Abstract
Background and objective
The optimal timing for initiation of dabigatran after acute ischaemic stroke (AIS) is not established. We aimed to evaluate initiation timing and clinical outcomes of dabigatran in AIS patients with non-valvular atrial fibrillation (NVAF).
Design
Retrospective study based on prospectively collected data in SITS (Safe Implementation of Treatment in Stroke) Thrombolysis and Thrombectomy Registry from July 2014 to July 2018.
Participants
European NVAF patients (≥18 years) hospitalised after first-ever ischaemic stroke.
Setting
A multinational, observational monitoring register.
Intervention
Dabigatran initiation within 3 months after the ischaemic stroke.
Primary and secondary outcomes
The primary outcome was time from first-ever ischaemic stroke (index event) to dabigatran initiation. Additional outcomes included physicians’ reasons for delaying dabigatran initiation beyond acute hospital discharge and outcomes within 3 months of index event.
Methods
We identified patients with NVAF who received dabigatran within 3 months of the index event. We performed descriptive statistics for baseline and demographic data and clinical outcomes after dabigatran initiation.
Results
In total, 1489 patients with NVAF received dabigatran after AIS treated with thrombolysis and/or thrombectomy. Of these, 1240 had available initiation time. At baseline, median age was 75 years; 53% of patients were women, 15% were receiving an oral anticoagulant, 29% acetylsalicylic acid and 4% clopidogrel. Most patients (82%) initiated dabigatran within 14 days after the index event. Patients initiating earlier had lower stroke severity from median NIHSS 8 (IQR 6–13) if initiated within 7 days to NIHSS 15 (9–19) if initiated between 28 days and 3 months. Most common reasons for delaying initiation were haemorrhagic transformation or intracranial haemorrhage, stroke severity and infarct size. Few thrombotic/haemorrhagic events occurred within 3 months after the index event (20 of 926 patients, 2.2% with the available data).
Conclusions
Our findings, together with previous observational studies, indicate that dabigatran initiated within the first days after an AIS is safe in patients treated with intravenous thrombolysis, endovascular thrombectomy or both.
Trial registration number
SITS Thrombolysis and Thrombectomy Registry (NCT03258645).
Keywords: anticoagulation, adult cardiology, stroke
Strengths and limitations of this study.
This study shows real-world clinical practice in a wide range of centres and countries.
To the best of our knowledge, this is the first study of dabigatran for secondary stroke prevention in patients treated with reperfusion therapies.
The study is observational and based on a retrospective analysis of an ongoing database, with all the limitations of this type of study design.
Another limitation is that we are only reporting cases deemed by participating clinicians to be eligible for oral anticoagulation for secondary prevention.
Introduction
Cardioembolic stroke, the most severe ischaemic stroke subtype, related mostly to non-valvular atrial fibrillation, accounts for 13%–26% of all ischaemic strokes.1 Its recurrence rate within the first 14 days without anticoagulation is around 5%.2 Anticoagulation using heparin decreases the risk of ischaemic stroke recurrence to 3.0%, but at the cost of 1.8% increase risk of the absolute risk of intracranial bleeding.3 Meanwhile, the rate of ischaemic stroke recurrence may decrease to as low as 2.8% within 90 days when a direct oral anticoagulant (DOAC) is prescribed.4 For clinicians, the decision on when to initiate anticoagulation after an acute ischaemic stroke (AIS) is still a challenge, mainly due to perceived risk of early intracerebral haemorrhage.
The latest Cochrane systematic review in 2015 concluded that early anticoagulant therapy is not associated with net short-term or long-term benefit in patients with AIS.5 Moreover, neither national nor international stroke guidelines give firm recommendations. The American Heart Association-American Stroke Assciation (AHA-ASA) 2018 guidelines state that starting oral anticoagulation (OAC) within 4–14 days after AIS is reasonable for most patients, and the European Society of Cardiology 2016 and European Heart Rhythm Association 2018 guidelines, endorsed by the European Stroke Organisation, recommend starting OAC 1, 3, 6 and 12 days, respectively, after transient ischaemic attack, minor, moderate and severe strokes.6–8
Clinical practice is, therefore, to delay anticoagulation by up to 14 days. As the risk of recurrence during this time is around 5%, many clinicians initiate anticoagulation earlier, guided by the approximate size of the infarct and the absence or the presence of any haemorrhagic transformation.
The lower overall risk of intracranial haemorrhage (ICH) with DOACs compared with vitamin K antagonists (VKA) may facilitate earlier anticoagulation using DOACs in these patients.9 Recent observational studies indicate that the risk of symptomatic ICH in patients treated with DOACs within the first 5 days of ischaemic stroke is low.10–12 A pooled individual patient data analysis of seven observational studies concluded that DOACs started early after AIS were associated with reduced risk of poor clinical outcomes compared with VKA, mainly due to lower risk of ICH.13
Regarding dabigatran, patients were randomised in the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial no sooner than 14 days after AIS.14 More recently, a smaller trial, including 301 patients with Transient Ischemic Attack (TIA) or minor ischaemic stroke (NIHSS <9), showed that dabigatran and aspirin had similar safety with a non-significant trend for fewer early recurrent ischaemic strokes in the dabigatran arm.15 16
The optimal timing of anticoagulation after an AIS is not established, and until results of ongoing randomised controlled trials are published, observational studies are needed to provide recommendations for clinical practice.
The primary aim of this observational study was to evaluate the timing of dabigatran initiation in AIS patients with NVAF treated with intravenous thrombolysis (IVT), endovascular thrombectomy (EVT) or both. Secondary aims were (1) to report physicians’ reasons to delay OAC and (2) to evaluate clinical outcomes at 3-month follow-up.
Material and methods
Patients presenting with first-ever AIS and NVAF recorded in the Safe Implementation of Treatment in Stroke-Atrial Fibrillation (SITS-AF) registry between July 2014 and July 2018 were included.
The SITS-AF registry is a subset of the Safe Implementation of Treatment in Stroke-International Stroke Thrombolysis Registry (SITS-ISTR), an ongoing, prospective, academic-driven and multinational, register for clinical centres treating patients with acute stroke. The methodology of the SITS-ISTR, including procedures for data collection and management, patient identification and verification of source data has been described previously.17
In the present study, patients were included if they presented with stroke symptoms and were treated with intravenous alteplase (Actilyse, Boehringer Ingelheim, Ingelheim, Germany) within or outside license criteria, and/or with endovascular thrombectomy (EVT). Need for ethical approval or patient consent for participation in the SITS-ISTR varied among participating countries. Ethics approval and patient consent were obtained in countries that required this; other countries approved the register for conduct as an anonymised audit.
We collected baseline and demographic characteristics, premorbid modified Rankin Scale (mRS), variables required for CHA2DS2-VASc and HAS-BLED scores, stroke severity as per the NIHSS, medication history, imaging data at admission and follow-up, time interval in days between index event and start of dabigatran and physicians’ reasons for delaying dabigatran initiation beyond acute hospital discharge. Follow-up period for this study was 3 months, during which we collected information on any new clinical events, functional outcome using the mRS and death. All assessments of imaging studies, neurological status and functional status were done according to clinical routine at centres participating in the SITS-ISTR.
Outcomes
The primary outcome was the time from index event (first-ever ischaemic stroke) to dabigatran initiation. Secondary outcomes included physicians’ reasons for delaying dabigatran initiation beyond acute hospital discharge and clinical outcomes of interest within 3 months of the index event. Clinical outcomes of interest include death, stroke or systemic embolism, ICH or major bleeding defined according to the International Society on Thrombosis and Hemostasis, all within 3 months after the index event.18 The timing of initiation was at the discretion of the treating physicians.
Statistical analysis
We performed descriptive statistics for baseline, imaging and demographic data. For continuous variables, median and IQR and mean and SD values were obtained. For categorical variables, we calculated percentage proportions by dividing the number of events by the total number of patients, excluding missing or unknown cases.16 Comparisons were made using Mann-Whitney U test and χ2 test as appropriate. Pearson correlation coefficient was used to correlate dabigatran initiation time with continuous variables. A multivariable regression model, including potential confounders (clinically relevant variables and variables based on a univariate significance of p<0.05), was used to establish association between baseline variables and dabigatran initiation time. Because of the low number of events, no inferential analysis was performed. To calculate annualised incidence rates, we calculated the number of patient-years (number of included patients multiplied by the follow-up time in years). Incidence rates were expressed per 100 person-years. The 95% CIs for incidence rates were calculated using Fisher’s exact test.
Patient and public involvement
Patients or the public were not involved in the design, conduct, reporting or dissemination plans of our research.
Results
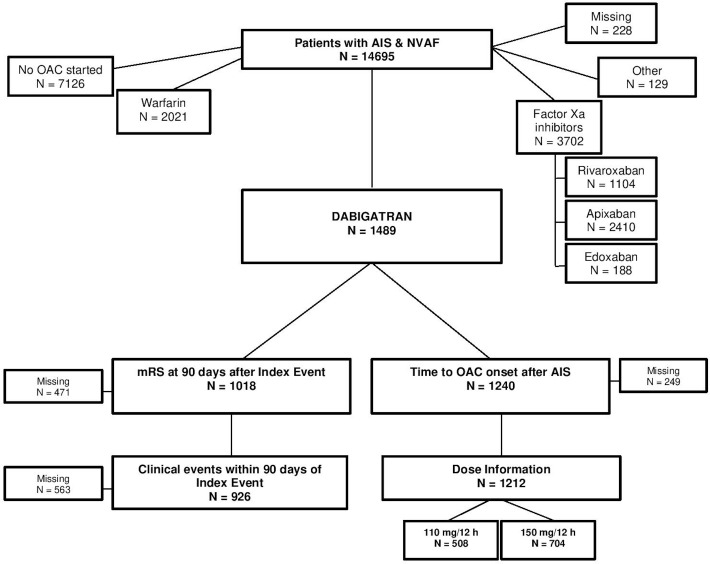
The dataset comprised 14 695 patients with first-ever AIS and NVAF, diagnosed either before the stroke or within 3 months after the event. Of these, 1489 patients received dabigatran treatment for secondary prevention. The information regarding dabigatran initiation timing was available in 1240 patients, who were the study population for primary outcome (figure 1). Baseline and demographic characteristics in aggregate are presented in table 1. Baseline characteristics according to time of dabigatran initiation are presented in online supplementary table I. The median age was 75 (69–82) years; 656 (53%) patients were women. The median NIHSS at admission was 10 (6–16). The median time from index stroke to dabigatran initiation was 8 (4–12) days. About 82% of patients initiated dabigatran within 14 days after the index stroke (online supplementary figure 1).
Figure 1.
Flowchart of the study.
Table 1.
Baseline characteristics of dabigatran patients included in the study
| Dabigatran patients with available time of initiation (n=1240) | |
| Age (mean, SD) (median, IQR) | 75±10 (69–82) |
| Gender (N, %, female) | 656 (52.9) |
| NIHSS baseline (median, IQR) | 10 (6–16) |
| SBP (mm Hg, mean, SD) | 153±23 |
| DBP (mm Hg, mean, SD) | 85±15 |
| Glucose (mmol/dL, mean, SD) | 7.3±2.3 |
| Weight (kg, mean, SD) | 78±15 |
| Hypertension (N, %) | 955 (77) |
| Diabetes (N, %) | 216 (17.4) |
| Hyperlipidemia (N, %) | 349 (28.1) |
| Previous TIA (N, %) | 65 (5.3) |
| Current smoker (N, %) | 88 (7.1) |
| Previous smoker (N, %) | 107 (8.8) |
| Congestive heart failure (N, %) | 134 (10.9) |
| Vascular disease (N, %) | 149 (12) |
| Renal impairment (N, %) | 30 (2.6) |
| Abnormal liver function (N, %) | 16 (1.4) |
| Alcohol use (N, %) | 37 (3.2) |
| History of/predisposition to bleeding (N, %) | 30 (2.6) |
| Labile INR (N, %) | 39 (3.5) |
| Previous AF (N,%) | 720 (58.6) |
| Previous modified Rankin Scale (median, IQR) | 0 (0–0) |
| Previous CHA2DS2-VASc (mean) (median, IQR) |
3.1 3 (2–4) |
| Previous HAS-BLED (mean) (median, IQR) |
1.7 1 (1–2) |
| CHA2DS2-VASc discharge (mean) (median, IQR) |
5.1 5 (4–6) |
| HAS-BLED discharge (mean) (median, IQR) |
2.7 3 (2–3) |
| IVT (N, %) | 1055 (85.1) |
| EVT (N, %) | 68 (5.5) |
| IVT+EVT (N, %) | 117 (9.4) |
AF, atrial fibrillation; DBP, diastolic blood pressure; EVT, endovascular thrombectomy; INR, International Normalised Ratio; IVT, intravenous thrombolysis; NIHSS, National Institutes of Health Stroke Scale; SBP, systolic blood pressure; TIA, Transient Ischemic Attack.
bmjopen-2020-037234supp001.pdf (50.8KB, pdf)
bmjopen-2020-037234supp002.pdf (37.9KB, pdf)
Univariate analysis showed that higher NIHSS at baseline and higher pre-stroke mRS were associated with a delay of dabigatran initiation (p<0.001 and p<0.01, respectively). Multivariate regression analysis, including clinically significant variables (age, gender, baseline NIHSS, systolic blood pressure on admission and glucose level at admission) showed that older age (p=0.02), higher diastolic blood pressure on admission (p=0.002), higher previous CHA2DS2-VASc score (p=0.04) and a history of/predisposition to bleeding (p=0.03), were independently associated with a delay of dabigatran initiation.
Reasons for delaying anticoagulation
Regarding reasons for delaying dabigatran initiation beyond the period of acute hospitalisation, a total of 268 reasons were reported in 203 patients (1 reason in 160 patients, more than one in 43). Table 2 shows the distribution of physician responses. Of all reasons given, 65.3% were related to the index event, the most frequent being stroke severity (22.8%), size of infarct (19.4%) and haemorrhagic transformation (14.9%).
Table 2.
Distribution of physician reasons to delay dabigatran initiation until after discharge from acute stroke care
| Reasons for delay | N | % |
| Severity of stroke | 61 | 22.8 |
| Size of infarct | 52 | 19.4 |
| Haemorrhagic transformation | 40 | 14.9 |
| Intracranial haemorrhage | 8 | 3.0 |
| Reason not specified | 27 | 10.1 |
| Patient bleeding risk factors | 18 | 6.7 |
| Location of infarct | 14 | 5.2 |
| Practical considerations | 14 | 5.2 |
| Intervention used to treat ischaemic stroke | 8 | 3.0 |
| Patient stroke risk factors | 6 | 2.2 |
| Recommendation from specialist | 6 | 2.2 |
| Altered coagulation parameters | 5 | 1.9 |
| Other reasons | 5 | 1.9 |
| Patient preference | 4 | 1.5 |
| Total | 268 | 100 |
Follow-up
In total, 926 patients had available information at 3-month follow-up regarding clinical events since discharge, resulting in a cumulative follow-up time of 231.5 patient-years. Of these 926 patients, the information about the primary outcome (timing of dabigatran initiation) was only available for 702 patients.
Among 926 patients, 101 experienced at least 1 event, with a total of 107 events reported. Of these, 20 (2.2%) were considered events of interest (embolism or haemorrhage, defined as new stroke, myocardial infarct, pulmonary embolism or systemic embolism, as well as ICH and major extracranial haemorrhage). Thirteen of these events were embolic/ischaemic (seven new stroke since discharge (3.02%/year, 95% CI 1.22 to 6.23), three myocardial infarction, two pulmonary embolism and one systemic embolism) and seven were haemorrhagic (one ICH (0.43%/year, 95% CI 0.01 to 2.13) and six major extracranial haemorrhage). There were no differences in the distribution of events of interest and initiation time.
The data on mRS at 3 months after the index event were available in 1018 patients. A total of 697 patients (68.5%) were functionally independent (mRS: 0–2), and 31 (3%) had died. The causes of death were recorded as follows: 10 (32%) due to index cerebral infarction, 1 (3.2%) patient due to ICH, 2 (6.5%) patients due to pneumonia, 2 (6.5%) patients due to pulmonary embolism, 6 (19.4%) patients due to other causes and 10 (32%) patients had an unknown cause.
Tables 3 and 4 show comparisons of our results with previously reported observational studies. Patients in our study were older and had a higher stroke severity. Our findings regarding events of interest are in line with those previously reported.
Table 3.
Comparison of our results with previous observational studies of NOACs with 90 days of follow-up
| Dabigatran SITS (n=1240) |
NOACISP (all patients; n=204) |
Gioia et al
19
(n=60) |
SAMURAI (NOACs; n=475) |
RAF-NOAC (dabigatran group; n=381) |
|
| Median/mean* age | 76 (69–82) | 79 (73–84) | 73.5±13.2* | 74.4±9.2* | 73.6±9.9* |
| Median/mean* NIHSS (at admission) |
10 (6–16) | 4 (2–8) | 2 (0–4) at rivaroxaban initiation | 4 (1–13) | 7.7±6.2* |
| Median delay (days) | 8 (4–12) | 5 (3–11) (dabigatran group) | 3 (1.5–6) | 4 (2–7) | 8 (3–14) |
* Mean and SD
NIHSS, National Institutes of Health Stroke Scale; NOACISP, Novel Oral Anticoagulants in Stroke Patients; RAF-NOAC, Early Recurrence and Major Bleeding in Patients With Acute Ischemic Stroke and Atrial Fibrillation Treated With Non–Vitamin K Oral Anticoagulants; SITS, Safe Implementation of Treatment in Stroke.
Table 4.
Comparison of our results with dabigatran-treated patients from a previous observational study with 90 days of follow-up
| Dabigatran (n=926) |
RAF-NOAC (dabigatran; n=381) |
|
| All safety events | 20 (2.2%) | 9 (2.4%) |
| Embolism | 13 (1.4%) | 7 (1.8%) |
| Stroke/TIA | 7 (0.8%) | 7 (1.8%) |
| Other thromboembolic events (MI, PE or SE) | 6 (0.7%) | 0 |
| Major haemorrhage | 7 (0.8%) | 2 (0.5%) |
| Intracranial haemorrhage | 1 (0.1%) | 2 (0.5%) |
MI, Myocardial Infarction; PE, Pulmonary Embolism; RAF-NOAC, Early Recurrence and Major Bleeding in Patients With Acute Ischemic Stroke and Atrial Fibrillation Treated With Non–Vitamin K Oral Anticoagulants; SE, Systemic Embolism; TIA, Transient Ischemic Attack.
Discussion
This large observational study shows that dabigatran in clinical practice is most commonly initiated early (82% patients within first 14 days) after an AIS. The rate of ischaemic or haemorrhagic complications during the first 3 months after early initiation of dabigatran is low. Our findings suggest that the safety profile of dabigatran for secondary stroke prevention in clinical practice is similar to findings in the RE-LY trial.14
We have compared our results with those in recently published observational studies (tables 3 and 4). At a median age of 76, the patients in our series were older than in other studies, with the exception of the Novel Oral Anticoagulants in Stroke Patients (NOACISP).10–12 19 Importantly, our patients had a much higher stroke severity than those in previous publications due to the fact that they received intravenous and/or endovascular reperfusion therapies, median NIHSS 10 in our patients versus 2–7 in previous observational studies.10–12 19 The higher NIHSS and older age likely had a major influence on our finding that dabigatran was initiated at median 8 days, compared with 2–4 days in previous studies.10 11 19 Both stroke severity and reperfusion treatment are associated with an elevated haemorrhagic risk. In spite of this, the rate of large parenchymal hematoma (PH2-PHr2) in our study was 1% compared with 2.7%–5.1% previously reported in IVT patients and the rate of ICH within 3 months from the index event was even lower, 0.1%, compared with 5.1% at 90 days in a meta-analysis of EVT.20–22 However, these findings should be interpreted with caution due to potential selection bias, as patients with early severe symptomatic bleeding after acute treatment may have died, or if alive, may have been too severely disabled to be considered for OAC initiation—potentially removing bleeding-prone patients from the treatment-eligible population.
According to the RAF-NOAC (Early Recurrence and Major Bleeding in Patients With Acute Ischemic Stroke and Atrial Fibrillation Treated With Non–Vitamin K Oral Anticoagulants) study, the period of DOAC initiation with the lowest rates of ischaemic recurrence and major bleeding events would be 3–14 days after the index event (2.1% for composite AIS, TIA, symptomatic systematic embolism and major bleeding).12 Although our numbers of events were too low for significance testing between periods, the period with the lowest rate of safety events was 3–7 days after AIS (1.7% for composite AIS, TIA, symptomatic systematic embolism and major bleeding). When comparing safety events in our study and the dabigatran subgroup of RAF-NOAC, the rate of the composite outcome is similar (2.2% vs 2.4%), but in our series the rates of stroke for TIA and ICH were lower.
Our study adds new data to the recent observational studies regarding anticoagulation after AIS. This literature together with guideline recommendations and patients’ individual embolic and haemorrhagic risks should guide the decision on when to start OAC therapy.
We have described physicians’ reasons to delay anticoagulation. Previous registry studies have shown an underutilisation of OAC both in primary prevention and after AIS.23–25 Several reasons could explain this: lack of knowledge of current guidelines, physician’s concern for the risk of bleeding and clinical factors, such as poor functional outcome after stroke, advanced age or the risk of falling. In our study, reasons for the delay of dabigatran initiation were mostly related to the index event and its putative high haemorrhagic risk.26
Our study has some limitations. The main one is that it only includes patients treated with IVT and/or EVT. Thus, there is a matter of selection of cases eligible for such therapies (whether treated on-label or off-label and within or outside guidelines). These cases are likely to have more severe strokes and may have a lower pre-morbid score on mRS and other differences, compared with an unselected NVAF stroke population. Another limitation is that 16% of patients initiating dabigatran within 3 months from the index event had no available information on exact initiation timing. A sensitivity analysis (online supplementary table II) comparing clinical characteristics between patients with and without known initiation time showed that the latter group had higher NIHSS and glucose levels at baseline, less frequent history of previous AF and more frequently had endovascular treatment. These differences could potentially have biased our results to some extent in favour of earlier dabigatran initiation. Moreover, we are only reporting cases deemed by participating clinicians to be eligible for OAC treatment. In four cases of events of interest, the information about dabigatran initiation timing was not available, but sensitivity analysis has been performed under different distribution assumptions and showed no statistical significance regarding time initiation groups.
The strengths of our study are that it shows real-world clinical practice in a wide range of centres and countries, in which the timing of OAC was not standardised across the study but left to the discretion of the individual physicians and centres. It is also, to the best of our knowledge, the first study of dabigatran for secondary stroke prevention in patients treated with IVT and/or EVT, a population in which there may be even more controversy about when to start OAC due to a potentially elevated risk of haemorrhage. In addition, our data add important safety information on dabigatran, as the population in this study was not included in the pivotal dabigatran trial RE-LY (patients with a recent acute stroke were excluded).
Four large randomised controlled trials, OPTIMAS (OPtimal TIMing of Anticoagulation After Acute Ischaemic Stroke : a Randomised Controlled Trial) (EudraCT, 2018-003859-38; UK), TIMING (TIMING of Oral Anticoagulant Therapy in Acute Ischemic Stroke With Atrial Fibrillation) (NCT02961348; Sweden), START (Optimal Delay Time to Initiate Anticoagulation After Ischemic Stroke in Atrial Fibrillation) (NCT03021928; USA) and ELAN (Early versus Late initiation of direct oral Anticoagulants in post-ischaemic stroke patients with atrial fibrillation) (NCT03148457; Switzerland) are investigating the benefit of early DOAC administration in patients with AF-related ischaemic stroke. The results of these trials are expected in the coming years; in the meantime, clinicians have to rely on data from observational studies.
Conclusions
Our findings, together with previous observational studies, suggest that dabigatran initiated within the first days after AIS is safe in patients treated with IVT, EVT or both.
Supplementary Material
Acknowledgments
The authors would like to thank the SITS Registry Investigators and patients.
Footnotes
Contributors: MM and NA were involved in protocol development. MM and IE-M were involved in data analysis. IE-M and NA wrote the first draft of the manuscript. CT, NL, ZG, LB, WF, MK, AK, GK, APN, KP, AP, PS, AV and DT reviewed and edited the manuscript and approved the final version of the manuscript.
Funding: This study is sponsored by Boehringer-Ingelheim. In addition, the SITS registry is financed directly and indirectly by grants from Karolinska Institutet, Stockholm County Council, the Swedish Heart-Lung Foundation, the Swedish Order of St. John, Friends of Karolinska Institutet, private donors as well as from an unrestricted sponsorship from Boehringer-Ingelheim. SITS has previously received grants from the European Union Framework 7, the European Union Public Health Authority and Ferrer International, EVER Pharma. SITS is currently conducting studies supported by Boehringer-Ingelheim as well as in collaboration with Karolinska Institutet supported by Stryker, Covidien and Phenox. IE-M has received a grant from 'Fundación Progreso y Salud, Junta de Andalucía' (grant EF-0437-2018).
Competing interests: NA is chair of SITS International, which receives a grant from Boehringer Ingelheim for the SITS-ISTR. MM is International Network and Research Executive at SITS International, which receives a grant from Boehringer Ingelheim for the SITS-ISTR.
Ethics approval: Data collection in this study was done within the framework of SITS-MOST II study, which was approved by the Stockholm Ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Seiffge DJ, Werring DJ, Paciaroni M, et al. Timing of anticoagulation after recent ischaemic stroke in patients with atrial fibrillation. Lancet Neurol 2019;18:117–26. 10.1016/S1474-4422(18)30356-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Saxena R, Lewis S, Berge E, et al. Risk of early death and recurrent stroke and effect of heparin in 3169 patients with acute ischemic stroke and atrial fibrillation in the International stroke trial. Stroke 2001;32:2333–7. 10.1161/hs1001.097093 [DOI] [PubMed] [Google Scholar]
- 3. Paciaroni M, Agnelli G, Micheli S, et al. Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials. Stroke 2007;38:423–30. 10.1161/01.STR.0000254600.92975.1f [DOI] [PubMed] [Google Scholar]
- 4. Paciaroni M, Agnelli G, Falocci N, et al. Early recurrence and major bleeding in patients with acute ischemic stroke and atrial fibrillation treated with Non-Vitamin-K oral anticoagulants (RAF-NOACs) study. J Am Heart Assoc 2017;6:e007034. 10.1161/JAHA.117.007034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sandercock PAG, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev 2015:CD000024. 10.1002/14651858.CD000024.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart Association/American stroke association. Stroke 2018;49:e46–110. 10.1161/STR.0000000000000158 [DOI] [PubMed] [Google Scholar]
- 7. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;39:2893–962. [DOI] [PubMed] [Google Scholar]
- 8. Steffel J, Verhamme P, Potpara TS, et al. The 2018 European heart rhythm association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J 2018;39:1330–93. 10.1093/eurheartj/ehy136 [DOI] [PubMed] [Google Scholar]
- 9. Ntaios G, Papavasileiou V, Diener H-C, et al. Nonvitamin-K-antagonist oral anticoagulants in patients with atrial fibrillation and previous stroke or transient ischemic attack: a systematic review and meta-analysis of randomized controlled trials. Stroke 2012;43:3298–304. 10.1161/STROKEAHA.112.673558 [DOI] [PubMed] [Google Scholar]
- 10. Seiffge DJ, Traenka C, Polymeris A, et al. Early start of DOAC after ischemic stroke: risk of intracranial hemorrhage and recurrent events. Neurology 2016;87:1856–62. 10.1212/WNL.0000000000003283 [DOI] [PubMed] [Google Scholar]
- 11. Arihiro S, Todo K, Koga M, et al. Three-month risk-benefit profile of anticoagulation after stroke with atrial fibrillation: the SAMURAI-Nonvalvular atrial fibrillation (NVAF) study. Int J Stroke 2016;11:565–74. 10.1177/1747493016632239 [DOI] [PubMed] [Google Scholar]
- 12. Paciaroni M, Agnelli G, Falocci N, et al. Early recurrence and major bleeding in patients with acute ischemic stroke and atrial fibrillation treated with non-vitamin-K oral anticoagulants (RAF-NOACs) study. J Am Heart Assoc 2017;6:e007034. 10.1161/JAHA.117.007034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Seiffge DJ, Paciaroni M, Wilson D, et al. DOAC vs VKA after recent ischemic stroke in patients with atrial fibrillation. Ann Neurol 2019;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Diener H-C, Connolly SJ, Ezekowitz MD, et al. Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: a subgroup analysis of the RE-LY trial. Lancet Neurol 2010;9:1157–63. 10.1016/S1474-4422(10)70274-X [DOI] [PubMed] [Google Scholar]
- 15. Ng KH, Sharma M, Benavente O, et al. Dabigatran following acute transient ischemic attack and minor stroke II (DATAS II). Int J Stroke 2017;12:910–4. 10.1177/1747493017711947 [DOI] [PubMed] [Google Scholar]
- 16. Butcher K, Ng K, Field T. The dabigatran following acute transient ischemic attack and minor stroke trial: final results. Eur Stroke J 2018;3 3 (abstr). [DOI] [PubMed] [Google Scholar]
- 17. Wahlgren N, Ahmed N, Dávalos A, et al. Thrombolysis with alteplase for acute ischaemic stroke in the safe implementation of thrombolysis in Stroke-Monitoring study (SITS-MOST): an observational study. Lancet 2007;369:275–82. 10.1016/S0140-6736(07)60149-4 [DOI] [PubMed] [Google Scholar]
- 18. Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692–4. 10.1111/j.1538-7836.2005.01204.x [DOI] [PubMed] [Google Scholar]
- 19. Gioia LC, Kate M, Sivakumar L, et al. Early rivaroxaban use after cardioembolic stroke may not result in hemorrhagic transformation: a prospective magnetic resonance imaging study. Stroke 2016;47:1917–9. 10.1161/STROKEAHA.116.013491 [DOI] [PubMed] [Google Scholar]
- 20. Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014;384:1929–35. 10.1016/S0140-6736(14)60584-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mazya MV, Lees KR, Collas D, et al. IV thrombolysis in very severe and severe ischemic stroke: results from the SITS-ISTR registry. Neurology 2015;85:2098–106. 10.1212/WNL.0000000000002199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016;387:1723–31. 10.1016/S0140-6736(16)00163-X [DOI] [PubMed] [Google Scholar]
- 23. Mazurek M, Shantsila E, Lane DA, et al. Guideline-adherent antithrombotic treatment improves outcomes in patients with atrial fibrillation: insights from the community-based Darlington atrial fibrillation registry. Mayo Clin Proc 2017;92:1203–13. 10.1016/j.mayocp.2017.05.023 [DOI] [PubMed] [Google Scholar]
- 24. Gundlund A, Xian Y, Peterson ED, et al. Prestroke and poststroke antithrombotic therapy in patients with atrial fibrillation: results from a nationwide cohort. JAMA Netw Open 2018;1:1–12. 10.1001/jamanetworkopen.2018.0171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Groot AE, Vermeij J-DM, Westendorp WF, et al. Continuation or discontinuation of anticoagulation in the early phase after acute ischemic stroke. Stroke 2018;49:1762–5. 10.1161/STROKEAHA.118.021514 [DOI] [PubMed] [Google Scholar]
- 26. Álvarez-Sabín J, Maisterra O, Santamarina E, et al. Factors influencing haemorrhagic transformation in ischaemic stroke. Lancet Neurol 2013;12:689–705. 10.1016/S1474-4422(13)70055-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-037234supp001.pdf (50.8KB, pdf)
bmjopen-2020-037234supp002.pdf (37.9KB, pdf)