As of April 27, altogether 629 coronavirus disease 2019 (COVID-19) cases have been diagnosed in Seoul, two of whom have died (fatality rate, 0.32%) since the first COVID-19 patient in Seoul was confirmed on January 24, 2020. There were 65.7 patients and 0.2 deaths per 1 million population, which is an exceptional result compared to that in other major metropolitan cities in the world (e.g., fatality rate of New York is 7.6% and Tokyo is 2.7%).1,2
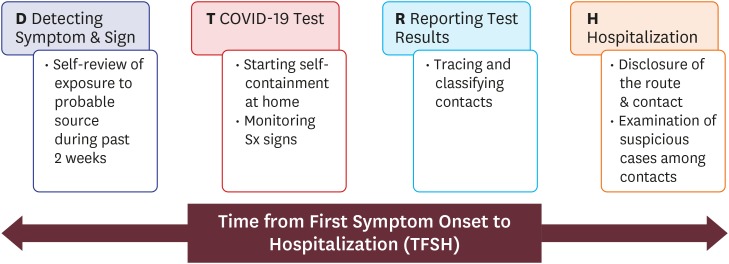
During this period, in total, 111,987 tests were conducted. Some people may judge that these relatively good results have been obtained due to massive, large-scale testing in Seoul.3,4 However, the proportion of screening is only 1.1% of 9.776 million Seoul citizens. We believe that the favorable results were possible because we tried to minimize the time from first symptom onset to hospitalization (TFSH) as well as conduct massive testing. Alternatively, detecting symptom expression (D)—COVID-19 test (T)—reporting examination results (R)—hospitalization (H) was considered one chain reaction. We focused on avoiding bottlenecks at each stage and completing this D-T-R-H process (Fig. 1) at the earliest.
Fig. 1. D-T-R-H process.
COVID-19 = coronavirus disease 2019.
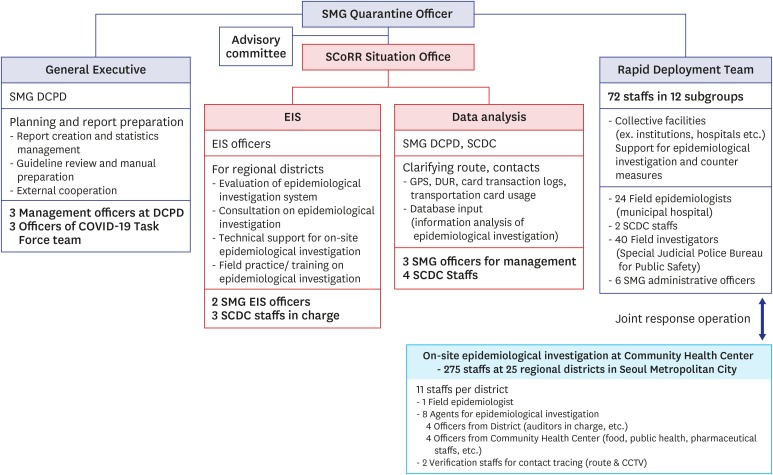
To achieve this goal, the Seoul Metropolitan Government (SMG) launched the SMG COVID-19 Rapid Response Team (SCoRR team) (Fig. 2), which would control the process at the time when there were over 130 confirmed cases. As of April 12, the average TFSH of patients confirmed is 3.93 days (94.3 hours). The TFSH had been 5.37 days (128.9 hours) prior to the set-up of the SCoRR team and decreased to 3.45 days (82.8 hours) after its establishment. The final goal is to achieve and maintain 3.0 days (72 hours). SCoRR Team is under the direction of SMG Quarantine Officer. The SCoRR Team is composed of four groups, approximately 400 staffs as below; General Executive, Epidemic Intelligence Service (EIS), Data Analysis, and Rapid Deployment Team. The General Executive group is composed of the SMG disease control and prevention division (DCPD) and COVID-19 Task Force. It is responsible for establishing plans related to COVID-19 in Seoul, reviewing guidelines, preparing manuals, and external cooperation. The Epidemic Intelligence Service (EIS) group is composed of the EIS officers and staffs at Seoul Center for Infectious Disease Control & Prevention (SCDC). It provides field training, practice and advice on epidemiological consult to regional districts and provides technical support for on-site surveillance. Based on objective data such as Global Positioning System (GPS), Drug Utilization Review (DUR) and credit card transaction logs, the Data Analysis group analyzes and integrates the epidemiological investigation and route information. Lastly, the Rapid Deployment Team consists of the field epidemiologists dispatched by municipal hospitals and the Seoul Center for Infectious Disease Control & Prevention (SCDC), the field investigators of Special Judicial Police Bureau for Public Safety (SMG Judicial Police) and SMG administrative officers. They support epidemiological investigations and operate countermeasures in case of hospital infections or group outbreaks due to unknown source of infection.
Fig. 2. The Organizational Chart of SCoRR Team.
SMG = Seoul Metropolitan Government, SCoRR = Seoul Metropolitan Government COVID-19 Rapid Response, DCPD = disease control & prevention division, COVID-19 = coronavirus disease 2019, EIS = epidemic intelligence service, SCDC = Seoul Center for Infectious Disease Control & Prevention.
Achieving TFSH of 72 hours is a challenging task, since the entire chain reaction must be managed quickly, accurately, and efficiently, including D—T—R—H—classifying and tracing contacts—disclosure of the route—examination of suspicious cases among the traced contacts.
First, the patient should be aware of symptom onset and visit a nearby test site for examination. The most critical and crucial factor is the patient himself, who recognizes early symptoms, suspects COVID-19, and seeks medical help immediately. To facilitate this process, the SMG has been actively encouraging testing for citizens with suspected symptoms; with symptoms, in accordance with KCDC case definition, the diagnostic test is free of cost, and the number of test sites has been increased for greater access. Currently, there are 39 COVID-19 test sites under the direct management of SMG.
Second, it is necessary to shorten the duration from testing to reporting examination results. The fastest testing laboratories may produce accurate results within 6 hours of the arrival of the test samples; SMG's objective is to obtain test results within 24 hours. To prevent delays in reporting test results, laboratory inspection was expanded to certified private agencies, and 74 sites are working laboratories in Seoul. Currently, the daily Korean COVID-19 test capacity reaches 20,000, including Seoul. When suspicious cases are registered and tested, self-isolation is performed until results are obtained. Field epidemiologists begin to trace the contact and path of movement up to 48 hours before onset of symptoms.
Third, when the test result is positive, the confirmed patient is immediately transferred to a medical institution equipped with a negative pressure room to start early treatment. Currently, it takes only 4.3 hours from confirmation to hospitalization. To this end, SMG secured 996 beds of negative pressure treatment with the cooperation of hospitals. In addition, inspections are conducted on the patients' contacts who have been investigated in advance; information about the path and route of each confirmed case, especially during the contagious period is released to encourage citizens who were in the vicinity to undergo testing voluntarily. This information is anonymous and marked only with a patient number to avoid privacy infringement; its purpose is to enhance public understanding of the epidemic and health policies. Currently, the time from testing to reporting is within 24 hours, and it takes only 2 hours from confirmation to hospitalization. The key to reducing TFSH is that individuals are aware of minor symptoms and actively undertake testing.
The SMG's intensive efforts to reduce TFSH have the following potential effects.
First, it minimizes the period of community transmission by promptly identifying the confirmed cases and quarantining them in a hospital. This is a more powerful and effective means of controlling the virus than social distancing and wearing a mask, because the infectious source is separated from the community. The Basic Reproductive Number (R0) value also confirms this effect. The R0 value before the launch of SCoRR was reached to around 2.0, while the recent R0 value fell to under 0.2.
Second, it prevents secondary and tertiary infections in the community and across the country, as those who were contacts of confirmed patients were promptly identified and notified to undertake testing. The proportion of asymptomatic infected patients in Seoul is about 28.3%, which is extremely high; this may be because, before symptoms appeared, i.e., in the pre-communicable stage, citizens were informed that they had contacted a confirmed patient and diagnostic tests were offered earlier in every neighborhood.3
Third, once the cases were confirmed, they were immediately transferred to a specialized hospital to receive appropriate and effective treatment, which prevented patients from deteriorating and spreading the disease to others in an early stage, and reduced the number of critically-ill cases and in-hospital COVID-19 exposure and outbreaks.
Nevertheless, in reality, things are getting a bit more complicated and difficult. This is because more and more people do not know the contact route, and asymptomatic infections from unknown sources lead to silent outbreaks that delay the diagnosis. So, excavation techniques for the possibility of large-scale unidentified contacts and publicity to citizens have been activated. Infectious disease prevention method effective on March 4, 2020, refer to Article 2-15, 2, Definition of Infectious Disease Deliberation, and the 8th edition of the COVID-19 Response Guideline,5 which was recently revised on May 11, highlights the epidemiological characteristics and active contact investigation. Emphasis is placed on strengthening surveillance of contacts during investigations, management in community outbreaks.
In the event of a community outbreak, the quarantine officer conducts an assessment of the epidemic situation at the municipality level; based on the results, he determines the priority (group) of monitoring and sets the monitoring method to conduct enhanced surveillance. For example, in cluster of the Itaewon Club, which is currently being carried out by the SCoRR team, it was recommended that the entire visitors be inspected at the same time due to the occurrence of a large number of confirmed COVID-19 cases in the facility users. Furthermore, another confirmed case existed outside of the known contacts' route, so the application of COVID-19 test was expanded to those simply visited the Itaewon area.
Maybe it's a real community infection from now on. Even though, the most important factor is citizenship. Citizens who would quickly recognize symptoms and risks on their own and apply for tests with minimal contact while adhering to personal hygiene. Although still in progress, the SCoRR Team would learn from the recent outbreaks to challenge the mitigation of COVID-19. It aims to establish hypothetical situations that may occur in communities, schools and institutions, and develop practical responses that are understandable at the eye level of institutional health personnel and the general public, especially students and youth.
The COVID-19 crisis is likely to be prolonged. The healthcare system in many cities has already collapsed. If we had not reduced the TFSH time in Seoul, we would have faced a similar fate. The basic principles of the Korean government's response to COVID-19 are transparency, openness, and democracy; following these principles, we will maintain containment. The best treatment is prevention; the best diagnosis is early diagnosis. Since the first case in January, our SCoRR team is at the vanguard against COVID-19. As watchmen who protect the lives of the citizens of Seoul, we will continue to challenge ourselves until the liberation in this all-out war against COVID-19.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Na BJ, Lee JY.
- Formal analysis: Park Y, Huh IS.
- Investigation: Park Y, Kang CR, Lee JY.
- Methodology: Huh IS.
- Project administration: Na BJ, Kang CR.
- Supervision: Lee JY.
- Validation: Lee J.
- Writing - original draft: Na BJ, Lee J, Lee JY.
- Writing - review & editing: Na BJ, Park Y, Huh IS, Kang CR, Lee J, Lee JY.
References
- 1.NYC. Coronavirus disease 2019 (COVID-19) daily data summary, NYC Department of Health and Mental Hygiene. [Updated 2020]. [Accessed April 26, 2020]. https://www1.nyc.gov/site/doh/covid/covid-19-data.page.
- 2.Latest update on COVID-19 in Tokyo, Tokyo Metropolitan Government. [Updated 2020]. [Accessed April 27, 2020]. https://stopcovid19.metro.tokyo.lg.jp/en/
- 3.Parodi SM, Liu VX. From containment to mitigation of COVID-19 in the US. JAMA. 2020;323(15):1441–1442. doi: 10.1001/jama.2020.3882. [DOI] [PubMed] [Google Scholar]
- 4.Zastrow M. South Korea is reporting intimate details of COVID-19 cases: has it helped? Nature. 2020 doi: 10.1038/d41586-020-00740-y. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 5.Korea Centers for Disease Control and Prevention. The COVID-19 response guidelines for local governments the 8th edition. [Updated 2020]. [Accessed May 11, 2020]. https://www.cdc.go.kr/board/board.es?mid=a20507020000&bid=0019.