Abstract
Oral squamous cell carcinoma (OSCC) is one of the most common type of head and neck squamous cell carcinoma and one of the multifactorial process that consists of most contributing factors such as tobacco smoking, chewing and alcohol consumption that altered the intracellular environment. Recent studies have shown relevance of Toll like receptor (TLR) associated with carcinogenesis. This review aim’s to explore that how TLR associates with progression and suppression of OSCC. This review is a classical review that has confined to articles published in the past 19 years (i.e. 2000-2019) and has summarized the perspective of the authors. 62 articles were reviewed and it was found that progression and suppression of OSCC is associated with different TLRs promoting tumor development and also inhibiting the progression of oral neoplasm. It was found that TLR2, TLR3, TLR4, TLR5, TLR7 and TLR9 are associated with tumor development i.e. in progression of OSCC, where as suppression of OSCC through TLR3 and TLR7. We authors would like to conclude that literature survey has indicated effective TLR’s against OSCC development and can be explored to investigate other TLRs that can be used for therapeutic purposes in near future.
Key words: Oral squamous cell carcinoma, Toll like receptor, tumor development, tumor suppression
Introduction
Oral cancer, accounts for approximately 10% of all head and neck tumor.1 Most common histopathological presentation in squamous cell carcinoma and main causes that induce oral neoplasms are cigarette smoking and consumption of alcohol. Oral squamous cell carcinoma (OSCC) is one of the most frequent types of cancer that is found to be present in developing countries such as India, Vietnam and Brazil. Oral cavity is constantly exposed to numerous and varied microbial species and has been reported that chronic periodontitis, which is an independent risk factor of head and neck cancer.2 New cellular signaling pathways has been extensively investigated in the scientific literature among others is Toll like receptors (TLRs) signaling pathway.3 Innate system employs germ line encoded pattern recognition receptors (PRRs) for the initial detection of microbes that recognize microbe specific molecular signature specifically known as PAMP (Pathogen associated molecular pattern) and DAMP (Damage associated molecular pattern), which is a self-derived molecule from damaged cells. PRRs are found in serums on the cell surface, in endosomes and in the cytoplasm. PRR activates downstream signaling pathways that lead to induction of innate immune response by producing inflammatory cytokines, type 1 interferon (IFN) and other mediators. Mammals have distinct class of PRRs that are broadly classified into three categories such as NOD like receptor (NLR), RIG like receptor (RLR) and Toll Like receptor. TLR are key molecules that discriminate between self and non self antigens. They are membrane spanning proteins that shows a common structural elements in the extracellular regions with repeating segments of 24 to 29 amino acids containing the sequences XLXXLXLXX (X is amino acids and L is leucine). These structural motifs are called leucine rich repeats. TLRs constitutes of exterior and interior domain that activates the signaling pathways. Interior domain (TIR) have the highly conserved domain regions i.e. boxes 1, 2 and 3 that serve as the binding sites for intracellular proteins, participating in the signaling pathway mediated by TLR. Genetic disruption of TLR and adaptor molecule of TLR pathway found to be associated with tumor development and progression in mice.4 TLRs has also been studied in relation to apoptosis but also have pro-apoptotic activity through a range of mechanism.5 With respect to the development of tumor, various TLRs have played different roles in Carcinogenesis. TLR3 and TLR5 has shown protumorigenic with their signaling mediating tumor invasion and metastasis by enhancing cell migration, whereas TLR4 have shown anticancerous effect in some situation.6,7 TLR has shown both suppression and progression in oral squamous cell carcinoma by mediating different signaling pathways.
So, in this review the attention will be focused on progression and suppression of OSCC in associated with TLR (see Figure 1).
Toll like receptors in carcinogenesis
TLR are member of the interleukin -1 receptor super family, that plays an important role in the innate immunity activation and also in the subsequent inflammatory process.8 With that also TLR in the epithelial and inflammatory cells induces persistent innate immunity response, expression of pro-inflammatory cytokines and the generation of ROS take place.9 Infection with bacterium such as Helicobacter pylori, Human papilloma virus (HPV), are an important cause of cancer, causing approximately one in five malignancies worldwide.10 The response of TLRs to these infections is crucial in the evolution of it and possibly in transformation to malignancy which is beyond the scope of review.11 But the modulation of inflammatory processes by TLRs is a key factor in tumor development and progression of tumor cells as well as found to be both tumor promoting anti-tumor response12 Genetic disruptions of TLRs and adaptor molecules of TLRs pathways has also been observed in previous studies that has shown association with tumor development and progression in mice.4 Tumor Cells consists of TLRs which get expressed when damage associated molecular pattern activates and mediate the release of cytokines and chemokines that recruits immune cells leading to the up regulation of NF-kB signaling which continue promoting the tumor survival and progression. 12,13With the apoptotic activity, TLRs have also played an important role in pro-apoptotic activity through a range of mechanisms, so their relation in this concern is also very complex.5 Previous studies also indicate that TLR signaling pathways were not only involved in human immune response but also play a crucial role in initiation and migration of tumor cells.5 Such as TLR- 2 and TLR-9 signaling pathway found to be involved in promoting tumor cell migrations in breast cancer.14 Whereas TLR4 and TLR9 found to be associated in accelerating cell invasion in prostate cancer. 15 TLR2 and TLR 4 signaling was also found to be activated to stimulate tumor cell movement in colon cancer.16 TLR-4 has also shown pro tumorigenic effects with mice deficient in TLR4 at reduced risk of developing gastrointestinal; and hepatocellular cancer.4 Release of HSP from tumor cells can lead to activation of TLR4 on tumor associated macrophages in turn mediating NF-kB activation of tumor cells.17 TLR2 signaling suppression was also found to be in cancer development and assisted in tumor regression. 18 TLR 2 was also found to be reported a tumor promoting role in gastric cancer.19
Above studies has revealed that there is a relationship between TLR signaling and tumor progression that may shed new light to understand the outcome.
Figure 1.
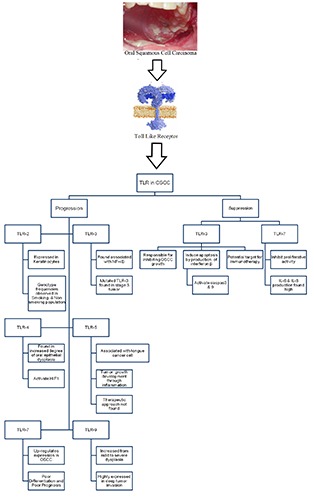
Graphical abstract.
Oral squamous cell carcinoma
Oral squamous cell carcinoma is the most common type of head and neck squamous cell carcinoma, and is among the 10 most prevalent cancer types worldwide.1 Oral cancer is highly prevalent in India, Pakistan, Brazil, France, Afghanistan, Bangladesh, Sri Lanka, Bhutan, Nepal, Iran and Maldives, ranking first or second with respect to different types of cancer occurrence in these countries. 20 Oral cancer occurrence is high in developing countries and is the most common cancer in India.21 Oral carcinogenesis is a highly complex, multifactorial process which consists of some of the most important factor contributing the etiology of oral cancer are tobacco smoking and alcohol consumptions.22 The altered intracellular environment leads to survival and the proliferation of OSCC. Tobacco smoke produces various free radicals, reactive oxygen species (ROS) and reactive nitrogen species (RNS). Oxidative stress is a significant imbalance between the production and removal of reactive oxygen species (ROS), resulting in irreversible oxidative damage to DNA and proteins, interfering with important cellular function.23 Tobacco (either in the form of smoking or chewing) and alcohol consumption are regarded as the main risk factors of oral cancers in Western countries.24 Tobacco quid chewing increases the risk of oral cancers by six fold.25 The human papillomavirus (HPV) infection is also considered as a factor involved in oropharyngeal cancer.26 Symptoms of OSCC are mucositis, dry mouth (xerostomia) and dysphagia, which generally appear during and after cancer treatments.27 The most commonly known symptom in oral cancer patients is xerostomia, in which there is reduction in salivary gland flow resulting in oral fungal infection, swallowing problems, and altered taste.28 The malignant neoplasm occurs at various sites, the most frequent being the lip, lateral edges of the tongue and floor of the oral cavity.29 Adaption of oral cancer-associated behaviors such as tobacco smoking, alcohol drinking, betel quid chewing and using smokeless tobacco, leads to genetic changes in TSGs and proto-oncogenes as well as produces defects in normal cellular processes like the segregation of chromosomes, genomic copy number, loss of heterozygosity, telomere stabilities, regulation of cell-cycle checkpoints and Notch signaling pathways.30
Toll like receptors in progression of oral squamous cell carcinoma
Progression of oral squamous cell carcinoma is associated with the TLR agonists that can promote the survival of malignant cells and also increase their resistance to chemotherapy.31 Previous studies state that endogenous DAMPs were released when tumor cell undergo apoptosis which is been reported by other Authors32 with that also TLR is seen contributing in tumor progression and chemo-resistance by indicating the expression of LRs on tumor cells and tissues.33 After observing Several TLRs are associated with progression of tumor cells that are given below:
TLR 2: This is the most investigated TLR for oral cancer in previous studies. When compared to hyperplastic tissue, TLR2 found to be expressed in oral carcinoma and oral dysplasia.34 Treg expansion and their suppressive capacity were found to be present in TLR 2.35 In the tumor environment positive TLR2 expression is found to be activated against neoplastic, cells as a results of resistance to apoptosis because of poor survival mechanism.34 TLR 2 was also found to be expressed in keratinocytes of OSCC than kerartinocytes in control epithelium. 34 Nuclear TLR2 expression is affiliated with large tumor and occurred more often in primary tumor than metastasis or even in recurrent tumor.36,37 As we know that cigar smoking is one of the main cause for inducing oral carcinoma in human as environmental factor and TLR 2 genotype frequencies were found to be observed in the smoking and nonsmoking population. 38 TLR 2 were also highly expressed in OSCC in comparison with adjacent non malignant tissues and it was also found that activated TLR2 by bacterial component enhances the progression of OSCC that may be implicated in acquired resistance to cisplatin-induced apoptosis regulation of the miR-146a pathway.39
TLR 3: This was found to be expressed in HNSCC and OSCC and has also shown association with activity of NF-kB by providing high level of expression.7,34,40 Significant increase in oral cancer risk was observed in mutated TLR3 genotype, where heterozygous and mutated TLR3 genotype and has worse survival in a group of patients with stage III tumor.41 This reveals that TLR3 play an important in the development of tumors and it could be considered as a target for OSCC therapy.
TLR 4: Anti-apoptotic proteins were found to be secreted when TLR 4 participates in oral carcinogenesis as TLR4 was highly expressed in OSCC.42 TLR4 and MyD88 were observed to be expressed in human OSCC cell lines and higher expression level with tumor differentiation was also noticed resulting in production of pro-inflammatory cytokines, chemokines, growth factor and thus enhancing the early stages of diseases.43 Increased expression of TLR4 are found to be in increased degree of oral epithelial dysplasia and distribution of TLR4 as dysplasia progressed from basal layer through the Stratum spinosum. 44 In short survival rate also TLR4 found to be associated with higher level of expression in it.45 High TLR4 expression were found to be correlated with deep tumor invasion.46 Increased expression of HIF-1 through NF- kB by activation of TLR4 found to be stimulated.47 Tumor progression found to be increased when Lipopolysaccharide (TLR4 ligand) induces TLR4 mediated epithelial-mesenchymal transition and cell migration in OSCC that affect tumor progression by inducing the tumor cell metastasis.48
TLR 5: Previous studies state that TLR5 expression were found to be more associated with tongue cancer cells adjacent to normal epithelium and with that high expression levels of TLR 5 with poorer prognosis.6 This TLR5 represents a link between bacteria and cancer with that it was found to be promoting tumor growth through inflammation dependent mechanism in epithelial cells.49 Subsequent release of cytokines and cancer invasion found to be present in expression of TLR5 and they could be linked to pathogenic bacteria or viral compound in oral cavity following carcinogenesis.49,50 In clinical behavior also TLR5 was found to be relevant in differentiating in oral cancer.42 Even in early stages, high TLR5 expression was found to associated with lower tumor grade.46 Female gender were found to be associated with higher level of TLR5 expression with age of >70 years at the time of diagnosis.6 Therapeutics approached was not found in association with TLR5 expression, tumor grade and stages but with that it was suggested from other authors, it could be useful marker for predicting recurrence or survival of OSCC patients.6,49
TLR7: Previous studies have investigated the role of TLR7 in oral tumor where it has revealed the up-regulated expression in oral carcinogenesis patients and with that it has shown poor differentiation and poor prognosis. Low tumor stages, no lymph node metastasis and better prognosis were observed with high expression of TLR7 in stroma fibroblast like cells.51 Recent study has shown that mRNA expression of TLR7 and its protein concentration observed significantly higher in tumors in esophageal cancer patients i.e. esophageal squamous cell carcinoma.52
TLR9: It’s a new member of the interleukin-1 receptor super family, which was found to be highly expressed in many of the carcinoma specimen. Expression of TLR9 was found to be significantly increased from mild to severe dysplasia compared to controls. TLR9 expression was higher in OSCC tissue when compared to ordinary controls53 but low in poorly differentiated squamous cell carcinoma.44 In deeper tumor invasion as well high TLR9 expression observed to be associated with it and hence it was clarified by high cytoplasmic TLR9 expression in primary tumors than local recurrent counterparts.36,54 This can be hypothesized that with increased expression levels of TLR9 may play important role as target for oral cancer prevention in near future.53
Toll like receptors as suppression of oral squamous cell carcinoma
Toll like receptors (TLR) plays an important role in recognition of invading pathogens and activation of immune response which protects the host, from the recognition lipopolysaccharide (LPS), peptidoglycans and lipoproteins by activating several cellular pathways following ligand stimulation.3,55 Varieties of TLRs such as TLR1, TLR2,TLR4, TLR5 and TLR6 found to be located on the cell surface and detect lipoproteins and bacterial LPS, which is essential for immune system modulation. This increased concentration of circulating LPS lead to low grade chronic inflammation which was found to be involved in the pathophysiology of inflammatory and metabolic disease. On the basis of previous studies TLRs have been identified as important regulators of metabolic inflammations in many tissues.56Within the progression of OSCC, suppression of OSCC has been also studied in association with TLRs that re given below:
i) TLR3: TLR3 activation found to be responsible for inhibiting the OSCC tumor growth in vivo studies as well.48 With the treatment of poly I:C, cell growth is found to be inhibited in a dose dependent manner.57 Synthetic dsRNA-polyinosinic-polycytidilic acid is a TLR3 ligand that induces apoptosis of OSCC by interferon- β production and activation of caspase 3 and 9.56 This direct proapoptotic activity of TLR3 in human oral squamous cell carcinoma can be utilized as therapeutic target for the treatment of OSCC in oral tumors with not sensitive to ant-cancer drugs.58 Immunotherapy was also observed where TLR3 indicted affect against OSCC development and can be considered as a potential target for future OSCC immunotherapy.59
ii) TLR7: Previous studies state that TLR7 were administrated to oral cancer cells and it has revealed inhibitory proliferative activity in OSCC. With that IL-6 and IL-8 production in OSCC found to be produced and suggest the functional expression of TLR7 against oral cancer development.60
Discussion
Toll like receptors was considered to be an important role in the innate immunity activation and also in the subsequent inflammatory process, has also shown its role in carcinogenesis. With respect to the development of oral squamous cell carcinoma, TLR2, TLR3, TLR4, TLR5, TLR7 and TLR9 found to be associated with the progression of OSCC. As far as the suppression of OSCC was concerned, TLR3 and TLR7 were observed in suppression of OSCC. From the present observation, toll like receptors found to be both progressive and suppressive in concern with oral squamous cell carcinoma. Being an agonist, they are found to be promoting the survival of malignant cells and this has also effects chemotherapy, where as TLRs has also shown its important role in recognition of pathogen and activation of immune response. From the above literature, it was observed that TLR 3 and TLR 7 found to be most common between progressing and suppressing the OSCC. As far as the progression was concerned mutant TLR3 genotype found to be significantly increase in oral cancer, where as it has act as ligand and induce apoptosis of OSCC by interferon-β production and activation of caspase 3 and 9.41 Immunotherpay was also observed against OSCC development of TLR3.59 Not only in OSCC, but also in breast cancer has shown its immunotherapy by effective inhibition of CSCs which was enhanced by TLR3 activation.61 TLR3 activation on cancer cells has been reported to mediate apoptosis in several cancer histotypes, primarily through an extrinsic pathway.62 TLR7 which was considered to be promoting OSCC by upregulating expression in oral carcinogenesis patient, has shown its inhibitory proliferative activity in OSCC with the IL-6 and IL-8 production.60 TLR 7 was also found to be activated by different agonist such as Imiquimod, resiquimod and gardiquimod that has shown an immune response reveals that TLR7 can also be considered as antitumor activity.62 From this study, it was observed that TLR found to be both progressive and suppressive in nature with respect to carcinogenesis, which signifies that TLR are also considered to be in association with OSCC.
Conclusions
TLRs revealed a significant role in PAMPS and DAMPS identification and stimulation of Innate Immune response. It has also revealed pivotal role in progression pattern and inflammation profile of OSCC. Relationship between TLRs and OSCC found to be linked with genetic disruption of TLR & adopter molecule that promote tumor development and progression, where as progression of OSCC found to be mainly associated with the TLR2, TLR3, TLR4, TLR5, TLR7 and TLR9. Suppression of OSCC through TLR3 and TLR7 was found to be observed in the above literature that indicates effectiveness against OSCC development and can be utilized as therapeutic insight for future treatment modality in OSCC.
Acknowledgments
The authors would like to acknowledge our Dr. Chandardeep Tandon, Professor, Director, Amity Institute of Biotechnology, Amity University, Noida, India for their valuable guidance and support.
Abbreviations
OSCC, Oral squamous cell carcinoma; TLR, Toll Like Receptor; PRRs, pattern recognition receptors PAMP, Pathogen associated molecular pattern; DAMP, Damage associated molecular pattern; NLR, NOD like receptor; RLR, RIG like receptor; IFN, type 1 interferon; HPV, Human papilloma virus; NF-κB, Nuclear factor kappa-light-chain-enhancer of activated B cells; MyD88, MYD88 Innate Immune Signal Transduction Adaptor; HIF-1, Hypoxia-inducible factors; LPS, lipopolysaccharide.
References
- 1.Vigneswaran N, Williams MD. Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac Surg Clin North Am 2014;26:123-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tezal M, Sullivan MA, Hyland A, et al. Chronic Periodontitis and the Incidence of Head and Neck Squamous Cell Carcinoma. Cancer Epidemiol Prev Biomark 2009;18:2406-12. [DOI] [PubMed] [Google Scholar]
- 3.Pisani LP, Estadella D, Ribeiro DA. The Role of Toll Like Receptors (TLRs) in Oral Carcinogenesis. Anticancer Res 2017;37:5389-94. [DOI] [PubMed] [Google Scholar]
- 4.Fukata M, Chen A, Vamadevan AS, et al. Toll-like receptor-4 promotes the development of colitis-associated colorectal tumors. Gastroenterology 2007;133:1869-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruckdeschel K, Pfaffinger G, Haase R, et al. Signaling of apoptosis through TLRs critically involves toll/IL-1 receptor domaincontaining adapter inducing IFN-beta, but not MyD88, in bacteria- infected murine macrophages. J Immunol 2004;173:3320-8. [DOI] [PubMed] [Google Scholar]
- 6.Kauppila JH, Mattila AE, Karttunen TJ, Salo T. Toll-like receptor 5 (TLR5) expression is a novel predictive marker for recurrence and survival in squamous cell carcinoma of the tongue. Br J Cancer 2013;108:638-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chuang H-C, Huang C-C, Chien C-Y, Chuang J-H. Toll-like. receptor 3-mediated tumor invasion in head and neck cancer. Oral Oncol 2012;48:226-32. [DOI] [PubMed] [Google Scholar]
- 8.Takeda K, Akira S. Toll-like receptors in innate immunity. Int Immunol 2005;17:1-14. [DOI] [PubMed] [Google Scholar]
- 9.Yang Z-H, Dai Q, Gu Y-J, et al. Cytokine and chemokine modification by Toll-like receptor polymorphisms is associated with nasopharyngeal carcinoma. Cancer Sci 2012;103:653-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer 2006;118:3030-44. [DOI] [PubMed] [Google Scholar]
- 11.Rich AM, Hussaini HM, Parachuru VPB, Seymour GJ. Toll-like receptors and cancer, particularly oral squamous cell carcinoma. Front Immunol 2014;5:464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ridnour LA, Cheng RYS, Switzer CH, et al. Molecular pathways: toll-like receptors in the tumor microenvironment—poor prognosis or new therapeutic opportunity. Clin Cancer Res 2013;19:1340-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pradere J-P, Dapito DH, Schwabe RF. The Yin and Yang of Tolllike receptors in cancer. Oncogene 2014;33:3485-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xie W, Wang Y, Huang Y, et al. Toll-like receptor 2 mediates invasion via activating NF-kappaB in MDA-MB-231 breast cancer cells. Biochem Biophys Res Commun 2009;379:1027-32. [DOI] [PubMed] [Google Scholar]
- 15.Hua D, Liu M-Y, Cheng Z, et al. Small interfering RNA-directed targeting of Toll-like receptor 4 inhibits human prostate cancer cell invasion, survival, and tumorigenicity. Mol Immunol 2009;46:2876-84. [DOI] [PubMed] [Google Scholar]
- 16.Killeen SD, Wang JH, Andrews EJ, Redmond HP. Bacterial endotoxin enhances colorectal cancer cell adhesion and invasion through TLR-4 and NF-kappaB-dependent activation of the urokinase plasminogen activator system. Br J Cancer 2009;100:1589-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee C-H, Wu C-L, Shiau A-L. Toll-like receptor 4 signaling promotes tumor growth. J Immunother 2010;33:73-82. [DOI] [PubMed] [Google Scholar]
- 18.Yu L, Wang L, Chen S. Dual character of Toll-like receptor signaling: pro-tumorigenic effects and anti-tumor functions. Biochim Biophys Acta 2013;1835:144-54. [DOI] [PubMed] [Google Scholar]
- 19.Xie W, Huang Y, Xie W, et al. Bacteria peptidoglycan promoted breast cancer cell invasiveness and adhesiveness by targeting toll-like receptor 2 in the cancer cells. PLoS One 2010;5:e10850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Camargo Cancela M, Voti L, Guerra-Yi M, et al. Oral cavity cancer in developed and in developing countries: populationbased incidence. Head Neck 2010;32:357-67. [DOI] [PubMed] [Google Scholar]
- 21.Shenoi R, Devrukhkar V, Sharma BK, et al. Demographic and clinical profile of oral squamous cell carcinoma patients: a retrospective study. Indian J Cancer 2012;49:21-6. [DOI] [PubMed] [Google Scholar]
- 22.Rivera C, Venegas B. Histological and molecular aspects of oral squamous cell carcinoma (Review). Oncol Lett 2014;8:7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Y, Azad MB, Gibson SB. Superoxide is the major reactive oxygen species regulating autophagy. Cell Death Differ 2009;16:1040-52. [DOI] [PubMed] [Google Scholar]
- 24.Akram S, Mirza T, Aamir Mirza M, Qureshi M. Emerging Patterns in Clinico-pathological spectrum of Oral Cancers. Pakistan J Med Sci 2013;29:783-7. [PMC free article] [PubMed] [Google Scholar]
- 25.Dikshit RP, Kanhere S. Tobacco habits and risk of lung, oropharyngeal and oral cavity cancer: a population-based case-control study in Bhopal, India. Int J Epidemiol 2000;29:609-14. [DOI] [PubMed] [Google Scholar]
- 26.D’Souza G, Gross ND, Pai SI, et al. Oral human papillomavirus (HPV) infection in HPV-positive patients with oropharyngeal cancer and their partners. J Clin Oncol 2014;32:2408-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Plemons JM, Al-Hashimi I, Marek CL. Managing xerostomia and salivary gland hypofunction: executive summary of a report from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2014;145:867-73. [DOI] [PubMed] [Google Scholar]
- 28.von Bultzingslowen I, Sollecito TP, Fox PC, et al. Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:S57.e1-15. [DOI] [PubMed] [Google Scholar]
- 29.Jerjes W, Upile T, Petrie A, et al. Clinicopathological parameters, recurrence, locoregional and distant metastasis in 115 T1- T2 oral squamous cell carcinoma patients. Head Neck Oncol 2010;2:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ali J, Sabiha B, Jan HU, et al. Genetic etiology of oral cancer. Oral Oncol 2017;70:23-8. [DOI] [PubMed] [Google Scholar]
- 31.Shcheblyakov DV, Logunov DY, Tukhvatulin AI, et al. Toll-Like Receptors (TLRs): The Role in Tumor Progression. Acta Naturae 2010;2:21-9. [PMC free article] [PubMed] [Google Scholar]
- 32.Yu L, Wang L, Chen S. Endogenous toll-like receptor ligands and their biological significance. J Cell Mol Med 2010;14:2592-603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu L, Chen S. Toll-like receptors expressed in tumor cells: targets for therapy. Cancer Immunol Immunother 2008;57:1271-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ng LK, Rich AM, Hussaini HM, et al. Toll-like receptor 2 is present in the microenvironment of oral squamous cell carcinoma. Br J Cancer 2011;104:460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sutmuller R, Garritsen A, Adema GJ. Regulatory T cells and toll-like receptors: regulating the regulators. Ann Rheum Dis 2007;66:iii91-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morais CA, de Rosso VV, Estadella D, Pisani LP. Anthocyanins as inflammatory modulators and the role of the gut microbiota. J Nutr Biochem 2016;33:1-7. [DOI] [PubMed] [Google Scholar]
- 37.Jouhi L, Koljonen V, Bohling T, et al. The expression of Toll-like receptors 2, 4, 5, 7 and 9 in Merkel cell carcinoma. Anticancer Res 2015;35:1843-9. [PubMed] [Google Scholar]
- 38.Kohailan M, Alanazi M, Rouabhia M, et al. Effect of smoking on the genetic makeup of toll-like receptors 2 and 6. Onco Targets Ther 2016;9:7187-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ikehata N, Takanashi M, Satomi T, et al. Toll-like receptor 2 activation implicated in oral squamous cell carcinoma development. Biochem Biophys Res Commun 2018;495:2227-34. [DOI] [PubMed] [Google Scholar]
- 40.Luo Q, Hu S, Yan M, et al. Activation of Toll-like receptor 3 induces apoptosis of oral squamous carcinoma cells in vitro and in vivo. Int J Biochem Cell Biol 2012;44:1266-75. [DOI] [PubMed] [Google Scholar]
- 41.Zeljic K, Supic G, Jovic N, et al. Association of TLR2, TLR3, TLR4 and CD14 genes polymorphisms with oral cancer risk and survival. Oral Dis 2014;20:416-24. [DOI] [PubMed] [Google Scholar]
- 42.Omar AAH, Korvala J, Haglund C, et al. Toll-like receptors -4 and -5 in oral and cutaneous squamous cell carcinomas. J Oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 2015;44:258-65. [DOI] [PubMed] [Google Scholar]
- 43.Sun Z, Luo Q, Ye D, et al. Role of toll-like receptor 4 on the immune escape of human oral squamous cell carcinoma and resistance of cisplatin-induced apoptosis. Mol Cancer 2012;11:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kotrashetti VS, Nayak R, Bhat K, et al. Immunohistochemical expression of TLR4 and TLR9 in various grades of oral epithelial dysplasia and squamous cell carcinoma, and their roles in tumor progression: a pilot study. Biotech Histochem 2013;88:311-22. [DOI] [PubMed] [Google Scholar]
- 45.Ren WH, Zhang LM, Liu HQ, et al. Protein overexpression of CIRP and TLR4 in oral squamous cell carcinoma: an immunohistochemical and clinical correlation analysis. Med Oncol 2014;31:120. [DOI] [PubMed] [Google Scholar]
- 46.Ruan M, Thorn K, Liu S, et al. The secretion of IL-6 by CpGODN- treated cancer cells promotes T-cell immune responses partly through the TLR-9/AP-1 pathway in oral squamous cell carcinoma. Int J Oncol 2014;44:2103-10. [DOI] [PubMed] [Google Scholar]
- 47.Han S, Xu W, Wang Z, et al. Crosstalk between the HIF-1 and Toll-like receptor/nuclear factor-kappaB pathways in the oral squamous cell carcinoma microenvironment. Oncotarget 2016;7:37773-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.He Z, Deng R, Huang X, et al. Lipopolysaccharide enhances OSCC migration by promoting epithelial-mesenchymal transition. J oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 2015;44:685-92. [DOI] [PubMed] [Google Scholar]
- 49.Grimm M, Munz A, Exarchou A, et al. Immunohistochemical detection of Helicobacter pylori without association of TLR5 expression in oral squamous cell carcinoma. J Oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 2014;43:35-44. [DOI] [PubMed] [Google Scholar]
- 50.Sato J, Nishimura M, Yamazaki M, et al. Expression profile of drosomycin-like defensin in oral epithelium and oral carcinoma cell lines. Arch Oral Biol 2013;58:279-85. [DOI] [PubMed] [Google Scholar]
- 51.Ni YH, Ding L, Zhang DY, et al. Distinct expression patterns of Toll-like receptor 7 in tumour cells and fibroblast-like cells in oral squamous cell carcinoma. Histopathology 2015;67:730-9. [DOI] [PubMed] [Google Scholar]
- 52.Diakowska D, Nienartowicz M, Grabowski K, et al. Toll-like receptors TLR-2, TLR-4, TLR-7, and TLR-9 in tumor tissue and serum of the patients with esophageal squamous cell carcinoma and gastro-esophageal junction cancer. Adv Clin Exp Med 2019;28:515-22. [DOI] [PubMed] [Google Scholar]
- 53.Min R, Siyi L, Wenjun Y, et al. Toll-like receptor-9 agonists increase cyclin D1 expression partly through activation of activator protein-1 in human oral squamous cell carcinoma cells. Cancer Sci 2012;103:1938-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Makinen LK, Atula T, Hayry V, et al. Predictive role of Toll-like receptors 2, 4, and 9 in oral tongue squamous cell carcinoma. Oral Oncol 2015;51:96-102. [DOI] [PubMed] [Google Scholar]
- 55.Mikulandra M, Pavelic J, Glavan TM. Recent Findings on the Application of Toll-like Receptors Agonists in Cancer Therapy. Curr Med Chem 2017;24:2011-32. [DOI] [PubMed] [Google Scholar]
- 56.Jin C, Flavell RA. Innate sensors of pathogen and stress: linking inflammation to obesity. J Allergy Clin Immunol 2013;132: 287-94. [DOI] [PubMed] [Google Scholar]
- 57.Park J-H, Jeon D-I, Yoon H-E, et al. Poly I:C inhibits cell proliferation and enhances the growth inhibitory effect of paclitaxel in oral sqaumous cell carcinoma. Acta Odontol Scand 2012;70: 241-5. [DOI] [PubMed] [Google Scholar]
- 58.Luo W, Wang C-Y, Jin L. Baicalin downregulates Porphyromonas gingivalis lipopolysaccharide-upregulated IL-6 and IL-8 expression in human oral keratinocytes by negative regulation of TLR signaling. PLoS One 2012;7:e51008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.He Z, Huang X, Ni Y, et al. Functional toll-like receptor 3 expressed by oral squamous cell carcinoma induced cell apoptosis and decreased migration. Oral Surg Oral Med Oral Pathol Oral Radiol 2014;118:92-100. [DOI] [PubMed] [Google Scholar]
- 60.Ahn M-Y, Kwon S-M, Cheong HH, et al. Toll-like receptor 7 agonist, imiquimod, inhibits oral squamous carcinoma cells through apoptosis and necrosis. J Oral Pathol Med Off Publ Int Assoc Oral Pathol Am Acad Oral Pathol 2012;416:540-6. [DOI] [PubMed] [Google Scholar]
- 61.Jia D, Wang L. The other face of TLR3: A driving force of breast cancer stem cells. Mol Cell Oncol 2015;2:e981443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bianchi F, Milione M, Casalini P, et al. Toll-like receptor 3 as a new marker to detect high risk early stage Non-Small-Cell Lung Cancer patients. Sci Rep 2019;9:14288. [DOI] [PMC free article] [PubMed] [Google Scholar]


