Abstract
Chronic obstructive pulmonary disease (COPD) has been considered a significant health challenge globally in recent years, which affects different aspects of the quality-of-life (QoL). A review was conducted of research output, research topics, and landscape to have a global view of the papers mentioning the interventions to increase QoL of patients with COPD. A total of 3242 research items from Web of Science during the period 1990–2018 were downloaded and analyzed. Analyses based on the different levels of data and methods using using VOSviewer software tool (version 1.16.15, Centre for Science and Technology Studies (CWTS), Leiden University, Leiden, The Netherlands) and Latent Dirichlet allocation. By exploring the trends in research productivity and topics, an increase was found in the number of papers mentioning non-pharmacological interventions as well as mental health illness and QoL among patients with COPD. In conclusion, the research on the interventions to increase the QoL of patients with COPD has attracted scientists globally. It is suggested that more research should be conducted on the effectiveness of non-pharmacological therapies to increase QoL of patients with COPD that can be applied broadly in the community. The collaboration and support from developed countries to developing countries are needed to increase the QoL of people living with COPD.
Keywords: scientometrics, content analysis, text mining, interventions, COPD, QoL
1. Introduction
Chronic obstructive pulmonary disease (COPD) is one of the chronic airway diseases, which characterized by the limitation in airflow and not fully reversible [1]. The reported prevalence of COPD is different among regions: 4% in Europe [2], 6.3% in the Asia Pacific region [3], from less than 4% to over 9% [4] in the US and predicted, with limited epidemiological evidence, to be at about 11% in 2010 in the African region [5,6].
This chronic disease has significant adverse effects on physical and mental conditions of those patients [7,8,9], as other systems and organs other than the lungs suffered the negative impacts, leading to pneumonia [10], pulmonary hypertension [11], and cardiovascular disease (CVD) [12]. A worsening mental status has been found in patients with COPD compared to non-COPD subjects, with higher rates of anxiety and depression [13,14], and the severity of fatigue [15]. Patients with COPD less frequently report a partner compared to others, and, when having a partner, they were less likely to be ‘very satisfied’ with the daily support and less often perceived emotional support from the partner [16]. They suffer worse quality of life with early-morning and nighttime symptoms compared to those without COPD [17,18]. COPD often results in a reduction in quality of life.
Quality of life (QoL) is defined by World Health Organization as a broad and complex concept of an individual about their physical health, mental health, social relationships and beliefs in the context of their living enviroment [19]. It is a “multidimensional measure” which focus on at least three domains: physics, psychology and society. Thus, several studies applied dimensions of QoL to to: (1) evaluate the efficiency of clinical therapies [20,21,22] or alternative therapies [23,24]; (2) identify factors associated with QoL [25] and increase health service quality [24]. In the case of COPD, improving QoL of patients with COPD becomes critical due to the incurables [26]. Medical methods have been used mainly to control COPD and strengthen prevention efforts, such as: (1) smoking cessation [27,28], (2) pharmacotherapy [29], and (3) Non-pharmacological therapy [30]. Therefore, measuring QoL could be useful in applying suitable interventions and preventing risk factors affected COPD.
Systematic reviews of interventions and treatments are considered as a reliable source of evidence to inform clinical practice and policy development [31]. Several systematic reviews and meta-analyses mentioning interventions to patients with COPD have been conducted. Gregersen et al. confirmed that telehealth showed promise for improving QoL of patients living with COPD, yet, this method call for more research to prove its effectiveness [32]. According to Coronini-Cronberg et al., psychosocial and pharmacological support is an effective intervention for smoking cessation [33], which raises the QoL in some health domains [34]. Moreover, breathing exercises can be used to improve the QoL of patients living with COPD, yet, the use of this method as a complementary therapy needs more research [35]. These literature review studies answer specific questions by gathering available empirical research evidence. However, a limitation of this approach is that it could review one method, which makes it difficult to compare the effects of all methods during a long period of study.
In addition, several researchers have used indicators of scientometric to review literature [36]. Prvevious studies used bibliometrics to explore research output, country collaboration, journal ranking or fundings of all papers mentioning COPD in European countries [37] or in Arab countries [38]. However, scientometric analyses may not have a deep understanding of the context of research or the landscape of research areas. Therefore, by combining scientometric and Latent Direcht allocation, topic modeling (in titles and abstracts), this study aims to describe the global trend in research outputs, countries collaboration, interdisciplinary research areas, as well as ten common topics among papers mentioning interventions to improve QoL of patients with COPD. The findings will emphasize research gaps, and make it possible to recommend some implications for future studies and policy.
2. Materials and Methods
2.1. Database and Search Strategy
The data were retrieved in the middle of 2019 from the Web of Science (WoS) Core Collection. It was decided to choose WoS because WoS (1) allows to download a large number of papers and (2) provides necessary information for scientometrics analysis, such as authors’ affiliations, authors’ keywords, the title of papers, publication year, research areas, as well as the number of citations and download times for each paper [39,40].
The search strategy was described as follow:
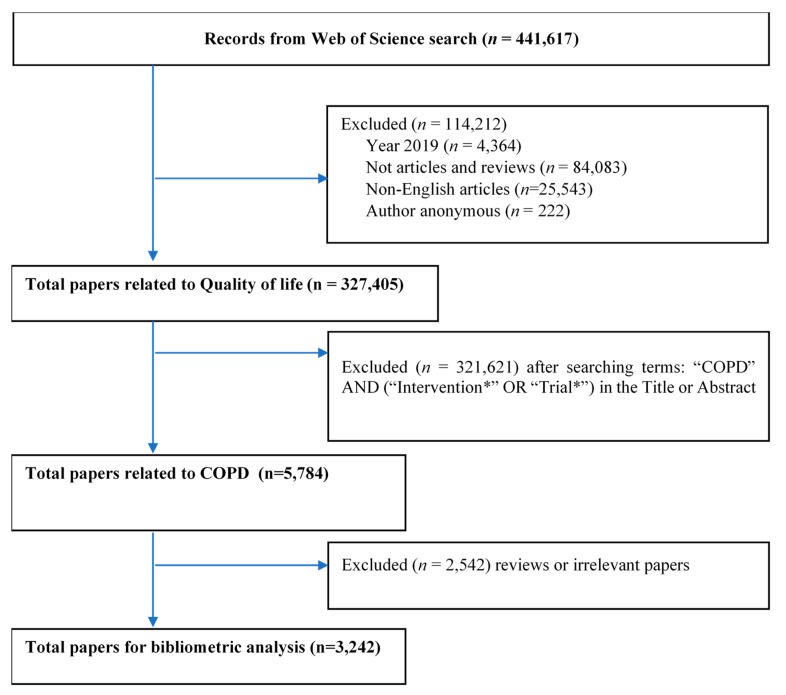
Step 1: With the use of Boolean operators “OR”, the search query was developed to identify the number of published items related to “Quality of life” OR “well-being”. Only English research articles and research reviews were included, while grey literature, conference proceedings, or books/book chapters in any other language were excluded. Papers having anonymous authors and publications in 2019 were also limited. This research began in the middle of 2019; thus, this data could not reflect the research trend for the whole year. Data in WoS databases under text format was downloaded and imported to STATA version 15.0 (STATACorp., Texas, TX, USA) for further extraction. (See Table A1)
Step 2: STATA syntax was applied to filter the papers in step 1 with the terms “Intervention” OR “Interventions” OR “trial” OR “trials” in titles or abstracts.
Step 3: The COPD keywords were formed by COPD specialists and reviewing some papers and MeSH term library of PubMed. These terms were used to search in the title and keyword fields among papers in step 2 (see Table A1), and there were 5784 papers for further screening.
Step 4: Two researchers separately screened the titles and abstracts of 5784 papers to exclude papers not related to COPD. A group discussion with a senior researcher was conducted if there were any contradictions. A total of 3242 papers were imported to STATA for further analysis. (See Figure A1).
2.2. Data Analysis
The corrected data after the screening was imported to STATA for further analysis using the following information of the articles: authors’ affiliations, the title of papers, the journals’ name, authors’ keywords, the number of citations, research areas, and abstracts.
Several basic characteristics of the data sets were included publication year, the number of papers /per year, total citations up to 2018, average citation rate per year, total number of downloads in the last six months/five years, and average number of downloads (mean use rate) the last six months/five years. Two network graphs showing the countries collaboration and co-occurrence terms in title and abstracts were established by VOSviewer (version 1.16.15, Centre for Science and Technology Studies (CWTS), Leiden University, Leiden, The Netherlands). Latent dirichlet allocation (LDA) was used for classifying papers into topics [41,42,43,44,45]. The titles and abstracts of most cited papers within each group were reviewed. After discussing with COPD specialists, the labels for each topic were named. In addition to the number and percentage of publications of each topic, these topics were ranked based on the total number of publications in the past five years to explore the research interests. Table 1 shows the methods and results for each kind of data.
Table 1.
Summary of analytical techniques for each data types.
| Type of Data | Unit of Analysis | Analytical Methods | Presentations of Results |
|---|---|---|---|
| Terms, Countries | Words | Frequency of co-occurrence | Map of terms co-occurrence clusters |
| Abstracts | Papers | Latent Dirichlet Allocation | Ten classifications of research topics |
| WoS classification of research areas | WoS research areas | Frequency of co-occurrence | Dendrogram of research disciplines (WoS classification) |
3. Results
Overall Growth and Essential Characteristics of Research
Table 2 described the basic characteristics of publications. The first seven papers related to this health issues in dataset were published in 1991. There has been a gradual raise in the annual number of papers on intervention to improve the QoL of patients with COPD within the period 1991–2018, contributing to a total of 3242 papers. The papers in 2018 showed the reading interests of readers in last six month with the average times of download (mean use rate) was 1.8; meanwhile, the papers in 2013 received the highest concern in last five years with average times of download (the mean use rate) was 2.1. The papers in the year 2000 had the highest average citation with 6.9 citations per paper.
Table 2.
General characteristics of publications.
| Year Published | Total Number of Papers | Total Citations | Mean Cite Rate per Year | Total Usage Last 6 Month | Total Usage Last 5 Years | Mean Use Rate Last 6 Month | Mean Use Rate Last 5 Year |
|---|---|---|---|---|---|---|---|
| 2018 | 314 | 197 | 0.6 | 562 | 822 | 1.8 | 0.5 |
| 2017 | 295 | 1763 | 3.0 | 356 | 1756 | 1.2 | 1.2 |
| 2016 | 306 | 1946 | 2.1 | 254 | 2055 | 0.8 | 1.3 |
| 2015 | 270 | 3311 | 3.1 | 219 | 2198 | 0.8 | 1.6 |
| 2014 | 284 | 5101 | 3.6 | 177 | 2753 | 0.6 | 1.9 |
| 2013 | 234 | 3970 | 2.8 | 128 | 2451 | 0.5 | 2.1 |
| 2012 | 199 | 4653 | 3.3 | 78 | 1825 | 0.4 | 1.8 |
| 2011 | 189 | 6880 | 4.6 | 90 | 1424 | 0.5 | 1.5 |
| 2010 | 144 | 5733 | 4.4 | 75 | 1146 | 0.5 | 1.6 |
| 2009 | 128 | 5719 | 4.5 | 61 | 823 | 0.5 | 1.3 |
| 2008 | 127 | 6549 | 4.7 | 36 | 819 | 0.3 | 1.3 |
| 2007 | 109 | 5158 | 3.9 | 33 | 492 | 0.3 | 0.9 |
| 2006 | 107 | 6800 | 4.9 | 28 | 514 | 0.3 | 1.0 |
| 2005 | 86 | 4625 | 3.8 | 37 | 422 | 0.4 | 1.0 |
| 2004 | 75 | 5445 | 4.8 | 30 | 448 | 0.4 | 1.2 |
| 2003 | 62 | 6317 | 6.4 | 20 | 385 | 0.3 | 1.2 |
| 2002 | 56 | 5847 | 6.1 | 15 | 257 | 0.3 | 0.9 |
| 2001 | 40 | 2757 | 3.8 | 3 | 157 | 0.1 | 0.8 |
| 2000 | 43 | 5670 | 6.9 | 28 | 324 | 0.7 | 1.5 |
| 1999 | 28 | 1612 | 2.9 | 6 | 112 | 0.2 | 0.8 |
| 1998 | 32 | 3324 | 4.9 | 14 | 196 | 0.4 | 1.2 |
| 1997 | 29 | 2223 | 3.5 | 8 | 146 | 0.3 | 1.0 |
| 1996 | 18 | 2275 | 5.5 | 3 | 91 | 0.2 | 1.0 |
| 1995 | 16 | 1681 | 4.4 | 9 | 80 | 0.6 | 1.0 |
| 1994 | 10 | 1060 | 4.2 | 0 | 40 | 0.0 | 0.8 |
| 1993 | 12 | 559 | 1.8 | 4 | 20 | 0.3 | 0.3 |
| 1992 | 9 | 420 | 1.7 | 2 | 14 | 0.2 | 0.3 |
| 1991 | 7 | 426 | 2.2 | 0 | 11 | 0.0 | 0.3 |
The paper having the highest influence was the second report entitled Global Strategy for the Diagnosis, Management, and Prevention of COPD published in 2007 with 3456 citations [46].
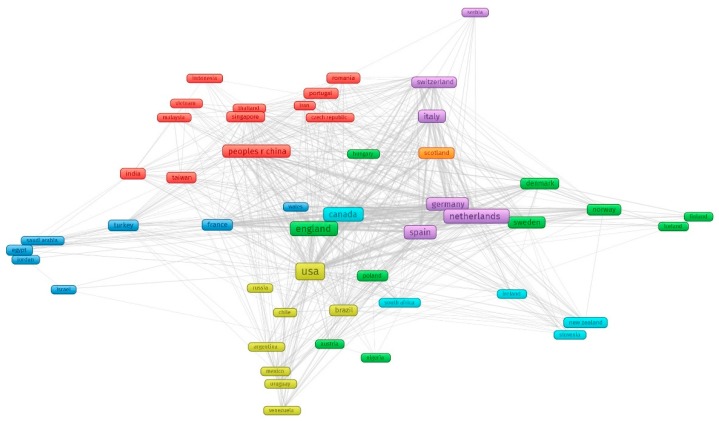
Figure 1 shows countries collaboration network. In total, there were 89 countries contributing for the research field (automatically calculated by VOSviewer). In figure there were 64 countries with minimum of 5 papers. Of those, the United States of America led in the number of studies with 786 papers (24.2%), followed by England (452 papers, 13.9%), the Netherlands (322 papers, 9.9%), and Canada (268 papers, 8.3%). Although people living in low-and middle-income countries (LMICs) are more vulnerable to developing COPD [47], there was only China in the list of top 10 countries having the highest volume. As can ben seen, there were four main clusters in this countries network (1) Asia with the leadership of China in collaboration with two East European countries (Czech and Romania) (red cluster); (2) the U.S and South American countries (yellow cluster); (3) Canada, South Africa, New Zealandm and European countries (turquoise cluster); (4) European countries with three subgroups with the lead of France, the Netherlands, and England (the rest).
Figure 1.
Countries collaboration network. Note: four main clusters, including (1) red cluster: Asia countries and two East European countries (Czech and Romania); (2) yellow cluster: the U.S and South American countries; (3) turquoise cluster Canada and South Africa, New Zealand and European countries; (4) the rest: European countries with three subgroups with the lead of France, the Netherlands and England.
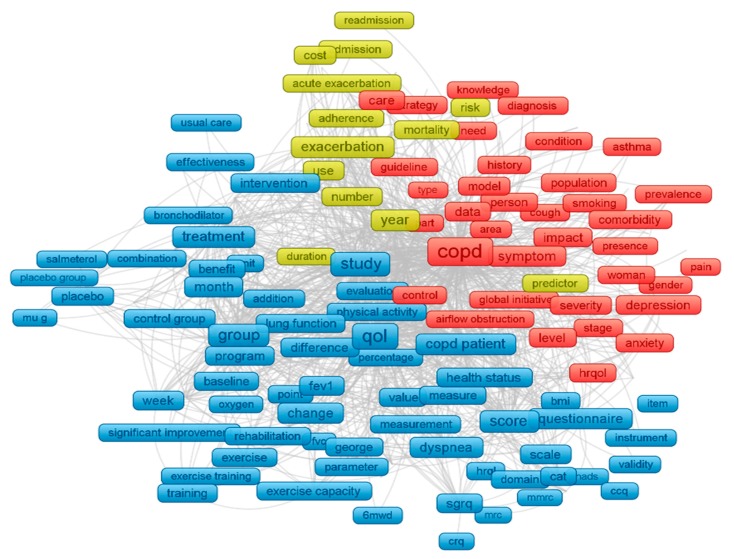
By analyzing abstracts and titles, the most co-occurrence terms were found to discover the scope of COPD research (Figure 2). Three major clusters were formed by 279 most common terms in title and abstract with the minimum appearance of 95 times. The three significant clusters are: Cluster 1 (red) refers to comorbidity and COPD, among which mental health illness (depression and anxiety) was most frequently mentioned. Cluster 2 (blue) focuses on interventions and treatment to increase QoL of people with COPD. Cluster 3 (yellow) points out the risk and mortality of exacerbation of COPD.
Figure 2.
Text mining using VOSviewer (titles and abstracts). Note: the colors of each node were automatically assigned by VOSviewer based on its score; the node size was based on the frequency of each term; the length and thickness of the lines reflected the association between two terms. Cluster 1 (red) refers to comorbidity and COPD; cluster 2 (blue) focuses on interventions and treatment to increase QoL of people with COPD, cluster 3 (yellow) points out the risk and mortality of exacerbation of COPD.
Table 3 shows the most cited papers. Each had more than 100 citations during the study period. Based on the list, three main topics which have been recently attracted the attention of researchers were: (1) The Global Initiative for chronic obstructive lung disease (GOLD) reports and other national reports. GOLD was a consensus report published periodically since 2001. It included the latest evidence for diagnosis and prevention from experts, which were as “strategy documents” for adequate care for COPD at a global level [48] (paper 1, paper 7, paper 4, paper 9, paper 28, paper 36 ); (2) Exacerbations in patients with COPD (paper 2, paper 3, paper 12, paper 25, paper 29, paper 32); (3) Treatments and interventions of COPD (paper 5, paper 6, paper 11, paper 14, paper 15, paper 17, paper 19, paper 20, paper 23, paper 24, paper 27, paper 33, paper 34, paper 35, paper 39, paper 40), (4) QoL, health-related QoL and COPD (paper 26, paper 30, paper 31, and paper 41), others topic (rehabilitation—paper 8; COPD and comorbidity—paper 10; COPD and its effects to patient health and life—paper 22 and paper 37).
Table 3.
Most cited papers.
| No | Title | Total Citation | Published Year | Cite Rate |
|---|---|---|---|---|
| 1 | The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease | 2046 | 2004 | 136.4 |
| 2 | A 4-year trial of tiotropium in chronic obstructive pulmonary disease | 1390 | 2008 | 126.4 |
| 3 | Susceptibility to Exacerbation in Chronic Obstructive Pulmonary Disease. | 1298 | 2010 | 144.2 |
| 4 | Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease | 1223 | 1998 | 58.2 |
| 5 | Randomised, double blind, placebo-controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial* | 964 | 2000 | 50.7 |
| 6 | Development and first validation of the COPD Assessment Test | 933 | 2009 | 93.3 |
| 7 | Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease | 868 | 2005 | 62.0 |
| 8 | Outcomes following acute exacerbation of severe chronic obstructive lung disease | 863 | 1996 | 37.5 |
| 9 | Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial | 749 | 2003 | 46.8 |
| 10 | Chronic obstructive pulmonary disease: current burden and future projections | 698 | 2006 | 53.7 |
| 11 | Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease | 655 | 2000 | 34.5 |
| 12 | A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease | 609 | 2002 | 35.8 |
| 13 | Azithromycin for Prevention of Exacerbations of COPD | 578 | 2011 | 72.3 |
| 14 | Reduction of hospital utilization in patients with chronic obstructive pulmonary disease—A disease-specific self-management intervention | 576 | 2003 | 36.0 |
| 15 | Effects of pulmonary rehabilitation on physiological and psychosocial outcomes in patients with chronic obstructive pulmonary disease | 568 | 1995 | 23.7 |
| 16 | Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease | 550 | 2003 | 34.4 |
| 17 | Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial | 536 | 2000 | 28.2 |
| 18 | Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD | 500 | 2002 | 29.4 |
| 19 | Improved health outcomes in patients with COPD during 1 year’s treatment with tiotropium | 492 | 2002 | 28.9 |
| 20 | Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease | 472 | 2003 | 29.5 |
| 21 | Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report | 467 | 2017 | 233.5 |
| 22 | Relation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbations | 458 | 2000 | 24.1 |
| 23 | Tiotropium in combination with placebo, salmeterol, or fluticasone-salmeterol for treatment of chronic obstructive pulmonary disease—A randomized trial | 448 | 2007 | 37.3 |
| 24 | Meta-analysis of respiratory rehabilitation in chronic obstructive pulmonary disease | 443 | 1996 | 19.3 |
| 25 | Risk factors of readmission to hospital for a COPD exacerbation: a prospective study | 421 | 2003 | 26.3 |
| 26 | Mortality after hospitalization for COPD | 380 | 2002 | 22.4 |
| 27 | Depressive symptoms and chronic obstructive pulmonary disease—Effect on mortality, hospital readmission, symptom burden, functional status, and quality of life | 369 | 2007 | 30.8 |
| 28 | How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer | 338 | 2000 | 17.8 |
| 29 | Randomized controlled trial of respiratory rehabilitation | 337 | 1994 | 13.5 |
| 30 | Early therapy improves of chronic obstructive outcomes of exacerbations pulmonary disease | 335 | 2004 | 22.3 |
| 31 | Quality of life changes in COPD patients treated with salmeterol | 331 | 1997 | 15.0 |
| 32 | Prevalence of COPD in Spain: impact of undiagnosed COPD on quality of life and daily life activities | 323 | 2009 | 32.3 |
| 33 | A 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterol | 323 | 2002 | 19.0 |
| 34 | Health outcomes following treatment for six months with once daily tiotropium compared with twice daily salmeterol in patients with COPD | 317 | 2003 | 19.8 |
| 35 | Roflumilast—an oral anti-inflammatory treatment for chronic obstructive pulmonary disease: a randomised controlled trial | 315 | 2005 | 22.5 |
| 36 | Analysis of the factors related to mortality in chronic obstructive pulmonary disease—Role of exercise capacity and health status | 314 | 2003 | 19.6 |
| 37 | Interpreting thresholds for a clinically significant change in health status in asthma and COPD | 313 | 2002 | 18.4 |
| 38 | Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: A randomized trial | 308 | 2000 | 16.2 |
| 39 | Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study | 299 | 2004 | 19.9 |
| 40 | Phosphodiesterase-4 inhibitors for asthma and chronic obstructive pulmonary disease | 298 | 2005 | 21.3 |
Note: * The inhaled steroids in obstructive lung disease in Europe (ISOLDE).
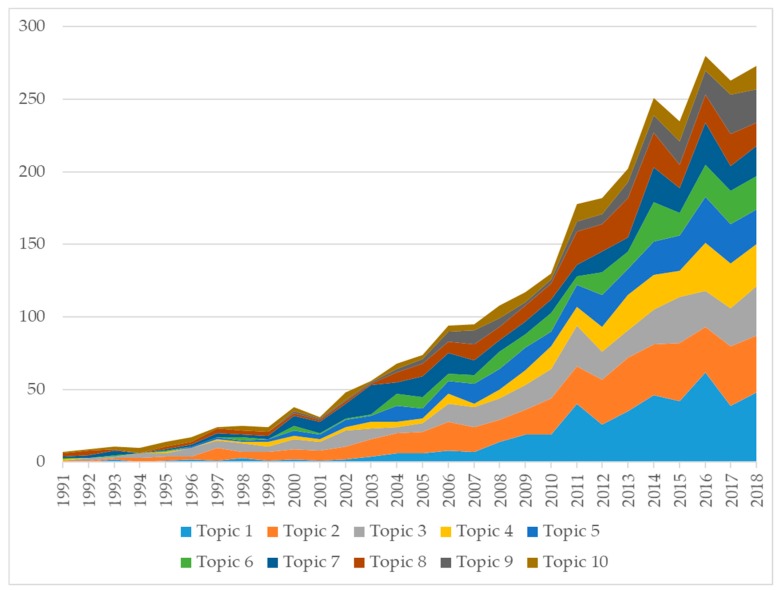
Applying latent dirichlet allocation in title and abstracts, ten major research topics were formed (Table 4). Topic 2 (n = 468 papers), Topic 1 (n = 436 papers), and topic 3 (n = 355 papers) were three topics with the highest volume of publications. Pulmonary rehabilitation has been a rapidly developed field in the last decades [49]. Further, improving QoL of patients living with COPD by pharmacological therapies (topic 6) or non-pharmacological therapies (topic 3, topic 10) has been a major area of focus. Notably, the domain of mental health received frequent attention from the scientific community with 436 papers. The reason for it could be that about 85% of people living with COPD were at high risk of developing anxiety disorders compared with healthy people [50].
Table 4.
Research topics classified by LDA.
| Rank by the Highest Volume | Research Topics | N | Percent |
|---|---|---|---|
| Topic 2 | Pulmonary rehabilitation for COPD | 468 | 16.30% |
| Topic 1 | Comorbidities, mental health and QoL in COPD patients | 436 | 15.20% |
| Topic 3 | QoL of patients with COPD: validity of questionnaire | 355 | 12.40% |
| Topic 5 | Predictors for mortality due to acute exacerbation of COPD | 287 | 10.00% |
| Topic 7 | Pharmacological Therapy and COPD | 272 | 9.50% |
| Topic 8 | Management of COPD | 257 | 9.00% |
| Topic 4 | Multicomponent interventions: home care, rehabilitation, self-care education, integrated care, and pharmacy-led management | 255 | 8.90% |
| Topic 6 | Perception and QoL of patients living with COPD and their caregivers | 217 | 7.60% |
| Topic 10 | Noninvasive Ventilation and Oxygen Therapy in patient with COPD | 160 | 5.60% |
| Topic 9 | COPD Phenotype and quality of life | 157 | 5.50% |
Figure 3 shows the changes in the development of topics. Topic 1 in the last five years (2014–2018) had the highest number of published papers (n = 237), followed by topic 2 (n = 186) and topic 3 (n = 141).
Figure 3.
Changes in research topics development.
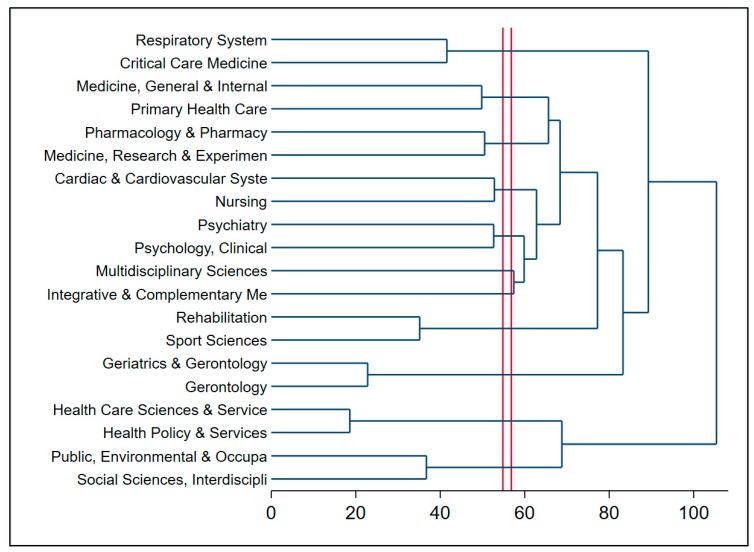
Figure 4 shows the cluster of research areas in QoL of patients with COPD. The horizontal axis represents the distance between clusters, while the vertical axis displays the research areas [51]. The red lines show the depth for the cut-off of the analysis [52]. Research landscapes were divided into three main parts. The root (first group) in the top of the dendrogram included (a) respiratory system and (b) critical care medicine. This cluster had a close relationship with (1) intervention and health care such as general & internal medicine, pharmacy, nursing, and cardiovascular system (second group); (2) comorbidities, for instance, psychiatry, clinical psychology, clinical neurology (third group). However, the first group did not have a strong relatedness to the cluster in the bottom, such as rehabiliation or the integration of public health, environmental and occupational health (health care science & services; health policy & services, occupational &public, environment, interdiscriplinary social sciences).
Figure 4.
Dendrogram of coincidence of research areas.
4. Discussion
This study investigated the global trend of 3242 research publications regarding interventions to increase QoL of patients with COPD. It was found that the publications of research related to in topic increased annually and gradually, and most of the contribution came from high income countries (HICs). Mental health issues and non-pharmacological therapy, including exercise, home care, self-care education, noninvasive ventilation, and oxygen therapy were common approaches. Current findings emphasize the importance of research that focuses on the effects of non-pharmacological therapy, which should be considered to increase QoL of people living with COPD. Additionally, mental health problems among people living with COPD have received more focus, especially in the last five years.
Notably, but unsurprisingly, a high number of research were conducted by authors from HICs than that of LMICs although more than 90% of COPD-related deaths occur in LMICs [53]. This work supports the conclusion of previous studies, which confirmed the main contribution of HICs in diabetes research [54] or HIV/AIDS research [55]. This phenomenon may be explained by the fact that risk factor prevention has not been fully recognized by the LMICs’ governments and populations, including using biomass fuels indoors for cooking [56] or occupational exposure [57]. Moreover, many LMICs faced the barriers in research and implication planning, such as information and communication technology limitations [58], lack of human resources and finance, and scientific findings [59]. Therefore, the support of HICs and actively joining in collaboration network with HICs are critical to LMICs [60].
Chronic obstructive pulmonary disease is a chronic disorder, which requires a long-term treatment with complementary and alternative therapy to reduce exacerbation and improve patients’ QoL [61]. Our finding were in line with the results of previous studies, which emphasized that pharmacological therapy [62], exercise [63], non-invasive ventilation [64], and oxygen therapy [65] increase the QoL of people living with COPD. In our study, the number of papers mentioning pharmacological treatment was in the top five of highest volume of work by LDA. It showed the concern of researchers and physicians on this therapy to control the symptoms in stable COPD as well as improve QoL of people suffered COPD. It confirmed the results of some papers which emphasize the effectiveness of pharmacotherapy in controlling symptoms to decrease recurrence and seriousness of exacerbations and improve QoL [66,67]. However, this topic rose at a lower level in the last five years compared with non-pharmacy therapies, such as mental health, or rehabilita. The results might be explained by the efficiency of the alternative therapies in improving the quality of life, controlling symptoms in daily life and when exacerbations occur [68], and reducing the frequency of hospitalization [69].
Furthermore, the topics receiving the most attention in the last five years were comorbidities and mental health issues in patients with COPD. A previous study showed that about one-third of patients living with COPD with depression or anxiety did not received appropriate treatment [50]. The comorbid condition of mental illness can increase the risk of exacerbations, reduce QoL, and raise the chance of mortality [70,71]. Thus, mental health illness should receive further piority, which may help to increase QoL among patients living with COPD [72].
The results provide some evidence to enhance designing interventions, health research, and policy. Most of the death cases related to COPD happened in LMICs, yet, most of the studies were conducted in HICs. The health research capacity in LMICs is lower than that of HICs could be explained by (1) the limitation of infrastructure and capacity [73], (2) a lack of investment funding in universities and research institutions, low wages for researchers [74], and (3) a lack of clear national research priorities [74]. Therefore, LMICs need to (1) actively create collaboration research networks with HICs and (2) prepare the national research priorities under the circumstance of understanding the local context. Moreover, the LMICs’ national health research priorities should be considered when international organizations or donors from HICs invest in LMICs. Secondly, we call for multidisciplinary collaboration of researchers and physicians among research areas, especially between psychological and respiratory physiologists since the complexity of this disease and negatives effects of depression and anxiety to patients with COPD.
Several limitations of this study should be mentioned. Firstly, WOS was the only database used in the analysis. However, for a large number of papers for analysis, there was a high possibility that these articles were in other databases, including PubMed and Scopus. Secondly, only English publications were included. Thus, it was more likely that our study did not reflect the trend in COPD research where English is not used. Finally, only titles and abstracts were used for topic modeling. However, by applying a different level of data and alternative method, the trends and hidden themes of the research studies could be discovered [74].
5. Conclusions
The findings of the study show that the interventions to increase QoL of patients with COPD has attracted increasing research interest in the last two decades. Non-pharmacological therapy and mental health problems were two common approaches. In addition, increasing support from HICs to LMICs in research together with the multidisciplinary collaboration of research areas are needed to improve the QoL of people living with COPD in LMICs.
Appendix A
Table A1.
Search query for “Quality of life” and “well-being”.
| No | Search Query | Search Result |
|---|---|---|
| # 1 | TS = (“quality of life”) | 355,541 |
| # 2 | TS = (“well-being”) | 104,048 |
| # 3 | #2 OR #1 | 441,617 |
| # 4 | #2 OR #1 | 437,253 |
| Refined by: [excluding] Publication Years: (2019) | ||
| # 5 | #2 OR #1 | 353,171 |
| Refined by: [excluding] Publication Years: (2019) AND [excluding] Document Types: ( Meeting Abstract Or Proceedings Paper Or Editorial Material Or Book Chapter Or Letter Or Book Review Or Correction Or Note Or News Item Or Book Or Reprint Or Early Access Or Retracted Publication Or Biographical Item Or Correction Addition Or Discussion Or Data Paper Or Retraction Or Bibliography Or Fiction Creative Prose Or Item About An Individual Or Poetry Or Software Review) | ||
| # 6 | #2 OR #1 | 353,170 |
| Refined by: [excluding] Publication Years: (2019) AND [excluding] Document Types: ( Meeting Abstract Or Proceedings Paper Or Editorial Material Or Book Chapter Or Letter Or Book Review Or Correction Or Note Or News Item Or Book Or Reprint Or Early Access Or Retracted Publication Or Biographical Item Or Correction Addition Or Discussion Or Data Paper Or Retraction Or Bibliography Or Fiction Creative Prose Or Item About An Individual Or Poetry Or Software Review ) AND [excluding] Document Types: (Tv Review Radio Review) | ||
| # 7 | #2 OR #1 | 327,627 |
| Refined by: [excluding] Publication Years: (2019) AND [excluding] Document Types: (Meeting Abstract Or Proceedings Paper Or Editorial Material Or Book Chapter Or Letter Or Book Review Or Correction Or Note Or News Item Or Book Or Reprint Or Early Access Or Retracted Publication Or Biographical Item Or Correction Addition Or Discussion Or Data Paper Or Retraction Or Bibliography Or Fiction Creative Prose Or Item About An Individual Or Poetry Or Software Review) AND [excluding] Document Types: (Tv Review Radio Review) AND [excluding]Languages: (German Or Spanish Or French Or Portuguese Or Russian Or Turkish Or Polish Or Italian Or Korean Or Czech Or Hungarian Or Croatian Or Greek Or Dutch Or Japanese Or Slovenian Or Slovak Or Lithuanian Or Serbian Or Persian Or Malay Or Romanian Or Chinese Or Icelandic Or Arabic Or Afrikaans Or Norwegian Or Ukrainian Or Danish Or Catalan Or Swedish Or Estonian Or Bulgarian Or Serbo Croatian Or Galician Or Georgian Or Esperanto Or Finnish Or Hebrew Or Indonesian Or Welsh) | ||
| # 8 | AU = (“Anonymous” OR “anonymous”) | 1,406,800 |
| # 9 | #7 NOT #8 | 327,405 |
Figure A1.
Selection of papers.
Author Contributions
Conceptualization, G.V.V., G.H.H., H.Q.P., C.A.L. and R.C.M.H.; Data curation, G.H.H., C.T.N. and H.Q.P.; Formal analysis, G.H.H., C.T.N., G.T.V., H.Q.P. and B.X.T.; Investigation, G.V.V., B.X.T. and C.S.H.H.; Methodology, G.H.H., C.T.N. and B.X.T.; Project administration, G.T.V. and C.S.H.H.; Software, C.T.N.; Supervision, G.V.V., C.A.L. and B.X.T.; Validation, G.V.V., C.A.L., R.C.M.H. and C.S.H.H.; Writing—original draft, G.H.H., G.V.V.and H.Q.P.; Writing—review & editing, G.V.V., C.A.L. and R.C.M.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.World Health Organization Chronic obstructive pulmonary disease: Definition. [(accessed on 12 July 2019)]; Available online: https://www.who.int/respiratory/copd/definition/en/
- 2.OECD/EUROPEAN UNION 2016 . Health at a Glance: Europe 2016–State of Health in the EU Cycle. OECD Publishing; Paris, France: 2016. Asthma and COPD prevalence. [DOI] [Google Scholar]
- 3.Group R.C.W. COPD prevalence in 12 Asia–Pacific countries and regions: Projections based on the COPD prevalence estimation model. Respirology. 2003;8:192–198. doi: 10.1046/j.1440-1843.2003.00460.x. [DOI] [PubMed] [Google Scholar]
- 4.National Center for Chronic Disease Prevention and Health Promotion COPD Prevalence in the United States. [(accessed on 12 July 2019)]; Available online: https://www.cdc.gov/copd/data.html.
- 5.Mehrotra A., Akanbi M.O., Gordon S.B. The burden of COPD in Africa: A literature review and prospective survey of the availability of spirometry for COPD diagnosis in Africa. Trop. Med. Int. Health TM IH. 2009;14:840–848. doi: 10.1111/j.1365-3156.2009.02308.x. [DOI] [PubMed] [Google Scholar]
- 6.Adeloye D., Basquill C., Papana A., Chan K.Y., Rudan I., Campbell H. An estimate of the prevalence of COPD in Africa: A systematic analysis. Copd J. Chronic Obstr. Pulm. Dis. 2015;12:71–81. doi: 10.3109/15412555.2014.908834. [DOI] [PubMed] [Google Scholar]
- 7.Peruzza S., Sergi G., Vianello A., Pisent C., Tiozzo F., Manzan A., Coin A., Inelmen E., Enzi G. Chronic obstructive pulmonary disease (COPD) in elderly subjects: Impact on functional status and quality of life. Respir. Med. 2003;97:612–617. doi: 10.1053/rmed.2003.1488. [DOI] [PubMed] [Google Scholar]
- 8.Agusti À., Soriano J.B. COPD as a systemic disease. Copd J. Chronic Obstr. Pulm. Dis. 2008;5:133–138. doi: 10.1080/15412550801941349. [DOI] [PubMed] [Google Scholar]
- 9.Agusti A., Calverley P.M., Celli B., Coxson H.O., Edwards L.D., Lomas D.A., MacNee W., Miller B.E., Rennard S., Silverman E.K. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir. Res. 2010;11:122. doi: 10.1186/1465-9921-11-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Restrepo M.I., Sibila O., Anzueto A. Pneumonia in patients with chronic obstructive pulmonary disease. Tuberc. Respir. Dis. (Seoul) 2018;81:187–197. doi: 10.4046/trd.2018.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaouat A., Naeije R., Weitzenblum E. Pulmonary hypertension in COPD. Eur. Respir. J. 2008;32:1371–1385. doi: 10.1183/09031936.00015608. [DOI] [PubMed] [Google Scholar]
- 12.Quint J. The Relationship between COPD and Cardiovascular Disease. Tanaffos. 2017;16:S16–S17. [PMC free article] [PubMed] [Google Scholar]
- 13.Maurer J., Rebbapragada V., Borson S., Goldstein R., Kunik M.E., Yohannes A.M., Hanania N.A., Anxiety A.W.P.O., Depression C. Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest. 2008;134:43S–56S. doi: 10.1378/chest.08-0342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim H.F.S., Kunik M.E., Molinari V.A., Hillman S.L., Lalani S., Orengo C.A., Petersen N.J., Nahas Z., Goodnight-White S. Functional impairment in COPD patients: The impact of anxiety and depression. Psychosomatics. 2000;41:465–471. doi: 10.1176/appi.psy.41.6.465. [DOI] [PubMed] [Google Scholar]
- 15.Spruit M.A., Vercoulen J.H., Sprangers M.A.G., Wouters E.F.M. Fatigue in COPD: An important yet ignored symptom. Lancet Respir. Med. 2017;5:542–544. doi: 10.1016/S2213-2600(17)30158-3. [DOI] [PubMed] [Google Scholar]
- 16.Franssen F.M.E., Smid D.E., Deeg D.J.H., Huisman M., Poppelaars J., Wouters E.F.M., Spruit M.A. The physical, mental, and social impact of COPD in a population-based sample: Results from the Longitudinal Aging Study Amsterdam. NPJ Prim. Care Respir. Med. 2018;28:30. doi: 10.1038/s41533-018-0097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Price D., Small M., Milligan G., Higgins V., Gil E.G., Estruch J. Impact of night-time symptoms in COPD: A real-world study in five European countries. Int. J. Chron. Obs. Pulmon. Dis. 2013;8:595. doi: 10.2147/COPD.S48570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stephenson J.J., Cai Q., Mocarski M., Tan H., Doshi J.A., Sullivan S.D. Impact and factors associated with nighttime and early morning symptoms among patients with chronic obstructive pulmonary disease. Int. J. Chron. Obs. Pulmon. Dis. 2015;10:577. doi: 10.2147/COPD.S76157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization WHOQOL: Measuring Quality of Life. [(accessed on 21 April 2020)]; Available online: https://www.who.int/healthinfo/survey/whoqol-qualityoflife/en/
- 20.Gandhi S.K., Kong S.X. Quality-of-life measures in the evaluation of antihypertensive drug therapy: Reliability, validity, and quality-of-life domains. Clin. Ther. 1996;18:1276–1295. doi: 10.1016/S0149-2918(96)80082-8. [DOI] [PubMed] [Google Scholar]
- 21.Taylor S.H. Drug therapy and quality of life in angina pectoris. Am. Heart J. 1987;114:234–240. doi: 10.1016/0002-8703(87)90971-9. [DOI] [PubMed] [Google Scholar]
- 22.Wright E.K., Kamm M.A. Impact of drug therapy and surgery on quality of life in Crohn‘s disease: A systematic review. Inflamm. Bowel Dis. 2015;21:1187–1194. doi: 10.1097/MIB.0000000000000271. [DOI] [PubMed] [Google Scholar]
- 23.Benzo R.P., Abascal-Bolado B., Dulohery M.M. Self-management and quality of life in chronic obstructive pulmonary disease (COPD): The mediating effects of positive affect. Patient Educ. Couns. 2016;99:617–623. doi: 10.1016/j.pec.2015.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tran B.X., Harijanto C., Vu G.T., Ho R.C. Global Mapping of Interventions to improve Quality of Life using Mind-body therapies during 1990–2018. Complementary Ther. Med. 2020;49:102350. doi: 10.1016/j.ctim.2020.102350. [DOI] [PubMed] [Google Scholar]
- 25.Hawthorne G., Richardson J., Osborne R. The Assessment of Quality of Life (AQoL) instrument: A psychometric measure of health-related quality of life. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 1999;8:209–224. doi: 10.1023/A:1008815005736. [DOI] [PubMed] [Google Scholar]
- 26.Feldman G.J. Improving the quality of life in patients with chronic obstructive pulmonary disease: Focus on indacaterol. Int. J. Chron. Obs. Pulmon. Dis. 2013;8:89. doi: 10.2147/COPD.S31209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Godtfredsen N.S., Lam T.H., Hansel T.T., Leon M., Gray N., Dresler C., Burns D., Prescott E., Vestbo J. COPD-related morbidity and mortality after smoking cessation: Status of the evidence. Eur. Respir. J. 2008;32:844–853. doi: 10.1183/09031936.00160007. [DOI] [PubMed] [Google Scholar]
- 28.Zamarro C.G., Bernabé M.B., Santamaría B.R., Rodríguez J.H. Smoking in COPD. Arch. De Bronconeumol. 2011;47:3–9. [Google Scholar]
- 29.Antus B. Pharmacotherapy of Chronic Obstructive Pulmonary Disease: A Clinical Review. ISRN Pulmonol. 2013;2013:11. doi: 10.1155/2013/582807. [DOI] [Google Scholar]
- 30.Safka K.A., McIvor R.A. Non-pharmacological management of chronic obstructive pulmonary disease. Ulst. Med. J. 2015;84:13–21. [PMC free article] [PubMed] [Google Scholar]
- 31.Ahn E., Kang H. Introduction to systematic review and meta-analysis. Korean J. Anesth. 2018;71:103–112. doi: 10.4097/kjae.2018.71.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gregersen T.L., Green A., Frausing E., Ringbæk T., Brøndum E., Suppli Ulrik C. Do telemedical interventions improve quality of life in patients with COPD? A systematic review. Int. J. Chron. Obs. Pulmon. Dis. 2016;11:809–822. doi: 10.2147/COPD.S96079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coronini-Cronberg S., Heffernan C., Robinson M. Effective smoking cessation interventions for COPD patients: A review of the evidence. JRSM Short Rep. 2011;2:1–12. doi: 10.1258/shorts.2011.011089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Papadopoulos G., Vardavas C.I., Limperi M., Linardis A., Georgoudis G., Behrakis P. Smoking cessation can improve quality of life among COPD patients: Validation of the clinical COPD questionnaire into Greek. BMC Pulm. Med. 2011;11:13. doi: 10.1186/1471-2466-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ubolnuar N., Tantisuwat A., Thaveeratitham P., Lertmaharit S., Kruapanich C., Mathiyakom W. Effects of Breathing Exercises in Patients With Chronic Obstructive Pulmonary Disease: Systematic Review and Meta-Analysis. Ann. Rehabil. Med. 2019;43:509–523. doi: 10.5535/arm.2019.43.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alvarez G.R., Vanz S.A.S., Barbosa M.C. Scientometric indicators for Brazilian research on High Energy Physics, 1983–2013. An. Da Acad. Bras. De Ciências. 2017;89:2525–2543. doi: 10.1590/0001-3765201720160620. [DOI] [PubMed] [Google Scholar]
- 37.Begum M., Lewison G., Wright J.S., Pallari E., Sullivan R. European non-communicable respiratory disease research, 2002–2013: Bibliometric study of outputs and funding. PLoS ONE. 2016:11. doi: 10.1371/journal.pone.0154197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sweileh W.M., Al-Jabi S.W., Sa′ed H.Z., Sawalha A.F. Bronchial asthma and chronic obstructive pulmonary disease: Research activity in Arab countries. Multidiscip. Respir. Med. 2014;9:38. doi: 10.1186/2049-6958-9-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martín-Martín A., Orduna-Malea E., Delgado López-Cózar E. Coverage of highly-cited documents in Google Scholar, Web of Science, and Scopus: A multidisciplinary comparison. Scientometrics. 2018;116:2175–2188. doi: 10.1007/s11192-018-2820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Clarivate Analytics Web of Science databases. [(accessed on 26 June 2019)]; Available online: https://clarivate.com/products/web-of-science/databases/
- 41.Li Y., Rapkin B., Atkinson T.M., Schofield E., Bochner B.H. Leveraging Latent Dirichlet Allocation in processing free-text personal goals among patients undergoing bladder cancer surgery. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2019 doi: 10.1007/s11136-019-02132-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valle D., Albuquerque P., Zhao Q., Barberan A., Fletcher R.J., Jr. Extending the Latent Dirichlet Allocation model to presence/absence data: A case study on North American breeding birds and biogeographical shifts expected from climate change. Glob. Chang. Biol. 2018;24:5560–5572. doi: 10.1111/gcb.14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen C., Zare A., Trinh H.N., Omotara G.O., Cobb J.T., Lagaunne T.A. Partial Membership Latent Dirichlet Allocation for Soft Image Segmentation. IEEE Trans. Image Process. A Publ. IEEE Signal. Process. Soc. 2017;26:5590–5602. doi: 10.1109/TIP.2017.2736419. [DOI] [PubMed] [Google Scholar]
- 44.Lu H.M., Wei C.P., Hsiao F.Y. Modeling healthcare data using multiple-channel latent Dirichlet allocation. J. Biomed. Inform. 2016;60:210–223. doi: 10.1016/j.jbi.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 45.Gross A., Murthy D. Modeling virtual organizations with Latent Dirichlet Allocation: A case for natural language processing. Neural Netw. Off. J. Int. Neural Netw. Soc. 2014;58:38–49. doi: 10.1016/j.neunet.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 46.Rabe K.F., Hurd S., Anzueto A., Barnes P.J., Buist S.A., Calverley P., Fukuchi Y., Jenkins C., Rodriguez-Roisin R., van Weel C., et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization . Global Status Report on Noncommunicable Diseases 2014. World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 48.Global Initiative for Chronic Obstructive Lung Disease . Global Strategy for the Diagnosis, Management, and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease, Inc.; Fontana, WI, USA: 2019. [Google Scholar]
- 49.Troosters T., Gosselink R., Janssens W., Decramer M. Exercise training and pulmonary rehabilitation: New insights and remaining challenges. Eur. Respir. Rev. 2010;19:24–29. doi: 10.1183/09059180.00007809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yohannes A.M., Alexopoulos G.S. Depression and anxiety in patients with COPD. Eur. Respir. Rev. 2014;23:345–349. doi: 10.1183/09059180.00007813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.STATA Cluster Dendrogram—Dendrograms for Hierarchical Cluster Analysis. [(accessed on 22 April 2020)]; Available online: https://www.stata.com/manuals13/mvclusterdendrogram.pdf.
- 52.Moffat D., Ronan D., Reiss J.D. Unsupervised taxonomy of sound effects. Context. 2017;6:7. [Google Scholar]
- 53.Laniado-Laborin R. Smoking and chronic obstructive pulmonary disease (COPD). Parallel epidemics of the 21 century. Int. J. Environ. Res. Public Health. 2009;6:209–224. doi: 10.3390/ijerph6010209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tran B.X., Nguyen L.H., Pham N.M., Vu H.T.T., Nguyen H.T., Phan D.H., Ha G.H., Pham H.Q., Nguyen T.P., Latkin C.A. Global Mapping of Interventions to Improve Quality of Life of People with Diabetes in 1990–2018. Int. J. Environ. Res. Public Health. 2020;17:1597. doi: 10.3390/ijerph17051597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vu G.T., Tran B.X. Global Research on Quality of Life of Patients with HIV/AIDS: Is It Socio-Culturally Addressed? (GAP(RESEARCH)) Int. J. Environ. Res. Public Health. 2020;17:2127. doi: 10.3390/ijerph17062127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Torres-Duque C., Maldonado D., Perez-Padilla R., Ezzati M., Viegi G. Biomass fuels and respiratory diseases: A review of the evidence. Proc. Am. Thorac. Soc. 2008;5:577–590. doi: 10.1513/pats.200707-100RP. [DOI] [PubMed] [Google Scholar]
- 57.Pleasants R.A., Riley I.L., Mannino D.M. Defining and targeting health disparities in chronic obstructive pulmonary disease. Int. J. Chron. Obs. Pulmon. Dis. 2016;11:2475–2496. doi: 10.2147/COPD.S79077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bezuidenhout L., Chakauya E. Hidden concerns of sharing research data by low/middle-income country scientists. Glob. Bioeth. Probl. Di Bioet. 2018;29:39–54. doi: 10.1080/11287462.2018.1441780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ritchie L.M.P., Khan S., Moore J.E., Timmings C., van Lettow M., Vogel J.P., Khan D.N., Mbaruku G., Mrisho M., Mugerwa K. Low-and middle-income countries face many common barriers to implementation of maternal health evidence products. J. Clin. Epidemiol. 2016;76:229–237. doi: 10.1016/j.jclinepi.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 60.Nuwayhid I.A. Occupational health research in developing countries: A partner for social justice. Am. J. Public Health. 2004;94:1916–1921. doi: 10.2105/AJPH.94.11.1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Viniol C., Vogelmeier C.F. Exacerbations of COPD. Eur. Respir. Rev. 2018;27:170103. doi: 10.1183/16000617.0103-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Montuschi P. Pharmacological treatment of chronic obstructive pulmonary disease. Int. J. Chron. Obs. Pulmon. Dis. 2006;1:409. doi: 10.2147/copd.2006.1.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xu Y., Wang J., Li H., Zhu X., Wang G. Efficacy of integrative respiratory rehabilitation training in exercise ability and quality of life of patients with chronic obstructive pulmonary disease in stable phase: A randomized controlled trial. Zhong Xi Yi Jie He Xue Bao J. Chin. Integr. Med. 2010;8:432–437. doi: 10.3736/jcim20100506. [DOI] [PubMed] [Google Scholar]
- 64.Díaz-Lobato S., Alises S.M., Rodríguez E.P. Current status of noninvasive ventilation in stable COPD patients. Int. J. Chron. Obs. Pulmon. Dis. 2006;1:129–135. doi: 10.2147/copd.2006.1.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Murphy P.B., Rehal S., Arbane G., Bourke S., Calverley P.M.A., Crook A.M., Dowson L., Duffy N., Gibson G.J., Hughes P.D., et al. Effect of Home Noninvasive Ventilation With Oxygen Therapy vs Oxygen Therapy Alone on Hospital Readmission or Death After an Acute COPD Exacerbation: A Randomized Clinical Trial. JAMA. 2017;317:2177–2186. doi: 10.1001/jama.2017.4451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Institute for Health and Care Excellence . Chronic Obstructive Pulmonary Disease in over 16s: Diagnosis and Management Evidence Reviews for Self Management, Education and Telehealth. National Institute for Health and Care Excellence; London, UK: 2018. [PubMed] [Google Scholar]
- 67.Zwerink M., Brusse-Keizer M., van der Valk P.D., Zielhuis G.A., Monninkhof E.M., van der Palen J., Frith P.A., Effing T. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2014 doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smith M.C., Wrobel J.P. Epidemiology and clinical impact of major comorbidities in patients with COPD. Int. J. Chron. Obs. Pulmon. Dis. 2014;9:871. doi: 10.2147/COPD.S49621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cavaillès A., Brinchault-Rabin G., Dixmier A., Goupil F., Gut-Gobert C., Marchand-Adam S., Meurice J.-C., Morel H., Person-Tacnet C., Leroyer C. Comorbidities of COPD. Eur. Respir. Rev. 2013;22:454–475. doi: 10.1183/09059180.00008612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Australian Institute of Health and Welfare COPD, associated Comorbidities and Risk Factors. [(accessed on 17 June 2019)]; Available online: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/copd-associated-comorbidities-risk-factors/contents/about-copd-and-associated-comorbidities.
- 71.Khanal P. Bringing all together for research capacity building in LMICs. Lancet Glob. Health. 2017;5:e868. doi: 10.1016/S2214-109X(17)30259-0. [DOI] [PubMed] [Google Scholar]
- 72.ESSENCE on Health Research . Seven Principle for Strengthening Research Capacity in Low-and-middle-income Countries: Simple Ideas in a Complex World. TDR/World Health Organization; Geneva, Switzerland: 2014. [Google Scholar]
- 73.Ali N., Hill C., Kennedy A., IJsselmuiden C.C. What Factors Influence National Health Research Agendas in Low and Middle Income Countries? Council on Health Research for Development (COHRED); Geneva, Switzerland: 2006. COHRED Record Paper 5. [Google Scholar]
- 74.Wang H., Wu F., Lu W., Yang Y., Li X., Li X., Zhuang Y. Identifying Objective and Subjective Words via Topic Modeling. IEEE Trans. Neural Netw. Learn. Syst. 2018;29:718–730. doi: 10.1109/TNNLS.2016.2626379. [DOI] [PubMed] [Google Scholar]