, Italy; FAR 2019 University of Ferrara, Italy
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mehy.2020.109876.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Ylikoski J.A., Savolainen S.A., Jousimies-Somer H. Bacterial flora in the nasopharynx and nasal cavity of healthy young men. ORL J Otorhinolaryngol Relat Spec. 1989;51(1):50–55. doi: 10.1159/000276031. [DOI] [PubMed] [Google Scholar]
- 2.Institute for Clinical Systems Improvement. Healthcare guideline: acute pharyngitis, general implementation. Bloomington, MN; 2000. Available from: www.icsi.org.
- 3.Barbini P. Misure dell’apparato respiratorio. Appunti. Publichealth.it/wp-content/uploads/2016/06MISURE-RESPIRATORIE-Medicina.pdf.
- 4.Webster J.G. Strumentazione Biomedica. EdiSES. 2010 [Google Scholar]
- 5.Efron N., Young G., Brennan N.A. Ocular surface temperature. Curr Eye Res. 1989;8:901–906. [PubMed] [Google Scholar]
- 6.Morgan P.B., Tullo A.B., Efron N. Ocular surface cooling in dry eye a pilot study. J British Contact Lens Ass. 1996;19:7–10. [Google Scholar]
- 7.a). Sun X, Zhang X, Chen X, Chen L, Deng CH, et al. The infection evidence of SARS-COV-2 in ocular surface: a single-center cross-sectional study. February 2020. MedRxiv preprint. doi :10.1101/2020.02.26.20027938; b). Chen L, Deng CH, ChenX, Zhang X, Chen B, et al. Ocular manifestations and clinical characteristics of 534 cases of COVID-19 in China: A cross-sectional study. March 2020. MedRxiv preprint. doi: 10.1101/2020.03.12.20034678.
- 8.Guan Wei-jie, Ni Zheng-yi, Hu Yu, Liang Wen-hua, Ou Chun-quan, He Jian-xing, Liu Lei, Shan Hong, Lei Chun-liang, Hui David S.C., Du Bin, Li Lan-juan, Zeng Guang, Yuen Kwok-Yung, Chen Ru-chong, Tang Chun-li, Wang Tao, Chen Ping-yan, Xiang Jie, Li Shi-yue, Wang Jin-lin, Liang Zi-jing, Peng Yi-xiang, Wei Li, Liu Yong, Hu Ya-hua, Peng Peng, Wang Jian-ming, Liu Ji-yang, Chen Zhong, Li Gang, Zheng Zhi-jian, Qiu Shao-qin, Luo Jie, Ye Chang-jiang, Zhu Shao-yong, Zhong Nan-shan. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liang L., Wu P. There may be virus in conjunctival secretion of patients with COVID-19. Acta Ophthalmol. 2020 Mar 18 doi: 10.1111/aos.14413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belcaro G., Cornelli U., Cesarone M.R., Feragalli B., Bombardelli E. Spread of respiratory viruses: Temperature and physical environment temperature control may exploit virus hypo- thermolability. A possible, immediate solution for COVID-19. Med. Clin Res. 2020;5(2) [Google Scholar]
- 11.Conti P., Ronconi G., Caraffa A., Gallenga C.E., Ross R., Frydas I., Kritas S.K. Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV- 2): anti-inflammatory strategies. J Biol Homeost Agents. 2020 Mar 14;32(2) doi: 10.23812/Conti-E. Pii: 1. [DOI] [PubMed] [Google Scholar]
- 12.Guo T., Fan Y. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-2019) JAMA Cardiol. 2020 March 27 doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shi S., Qin M., Shen B., Cai Y., Tao L. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan. Cina. JAMA Cardiol. 2020 March 25 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao Q.Y., Chen Y.X., Fang J.Y. Novel coronavirus infection and gastrointestinal tract. J Dig Dis. 2019;2020 doi: 10.1111/1751-2980.12851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Posid J.M., Bruce S.M., Guarnizo J.T., Taylor M.L., Garza B.W. SARS: mobilizing and maintaining a public health emergency response. J Public Health Manag Pract. 2005;1:208. doi: 10.1097/00124784-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Milne-Price S. The emergence of the Middle East respiratory syndrome coronavirus. Pathog Dis. 2014 Apr 9;7:121–136. doi: 10.1111/2049-632X.12166. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Contini C., Di Nuzzo M., Barp N., Bonazza A., DeGiorgio R., Tognon M. The novel zoonotic COVID-19 pandemic: an expected global health concern. J Infect Dev Ctries. 2020;14:254–264. doi: 10.3855/jidc.12671. [DOI] [PubMed] [Google Scholar]
- 18.van Doremalen N, Bushmaker T, Morris D, Holbrook M, Gamble A, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1.NEJM doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed]
- 19.Addie D.D. Feline coronavirus – that enigmatic little critter. Vet J. 2004;167:5–6. doi: 10.1016/S1090-0233(03)00083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baig AM. Neurological manifestations in COVID-19 caused by SARS-CoV-2 NS Neurosci Ther 2020 Apr 7. doi: 10.1111/cns.13372. [DOI] [PMC free article] [PubMed]
- 21.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhai S.L., Wei W., Lv D.H., Xu Z.H., Chen Q.L. Where did SARS-CoV-2 come from? Vet Rec. 2020;186:254. doi: 10.1136/vr.m740. [DOI] [PubMed] [Google Scholar]
- 23.Wang C, Li W, Drabek D, et al. A human monoclonal antibody blocking SARS-CoV-2 infection. bioRxiv. 2020. doi: 10.1101/2020.03.11.987958. [DOI] [PMC free article] [PubMed]
- 24.Bb Ural, Yeung S.T., Damani-Yokota P. Identification of a nerve-associated, lung-resident interstitial macrophage subset with distinct localization and immunoregulatory properties. Sci Immunol. 2020;5:eaax8756. doi: 10.1126/sciimmunol.aax8756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao Bin, Wang Yeming, Wen Danning, Liu Wen, Wang Jingli, Fan Guohui, Ruan Lianguo, Song Bin, Cai Yanping, Wei Ming, Li Xingwang, Xia Jiaan, Chen Nanshan, Xiang Jie, Yu Ting, Bai Tao, Xie Xuelei, Zhang Li, Li Caihong, Yuan Ye, Chen Hua, Li Huadong, Huang Hanping, Tu Shengjing, Gong Fengyun, Liu Ying, Wei Yuan, Dong Chongya, Zhou Fei, Gu Xiaoying, Xu Jiuyang, Liu Zhibo, Zhang Yi, Li Hui, Shang Lianhan, Wang Ke, Li Kunxia, Zhou Xia, Dong Xuan, Qu Zhaohui, Lu Sixia, Hu Xujuan, Ruan Shunan, Luo Shanshan, Wu Jing, Peng Lu, Cheng Fang, Pan Lihong, Zou Jun, Jia Chunmin, Wang Juan, Liu Xia, Wang Shuzhen, Wu Xudong, Ge Qin, He Jing, Zhan Haiyan, Qiu Fang, Guo Li, Huang Chaolin, Jaki Thomas, Hayden Frederick G., Horby Peter W., Zhang Dingyu, Wang Chen. A trial of Lopinavir–Ritonavir in adults hospitalized with severe Covid-19. N Engl J Med. 2020;382(19):1787–1799. doi: 10.1056/NEJMoa2001282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Touret Franck, de Lamballerie Xavier. Of chloroquine and COVID-19. Antiviral Res. 2020;177:104762. doi: 10.1016/j.antiviral.2020.104762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baden Lindsey R., Rubin Eric J. Covid-19 — the search for effective therapy. N Engl J Med. 2020;382(19):1851–1852. doi: 10.1056/NEJMe2005477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shen Chenguang, Wang Zhaoqin, Zhao Fang, Yang Yang, Li Jinxiu, Yuan Jing, Wang Fuxiang, Li Delin, Yang Minghui, Xing Li, Wei Jinli, Xiao Haixia, Yang Yan, Qu Jiuxin, Qing Ling, Chen Li, Xu Zhixiang, Peng Ling, Li Yanjie, Zheng Haixia, Chen Feng, Huang Kun, Jiang Yujing, Liu Dongjing, Zhang Zheng, Liu Yingxia, Liu Lei. Treatment of 5 critically Ill patients with COVID-19 with Convalescent Plasma. JAMA. 2020;323(16):1582. doi: 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paglia S. Lesson on SARS –CoV-2 clinical phenotypes. Hospital Emergency Dept, Lodi, Italy. Shared with Wuhan doctors, March 16th, 2020.
- 30.House S.A., Gadomski A.M., Ralston S.L. Evaluating the placebo status of nebulized normal saline in patients with acute viral bronchiolitis: a systematic review and meta-analysis. JAMA Pediatr. 2020 Jan 6 doi: 10.1001/jamapediatrics.2019.5195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cortelli J.R., Thénoux R.E. The effect of mouthrinses against oral microorganisms. Braz Oral Res. 2007;21:23–28. doi: 10.1590/S1806-83242007000500005. [DOI] [Google Scholar]
- 32.Kitamura T., Nakagomi O., Matsumoto I., Arita M. Inactivation of human viruses by Povidone-iodine in comparison with other antiseptics. Dermatology. 1997;195(Suppl 2):29–35. doi: 10.1159/000246027. [DOI] [PubMed] [Google Scholar]
- 33.Huang C., Wang Y., Li X., Ren L., Zhao J. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheahan T.P., Sims A.C., Zhou S., Graham R.L., Pruijssers An orally bioavailable broad-spectrum antiviral inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. Sci Transl Med. 2020;2020 doi: 10.1126/scitranslmed.abb5883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Safety and Tolerability Study of APN01 (Recombinant Human Angiotensin Converting Enzyme 2). NCT00886353, 2019.
- 36.APEIRON Biologics Initiates Phase II Clinical Trial of APN01 for Treatment of COVID-19. PipelineReview.com 2 April 2020.
- 37.Uematsu S., Akira S. Toll-like receptors and type I interferons. J Biol Chem. 2007;282:15319–15323. doi: 10.1074/jbc.R700009200. [DOI] [PubMed] [Google Scholar]
- 38.Leng Z., Zhu R., Hou W., Feng Y., Yang Y. Transplantation of ACE2-mesenchimal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11:216–228. doi: 10.14336/AD.2020.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhavoronkov A. Geroprotective and senoremediative strategies to reduce the comorbidity, infection rates, severity, and lethality in gerophilic and gerolavic infections. Aging. 2020 Mar;31:12. doi: 10.18632/aging.102988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gralinski LE, Sheahan TP, Morrison TE, Menachery VD3, Jensen K, et al. Complement Activation Contributes to Severe Acute Respiratory Syndrome Coronavirus Pathogenesis. mBio 2018; Oct 9;9(5). pii: e01753–18. doi: 10.1128/mBio.01753-18. [DOI] [PMC free article] [PubMed]
- 41.Hansen C.B., Bayarri-Olmos R., Kristensen M.K., Pilely K., Hellemann D. Complement related pattern recognition molecules as markers of short-term mortality in intensive care patients. J Infect. 2020;80(4):378–387. doi: 10.1016/j.jinf.2020.01.010. [DOI] [PubMed] [Google Scholar]
- 42.Lee Y.T. Pentraxin-3 as a marker of sepsis severity and predictor of mortality outcomes: a systematic review and meta-analysis. J. Infect. 2018;76(1):1–10. doi: 10.1016/j.jinf.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 43.Sheahan T.P., Sims A.C., Graham R.L., Menachery V.D., Gralinski L.E., Case J.B. Broad- spectrum antiviral GS-5734 inhibits both epidemic and zoonotic coronaviruses. Sci Translat Med. 2017;9:396. doi: 10.1126/scitranslmed.aal3653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, et al. Compassionate Use of Remdesivir for Patients with Severe Covid-19. NEJM April 10, 2020. DOI: 10.1056/NEJMoa2007016. [DOI] [PMC free article] [PubMed]
- 45.World Health Organisation (WHO). https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html.
- 46.Cerullo M. Gilead suspends emergency access to experimental coronavirus drug remdesivir. CBS News. Retrieved 23 March 2020.
- 47.Ferguson NM, Laydon D, Nedjati-Gilani GM, Natsuko I, Kylie A, et al. Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand. Imperial College of Science, Technology and Medicine: 20. Retrieved 22 March 2020.
- 48.Conti P., Gallenga C.E., Tetè G., Caraffa A., Ronconi G. How to reduce the likelihood of coronavirus-19 (CoV-19 or SARS-CoV-2) infection and lung inflammation mediated by IL-1. J Biol Regul Homeost Agents. 2020 Mar 31;34(2) doi: 10.23812/Editorial-Conti-2. [DOI] [PubMed] [Google Scholar]
- 49.Tang Ning, Li Dengju, Wang Xiong, Sun Ziyong. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844–847. doi: 10.1111/jth.v18.410.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franza L., Carusi V., Altamura S., Gallenga C.E., Kritsas S.K. Interrelationship between inflammatory cytokines (IL-1, IL-6, IL-33, IL-37) and acquired immunity. J Biol Regul Homeost Agents. 2019;33:1321–1326. doi: 10.23812/editorial. [DOI] [PubMed] [Google Scholar]
- 51.Nguyen C., Oh L.J., Wong E., Francis I.C. Povidone-iodine 3-minute exposure time is viable in preparation for cataract surgery. Eur J Ophthalmol. 2017;27:573–576. doi: 10.5301/ejo.5000964. [DOI] [PubMed] [Google Scholar]
- 52.Koerner J.C., George M.J., Meyer D.R., Rosco M.G., Habib M.M. Povidone-iodine concentration and dosing in cataract surgery. Surv Ophthalmol. 2018;63:862–868. doi: 10.1016/j.survophthal.2018.05.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.