Dear Editor,
The unexpectedly rapid spread and fast progression of coronavirus disease 2019 (COVID-19) call for early screening, detection and timely monitoring by imaging modalities. Chest computed tomography (CT) has been dominantly used for COVID-19 diagnosis; however, limitations including radiation exposure, limited mobility and expensive devices may constrain its usefulness, especially during this public health emergency with deficient medical resources.
Lung ultrasonography (LUS) has been increasingly used as a reliable tool for lung disease assessment especially in intensive care medicine [1, 2]. Lesions of COVID-19 pneumonia have shown predominantly peripheral distribution [3], which makes LUS detection more suitable. However, there is no information available to determine the diagnostic value of LUS in COVID-19 in comparison with chest CT.
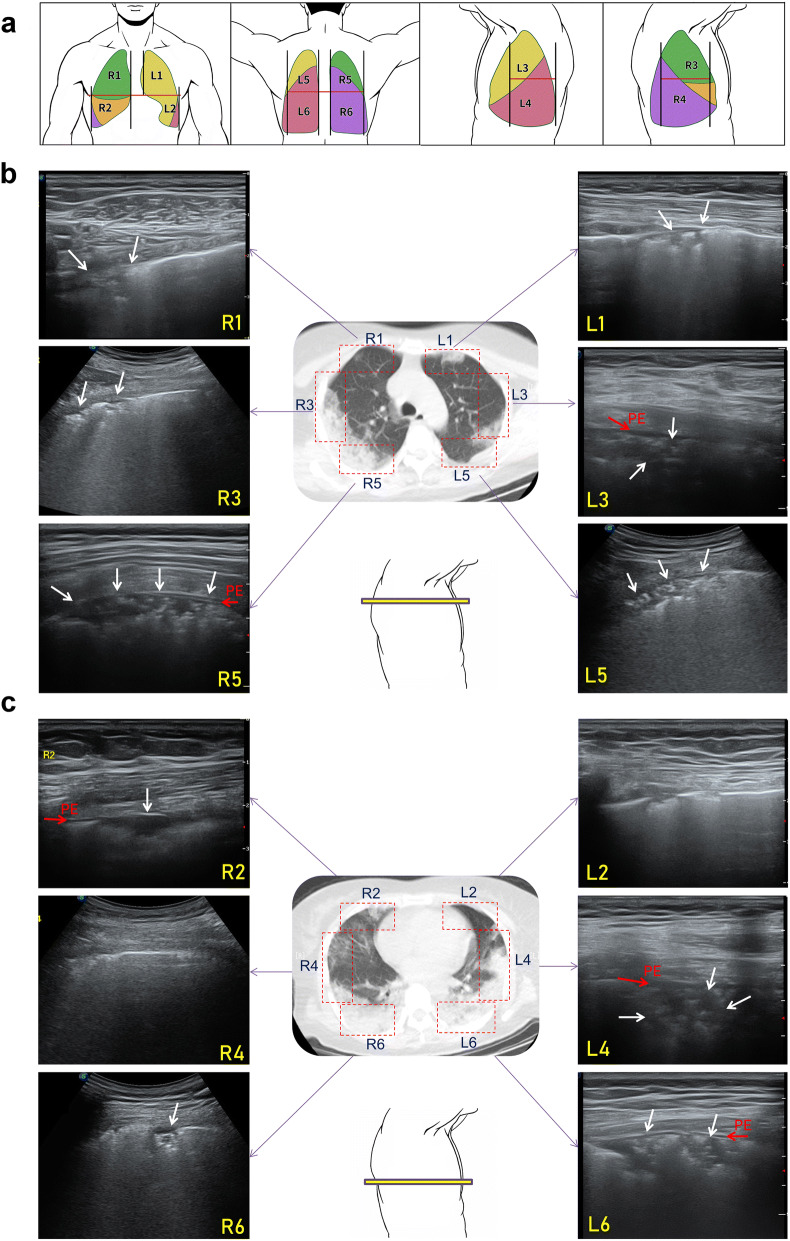
In this retrospective study, patients with laboratory-confirmed COVID-19 pneumonia (clinical classification: common type [4]) from two local government designated medical centers in Xi’an, China, receiving simultaneous LUS and chest CT scans (defined as exam interval ≤ 12 h) by independent investigators were included. To facilitate the comparison between LUS and chest CT, lungs were divided into 12 regions (Fig. 1a), and in each region, LUS features including A-lines, B-lines, consolidation and pleural effusion (PE) and CT features including ground glass opacity (GGO), consolidation and PE were evaluated. The regional alveolar-interstitial pattern (AIP) was defined as multiple B-lines (≥ 3) shown within a region by LUS and as the presence of GGO pattern by CT. Alveolar-interstitial syndrome (AIS) was defined as positive AIP regions (≥ 2) per side + bilateral positivity [5]. The consolidations and PE were diagnosed as previously described [1, 5] (see detailed methods in Supplementary File).
Fig. 1.
LUS and chest CT findings of a 42-year-old female with COVID-19. a Lungs are divided into 12 regions. b The upper lungs, LUS: multiple B-lines, abnormal pleural lines and consolidations (white arrow) are shown in all regions; the air bronchogram can be seen in large consolidations in L3, L5 and R5; extremely little PE (red arrow) can be seen in L3 and R5. Chest CT: patchy GGO with blurred margins in all regions; small patchy consolidations can be seen in R3 and R5; no PE is shown. c The lower lungs, LUS: multiple B-lines and abnormal pleural lines are shown in all regions; consolidations or consolidations with air bronchogram can be seen in R2, L4, R6 and L6; extremely little PE can be seen R2, L4 and L6. Chest CT: patchy GGO with blurred margins in all regions; large patchy consolidations in L4 and L6 and large patchy consolidations with air bronchogram are shown in R6; no PE is shown. R, right; L, left; GGO, ground glass opacity; PE, pleural effusion
We finally included 29 patients (aging 55.2 ± 16.2 years, 18 males) with 45 paired LUS + CT imaging data. In the total 540 lung regions, 340 (63%) positive regions were detected by LUS, including multiple B-lines (324 regions), consolidations (210 regions) and PE (67 hemithoraxes). In contrast, chest CT showed 209 (38.7%) regions with abnormal findings, including GGO (208 regions), consolidations (16 regions) and PE (14 hemithoraxes). LUS was more sensitive than chest CT in the diagnosis of regional AIP (60% vs. 38.5%, P < 0.0001, by McNemar’s test), AIS (93.3% vs. 68.9%, P = 0.001), consolidation (38.9% vs. 3%, P < 0.0001) and PE (74.4% vs. 15.6%, P < 0.0001) (detailed results are in Supplementary File). Both LUS and CT findings showed the lesions of COVID-19 were more likely to occur in the posterior regions of lungs with bilateral distribution. Figure 1 shows the simultaneous LUS and chest CT findings in a representative patient.
Due to its superior capacity in tissue density resolution, LUS is highly sensitive to variations of the pulmonary content balance between air and fluids. COVID-19 pneumonia is characterized by alveolar-interstitial damage with inflammatory exudation and edema, which can be clearly detected by LUS as shown in this study. The findings of this study demonstrate that LUS is more sensitive than chest CT in detecting lesions such as alveolar-interstitial disorders, consolidation and PE in patients with COVID-19 pneumonia. Given the sensitivity, portability and safety, LUS can be a preferable imaging modality for assisting early diagnosis and assessment of COVID-19.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Authors' contribution
Wang Z. contributed to study conception and design. Yang Y. and Huang Y. helped with data collection. Wang Z., Yuan L. and Gao F. contributed to data analysis and interpretation. The first draft was written by Wang Z., and all authors revised the manuscript substantially. All authors read and approved the final manuscript.
Funding
This research was supported by grants from the National Natural Science Foundation of China (No. 81801865 to W.Z. and No. 81671690 to Y.L.) and the Natural Science Foundation Research Program in Shaanxi Province (No. 2019JQ-700 to W.Z., No. 2019JM-191 to Y.Y.).
Compliance with ethical standards
Conflicts of interest
The authors declared no conflict of interest.
Ethical statement
This study was approved by the institutional review boards of the relevant centers. The requirement for informed patient consent was waived for this retrospective study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yong Yang and Yi Huang have contributed equally to this work.
Contributor Information
Lijun Yuan, Email: yuanlj@fmmu.edu.cn.
Zhen Wang, Email: swzwang@126.com.
References
- 1.Xirouchaki N, Magkanas E, Vaporidi K, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensiv Care Med. 2011;37(9):1488–1493. doi: 10.1007/s00134-011-2317-y. [DOI] [PubMed] [Google Scholar]
- 2.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensiv Care Med. 2012;38(4):577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 3.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Health Commission of the People’s Republic of China. Guideline for the Diagnosis and Treatment of COVID-19 (7th edition). http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989/files/ce3e6945832a438eaae415350a8ce964.pdf; http://kjfy.meetingchina.org/msite/news/show/cn/3337.html. Accessed 4 Mar 2020
- 5.Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensiv Care. 2014;4(1):1. doi: 10.1186/2110-5820-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.