Abstract
The role of smoking cessation treatments in the link between clean indoor air laws and cigarette taxes with smoking cessation is not known. This study examined whether the use of smoking cessation treatments mediates the association between clean indoor air laws and cigarette excise taxes, on the one hand, and recent smoking cessation, on the other hand. Using data on 62,165 adult participants in the 2003 and 2010–2011 Current Population Survey-Tobacco Use Supplement who reported smoking cigarettes in the past year, we employed structural equation models to quantify the degree to which smoking cessation treatments (prescription medications, nicotine replacement therapy, counselling/support groups, quitlines, and internet-based resources) mediate the association between clean indoor air laws, cigarette excise taxes and recent smoking cessation. Recent smoking cessation was associated with clean indoor air laws in 2003 and with both clean indoor air laws and excise taxes in 2010–2011. Smoking cessation treatments explained between 29% to 39% of the effect of clean indoor air laws and taxes on recent smoking cessation. While clean indoor air laws remained significantly associated with the recent smoking cessation over the first decade of the 2000s, excise taxes gained a more prominent role in later years of that decade. The influence of these policies was partly mediated through the use of smoking cessation treatments, underscoring the importance of policies that make these treatments more widely available.
INTRODUCTION
Cigarette smoking remains an entrenched public health challenge, with 14% of U.S. adults classified as current smokers.1 Despite recent decreases in its prevalence2 and increases in quit attempts3,4 smoking continues to be associated with more than 480,000 deaths each year,5 making it the foremost cause of preventable death in the U.S. Cessation of smoking can lessen this health risk and extend the lives of former smokers.5–7 An increasing number of effective cessation treatment options are available.8,9 Despite this, relatively little is known about the structural factors that drive individuals towards smoking cessation treatment.
The past two decades have seen a dramatic rise in the prominence and scope of tobacco control policies. In a systematic review, clean indoor air laws and cigarette excise taxes were identified as the tobacco control policies most consistently associated with reductions in smoking behavior.10 Clean indoor air laws–which prohibit smoking in public spaces such as workplaces, bars, and restaurants–are associated with reductions in cigarette consumption, smoking initiation, and exposure to second-hand smoke.11–15 These laws may impact smoking cessation intentions and behaviors through effects on attitudes, norms, and perceived self-efficacy for quitting.16 Taxes on cigarettes are associated with reduced prevalence of smoking,17,18 and have a strong impact on smoking among individuals who are especially vulnerable to cigarette use initiation, such as young people.19,20 Existing evidence suggests that cigarette taxes also impact smokers’ decisions to quit or reduce smoking.21,22
Despite evidence of effects of tobacco control policies on smoking cessation, it is not known whether these policies impact the use of smoking cessation treatments (e.g., pharmacotherapy or behavioral counseling). With increases in health insurance coverage of cessation treatments,23,24 the proportion of quit attempts unassisted by pharmacological or behavioral interventions has decreased over time,25 which suggests that more smokers than ever turn to some form of cessation treatment when attempting to quit. These trends in cessation treatment use coincide with the expansion of clean indoor air laws and increases in excise taxes, but it is unclear whether increased use of smoking cessation treatments explains the observed association between these tobacco control policies and smoking patterns, and if so, to what extent.
In a previous report, we observed a significant reduction in smoking behavior between 2003 and 2010–2011, which was largely mediated by changes in clean indoor air laws and excise taxes.26 The current study builds on this report by evaluating the extent to which the association between state and local cigarette excise taxes and clean indoor air laws with recent smoking cessation is mediated by use of smoking cessation treatments. We used data from the American Nonsmokers’ Rights Foundation (ANRF) on state and local cigarette excise taxes and clean indoor air laws. Data on smoking behavior and use of cessation treatments was derived from the 2003 and 2010/2011 Current Population Survey-Tobacco Use Supplement (CPS-TUS). We hypothesized that use of smoking cessation treatments would account for a significant proportion of the observed association of clean indoor air laws and cigarette excise taxes with recent smoking cessation in both 2003 and 2010–2011.
METHODS
Sample
The CPS-TUS, a national population-level study of tobacco use, is conducted at regular intervals in conjunction with the CPS. We used data from the 2003 and the 2010 and 2011 CPS-TUS waves. In 2003, the supplement was administered in February, June, and November; in 2010 and 2011, TUS was administered in May and August 2010, and January 2011. CPS used multi-stage stratified sampling to interview a nationally representative sample of the civilian, non-institutionalized U.S. population aged 15 years and older in 2003 and 18 years and older in 2010–2011. The CPS-TUS was completed by approximately 64% of respondents by telephone and 36% in person. While most interviewees reported on their own tobacco use behavior, 20% reported as proxies for household members. Additional information about the CPS-TUS is available from the CPS-TUS website (https://cancercontrol.cancer.gov/brp/tcrb/tus-cps/).
Our sample was limited to past-year adult smokers, aged 18 and older, who reported on their own smoking behavior in CPS-TUS. A total of 34,842 participants in 2003 and 27,323 in 2010–2011 met these criteria and were included.
Variables
Past year smoker status was determined by asking participants about their smoking pattern during the 12 months immediately prior to the interview. For this study, those who reported smoking every day or on some days one year ago were treated as past-year smokers.
Recent smoking cessation was ascertained by the response, “not at all”, to the question: “Do you now smoke cigarettes every day, some days, or not at all?” among past-year smokers. Among people who responded “not at all”, 82.7% had last smoked 30 days or longer before the time of interview. Nevertheless, as this measure of smoking cessation likely captures many individuals who return to smoking within a few weeks or months, we used the qualifier “recent”.
Applicable state and local clean indoor air laws and cigarette excise taxes were ascertained for each participant at the time point one year prior to their CPS-TUS interview. This timeframe was selected because CPS-TUS questions about smoking behavior referred to the past year. For example, for an individual interviewed in January 2011 CPS-TUS, laws and taxes in effect in January 2010 were ascertained. For clean indoor air laws, we obtained data from ANRF on state and county clean indoor air laws separately for laws that affect workplace areas, bars, and restaurants. We used the following categorization, developed by ANRF,27 of these laws: 1) “100% smoke free policy”; 2) “qualified 100% smoke free policy”; 3) laws providing “some” coverage; and 4) a category of “no coverage” for jurisdictions with no clean indoor air laws. We coded these laws from 4 for “100% smoke free policy” to 1 for “no coverage”. When the applicable state and county laws for a participant were inconsistent with one another, we based the analyses on the more comprehensive law. While some states pre-empt, or do not allow, localities to impose their own tobacco control laws, the number of such pre-emptive state laws affecting clean indoor air policies decreased markedly in the study period: in 2000, 18 states had these laws but only 12 states had them in 2010.28 The state and county policy data were linked to the CPS-TUS data via state and county FIPS codes. Because state and local laws affecting workplaces, bars, and restaurants are strongly correlated (r range=.61 to .83), an average clean indoor air law index was computed by averaging over the three sets of laws. Data for cigarette excise taxes were also obtained from ANRF; federal, state, and local taxes were summed to compute a total excise tax (median [IQR] was $0.94 [$0.67-$1.37] in 2003 and $2.16 [$1.80-$3.00] in 2010–2011). In cases where county clean indoor air law or tax information were not available (66.5% for laws and 64.6% for taxes), we used state information only.
Cessation treatments were assessed by asking past-year smokers who had quit about the methods they had used. These methods included nicotine replacement treatment (NRT) (nicotine gum, lozenge, patch, inhaler, or nasal spray); prescription pills (Zyban, Wellbutrin, or bupropion; Chantix or varenicline was added in 2010–2011); telephone help line or quitline; one-on-one counseling, stop smoking clinic, class, or support group (combined into “counseling/groups”); and internet-based resources.
In addition to questions about smoking and smoking cessation treatments, CPS-TUS collected sociodemographic data including sex, age, race/ethnicity, whether born in the US or other countries, education level, marital status, and employment status. We also adjusted the analyses for state-level expenditure for tobacco prevention programs compared to US Centers for Disease Control and Prevention (CDC) recommended expenditure for years 2003 and 2011 compiled by the Tobacco-Free Kids organization (https://www.tobaccofreekids.org/assets/factsheets/0209.pdf).
Analyses
We analyzed the data in three stages. First, we examined the association between clean indoor air laws and excise taxes with recent smoking cessation using multivariable logistic regression models. These analyses were conducted separately for the 2003 and the 2010–2011 periods. The odds ratios from these logistic models represent the change in the odds of the outcome for every 1 higher score on the summary index for clean indoor air laws described above or every $1.00 higher taxes. The models were adjusted for sociodemographic characteristics, including sex, age, race/ethnicity, being born in the US, marital status, education, employment status, and state expenditure on tobacco prevention. Analyses were conducted separately for the 2003 and 2010–2011 periods, as we believed that the association of laws or taxes might vary between the two time periods and also to remove the potential confounding effect of time-varying factors (e.g., temporal changes in attitudes).
Second, we conducted mediation analyses using structural equation modeling (SEM) with binary outcomes and multiple binary mediators29,30 to examine the extent to which significant associations between policies and recent smoking cessation were mediated by use of smoking cessation treatments. The SEM mediation model would have a causal interpretation under a number of assumptions, including “sequential ignorability,” which implies no unmeasured confounding of the relationship of the exposure with the mediators and of the mediators with the outcome.31 This assumption cannot be tested. However, in this case, is theoretically plausible. Further, we strived to limit such confounding by adjusting the analyses for individual and contextual factors that could potentially act as confounders. Finally, by conducting analyses separately for 2003 and 2010–2011, we limited confounding by time-varying contextual factors such as public attitudes towards smoking.
Another important assumption of SEM mediation analysis is absence of interaction between the exposures and mediators. We conducted joint tests of interaction between the mediators and the exposures of interest in a series of logistic models in which we regressed recent smoking cessation on the exposures (clean indoor air laws and taxes), the mediators (smoking cessation treatments) and the interaction of the exposures with mediators. Separate regression models were run for clean indoor air laws in 2003, clean indoor air laws in 2010–2011 and taxes in 2010–2011 which were significantly associated with smoking cessation in stage two analyses. None of the joint tests of interactions of exposures and mediators reached the p<.05 significance level (data not shown).
Three sets of SEM mediation models were run: one each for clean indoor air laws of 2003 and 2010–2011, and one for excise taxes of 2010–2011. These models were adjusted for the same sociodemographic characteristics listed above. The models allowed us to compute odds ratios for the associations of the policies with each treatment and the odds ratios for the association of receiving each treatment with recent smoking cessation. Also, the odds ratio for the direct association of policies with recent smoking cessation could be computed in these models.
In a further step, analyses were repeated using the potential outcomes modeling approach proposed by Vanderweele and colleagues.32 This model can accommodate binary outcomes and mediators, interactions between exposures and mediators and adjust for covariates. The model allows for computing a “marginal total effect,” defined as the overall effect of the exposure on the outcome, a “natural indirect effect,” defined as the effect of the exposure on the outcome that is due to the effect of exposure on mediators and a “natural direct effect,” defined as the effect of exposure on the outcome via pathways that do not involve the mediator of interest.
All analyses were conducted using Stata 16 software (StataCorp LLC, College Station, TX, 2019) from April 2019 to April 2020. SEM analyses were conducted using the gsem routine of Stata which accommodates complex survey data, multiple mediators, and binary outcome and mediator variables. Survey and replicate weights were included in these analyses to compute population representative estimates and confidence intervals.
The potential outcome modeling was implemented in the Stata paramed program.32 The paramed program does not accommodate multiple mediators or weights. Therefore, smoking cessation treatments were combined into a binary measure of any treatment vs. none and survey weight were not used for these analyses. However, all individual and contextual covariates used in the main analyses were included in these analyses.
RESULTS
Characteristics of past-year smokers in the 2003 and the 2010–2011 samples have been described elsewhere.26 Briefly, the majority of participants in both time periods were male (53.7% in 2003 and 54.1% in 2010–2011), non-Hispanic white (75.7% and 74.4%), US born (91.2% and 90.9%), had at least high school diploma or GED (80.3% and 82.7%), and currently employed (66.0% and 58.6%). The average age of the participants was 41.41 years (standard error [SE]=0.05) in 2003 and 42.69 years (SE=0.10) in 2010–2011. The proportion married or living as married was 43.7% in 2003 and 39.9% in 2010–2011.
Variations in clean indoor air laws and taxes in the two time periods were also previously reported.26 State and county governments varied considerably in their adoption of tobacco control policies and the strength and coverage of these policies changed markedly over time. In 2003, only 1.9% of past-year smokers lived in states and localities with 100% smoke-free workplace laws, 8.2% in states and localities with 100% smoke-free bar laws, and 9.0% in states and localities with 100% smoke-free restaurant laws. These numbers increased to 47.7%, 44.3% and 53.5%, respectively, in 2010–2011. Excise taxes also increased over time from an average of $1.00 (SE=0.001) to $2.25 (SE=0.005).
Overall, 7.3% of past-year smokers in 2003 and 7.8% in 2010–2011 quit smoking. The methods used for quitting smoking changed between 2003 and 2010–2011 (Table 1). While the overall prevalence of NRT did not change and this method was the most common method in both times, the specific type of treatment did change: the use of gum/lozenge increased, whereas the use of inhaler/nasal spray decreased. The use of bupropion also decreased, although it was potentially replaced by varenicline, which was only assessed in the 2010–2011 survey. Overall, the use of prescription medications increased from 7.5% to 12.1%. The use of other treatment methods–including quitlines, counseling and support groups, and internet-based resources–also increased.
Table 1:
Smoking cessation treatments used in past-year smokers who quitted smoking in the past year in the Current Population Survey—Tobacco Supplements 2003 and 2010–2011.
| Methods | 2003 surveys | 2010–2011 surveys | Comparison | |||
|---|---|---|---|---|---|---|
| N | % | N | % | OR | 95% CI | |
| Nicotine replacement therapy | ||||||
| Nicotine gum/lozenge | 185 | 6.8 | 193 | 8.5 | 1.26 | 1.07–1.50 |
| Nicotine patch | 388 | 14.6 | 319 | 13.8 | 0.93 | 0.81–1.07 |
| Nicotine inhaler/nasal spray | 39 | 1.7 | 24 | 0.9 | 0.54 | 0.33–0.87 |
| Any replacement therapy | 519 | 19.5 | 447 | 19.3 | 0.98 | 0.87–1.11 |
| Prescription medications | ||||||
| Zyban, buproprion, or Wellbutrin | 215 | 7.5 | 72 | 2.9 | 0.37 | 0.29–0.48 |
| Chantix or varenicline | 0a | 0.0a | 248 | 10.2 | --a | --a |
| Any prescription medications | 215 | 7.5 | 292 | 12.1 | 1.54 | 1.45–1.63 |
| Other treatments | ||||||
| Telephone help line or quit line | 31 | 0.9 | 71 | 2.4 | 2.76 | 2.02–3.77 |
| Stop smoking clinic, class, or support group, one-on-one counseling | 90 | 2.8 | 103 | 4.0 | 1.43 | 1.15–1.78 |
| Acupuncture/hypnosis | 55 | 1.8 | 36 | 1.7 | 0.97 | 0.68–1.38 |
| The Internet | 28 | 1.1 | 42 | 1.9 | 1.79 | 1.15–2.78 |
Questions about Chantix/Varenicline were asked only in the 2010–2011 surveys.
Both clean indoor air laws and cigarette excise taxes were associated with higher odds of recent smoking cessation. However, clean indoor air laws were associated with recent smoking cessation both in 2003 and 2010–2011; whereas, taxes were associated with recent smoking cessation only in 2010–2011. In logistic regression analyses, adjusted for participant sociodemographic characteristics, each 1-point increase in the score for clean indoor air laws was associated with 5% and 8% higher odds of recent smoking cessation in 2003 and 2010–2011, respectively. Similarly, each $1.00 higher excise tax was associated with 10% higher odds of recent smoking cessation in 2010–2011 (Table 2).
Table 2:
Association of clean indoor air laws and excise taxes (combined federal, state and local) with recent smoking cessation in participants of the Current Population Survey—Tobacco Supplements 2003 and 2010–2011.
| Clean indoor air laws | Cigarette excise taxes | |||||||
|---|---|---|---|---|---|---|---|---|
| 2003 surveys | 2010–2011 surveys | 2003 | surveys | 2010–2011 surveys | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Clean indoor air laws | 1.05 | 1.01–1.09 | 1.08 | 1.04–1.12 | -- | -- | -- | -- |
| Excise taxes (in $’s) | -- | -- | -- | -- | 1.01 | 0.96–1.07 | 1.11 | 1.05–1.17 |
| Sex | ||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 1.17 | 1.11–1.23 | 1.04 | 0.95–1.14 | 1.17 | 1.11–1.23 | 1.04 | 0.95–1.14 |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Non-Hispanic black | 0.85 | 0.75–0.96 | 0.95 | 0.79–1.14 | 0.85 | 0.75–0.96 | 0.95 | 0.79–1.14 |
| Hispanic | 1.22 | 1.09–1.36 | 1.12 | 0.94–1.34 | 1.23 | 1.10–1.38 | 1.11 | 0.93–1.33 |
| Other | 1.00 | 0.89–1.12 | 0.91 | 0.72–1.14 | 1.01 | 0.90–1.14 | 0.91 | 0.72–1.15 |
| Place of birth | ||||||||
| Outside of the US | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| US | 1.10 | 1.00–1.22 | 0.93 | 0.78–1.13 | 1.10 | 0.99–1.21 | 0.93 | 0.77–1.16 |
| Age, years | ||||||||
| 18–29 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 30–49 | 0.61 | 0.56–0.65 | 0.61 | 0.54–0.68 | 0.61 | 0.56–0.65 | 0.61 | 0.54–0.68 |
| 50–64 | 0.57 | 0.53–0.63 | 0.51 | 0.44–0.59 | 0.57 | 0.53–0.63 | 0.51 | 0.44–0.59 |
| 65+ | 0.80 | 0.71–0.91 | 0.59 | 0.45–0.68 | 0.81 | 0.72–0.91 | 0.55 | 0.45–0.68 |
| Education | ||||||||
| <High school diploma | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| High school diploma or GED | 1.20 | 1.17–1.30 | 1.47 | 1.27–1.70 | 1.21 | 1.18–1.30 | 1.47 | 1.27–1.71 |
| Some college | 1.54 | 1.41–1.68 | 1.81 | 1.57–2.08 | 1.55 | 1.42–1.69 | 1.82 | 1.58–2.09 |
| Bachelor’s degree or higher | 1.97 | 1.80–2.15 | 2.63 | 2.22–3.13 | 1.98 | 1.81–2.16 | 2.66 | 2.24–3.15 |
| Employment status | ||||||||
| Employed | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Unemployed | 0.75 | 0.66–0.85 | 0.97 | 0.83–1.13 | 0.75 | 0.66–0.86 | 0.97 | 0.83–1.13 |
| Not in labor force | 0.95 | 0.89–1.02 | 1.21 | 1.09–1.34 | 0.95 | 0.89–1.02 | 1.21 | 1.09–1.34 |
| Marital status | ||||||||
| Married or living as married | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Divorced/separated | 0.70 | 0.61–0.81 | 1.01 | 0.81–1.25 | 0.70 | 0.61–0.81 | 1.01 | 0.81–1.25 |
| Widowed | 0.69 | 0.65–0.75 | 0.86 | 0.76–0.97 | 0.70 | 0.65–0.75 | 0.86 | 0.76–0.96 |
| Never married | 0.84 | 0.78–0.90 | 0.80 | 0.71–0.91 | 0.84 | 0.78–0.90 | 0.80 | 0.71–0.90 |
| State spending on tobacco prevention compared to CDC recommended expenditurea | 1.16 | 1.08–1.25 | 1.17 | 0.88–1.54 | 1.18 | 1.09–1.28 | 1.25 | 0.95–1.63 |
Data from Tobacco-Free Kids organization (https://www.tobaccofreekids.org/assets/factsheets/0209.pdf).
In 2003, women had significantly higher odds of recent smoking cessation compared to men and non-Hispanic Blacks had significantly lower odds compared to non-Hispanic Whites. Compared to the 18–29 years age group, older age groups had significantly lower odds of recent smoking cessation at both time points. Participants with high school diploma education or more had higher odds of smoking cessation in both periods. In 2003, participants who were unemployed or not in the labor force had significantly lower odds of recent smoking cessation compared to those who were employed.
Compared to married participants, those who were widowed or never married had significantly lower odds of recent smoking cessation at both time points, whereas divorced or separated participants had significantly lower odds only in 2003. Higher state spending on tobacco prevention compared to CDC recommended expenditure was associated with higher odds of recent smoking cessation only in 2003 (Table 2).
The mediation analyses were limited to examining the mediating role of smoking cessation treatments in the association of clean indoor air laws with recent smoking cessation in 2003 and the association of these laws and excise taxes with recent smoking cessation in 2010–2011. Because taxes were not associated with recent smoking cessation in 2003, mediation analyses were not conducted for this year.
In the SEM mediation analyses, the use of prescription medications and NRT mediated the association of clean indoor laws with recent smoking cessation in 2003 (Figure 1) as indicated by significant odds ratios for the association of the treatments with clean indoor air laws (OR=1.08, 95% confidence interval=1.02–1.13 for prescription medications and OR=1.11, 1.07–1.15 for NRT) and significant association of recent smoking cessation with these treatments (OR=1.58, 1.41–1.77 for prescription medications and OR=2.19, 2.05–2.35 for NRT). Furthermore, use of prescription medications, NRT and counseling and groups mediated the association of taxes with recent smoking cessation in 2010–2011 (Figure 2) as indicated by significant coefficients for the association of these treatments with taxes (OR=1.23, 1.15–1.31 for prescription medications; OR=1.22, 1.15–1.28 for NRT; OR=1.19, 1.05–1.34 for counseling and groups) and significant association of recent smoking cessation with these treatments (OR=1.90, 1.64–2.20 for prescription medications, OR=1.89, 1.66–2.16 for NRT and OR=1.61, 1.25–2.09 for counseling and groups). Similarly, the use of prescription medications and NRT mediated the association of clean indoor air laws with recent smoking cessation in 2010–2011 as indicated by significant association of these treatments with the laws (OR=1.08, 1.03–1.14 for prescription medications and OR=1.09, 1.05–1.13 for NRT) and the significant association of these treatments with recent smoking cessation (OR=2.05, 1.76–2.34 and OR=1.93, 1.70–2.20) (Figure 3). Direct effects of clean indoor air policies and excise taxes were significant in all three models (Figures 1–3).
Figure 1:

Structural equation model for the mediated association of clean indoor air laws (combined workplace, bar and restaurant laws)a with recent smoking cessation in participants of the Current Population Survey—Tobacco Supplements, 2003. Regression coefficients were exponentiated to compute odds ratios for the association of the continuous independent variable (summary index for clean indoor air laws) with binary mediators and outcome.
Footnote: aBecause state and local laws affecting workplaces, bars, and restaurants are strongly correlated, an average clean indoor air law index was computed by averaging over the three sets of laws.
Figure 2:
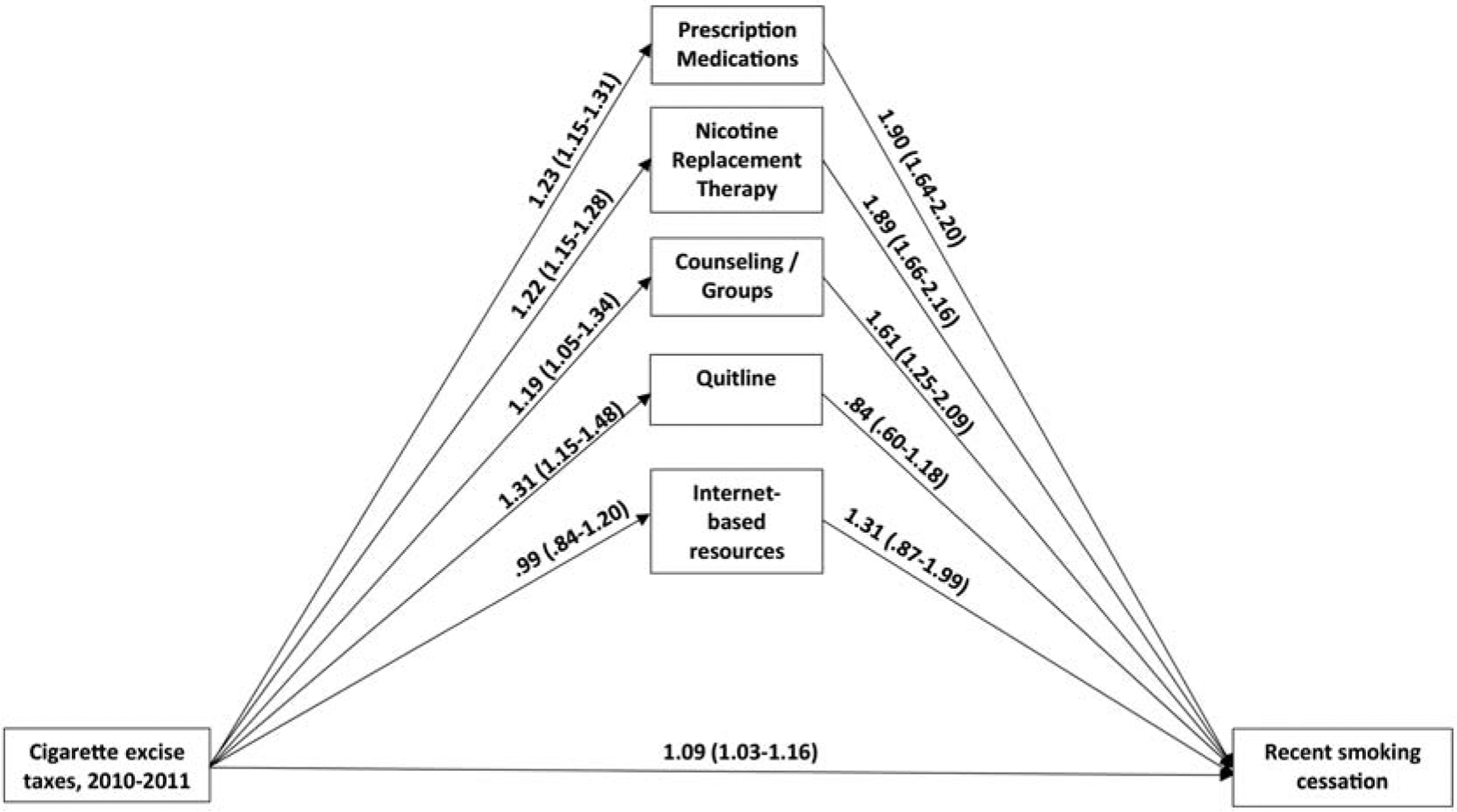
Structural equation model for the mediated association of excise taxes (total federal, state and local taxes in $’s) with recent smoking cessation in participants of the Current Population Survey—Tobacco Supplements 2010–2011. Regression coefficients were exponentiated to compute odds ratios for the association of the continuous independent variable (excise taxes in $ units) with binary mediators and outcome.
Footnote: aBecause state and local laws affecting workplaces, bars, and restaurants are strongly correlated, an average clean indoor air law index was computed by averaging over the three sets of laws.
Figure 3:
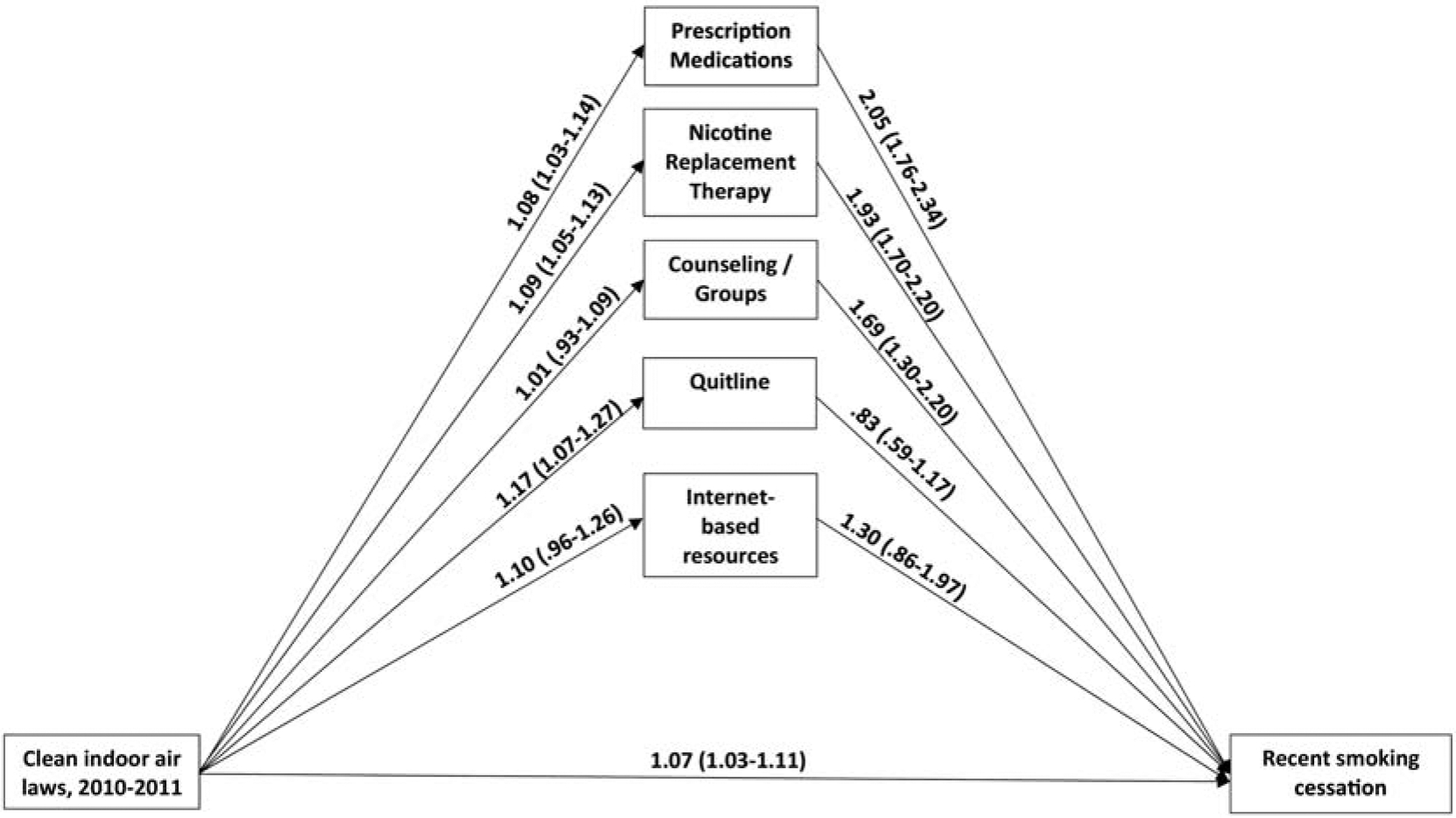
Structural equation model for the mediated association of clean indoor air laws (combined workplace, bar and restaurant laws)a with recent smoking cessation in participants of the Current Population Survey—Tobacco Supplements, 2010–2011. Regression coefficients were exponentiated to compute odds ratios for the association of the continuous independent variable (summary index for clean indoor air laws) with binary mediators and outcome.
Footnote: aBecause state and local laws affecting workplaces, bars, and restaurants are strongly correlated, an average clean indoor air law index was computed by averaging over the three sets of laws.
These results were broadly supported by the potential outcomes analyses (data not shown). Similar to the SEM mediation analyses, “marginal total effects”, “natural direct effects” and “natural indirect effects” were statistically significant in potential outcomes mediation models for the association of clean indoor air laws with recent smoking cessation in 2003 (marginal total effect OR=1.07, 1.02–1.15; natural direct effect OR=1.04, 1.004–1.11; natural indirect effect OR=1.03, 1.02–1.04; percent effect mediated=38.5%), association of clean indoor air laws with recent smoking cessation in 2010–2011 (marginal total effect OR=1.15, 1.07–1.22; natural direct effect OR=1.10, 1.01–1.18; natural indirect effect OR=1.04, 1.03–1.06; percent effect mediated=29.0%), and the association of cigarette excise taxes with recent smoking cessation in 2010–2011 (marginal total effect OR=1.14, 1.06–1.24; natural direct effect OR=1.09, 1.0003–1.18; natural indirect effect OR=1.05, 1.04–1.06; percent effect mediated=29.6%). The marginal total effect in the potential outcomes mediation model for the association of cigarette excise taxes and recent smoking cessation for 2003 was not statistically significant (data not shown).
DISCUSSION
There were two main findings in this study. First, clean indoor air laws and excise taxes might have had different impacts on smoking cessation behavior of cigarette smokers in the 2003 period compared to the 2010–2011 period. While only clean indoor air laws were associated with recent smoking cessation in 2003, these laws and taxes were both associated with recent smoking cessation in 2010–2011. Second, smoking cessation treatments mediated some of the association of these policies with recent smoking cessation.
The variation in our findings regarding tobacco control policy associations between 2003 and 2010–2011 may be due to changes in the population of smokers. There is some evidence that the rate of smoking declined more sharply between 1990 and 2016 in higher socio-economic population groups.33 As a result, the smoking behavior of current smokers in more recent years might have been more sensitive to cigarette prices which are affected by taxes.34 In support of this view, while unemployed participants were less likely than the employed to stop smoking in 2003, there were as likely to stop in 2010–2011. The role of excise taxes in more recent years highlights their importance in motivating smoking cessation, which is consistent with findings in the existing literature.21,22 Unfortunately, states and localities currently do not take full advantage of this policy tool. As recently as June 2019, state excise taxes ranged from a low of $0.17/pack in Missouri to a high of $4.50/pack in DC.35 Similarly, clean indoor air laws vary significantly across states and localities. Only half of the U.S. population lives in a jurisdiction with clean indoor air laws for workplaces, bars, and restaurants,36 and this coverage varies among racial and ethnic groups due to significant differences in states’ racial/ethnic composition.37 As of 2015, comprehensive clean indoor air laws had been implemented in only 27 states.38
The policies we examined are often cost-neutral or, in the case of cigarette taxes, revenue generating. Nevertheless, states have been slow in adopting them. Based on data from the American Lung Association,39 many states have not increased cigarette taxes over the past decade or only increased taxes by a small amount. Similarly, based on the American Lung Association grading system, 10 states received a grade of F for clean indoor air laws in 2017, indicating very weak or no laws.
Both clean indoor air laws and tobacco excise taxes have been shown to impact smokers’ attitudes, intentions, and behaviors.16,21,22 Our findings expand the existing literature by investigating smoking cessation strategy use as potential mediators between tobacco control legislation and smoking cessation. We demonstrate that clean indoor air laws and tobacco excise taxes may impact the uptake of evidence-based smoking cessation strategies, including the use of NRT and prescription medications.40 These two forms of treatment were significantly associated with laws in both periods, with excise taxes in 2010–2011 and with recent smoking cessation in the SEM analyses. Taken together, our findings suggest that tobacco control policies may not only impact smokers’ attitudes, norms, and intentions towards quitting, and quit attempts, but may also motivate them to use evidence-based strategies when they try to quit smoking.
The mediating role of smoking cessation of smoking cessation treatments highlights the potential effect of policies aimed at making these treatments more widely available. Despite availability of a range of pharmacologic and behavioral treatments in the US, only a small proportion of smokers use them.41 Lack of insurance coverage has traditionally been a major barrier to some of these treatments, but the Affordable Care Act (ACA) provided new opportunities to overcome these barriers.42 Nevertheless, increased insurance coverage may not be sufficient to overcome the attitudinal and social barriers to quitting that many current smokers face.43,44 The findings of this study suggest that the effect of improved access to cessation services through expanded health insurance coverage may be enhanced through the synergistic effects of clean indoor air laws and especially increased excise taxes.
Our study has several limitations. First, many individuals who reported having stopped smoking in recent days or weeks may relapse and start smoking again if followed over a longer time. Using a longer duration of smoking cessation to define quitting would identify many of these longer-term quitters. However, such a definition would miss those long-term quitters who have recently stopped smoking and who will continue to remain non-smokers if followed up. As a result, we chose to focus our analyses on “recent smoking cessation.” The results may be different for long-term cessation. Second, the mediation analysis has a causal interpretation only to the extent that its strong assumptions are met and most importantly the assumption of sequential ignorability is met. While we were able to adjust for many important individual and contextual variables, we were unable to adjust for some other important variables such as income or insurance status because these data are only collected for a subset of those who complete the CPS-TUS survey. Third, there have been some changes in health insurance policy and, possibly in access to smoking cessation treatments since 2011. However, at the time of this writing, CPS-TUS 2010–2011 was the most recent wave of the survey with data on smoking cessation treatments. Fourth, it may take months or even years for changes in taxes and clean indoor air laws to have their full effect,13 yet our data were limited to past year smoking behavior and we could not track the association of policies with smoking cessation over longer periods of time. Fifth, over the years, a number of public and private organizations have mounted various initiatives to combat smoking.45 These policies are likely impacted by political and economic factors, and it is often not feasible to separate the effects of these policies from the effects of clean indoor air laws and excise taxes.24 Relatedly, a number of other behaviors or attitudes may act as mediators between antismoking policies and recent smoking cessation. These other factors were subsumed in the significant “direct effects” in our mediation analyses. Further studies need to explore those other potential mediators. Sixth, county level data were missing for a majority of participants, limiting the study’s ability to fully capture heterogeneity of effects at this level. In addition, CPS-TUS geographic codes for cities often combined neighboring cities, precluding examining of policies at city level. Finally, due to the strong correlation between clean indoor air laws and cigarette taxes, we were not able to assess their joint effects in regression and mediation models.
CONCLUSION
The findings from this study provide evidence of an association of state and local tobacco control policies with smoking behavior in current smokers and the mediating role of cessation treatments. Wider adoption of these policies across state and local governments, along with greater availability of pharmacological and non-pharmacological smoking cessation treatments as envisioned in the ACA, would likely have a significant impact on smoking cessation.
Highlights.
Clean indoor air laws and excise taxes were associated with quitting smoking.
Excise taxes have gained a larger role in smoking cessation in recent years.
Use of smoking cessation treatments mediated these associations.
ACKNOWLEDGMENTS
The authors wish to thank Dr. Lainie Rutkow for her contribution to earlier versions of this paper.
Funding: This work was supported by the National Institutes of Health (R01DA042738). Ms. Riehm was supported by the National Institute of Mental Health (NIMH) Psychiatric Epidemiology Training Program (5T32MH014592-39) and by a Doctoral Foreign Study Award from the Canadian Institutes of Health Research.
Abbreviations:
- CPS-TUS
Current Population Survey-Tobacco Use Supplement
- ANRF
American Nonsmokers’ Rights Foundation
- FIPS
Federal Information Processing Standard
- OR
odds ratio
- aOR
adjusted odds ratio
- IQR
interquartile range
- NRT
nicotine replacement treatment
- ACA
Affordable Care Act
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
Dr. Alexander is past Chair of FDA’s Peripheral and Central Nervous System Advisory Committee; has served as a paid advisor to IQVIA; is a Principal and holds equity in Monument Analytics, a health care consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation; and is a member of OptumRx’s National P&T Committee. This arrangement has been reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. All other authors have no disclosures to report.
REFERENCES
- 1.Jamal A, Phillips E, Gentzke AS, et al. Current cigarette smoking among adults— United States, 2016. Morbidity and Mortality Weekly Report. 2018;67(2):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holford TR, Levy DT, McKay LA, et al. Patterns of birth cohort–specific smoking histories, 1965–2009. American Journal of Preventive Medicine. 2014;46(2):e31–e37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavinghouze SR, Malarcher A, Jama A, et al. Trends in quit attempts among adult cigarette smokers—United States, 2001–2013. Morbidity and Mortality Weekly Report. 2015;64(40):1129–1135. [DOI] [PubMed] [Google Scholar]
- 4.Méndez D, Tam J, Giovino GA, et al. Has smoking cessation increased? An examination of the US adult smoking cessation rate 1990–2014. Nicotine & Tobacco Research. 2016;19(12):1418–1424. [DOI] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. The Health Benefits of Smoking Cessation. U.S. Department of Health and Human Services. Public Health Service. Centers for Disease Control. Center for Chronic Disease Prevention and Health Promotion. Office on Smoking and Health; DHHS Publication No. (CDC) 90–8416. 1990. [Google Scholar]
- 6.Donald H Taylor J, Hasselblad V, Henley SJ, et al. Benefits of Smoking Cessation for Longevity. American Journal of Public Health. 2002;92(6):990–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babb S Quitting smoking among adults—United States, 2000–2015. Morbidity and Mortality Weekly Report. 2017;65. [DOI] [PubMed] [Google Scholar]
- 8.Soulakova JN, Crockett LJ. Unassisted quitting and smoking cessation methods used in the United States: analyses of 2010–2011 Tobacco Use Supplement to the Current Population Survey Data. Nicotine and Tobacco Research. 2016;20(1):30–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leischow SJ. Increasing Smoking Cessation in the United States: Expanding the Availability of Over-the-Counter Medications. JAMA. 2019;321(6):541–2. [DOI] [PubMed] [Google Scholar]
- 10.Hoffman SJ, Tan C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health. 2015;15(1):744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. 2008;4(4). [DOI] [PubMed] [Google Scholar]
- 12.Song AV, Dutra LM, Neilands TB, et al. Association of smoke-free laws with lower percentages of new and current smokers among adolescents and young adults: An 11-year longitudinal study. JAMA Pediatrics. 2015;169(9):e152285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hahn EJ, Rayens MK, Langley RE, et al. Time since smoke-free law and smoking cessation behaviors. Nicotine & Tobacco Research. 2009;11(8):1011–1015. [DOI] [PubMed] [Google Scholar]
- 14.Becker CM, Lee JGL, Hudson S, et al. A 14-year longitudinal study of the impact of clean indoor air legislation on state smoking prevalence, USA, 1997–2010. Preventive Medicine. 2017;99:63–66. [DOI] [PubMed] [Google Scholar]
- 15.Mayne SL, Auchincloss AH, Tabb LP, et al. Associations of Bar and Restaurant Smoking Bans With Smoking Behavior in the CARDIA Study: A 25-Year Study. American Journal of Epidemiology. 2018;187(6):1250–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nagelhout GE, de Vries H, Fong GT, et al. Pathways of Change Explaining the Effect of Smoke-Free Legislation on Smoking Cessation in the Netherlands. An Application of the International Tobacco Control Conceptual Model. Nicotine & Tobacco Research. 2012;14(12):1474–1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chaloupka FJ, Powell LM, Warner KE. The Use of Excise Taxes to Reduce Tobacco, Alcohol, and Sugary Beverage Consumption. Annual Review of Public Health. 2019;40(1):187–201. [DOI] [PubMed] [Google Scholar]
- 18.Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tobacco Control. 2012;21(2):172–180. [DOI] [PubMed] [Google Scholar]
- 19.Shmulewitz D, Stohl M, Keyes KM, et al. Effects of State-Level Tobacco Environment on Cigarette Smoking are Stronger Among Those With Individual-Level Risk Factors. Nicotine & Tobacco Research. 2016;18(10):2020–2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Franz G Price effects on the smoking behaviour of adult age groups. Public Health. 2008;122(12):1343–1348. [DOI] [PubMed] [Google Scholar]
- 21.Ross H, Blecher E, Yan L, et al. Predictors of what smokers say they will do in response to future price increases. Findings from the International Tobacco Control (ITC) Four Country Survey. Nicotine & Tobacco Research. 2011;13(6):419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi K, Boyle RG. Minnesota smokers’ perceived helpfulness of 2009 federal tobacco tax increase in assisting smoking cessation: a prospective cohort study. BMC Public Health. 2013;13(1):965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McMenamin SB, Halpin HA, Shade SB. Trends in employer-sponsored health insurance coverage for tobacco-dependence treatments. American Journal of Preventive Medicine. 2008;35(4):321–326. [DOI] [PubMed] [Google Scholar]
- 24.Dahne J, Wahlquist AE, Garrett-Mayer E, et al. State tobacco policies as predictors of evidence-based cessation method usage: results from a large, nationally representative dataset. Nicotine and Tobacco Research. 2017;20(11):1336–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edwards SA, Bondy SJ, Callaghan RC, et al. Prevalence of unassisted quit attempts in population-based studies: a systematic review of the literature. Addictive Behaviors. 2014;39(3):512–519. [DOI] [PubMed] [Google Scholar]
- 26.Mojtabai R, Riehm KE, Cohen JE, et al. Clean indoor air laws, cigarette excise taxes, and smoking: Results from the current population survey-tobacco use supplement, 2003–2011. Preventive Medicine. 2019;126:105744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.American Nonsmokers’ Rights Foundation. U.S. Tobacco Control Laws Database©: Research Applications. 2018. Retrieved from https://no-smoke.org/wp-content/uploads/2018/01/USTobaccoControlLawsDatabase-Jan-18-2018.pdf.
- 28.Centers for Disease Control and Prevention. State preemption of local tobacco control policies restricting smoking, advertising, and youth access--United States, 2000–2010. Morbidity and Mortality Weekly Report. 2011;60(33):1124. [PubMed] [Google Scholar]
- 29.VanderWeele TJ. Mediation analysis: a practitioner’s guide. Annual Review of Public Health. 2016;37:17–32. [DOI] [PubMed] [Google Scholar]
- 30.Wang W, Nelson S, Albert JM. Estimation of causal mediation effects for a dichotomous outcome in multiple-mediator models using the mediation formula. Statistics in Medicine. 2013;32(24):4211–4228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Linden A, Karlson KB. Using mediation analysis to identify causal mechanisms in disease management interventions. Health Services and Outcomes Research Methodology. 2013;13(2–4):86–108. [Google Scholar]
- 32.Valeri L, VanderWeele TJ. Mediation analysis allowing for exposure–mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychological Methods. 2013;18(2):137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Drope J, Liber AC, Cahn Z, et al. Who’s still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA: A Cancer Journal for Clinicians. 2018;68(2):106–115. [DOI] [PubMed] [Google Scholar]
- 34.Hill S, Amos A, Clifford D, et al. Impact of tobacco control interventions on socioeconomic inequalities in smoking: review of the evidence. Tobacco Control. 2014;23(e2):e89. [DOI] [PubMed] [Google Scholar]
- 35.Campaign for Tobacco-Free Kids. State Cigarette Excise Tax Rates & Rankings. 2019. Retrieved from https://www.tobaccofreekids.org/assets/factsheets/0097.pdf
- 36.American Nonsmokers’ Rights Foundation. Summary of 100% Smokefree State Laws and Populations Protected by 100% U.S. Smokefree Laws. 2014. Retrieved from https://no-smoke.org/wp-content/uploads/pdf/SummaryUSPopList.pdf
- 37.Gonzalez M, Sanders-Jackson A, Song AV, et al. Strong smoke-free law coverage in the United States by race/ethnicity: 2000–2009. American Journal of Public Health. 2013;103(5):e62–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tynan MA, Holmes CB, Promoff G, et al. State and local comprehensive smoke-free laws for worksites, restaurants, and bars—United States, 2015. Morbidity and Mortality Weekly Report. 2016;65(24):623–626. [DOI] [PubMed] [Google Scholar]
- 39.American Lung Association. Smokefree Air Laws. Retrieved from http://www.lung.org/our-initiatives/tobacco/reports-resources/sotc/state-grades/state-rankings/smokefree-air-laws.html
- 40.Fiore MC, Jaen CR, Baker TB. Treating Tobacco Use and Dependence: 2008 Update Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. www.surgeongeneral.gov/tobacco/treating_tobacco_use08.pdf. [Google Scholar]
- 41.Watkins SL, Thrul J, Max W, et al. Cold Turkey and Hot Vapes? A National Study of Young Adult Cigarette Cessation Strategies. Nicotine & Tobacco Research. 2018; nty270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McAfee T, Babb S, McNabb S, et al. Helping smokers quit—opportunities created by the Affordable Care Act. New England Journal of Medicine. 2015;372(1):5–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DiGiulio A, Jump Z, Yu A, et al. State Medicaid Coverage for Tobacco Cessation Treatments and Barriers to Accessing Treatments - United States, 2015–2017. Morbidity and Mortality Weekly Report. 2018;67(13):390–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Young-Wolff KC, Klebaner D, Campbell CI, et al. Association of the Affordable Care Act with Smoking and Tobacco Treatment Utilization among Adults Newly Enrolled in Healthcare. Medical Care. 2017;55(5):535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brown HS, Karson S. Cigarette Quitlines, Taxes, And Other Tobacco Control Policies: A State-Level Analysis. Health Economics. 2013;22(6):741–748. [DOI] [PubMed] [Google Scholar]


