Abstract
Background:
Early treatment is key to a successful recovery for ischemic stroke patients. From time of onset, a patient’s chances of permanent disability only increase until they can receive reperfusion intervention.
Objective:
We sought to identify potential delays that occur during evaluation and treatment of patients in a rural regional health system.
Methods:
We conducted a single-center retrospective review of all patients that arrived at our comprehensive stroke center (CSC) between July 2011 and March 2017, and received thrombectomy, with or without prior treatment with intravenous recombinant tissue plasminogen activator (r-tPA).
Results:
154 patients met our criteria for inclusion. Patients were divided into two groups: Direct (patients brought to our CSC from scene) and Transfer (patients taken to an outside hospital then transferred to our CSC). The median time to CSC for Direct patients was 82 (range: 15–863) minutes after onset of symptoms, compared to 237 (range: 98–1215) minutes for the Transfer group. The median time for Transfer patients to reach an outside hospital was 74 (range: 5–840) minutes, with an additional average time of 90 minutes in the outside hospital prior to transferred to our CSC.
Conclusions -
Based on our findings, patients brought directly to our CSC saved a significant amount of time, which may improve functional outcomes. Both groups (Direct and Transfer) spent a similar amount of time between last known normal and emergency medical services (EMS) arrival, highlighting the need for increased awareness among the public to activate the stroke system of care.
Keywords: Stroke, Rural, Regional, Thrombectomy, Transfer, Transport
Introduction
Stroke is a leading cause of long-term disability in adults over 65, and the fifth leading cause of death in the United States, and Kentucky is consistently ranks among the top 12 states in the nation for stroke-related deaths [1–3]. Interventions such as intravenous tissue plasminogen activator (IV r-tPA) and mechanical thrombectomy (MT), when employed rapidly, can minimize the extent of cerebral damage in cases of ischemic strokes. While MT has extended the window for acute revascularization up to 24 hours, outcomes are optimized by expedient clot removal [4]. Given that most of Kentucky is geographically rural, and most patients live outside of one of two counties with Comprehensive Stroke Centers, rapid access may be a challenge.
Previous studies regarding the use of IV r-tPA and urban-rural stroke care disparities have reported significant differences, with frequency of use of IV r-tPA in urban hospitals being four-times that of rural hospitals [5]. As per a 2010 survey conducted in the northwest United States, which is also made up of substantial rural areas, almost half of the rural hospitals lacked appropriate resources to immediately treat patients with stroke [6]. The southeastern United States has a higher rate of stroke mortality than the rest of the country, but the data on rural stroke care in this region is sparse. Thus far, most studies evaluating delays in stroke care have been conducted in mainly urban areas [7–10]. In order to improve stroke care in rural regions, it is important to identify the potential delays in rapid response by EMS and transport of patients to appropriate medical centers with stroke treatment capabilities. The goal of this study was to recognize where potential delays in treatment occur. We quantified the various time intervals involved in transferring Kentucky stroke patients from a first-encounter hospital to the University of Kentucky Medical Center, a Comprehensive Stroke Center (CSC) as certified by the Joint Commission, and compare those intervals to those patients brought directly to UKMC.
Methods
Twenty-two hospitals feed directly into our CSC through an informal network, and five additional hospital send transfer patients intermittently. There are four PSCs in the network, with the closest one 30 miles away, and the farthest one 142 miles away.
Study Sample
After receiving approval from our Institutional Review Board, we retrospectively collected data on patients evaluated for thrombectomy between July 2011 and March 2017 at the UK Chandler Medical Center. We collected demographic data, including age, sex, body mass index, and comorbidities. We also recorded NIH Stroke Scale (NIHSS) scores at our CSC upon admission and discharge, as well whether the patient was transported directly our hospital vs. transfer from an outside hospital (OSH). The date and time of the following events were captured: time of last known normal (LKN), time of arrival at first hospital, time of discharge from first hospital, time of arrival at our institution, time IV r-tPA bolus, and time of recanalization (MT).
Statistical Analysis
Differences between patients who arrived direct to our CSC vs. transfer were assessed with t tests and chi-square tests. Since no times were censored, we used Wilcoxon Rank-Sum tests to evaluate time distributions between the patient groups. Finally, we evaluated factors associated with change in the NIHSS (i.e., between admission and discharge at our institution) using generalized estimating equations (GEE), where the distribution was assumed to be Gaussian. The model contained a dummy indicator for Direct vs. Transfer, dummy indicator for IV r-tPA administration, patient age, patient sex, time to recanalization from LKN, NIHSS at admission, and Case Mix Index (CMI). Patients were assumed to be clustered within Medicaid Managed Care Organization regions (n=6). A p-value of 0.05 was considered significant for all tests.
Results
Of the 198 patients who were admitted to our institution during the study window, 154 patients met criteria, and 44 were excluded from the analysis (See Supplemental Figure). Of the 154 patients, 71 patients were brought directly to our CSC (deemed ‘Direct’), while 83 were first taken to an outside hospital and then transferred to our CSC (deemed ‘Transfer’).
While there were no statistically significant differences between the Direct vs. Transfer patients in terms of demographics (Table 1), there was a non-significant trend toward Transfer patients being younger, with higher rates of hypercholesterolemia and tobacco use.
TABLE 1.
Patient Demographics
| All patients (N=154) |
Direct (n=71) |
Transfer (n=83) |
P value | |
|---|---|---|---|---|
| Age, y | 62.8±14.7 | 64.9±14.7 | 61.0±14.5 | 0.10 |
| Sex (n, %F) | 72 (46.8) | 30 (42.3) | 42 (50.6) | 0.30 |
| Body Mass Index | 29.6±6.8 | 29.3±6.1 | 29.9±6.2 | 0.57 |
| Comorbidities (n, %) | ||||
| High Cholesterol | 71 (46.1) | 27 (38.0) | 44 (53.0) | 0.06 |
| Hypertension | 127 (82.5) | 58 (81.7) | 69 (83.1) | 0.81 |
| Previous Stroke | 26 (16.9) | 13 (18.3) | 13 (15.7) | 0.66 |
| Diabetes | 39 (25.3) | 18 (25.4) | 21 (25.3) | 0.99 |
| Heart Disease | 66 (42.9) | 33 (46.5) | 33 (39.8) | 0.40 |
| Tobacco Use | 58 (37.7) | 22 (31.0) | 36 (43.4) | 0.11 |
Table 2 shows the elements of treatment time and outcomes, and Figure 1A shows the time epochs based on patient type. The average time to thrombectomy since LKN (LKN to Groin Stick) for Direct patients was 330 ± 264 minutes, whereas patients that were transferred to our CSC from a regional outside hospital (OSH) took 486 ± 276 minutes (p = 0.0008). When analyzing the various time intervals, both groups had similar times spent between LKN and arrival to first hospital, as well as similar times of treatment between arrival at our CSC and thrombectomy time. However, patients taken to an OSH, on average, spent an additional 114± 98 minutes in transport and 69 ± 41 minutes in stay at outside hospital. The average total transport (LKN to CSC arrival) time for Direct patients (n = 71) was 161 ±209 minutes, and 356 ± 264 minutes for Transfer patients (n=83); a significant difference of 149 minutes or almost 2.5 hours (p <0.0001). The median time between LKN and arrival for Direct patients was 82 (range: 15 to 863) minutes. While this was slightly longer than the LKN to Hospital 1 time for Transfer patients, the difference was not significant. Of note, patients spent a median 90 (range: 17 to 500) minutes at the initial hospital before being discharged to transfer to our CSC.
TABLE 2.
| All patients (N=154) |
Direct (n=71) |
Transfer (n=83) |
P value | |
|---|---|---|---|---|
| CMI* | 6.3±4.3 | 6.4±4.2 | 6.2±4.4 | 0.73 |
| NIHSS at Admission to CSC | 16.7±6.4 | 17.2±5.4 | 16.4±7.2 | 0.42 |
| NIHSS at Discharge from CSC | 9.8±8.4 | 8.9±7.8 | 10.4±8.8 | 0.31 |
| Change in NIHSS | 5.16 | 5.72 | 4.68 | 0.06 |
| Died in hospital (n, %) | 26 (16.9) | 15 (21.1) | 11 (13.3) | 0.19 |
| Time to CSC, minutes (LKN† to CSC) | 264 ± 258 | 162 ± 210 | 354 ± 264 | <0.0001 |
| t-PA Administered (n, %) | 89 (57.8) | 46 (64.8) | 43 (51.8) | 0.10 |
| Time to t-PA, minutes | 162 ± 144 | 180 ± 192 | 144 ± 72 | 0.20 |
| Time to Thrombectomy, minutes (LKN to Groin Stick) | 414 ± 282 | 330 ± 264 | 486 ± 276 | 0.0008 |
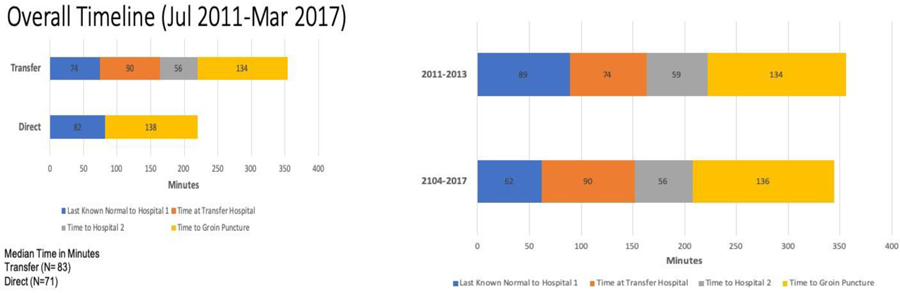
Figure 1.
Timelines showing epochs from Last Known Normal through Thrombectomy. Overall difference between Transferred patients and Direct patients shows a notable amount of time spent in the first hospital prior to transfer (A). Furthermore, while certification of the CSC resulted in reduction in Time to Groin Puncture, time spent at the first hospital for transfer patients increased (B).
Our institution gained CSC status in 2014. Inherent in this achievement is the need to build networks of care, and to perform stroke education with outside surrounding providers, facilities, and the community. Furthermore, with the publication of the thrombectomy trials in 2015, there has been an effort to improve time intervals between LKN and thrombectomy. To evaluate the impact of these issues, we separated the data into 2 subgroups (2011–2013, and 2014–2017; Figure 1B). The median arrival at our CSC to groin puncture time for Direct patients was 138 (range: 65–462) minutes. However, when we divided the groups into 2 subgroups, there is a substantial difference: between 2011 and 2013 the median time to groin puncture after arrival to CSC was 187 (range: 99–462) minutes, this same interval was 125 (range: 65–430) minutes for 2014–2017 (p = 0.0047).
The median LKN to OSH time for Transfer patients between 2011 and 2013 was 89 (range: 29–771) minutes, and the median time for the same segment between 2014 and 2017 decreased to 62 (range: 5–840) minutes. The median time spent in OSH for patients brought between 2011 and 2013 was 74 (range: 18–195) minutes, this interval increased to 90 (range:18–500) minutes for patients brought between 2014 and 2017 (p= 0.015).
The average NIHSS score at admission to our CSC was 16.7 ± 6.4, and the average discharge score was 9.8 ± 8.4. When analyzing the change in NIHSS score among Direct versus Transfer patients, Direct patients experienced an improvement of 5.72 whereas Transfer patients experienced an improvement of 4.68 (p=.06). For patients brought directly to our CSC from 2011–2013, the median NIHSS score change was −1 (range: −21 to 14), the same was −7 (range: −28 to 18) for 2014–2017 patients brought directly to CSC. The median change in NIHSS score of patients transferred from OSH was −3 (range: −16 to 14) in 2011–2013 group, whereas the median was −7 (range: −28 to 17) in the same group in 2014–2017 (Table 3). Negative values indicate a decrease in the scores since admission, reflecting symptom improvement in patients.
TABLE 3.
| 2011–2013 (N=50) | 2014–2017 (N=104) | |||||
|---|---|---|---|---|---|---|
| Overall (N=50) |
Direct (n=26) |
Transfer (n=24) |
Overall (N=104) |
Direct (n=45) |
Transfer (n=59) |
|
| Median NIHSS Admission (Range) | 17 (0–34) | 18 (7–26) | 17 (0–34) | 16 (2–31) | 17 (3–29) | 16 (2–31) |
| Median NIHSS Discharge (Range) | 13 (1–30) | 13 (1–25) | 14 (1–30) | 5 (0–38) | 4 (0–28) | 7 (0–38) |
Finally, to evaluate the role of Primary Stroke Centers (PSCs) in our network, we compared the time epochs for patients presenting to PSCs (N=12) as the first hospital versus all other types of hospitals (Acute Stroke Ready Hospitals, non-Joint Commission certified hospitals; N = 71). The mean time from LKN to arrival was 148+/− 218 minutes for PSCs and 177 +/− 216 minuts for non-PSCs (not significant). The time spent at the outside hospital was not significantly different (152+/− 131 minutes for PSCs vs. 108 +/− 91 minutes for non-PSCs). Finally, there was no significant difference in LKN to groin puncture time (522+/−389 minutes for PSCs vs 508+/− 289 minutes for non-PSCs).
Discussion
Kentucky is a mostly rural state. Of the one hundred and twenty counties in Kentucky, eighty-five are considered rural. Interestingly, many of these counties also have a larger population of adults over the age of 65 in comparison to the more urban counties in Kentucky.[11, 12] Considering the large elderly population in rural areas, it is important to identify epidemiologic healthcare disparities. Most studies have focused on general urban-rural healthcare disparities, very few have focused on stroke care. A 2011 study showed that rural populations were less likely to use important stroke interventions, such as advanced imaging and therapy consults, compared to urban population.[13] A 2013 study done in Kentucky to understand the experience of stroke and stroke care in Appalachian Kentucky revealed many of the barriers and hurdles that stroke patients in these rural settings have to face after being discharged from the hospital.[14] The goal of this paper was to identify healthcare access issues in relation to stroke.
In 2014, University of Kentucky Medical Center received the designation of Comprehensive Stroke Center by the Joint Commission. Since then, we have made progress towards improving stroke care protocol and time to thrombectomy for Kentucky residents. For example, when comparing patients brought directly to our CSC between 2011–2013 and 2014–2017, there is significant improvement in the amount of time between arrival at CSC and groin stick. However, we continue to face challenges in two major areas. First, the time between LKN and arrival at first facility remains high. While distance to a stroke center is a factor, recognition and triage in the field is also a concern. In October of 2017, the Kentucky Board of Emergency Medical Services codified a Severity-Based Stroke Triage Algorithm for EMS. This protocol uses pre-hospital clinical scale evaluation, in-field triage, and a number of short questions about time to determine optimal destination for the patient. The overall goal of this set of practice guidelines is to reduce the time between recognition of the stroke and arrival at the first hospital. Another major challenge remains patient population education. Community education is vital here, providing skills in recognition of stroke, as well as emphasizing the use of EMS services.
Since attaining CSC designation, most time intervals of stroke care timeline among our patients have improved. However, a major continuing opportunity is the overall time that it takes transfer patients to reach our CSC. For transfer patients, while the median time from LKN to first hospital decreased from 89 minutes in the 2011–2013 group to 62 minutes in the 2014–2017 group, the time spent at the first hospital increased. Therefore, the amount of time it took patients to arrive at our CSC from LKN remained unchanged. This highlights continued opportunities in collaborative elements to improve the ideal stroke workflow. While great effort has been placed on ‘direct to CT’ protocols, resulting in rapid initial assessment of stroke patients across emergency departments, more emphasis is required on maintaining the immediacy of decision-making and transfer out to CSC when necessary. This time interval is particularly vulnerable to delays, as it depends on protocols for acceptance at the CSC, and upon local-regional EMS resources to transport patients from one hospital to the next. While we cannot know the underlying reason for delay in door-in, door-out for these hospitals, it may reflect a suboptimal situation in which, as referring hospitals have become stroke centers, they are doing more evaluation in their emergency departments (imaging determination, evaluation for IV thrombolysis, etc) prior to initiating transfer. Furthermore, it may also reflect delays in obtaining imaging results.
One might assume that PSC to CSC transfers would lead to shorter time epochs between LKN and thrombectomy. However, our data do not support such a uniform conclusion. The time epochs for transfers from PSCs were not significantly different than for those of non-PSC hospitals. However, these values should be interpreted with caution, as geographic distance from our hospital, distance of the patient origins to the PSCs, as well as systems of evaluation and radiographic turnaround could all affect each PSC and non-PSC hospital system. What is clear from these data are that overall times spent in both PSC and non-PSC hospitals were high. With a mean time of 152+/− 131 minutes spent at PSCs prior to transfer to our CSC, there is a clear need for efficient identification and triage of patients. Door In-Door Out (DIDO) policies play a major role. Furthermore, automated radiographic interpretation through technologies such as RAPID (Golden, CO) and Viz.ai (San Francisco, CA) could have great impact on improving this DIDO efficiency. One current limitation of our hospital system is that none of our referring institutions are owned by or managed by UK Healthcare. As a result, our system reflects one in which the ‘hub’ CSC relies on community relationships with referring ‘spoke’ hospitals rather than systematic protocols that can be adopted across a single hospital network.
Our study has several limitations. First, as a single center retrospective review of data, this does not represent a randomized or controlled study of evaluation. However, the data are reflective of ‘real-world’ experience, and are applicable to other centers that serve primarily rural populations. The analysis does not account for recent changes in indications for thrombectomy such as recent time windows [15, 16], or knowledge/experience of referring providers. For example, as emergency department providers become more knowledgeable about thrombectomy, they may be referring more patients for thrombectomy in longer time windows, who may or may not be good thrombectomy candidates. This is supported by the fact that more patients were referred to our institution in the later years (2014–2017) for thrombectomy, as the randomized clinical trials showed the benefit of the procedure. This could falsely elevate the overall time from LKN at later time points. Therefore, if this has any impact on the data, it only further underscores the need to reduce time intervals once the patient is recognized as a stroke patient. It further highlights the problem of delay in evaluation and transfer out of the transferring hospital and to the CSC. Another limitation was the lack of outpatient outcome data. However, due to a lack of network coordination, this data was not available. We did collect admission and discharge NIHSS scores; discharge NIHSS has been shown to be a strong predictor of long-term outcome [17–19].
Despite these limitations, our findings demonstrate both active improvements in stroke time intervals, while exposing continued opportunities for improvement in a primarily rural stroke network. Our experience provides insight into the realities of time intervals for thrombectomy patients, and highlights the role of improved protocols both within a Comprehensive Stroke Center and among a referring hospital network, particularly the importance of door-in-to-door-out times from referring hospitals.
Supplementary Material
Acknowledgments
Funding Statement
This project was supported by the National Center for Advancing Translational Sciences: UL1TR000117/UL1TR001998 and UK Healthcare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Data Sharing Statement – Authors are willing to share data from the study with permission from the institutional IRB upon request to the Corresponding Author.
Competing Interests Statement
None of the authors have any competing interests.
Potentially Relevant Conflicts of Interest
Dr. Fraser is an equity interest holder for Fawkes Biotechnology, LLC, and for Cerelux, LLC. He is a consultant for Stream Biomedical, Penumbra and Medtronic Neurovascular.
References
- 1.Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association, in Circulation. 2016, American Heart Association; p. e38–360. [DOI] [PubMed] [Google Scholar]
- 2.Benjamin EJ, et al. , Heart Disease and Stroke Statistics—2017 Update: A Report From the American Heart Association. Circulation, 2017. [DOI] [PMC free article] [PubMed]
- 3.National Center for Health Statistics. Stats of the State of Kentucky. April 11 2018; Available from: https://www.cdc.gov/nchs/pressroom/states/kentucky/kentucky.htm.
- 4.Jovin TG, et al. , Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med, 2015. 372(24): p. 2296–306. [DOI] [PubMed] [Google Scholar]
- 5.Gonzales S, et al. , Progressive rural–urban disparity in acute stroke care. Neurology, 2017. 88(5): p. 441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shultis W, et al. , Striking rural-urban disparities observed in acute stroke care capacity and services in the pacific northwest: implications and recommendations. Stroke, 2010. 41(10): p. 2278–82. [DOI] [PubMed] [Google Scholar]
- 7.Fang J, et al. , Time interval between stroke onset and hospital arrival in acute ischemic stroke patients in Shanghai, China. Clin Neurol Neurosurg, 2011. 113(2): p. 85–8. [DOI] [PubMed] [Google Scholar]
- 8.Prabhakaran S, et al. , Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke, 2011. 42(6): p. 1626–30. [DOI] [PubMed] [Google Scholar]
- 9.Morris DL, et al. , Time Delays in Accessing Stroke Care in the Emergency Department. Academic Emergency Medicine, 1999. 6(3): p. 218–223. [DOI] [PubMed] [Google Scholar]
- 10.Kodankandath TV, et al. , Improving Transfer Times for Acute Ischemic Stroke Patients to a Comprehensive Stroke Center. Journal of Stroke and Cerebrovascular Diseases, 2017. 26(1): p. 192–195. [DOI] [PubMed] [Google Scholar]
- 11.Davis AF, Kentucky’s Urban/Rural Landscape: What is driving the differences in wealth across Kentucky.
- 12.United Stated Department of Agriculture Economic Research Service. State Data. 2018. July 17, 2018 [cited 2018 July 26]; Available from: https://data.ers.usda.gov/reports.aspx?StateFIPS=21&StateName=Kentucky&ID=17854.
- 13.Koifman J, et al. , The association between rural residence and stroke care and outcomes. J Neurol Sci, 2016. 363: p. 16–20. [DOI] [PubMed] [Google Scholar]
- 14.Danzl MM, et al. , “Living with a ball and chain”: the experience of stroke for individuals and their caregivers in rural Appalachian Kentucky. J Rural Health, 2013. 29(4): p. 368–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Albers GW, et al. , Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med, 2018. 378(8): p. 708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Desai SM, et al. , Thrombectomy 6–24 hours after stroke in trial ineligible patients. J Neurointerv Surg, 2018. 10(11): p. 1033–1037. [DOI] [PubMed] [Google Scholar]
- 17.Fischer U, et al. , NIHSS score and arteriographic findings in acute ischemic stroke. Stroke, 2005. 36(10): p. 2121–5. [DOI] [PubMed] [Google Scholar]
- 18.Schlegel, et al. , Utility of the NIH Stroke Scale as a Predictor of Hospital Disposition. Stroke, 2002. 34(1): p. 134–137. [DOI] [PubMed] [Google Scholar]
- 19.Weimar C, et al. , Age and National Institutes of Health Stroke Scale Score within 6 hours after onset are accurate predictors of outcome after cerebral ischemia: development and external validation of prognostic models. Stroke, 2004. 35(1): p. 158–62. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.