Abstract
Radiotherapy (RT) is one of the primary cancer treatment modalities. To estimate the actual utilization of RT and infrastructure in Korea, the current study was performed. Data from 2012 to 2016 were extracted from the Health Insurance Review and Assessment Service. In addition, a nationwide survey was conducted to collect the statistics of RT facilities, equipment and human resources in Korea. The total number of patients treated with RT was 72 563 in 2016. The five cancers that were most commonly treated with RT in 2016 were breast, lung, colorectal, liver and prostate cancer. According to analyses of specific treatment modalities, the number of patients treated with intensity-modulated radiotherapy (IMRT), stereotactic radiation therapy (SRT) and proton therapy increased from 6670, 6306 and 50 in 2012 to 21584, 9048 and 703 in 2016, respectively. Ninety radiation oncology centers were working in 2015 and there were a total of 213 megavoltage teletherapy machines. In 2015, 310 patients were treated per megavoltage RT machine, 246 patients per radiation oncologist, 501 patients per medical physicist and 111 patients per radiotherapy technologist. In conclusion, the number of patients who underwent RT in Korea has increased steadily from 2012 to 2016. The IMRT utilization rate remarkably increased in 2016, and the number of patients treated with advanced treatment modalities such as IMRT, SRT and proton therapy is expected to increase.
Keywords: neoplasms, radiotherapy, statistics, infrastructure, Korea
INTRODUCTION
Cancer is a leading cause of death. According to recent statistics, the global burden of cancer has been estimated to have increased to 18.1 million new cases and been responsible for 9.6 million deaths in 2018 [1]. Cancer burden is also rapidly increasing due to population growth, aging and socio-economic changes [2]. In Korea, 229 180 patients were newly diagnosed and 78 194 patients died from cancer in 2016 [3]. The cancer prevalence has risen significantly with an improved survival rate in Korea.
Radiotherapy (RT) is an irreplaceable part of cancer treatment. As the demand for RT increases, modern RT facilities and qualified human resources are also needed. To identify the actual utilization of treatments and status of RT infrastructure, analyses have been performed [4–10]. From 1999 to 2006, the statistics of RT utilization in Korea was reported using questionnaires from each institution [4–7]. However, this was a limitation, as questionnaire-based methods could have recall bias and are time-consuming. Since 2009, the clinical utilization of RT has been demonstrated using national claims data [8, 9]. Because National Health Insurance covers 98% of the Korean population, the claims data collected from the Health Insurance Review and Assessment Service (HIRA) offer valuable information regarding healthcare services in Korea [11]. The data contain details on diagnosis, treatment, procedures, pharmaceuticals and demographic characteristics. The present study was carried out to estimate the clinical utilization of RT in 2016 using claims data from the HIRA.
MATERIALS AND METHODS
We analyzed the claims data from the HIRA between 2012 and 2016. The detailed methods are described in previous reports [8,9]. Table 1 shows the source population criteria for the current study. Patients with diseases corresponding to diagnostic codes C00−C97 or D00−D48 based on the International Classification of Diseases, 10th edition (ICD-10) and those who underwent at least one RT procedure, according to the RT procedure codes, were included. Patients who received two or more courses of RT with interruption in the same year were counted as one.
Table 1.
The customized source population
| List | Criteria |
|---|---|
| Treatment period | 1 January 2012 to 31 December 2016 |
| Type of healthcare facility | Tertiary, secondary, primary, sanatorium |
| Diagnostic code | C00–C97, D00–D48 |
| Type of insurance | Health insurance, medical aid, patriots and veterans affairs’ insurance expenditure by government |
| Hospital region | National |
| Gender | Male, female |
| Age | All ages |
Table 2.
The number of patients according to specific radiotherapy modalities between 2012 and 2016
| Radiation therapy modality | Year | ||||
|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | |
| Brachytherapy | 1409(2.4) | 1396(2.3) | 1251(2.0) | 1242(1.9) | 1302(1.8) |
| Intensity-modulated radiation therapy | 6670(11.2) | 6772(11.0) | 7648(11.9) | 12248(18.5) | 21584(29.7) |
| Stereotactic radiation therapy | 6306(10.6) | 6649(10.8) | 6962(10.9) | 8277(12.5) | 9048(12.5) |
| Proton therapy | 50(0.1) | 33(0.1) | 34(0.1) | 158(0.2) | 703(1.0) |
values are presented as number (%), calculated as the number of each radiotherapy modality over the total number of radiotherapy in each year as a percentage.
We classified the number of patients treated with RT according to primary cancer site, gender and age group. The RT utilization rate was calculated as the ratio of RT cases to the number of newly diagnosed patients that year [3]. The number of patients by geographic region was also analysed, on the basis of the location of the hospital where the patient received RT. In addition, we analysed the number of patients who were treated with specific treatment modalities, such as brachytherapy, intensity-modulated radiation therapy (IMRT), stereotactic radiation therapy (SRT) and proton therapy using each procedure code.
The nationwide survey evaluated RT facilities, equipment and human resources in 2015. Where possible, the data were compared with previous surveys in 2006 [10]. The geographical distribution of RT centers and megavoltage teletherapy machines was analysed.
RESULTS
The total number of patients who received RT in 2012, 2013, 2014, 2015 and 2016 were 59 435, 61 839, 64 069, 66 240 and 72 563, respectively (Fig. 1). The number of patients diagnosed with ICD-10 C- and D-code were 66 763 (92.0%) and 5800 (8.0%) in 2016. The number of patients treated with RT increased by 9.5% in 2016 as compared to that in 2015. The total numbers of male and female patients were 32 902, and 39 661 in 2016. The incidence of cancer and the number of cancer patients who received RT are described in Fig. 2. The rate of utilization of RT among cancer patients increased from 24.3% in 2012 to 29.1% in 2016.
Fig. 1.
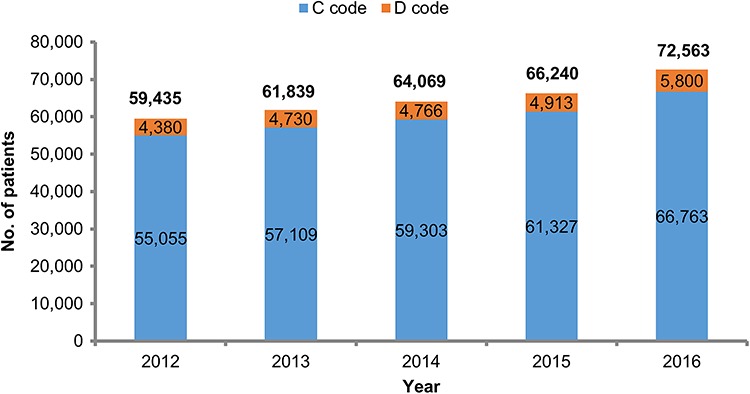
Total number of patients who received radiotherapy between 2012 and 2016 in Korea.
Fig. 2.
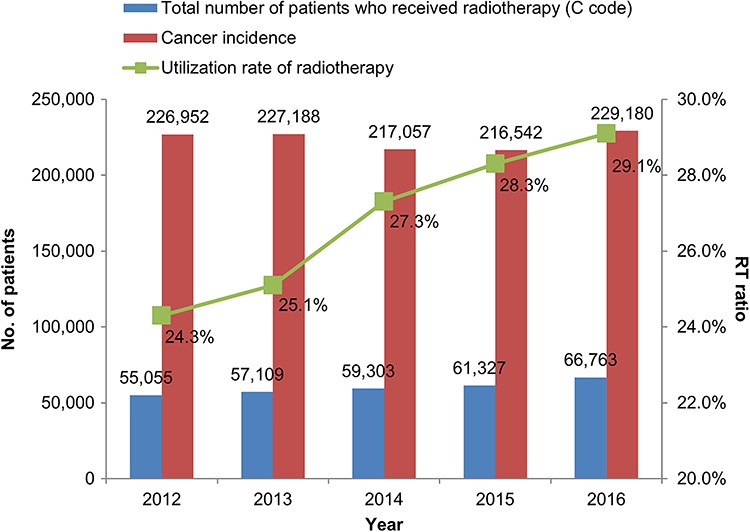
Cancer incidence and the total number of cancer patients who received radiotherapy between 2012 and 2016 in Korea.
The distribution of patients who received RT by diagnosis between 2012 and 2016 is shown in Supplementary Table 1, see online supplementary material. In 2016, patients diagnosed with breast cancer and carcinoma in situ of the breast made up 29.9% of the total patients who received RT. The diseases with ICD-10 ‘D00-D48’ codes accounted for 8% of the total patients who received RT, and carcinoma in situ of the breast was the most common disease.
The five most common diseases treated with RT were breast, lung, colorectal, liver and prostate cancer in 2016 (Fig. 3). Uterine cervical cancer, the fifth most common cancer treated with RT in 2012 was replaced by prostate cancer since 2013. The total number of patients with breast, lung, liver and prostate cancer who received RT has been steadily increasing, whereas the total number of patients with colorectal and uterine cervical cancer who received RT has remained stable between 2012 and 2016.
Fig. 3.
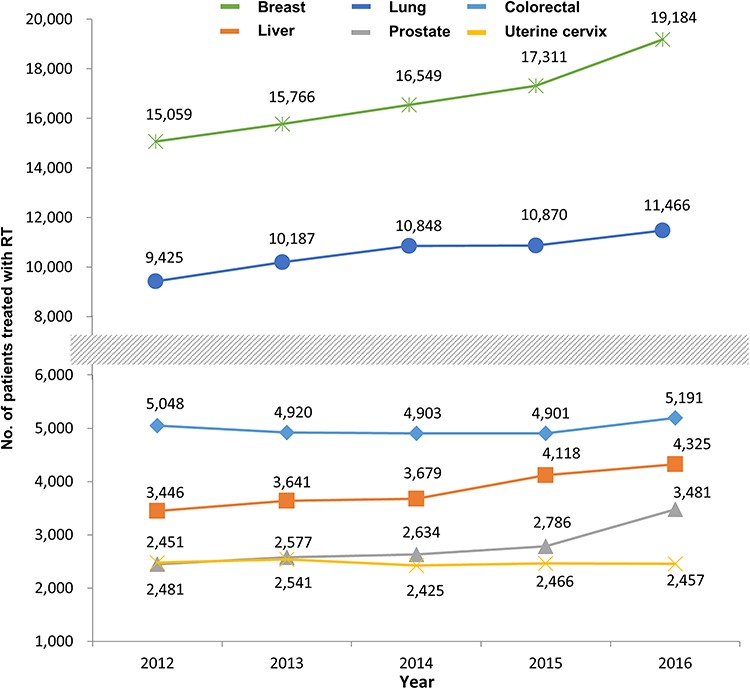
Most common cancers treated with radiotherapy (RT) between 2012 and 2016 in Korea.
The relative ratio of patients receiving RT among those diagnosed with specific cancers is shown in Fig. 4. Although the absolute number of breast cancer patients who received RT increased, the relative proportion of breast cancer patients decreased from 90.0% in 2012 to 87.8% in 2016. The RT utilization ratio of RT increased between 2012 and 2016 for lung (from 42.0 to 44.5%), colorectal (from 17.2 to 18.5%), liver (from 21.0 to 27.4%) and prostate (from 26.2 to 29.5%) cancer. The proportion of patients who received RT for uterine cervical cancer remained about 68% between 2012 and 2016.
Fig. 4.
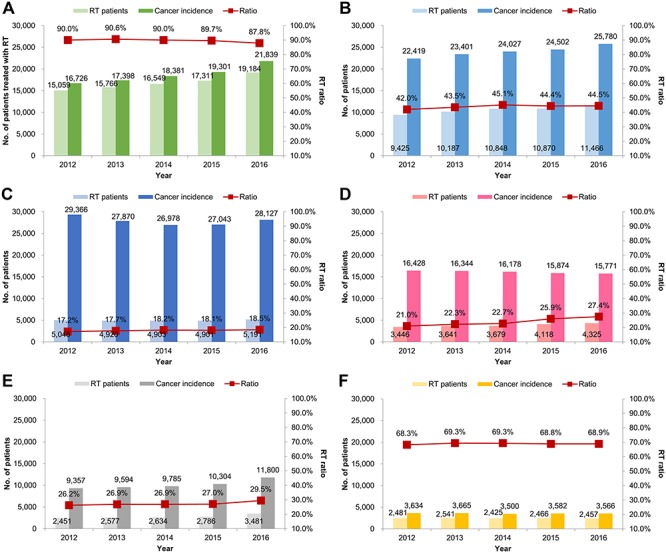
Utilization rate of radiotherapy (RT) for each cancer: (A) breast, (B) lung, (C) colorectal, (D) liver, (E) prostate, and (F) uterine cervix between 2012 and 2016 in Korea.
The number of patients who received RT in 2016 according to diagnosis and age is shown in Supplementary Table 2, see online supplementary material. The most common cancers treated with RT by age group are malignant neoplasm of the brain in patients aged ≤20 years, breast cancer in patients aged 30–50 years and lung cancer in patients aged ≥60 years. This pattern has been continued since 2009 [8, 9].
The utilization pattern of RT according to treatment-specific modalities between 2012 and 2016 is shown in Table 2. Although the number of patients treated with brachytherapy has gradually decreased over time, the number of patients treated with more recent treatment modalities such as IMRT, SRT and proton therapy has increased. The number of patients treated with IMRT and proton therapy increased sharply in 2016. IMRT accounted for 29.7%, SRT for 12.5% and proton therapy for 1.0% of the total RT cases. Table 3 demonstrates the five cancers that were most frequently treated with advanced RT modalities in 2016: head and neck, lung, prostate, breast and colorectum with IMRT; lung, secondary malignant neoplasm (unknown primary), liver, colorectum and breast with SRT; and liver, lung, brain, head and neck, and colorectum with proton therapy.
Table 3.
The five most common cancers treated with IMRT, SRT and proton therapy in 2016
| Intensity-modulated radiotherapy (n = 21 584, %a) | Stereotactic radiation therapy (n = 9048, %a) | Proton therapy (n = 703, %a) | |
|---|---|---|---|
| 1 | Head and neck (17.6%) | Lung (22.3%) | Liver (23.0%) |
| 2 | Lung (13.9%) | Secondary malignant neoplasm (10.6%) | Lung (18.9%) |
| 3 | Prostate (12.8%) | Liver (10.4%) | Brain (12.5%) |
| 4 | Breast (9.1%) | Colorectum (4.7%) | Head and neck (9.5%) |
| 5 | Colorectum (7.1%) | Breast (4.0%) | Colorectum (4.8%) |
aPercentage of number of patients with each disease over the number of patients treated with the specific radiotherapy modality.
Table 4.
Demographic data of patients who received radiotherapy between 2012 and 2016 for each prefecture
| Prefecture | Population (2016) × 103 | Year | ||||
|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | ||
| Seoul | 9805 (19.1) | 26 996 (45.4) | 27 458 (44.4) | 28 305 (45.8) | 29 122 (44.0) | 31 842 (43.9) |
| Gyeonggi, Incheon | 15 584 (30.4) | 11 543 (19.4) | 12 228 (19.8) | 12 858 (20.7) | 13 682 (20.7) | 15 053 (20.7) |
| Gangwon | 1521 (3.0) | 1422 (2.4) | 1365 (2.2) | 1406 (2.3) | 1503 (2.3) | 1721 (2.4) |
| Chungbuk | 1833 (3.6) | 684 (1.2) | 683 (1.1) | 697 (1.1) | 742 (1.1) | 866 (1.2) |
| Chungnam, Daejeon | 3667 (7.2) | 2822 (4.7) | 3029 (4.9) | 3047 (4.8) | 3167 (4.8) | 3517 (4.8) |
| Jeonbuk | 1833 (3.6) | 1334 (2.2) | 1366 (2.2) | 1466 (2.4) | 1393 (2.1) | 1632 (2.2) |
| Jeonnam, Gwangju | 3297 (6.4) | 3024 (5.1) | 3119 (5.0) | 3195 (5.0) | 3359 (5.1) | 3528 (4.9) |
| Gyeongbuk, Daegu | 5143 (10.0) | 4388 (7.4) | 4702 (7.6) | 4922 (7.7) | 4938 (7.5) | 5340 (7.4) |
| Gyeongnam, Busan, Ulsan | 7945 (15.5) | 6774 (11.4) | 7429 (12.0) | 7657 (12.0) | 7805 (11.8) | 8542 (11.8) |
| Jeju | 623 (1.2) | 448 (0.8) | 460 (0.7) | 516 (0.8) | 529 (0.8) | 522 (0.7) |
| Total | 51 251 (100) | 59 435 (100) | 61 839 (100) | 64 069 (100) | 66 240 (100) | 72 563 (100) |
values are presented as number (%)
Table 4 shows the distribution of patients treated with RT between 2012 and 2016 in Korea for each prefecture. The population in Seoul was 19.1% of the total population. However, the number of patients receiving RT in Seoul accounted for 43.9% of the total patients in 2016. Patients receiving RT in Seoul, Gyeonggi and Incheon constituted 64.6% of the treatment cases.
The number of patients treated with brachytherapy, IMRT and SRT according to the different regions is shown in Supplementary Table 3, see online supplementary material. Brachytherapy was not performed in Chungbuk and Jeju, and 3.9% of all the patients were treated with brachytherapy in Jeonnam and Gwangju. The rate of patients treated with IMRT varied according to the region (13.5% for Chungbuk and 35.4% for Jeju). SRT was performed in 0.8% of the patients in Chungbuk and 17.2% in Seoul.
Table 5 demonstrates RT infrastructure in Korea, and the changes in radiation oncology infrastructure and human resources are shown in Supplementary Table 4, see online supplementary material. Radiation oncology facilities have steadily increased over the past 10 years and reached 90 centers in 2015, showing an increase of 48% since 2006. There were a total of 213 megavoltage teletherapy machines, showing an increase of 88% since 2006. Furthermore, there were 269 radiation oncologists, 132 medical physicists, 595 radiotherapy technologists and 187 nurses in 2015. In 2015, 310 patients were treated per megavoltage teletherapy machine, 246 patients per radiation oncologist, 501 patients per medical physicist and 111 patients per radiotherapy technologist. The number of RT centers and machines for each prefecture is shown in Table 6. In Korea, the ratio of megavoltage teletherapy machines to the population is 4.2 per million. The distribution of facilities and machines per million inhabitants varied, ranging from 1.3 unit per million in Chungbuk to 8.3 unit per million in Seoul.
Table 5.
Radiotherapy infrastructure of Korea in 2015
| Number | |
|---|---|
| Radiotherapy centers | 90 |
| Medical accelerators | Total 196 |
| Linear accelerators (Linacs) | 163 |
| (Linacs with IMRT) | (134) |
| (Linacs with IGRT) | (62) |
| CyberKnife | 11 |
| Helical tomotherapy units | 20* |
| Proton accelerator | 1 |
| Radionuclide units | Total 19 |
| GammaKnife | 18 |
| Viewray | 1 |
| Brachytherapy equipment | Total 31 |
| Afterloaders | 31 |
*One unit of Vero was included.
Table 6.
Demographic data of radiotherapy infrastructure in 2015 for each prefecture
| Prefecture | Population (2015) × 103 | No. of radiotherapy centers | Megavoltage teletherapy machines | ||
|---|---|---|---|---|---|
| No. of machines | Mean no. of machines per center | Machines per million people | |||
| Seoul | 9860 | 26 | 82 | 3.2 | 8.3 |
| Gyeonggi, Incheon | 15 284 | 22 | 47 | 2.1 | 3.1 |
| Gangwon | 1506 | 4 | 6 | 1.5 | 4.0 |
| Chungbuk | 1561 | 1 | 2 | 2.0 | 1.3 |
| Chungnam, Daejeon | 3822 | 8 | 15 | 1.9 | 3.9 |
| Gyeongbuk, Daegu | 5097 | 10 | 18 | 1.8 | 3.5 |
| Gyeongnam, Busan, Ulsan | 7827 | 11 | 27 | 2.5 | 3.4 |
| Jeonbuk | 1798 | 3 | 3 | 1.3 | 2.2 |
| Jeonnam, Gwanju | 3274 | 3 | 10 | 3.3 | 3.1 |
| Jeju | 587 | 2 | 2 | 1.0 | 3.4 |
| Total | 50 616 | 90 | 213 | 2.4 | 4.2 |
DISCUSSION
The current study assessed the clinical utilization of RT between 2012 and 2016 in Korea using recently registered claims data from the HIRA. In 2016, the total number of patients treated with RT was 72 563, significantly increased by 9.5% as compared to that in 2015. The utilization rate of RT in cancer patients was 29.1% in 2016. IMRT was performed for 29.7%, SRT for 12.5% and proton therapy for 1.0% of the total RT cases.
The incidence of cancer is rapidly increasing worldwide [1]. A total of 229 180 cancer patients were newly diagnosed in 2016 in Korea [3]. According to recent statistics, stomach cancer was the most common cancer followed by colorectal, thyroid, lung and breast cancer. In the present study, the five cancers that were most commonly treated with RT were breast, lung, colorectal, liver and uterine cervical cancer. The number of uterine cervical cancer cases treated with RT remained unchanged, but the RT utilization increased steadily for most of the cancers.
In Australia, decision tree models were developed according to epidemiological data and RT indications based on evidence-based treatment guidelines [12]. They revealed that RT has been indicated in nearly half of the newly diagnosed cancer patients. The overall optimal RT utilization rate was found to be 48% in 2012 (34% for curative and 14% for palliative aim). It provides significant 5-year local control and survival benefits (10% and 2.4%, respectively) [13]. From population-based cancer registries, the optimal utilization rate of RT ranges from 47 to 53% in Europe [14]. The European Society for Radiotherapy and Oncology-Health Economics in Radiation Oncology (ESTRO-HERO) study also expects a 16% increase in the proportion of patients receiving RT by 2025 [15]. In the current study, the actual RT utilization rate steadily increased from 24.3% in 2012 to 29.1% in 2016. Although the distribution of disease and its stages are different across the countries, the RT utilization rate in Korea seems to be relatively low as compared to that in other countries. To increase the utilization rate of RT, physicians could find more patients who are indicated for RT from the multidisciplinary team care. In Korea, the 5-year relative survival rate for patients diagnosed recently has improved: it was 41.2% in patients diagnosed between 1993 and 1995 and 70.6% for patients diagnosed between 2012 and 2016 [3]. Furthermore, the need for RT in elderly cancer patients is expected to rise with improving life expectancy [16]. Because advances in RT technology could reduce treatment-related toxicities and improve quality of life, these precise RT techniques allow more patients to be safely and effectively treated.
The development of RT techniques such as IMRT, SRT and proton therapy has enabled the irradiation of tumors with high radiation doses and has reduced treatment-related toxicity. As a result, the use of advanced RT techniques has been increasing worldwide. In the USA, analysis based on private insurance claims revealed that IMRT constituted 39% of all radiation treatment claims in 2014 [17]. In 2010, a survey carried out in the UK and Canada reported that 76 and 72% of the centers offer IMRT, respectively [18, 19]. In New Zealand, IMRT and SRT were available in 100% and 86% of surveyed centers in 2015, respectively [20]. Although the availability of the treatment was similar, a significant variation existed in application of the treatment between centers. The Japan Society of Medical Physics performed a web-based survey to assess the current use of advanced RT techniques [21]. They described the detailed implementation status of SRT, IMRT, image-guided RT and respiratory motion management according to the questionnaire. IMRT and SRT were provided at 66 and 77% of participating institutions, respectively. For image-guided RT, target-based image registration using integrated computed tomography was most frequently applied. In addition, breath holding was the most commonly used technique for respiratory motion management. In Korea, IMRT increased from 6670 to 21 584 cases from 2012 to 2016 and accounted for 29.7% of the patients receiving RT in 2016. Because national insurance has been extended to cover IMRT for all cancers since 2016 in Korea, it is expected that the number of patients receiving IMRT will increase to the rate of the developed countries in the next report. In this study, we could not demonstrate the detailed RT practice because of the limited information from the HIRA database. If both analysis of HIRA data and an online-based survey are performed together, we will be able to investigate in-depth the current utilization of RT.
SRT is a technique delivering high ablative radiation doses within a limited number of fractions, and the biological mechanisms of SRT have been investigated [22]. In Korea, SRT accounted for 12.5% of total radiation therapy in 2016, as in 2015. Lung, secondary malignant neoplasm including bone or brain metastases, and liver cancers were frequently treated with SRT. Because high-dose irradiation may increase tumor antigen release and enhance the effect of checkpoint inhibition, there has been profound interest in the synergistic effects of RT and immunotherapy [23]. Recent phase II studies reported well tolerable combination treatment and promising progression-free survival and response rate, although the study by Theelen et al. did not meet the study criteria for meaningful clinical benefit [24, 25]. In addition, two randomized trials demonstrated outstanding clinical outcomes of SRT for patients with limited metastatic disease [26, 27]. Several trials registered with ClinicalTrials.gov (number NCT03833154, NCT03148327 and NCT03391869) are still underway to investigate the effects of SRT and immune checkpoint inhibitors. The clinical utilization of SRT may be extended with the outcomes of these research studies.
Two proton facilities have been working in Korea since April 2016, and the number of patients treated with proton therapy has increased from 158 in 2015 to 703 in 2016. In Japan where a clinical trial using proton beam treatment started in 1979, ~3000 patients received proton therapy in 2013, and 11 facilities were available in 2016 [28]. The major treatment sites were prostate, liver, head and neck, and lung cancers between 1979 and 2013. The number of patients treated with proton therapy for pediatric, esophageal and pancreatic cancers has been increasing. In Korea, liver, lung, brain, head and neck, and colorectal cancers were the most frequently treated with proton therapy. Compared with the Japanese study, the difference in therapeutic targets seems to be attributable to the accessibility of proton facilities and the studies in which the efficacy of proton therapy has been recently published.
In 2016, although the population of Seoul was only 19.1% of the overall population, 43.9% of patients receiving RT were treated in Seoul. The concentration of patients in Seoul has been observed in previous studies as well [8, 9]. Furthermore, the current study revealed that there is a disproportion in the infrastructure between regions: 82 (38.5%) of 213 megavoltage teletherapy machines were installed in Seoul. Rim et al. [29] observed various utilization rates of IMRT according to the regional area. The utilization of IMRT increased from 2010 to 2016 regardless of the region. IMRT was more frequently used in the capital areas (Seoul, Incheon and Gyeonggi) and metropolitan areas (Seoul, Daegu, Daejeon, Gwangju, Busan, Incheon, Ulsan and Gyeonggi province). We also demonstrated various utilization rates of brachytherapy, IMRT, SRT and proton therapy according to region. The various utilization rates might have resulted from the distribution of the cancer being treated and the types of equipment present in the various institutions.
CONCLUSIONS
In conclusion, the total number of patients who received RT in Korea has steadily increased up to 2016. The utilization of IMRT predominantly increased in 2016 due to the extended coverage of national insurance. In addition, the number of patients treated with SRT and proton therapy is expected to increase with ongoing clinical studies and newly implemented facilities.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by a Korea Institute of Radiological and Medical Sciences (KIRAMS) grant (No. 50432-2018) and a National Research Foundation of Korea (NRF) grant (No. 2019M2A2B4095150), funded by the Korean government (the Ministry of Sciences and ICT).
CONFLICT OF INTEREST
None declared.
References
- 1. Global cancer observatory Lyon: International Agency for Research on Cancer; c2018. https://gco.iarc.fr. Accessed Oct 10, 2019.
- 2. Bray F, Ferlay J, Soerjomataram I et al. . Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 3. Jung KW, Won YJ, Kong HJ et al. . Cancer statistics in Korea: Incidence, mortality, survival, and prevalence in 2016. Cancer Res Treat 2019;51:417–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yoo SY, Kim MS, Ji YH et al. . Statistics for department of radiation oncology (1999-2001). J Korean Soc Ther Radiol Oncol 2004;22:234–6. [Google Scholar]
- 5. Kim MS, Ji YH, You SY et al. . National statistics of radiation oncology in Korea (2002-2004). J Korean Soc Ther Radiol Oncol 2006;24:77–80. [Google Scholar]
- 7. Ji YH, Kim MS, You SY et al. . National statistics of radiation oncology in Korea (2006). J Korean Soc Ther Radiol Oncol 2008;26:131–3. [Google Scholar]
- 8. Kang JK, Kim MS, Jang WI et al. . The clinical utilization of radiation therapy in Korea between 2009 and 2013. Radiat Oncol J 2016;34:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seo YS, Kim MS, Kang JK et al. The clinical utilization of radiation therapy in Korea between 2011. and 2015. Cancer Res Treat 2018;50:345–55. [DOI] [PMC free article] [PubMed]
- 10. Huh SJ; Korean Society of Therapeutic Radiology and Oncology (KOSTRO) Current status of the infrastructure and characteristics of radiation oncology in Korea. Jpn J Clin Oncol 2007;37:623–7. [DOI] [PubMed] [Google Scholar]
- 11. Kim JA, Yoon S, Kim LY et al. . Towards actualizing the value potential of Korea health insurance review and assessment (HIRA) data as a resource for health research: Strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci 2017;32:718–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barton MB, Jacob S, Shafiq J et al. . Estimating the demand for radiotherapy from the evidence: A review of changes from 2003 to 2012. Radiother Oncol 2014;112:140–4. [DOI] [PubMed] [Google Scholar]
- 13. Hanna TP, Shafiq J, Delaney GP et al. . The population benefit of evidence-based radiotherapy: 5-year local control and overall survival benefits. Radiother Oncol 2018;126:191–7. [DOI] [PubMed] [Google Scholar]
- 14. Borras JM, Lievens Y, Dunscombe P et al. . The optimal utilization proportion of external beam radiotherapy in European countries: An ESTRO-HERO analysis. Radiother Oncol 2015;116:38–44. [DOI] [PubMed] [Google Scholar]
- 15. Borras JM, Lievens Y, Barton M et al. . How many new cancer patients in Europe will require radiotherapy by 2025? An ESTRO-HERO analysis. Radiother Oncol 2016;119:5–11. [DOI] [PubMed] [Google Scholar]
- 16. Pfeffer MR, Blumenfeld P. The changing paradigm of radiotherapy in the elderly population. Cancer J 2017;23:223–30. [DOI] [PubMed] [Google Scholar]
- 17. Pan HY, Jiang J, Shih YT et al. . Adoption of radiation technology among privately insured nonelderly patients with cancer in the United States, 2008 to 2014: A claims-based analysis. J Am Coll Radiol 2017;14:1027–33. [DOI] [PubMed] [Google Scholar]
- 18. Mayles WP. Radiotherapy development board. Survey of the availability and use of advanced radiotherapy technology in the UK. Clin Oncol (R Coll Radiol) 2010;22:636–42. [DOI] [PubMed] [Google Scholar]
- 19. AlDuhaiby EZ, Breen S, Bissonnette JP et al. . A national survey of the availability of intensity-modulated radiation therapy and stereotactic radiosurgery in Canada. Radiat Oncol 2012;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Padayachee J, Loh J, Tiong A et al. . National survey on image-guided radiotherapy practice in New Zealand. J Med Imaging Radiat Oncol 2018;62:262–9. [DOI] [PubMed] [Google Scholar]
- 21. Akino Y, Tohyama N, Akita K et al. . Modalities and techniques used for stereotactic radiotherapy, intensity-modulated radiotherapy, and image-guided radiotherapy: A 2018 survey by the Japan Society of Medical Physics. Phys Med 2019;64:182–7. [DOI] [PubMed] [Google Scholar]
- 22. Kim MS, Kim W, Park IH et al. . Radiobiological mechanisms of stereotactic body radiation therapy and stereotactic radiation surgery. Radiat Oncol J 2015;33:265–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rodríguez-Ruiz ME, Vanpouille-Box C, Melero I et al. . Immunological mechanisms responsible for radiation-induced abscopal effect. Trends Immunol 2018;39:644–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Theelen WSME, Peulen HMU, Lalezari F et al. . Effect of pembrolizumab after stereotactic body radiotherapy vs pembrolizumab alone on tumor response in patients with advanced non–small cell lung cancer: Results of the PEMBRO-RT phase 2 randomized clinical trial. JAMA Oncol 2019; Jul 11. [Epup ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bauml JM, Mick R, Ciunci C et al. . Pembrolizumab after completion of locally ablative therapy for oligometastatic non–small cell lung cancer: A phase 2 trial. JAMA Oncol 2019; Jul 11. [Epup ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Palma DA, Olson R, Harrow S et al. . Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): A randomised, phase 2, open-label trial. Lancet 2019;393:2051–8. [DOI] [PubMed] [Google Scholar]
- 27. Gomez DR, Tang C, Zhang J et al. . Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: Long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol 2019;37:1558–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sakurai H, Ishikawa H, Okumura T. Proton beam therapy in Japan: Current and future status. Jpn J Clin Oncol 2016;46:885–92. [DOI] [PubMed] [Google Scholar]
- 29. Rim CH, Lee J, Kim WC et al. . A survey of radiation therapy utilization in Korea from 2010 to 2016: Focusing on use of intensity-modulated radiation therapy. J Korean Med Sci 2018;33:e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


