Abstract
Debate continues in the medical literature on the role of the renin angiotensin system (RAS) in Coronavirus disease 2019 (COVID-19) pathophysiology and the implications for the use of cardiovascular drugs acting on the RAS. Could these drugs – which include angiotensin converting enzyme inhibitors (ACEIs) and angiotensin receptors blockers (ARBs) – be harmful or potential key therapeutic agents in COVID-19? And, could potentially helpful measures be available and in plain view on the pharmacy shelf?
Keywords: COVID 19, Renin angiotensin system, Angiotensin converting enzyme inhibitors, Angiotensin receptor blockers, Neprilysin, Vitamin D
Debate has arisen due to the finding that underlying cardiovascular disease and hypertension are associated with significantly increased risk of hospitalisation and death in COVID-19 [1,2], in addition to the viral receptor being angiotensin-converting enzyme-2 (ACE-2) [[3], [4], [5]]. Coronaviruses down-regulate ACE-2 anti-inflammatory actions leading to imbalance in ACE:ACE-2 [4] which may be fundamental in COVID-19 pathophysiology. Key gender and genetic differences in the regulation of ACE:ACE-2 balance [[6], [7], [8]] may explain differences observed in disease severity [2,9,10].
Social media amplification of concern about continuation of renin angiotensin system (RAS) medications during the current pandemic prompted cardiovascular societies to publish position statements strongly advising continued use, given a lack of evidence that RAS drugs were unsafe and the substantial risk of hospitalisation when these drugs are withdrawn from patients with valid indications for treatment [11,12]. Three (3) large observational studies published in The New England Journal of Medicine (NEJM) now support the view that there is no evidence for harm due to RAS medications in COVID-19 [10,13,14].
However, given the fundamental role of the RAS in COVID-19, a broader therapeutic indication for ACEI and ARBs, over and above treatment of patients with established cardiovascular indications has been suggested [15,16] but is yet to be tested in randomised trials. Vitamin D status may also be linked to the RAS impacts of COVID-19, as vitamin D is a negative regulator of renin synthesis, and a small study has reported high rates of vitamin D deficiency in COVID patients requiring intensive care [17]. Both vitamin D and ACE have a role in the immune system, which may add a complex dimension to the issue of RAS drugs and vitamin D status in COVID-19 [18,19].
COVID-19 has a more severe course in patients with pre-existing cardiovascular disease [1,2,10] and causes a significant rate of cardiovascular events [20]. Further research is required to define the pathological mechanisms and the basis for the observed gender, age, and racial differences in severity. RAS medications can be used with greater confidence in COVID-19 patients with valid indications for their use, but a broader role for manipulation of the RAS in COVID-19 will require randomised trial data.
Role of the RAS in Coronavirus Infection
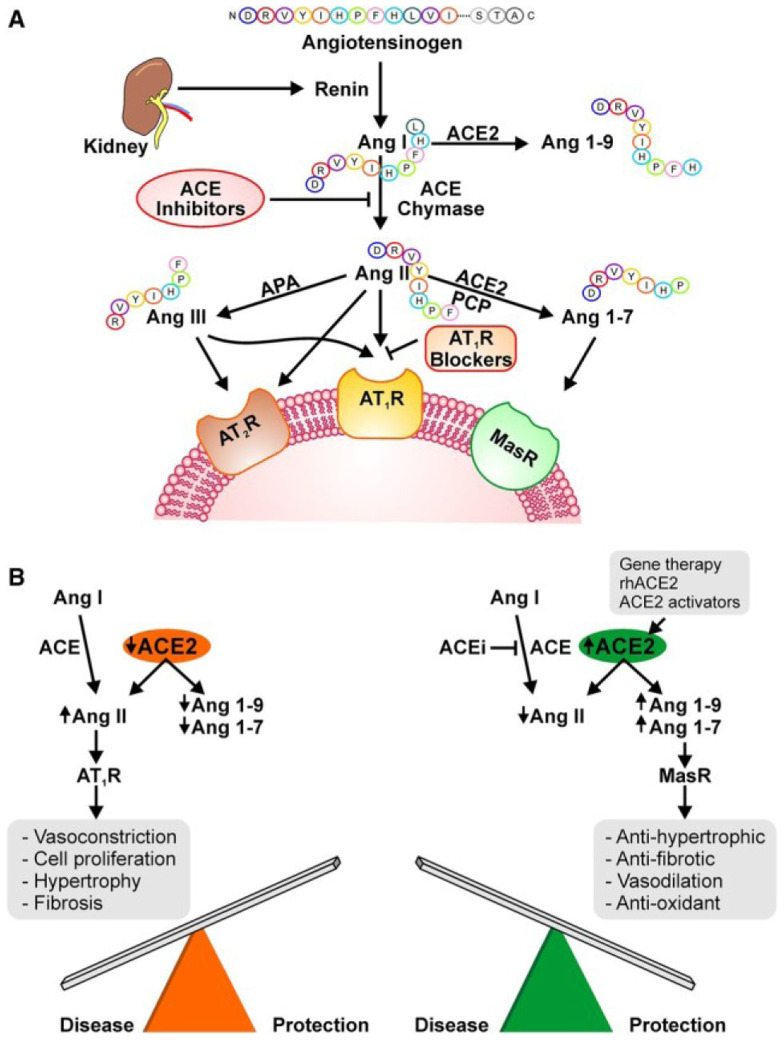
Coronavirus-2 (SARS-CoV-19) is believed to gain cell entry via a viral spike protein binding to the ACE-2 receptor [3,4]. Virology research for other similar coronaviruses indicates that viral cell infection is followed by rapid downregulation of ACE-2 [4,5]. The ACE-2 system is the yang of the yin-yang balance of the RAS hypertension system. ACE-2 is a zinc metalloprotease, discovered in 2000 [21], which mainly breaks down angiotensin II (Ang II), the main effector of the RAS system, to Ang(1-7), resulting in a decrease in blood pressure, vasoconstriction and decreased inflammation. ACE-2 is usually membrane bound but is shed in COVID infection, in acute lung injury and myocardial infarction [16]. Whilst the role of circulating ACE-2 is unclear, conditions such as advanced heart failure have higher plasma ACE-2 proportional to worsening clinical status [22,23]. Serum ACE-2 levels are also significantly higher in hypertensive patients [23] and gender differences are described with up to 50% greater levels in male patients [23]. There is debate as to whether the observed higher levels in male, hypertensive, and diabetic patients are related to increased ACE-2 expression as a compensatory mechanism, or whether it is due to increased ACE-2 shedding, limiting tissue ACE-2 activity and causing excess tissue Ang II. The role of circulating, versus tissue, ACE-2 levels in susceptibility to COVID infection is unclear [24]. In viral downregulation of ACE-2, unopposed ACE generates high Ang II causing increased BP, vasoconstriction, inflammation and cell damage. To exacerbate matters, the active metabolite generated by ACE-2, Ang(1-7), can be broken down by ACE itself, accentuating the RAS imbalance caused by COVID-19 [21] (Figure 1 ).
Figure 1.
Renin angiotensin system showing the balance between angiotensin converting enzyme (ACE) and ACE-2.
Diagram from Patel et al. Circ Res 2016 [21].
COVID-19 Pandemic
COVID-19 is highly contagious spreading from one province, in December 2019, to the whole of China in 30 days, despite extreme shutdown measures [2]. By May 2020, the disease has infected 3,392,718 people with 239,178 deaths worldwide [9] and is causing enormous global economic and social impacts. Epidemiology for 72,314 confirmed, suspected and asymptomatic cases in China suggested mild disease in 81%, with 2.3% fatality overall [2]. Early mortality figures in different countries have shown striking differences, with greater mortality in Europe, compared to Asian countries [9], which may relate to fundamental differences in racial ACE and ACE-2 polymorphisms, impacting both susceptibility to the disease and subsequent pathological severity. Population demographics clearly play a role with elderly patients at greatest risk of severe disease and death. Key differences in the speed of government actions to implement extensive public health measures, as recommended by the World Health Organization (WHO), have also impacted mortality rates as hospitals in some countries have been overwhelmed by a rapid rise in cases.
Factors Influencing Disease Severity
Why do 81% of cases have a mild disease and yet 19% have a more severe disease? The Chinese Center for Disease Control and Prevention (CCDC) epidemiology showed that there was an overall mortality of 2.3% [2]. The death rate increased with age and with co-morbidities, particularly cardiovascular disease (13.2%), diabetes (9.2%) and hypertension (8.4%), all the risk factors typically seen in those with “metabolic syndrome”. Whilst it is clear that co-morbidities and age increase mortality, what is not clear is whether this excess is due to the impact of the co-morbid conditions on host inflammatory response alone, or to the impact of a treatment some of this patient group is taking [25]. Since the RAS system is fundamentally involved in COVID-19 pathogenesis, there was great speculation that drugs widely used in hypertension and heart failure treatment, acting on the RAS, may impact disease severity, with some suggesting a protective effect [15,16] and others concerned about potential harm [24]. These drugs include ARBs, ACEIs and the combination drug valsartan/sacubitril (Entresto) which combines an ARB with a neprilysin inhibitor (also known as an angiotensin receptor-neprilysin inhibitor [ARNI]). Whilst there is evidence that ACEI and ARB treatment may increase expression of ACE-2 in some tissues in animal models, data supporting or quantifying this effect in human subjects at clinical doses of RAS medications is lacking [24]. Hence the relevance of possible medication-induced alteration in ACE-2 levels, over and above the well-described significant differences in circulating levels of ACE-2 in advanced heart failure, hypertension, males and diabetics, and the implications for COVID-19 severity, is unclear [22,23,25]. Increased ACE-2 was speculated to increase susceptibility to COVID-19 by allowing more virus into cells which, in turn, may exacerbate disease severity. The counter argument is that, once infected, having more ACE-2 could be protective against viral attack and downregulation of the ACE-2 anti-inflammatory system [26,27]. Three (3) large observational studies reported in the NEJM have now examined this issue and found no evidence for increased risk of adverse outcomes in COVID-19 patients taking ACEI or ARBs [10,13,14] adding weight to previously reported smaller retrospective clinical studies [[28], [29], [30]] which also showed no excess mortality for ACEI/ARBs. Mehra et al. [10] reported data for 8,910 patients admitted with COVID-19 in 169 hospitals in Europe, Asia and North America, and confirmed that age, coronary disease, heart failure, cardiac arrhythmia, chronic obstructive pulmonary disease and current smoking were all associated with increased in-hospital mortality but there was no increased risk of mortality associated with risk of ACEI or ARBs. They did find that use of ACEI and statins was more common in survivors, however this was not randomised data. A multicentre Chinese study of 1,128 hospitalised patients with COVID-19 and pre-existing hypertension showed a death rate of 3.7% in those on ACEI or ARB versus 9.8% in non-users (p=0.03). The data was observational and not randomised, but even after adjustment for confounding variables a lower mortality, with a hazard ratio of 0.37 (p=0.03) persisted for those receiving ACEI/ARBs, with a HR of 0.3 (p=0.03) compared to use of other antihypertensive agents [28]. The study did not separate treatment with ARBs from ACEI [29].
Polymorphisms of ACE and ACE-2 Impacting RAS Balance
The answer to observed differences in COVID-19 death rates could lie in key differences in the ACE:ACE-2 system balance related to age, gender and racial variation in genetic ACE and ACE-2 polymorphisms and environmental factors influencing ACE-2 expression [6,31]. There are ACE gene polymorphisms that cause insertion (I) or deletion (D) of a sequence of the gene, and ACE activity levels in DD carriers are approximately twice that found in II genotypes [7]. The possible impact of ACE genotype in the COVID-19 disease state, when the ability to breakdown Ang II is impaired, could be hypothesised to cause a greater quantity of circulating Ang II and a more marked imbalance of the RAS and more severe disease. Genetic and environmental factors influencing ACE-2 expression could also result in differences in the risk of becoming infected in the first place by affecting the affinity of the ACE-2 binding domain for the viral spike protein and by causing differences in the density of ACE-2 receptors present in tissues such as the lungs. ACE-2 polymorphisms may then contribute to significant differences in disease severity by determining the extent of the ACE:ACE2 imbalance, particularly in the endothelium of the lungs, where the virus attacks at the same time as disabling the ACE2-mediated repair systems.
Chen and co-workers (2020) [8] have analysed 30 tissues in thousands of individuals and found significantly higher tissue ACE-2 in Asian females compared to males and other ethnic groups. They have described an age-dependent decrease in ACE-2 expression and a highly significant decrease in type II diabetic patients. The loci for higher ACE-2 expression is almost 100% in East Asians and >30% higher than other ethnic groups. ACE-2 is suppressed by inflammatory cytokines, by diabetes and induced by oestrogen and androgen, both of which are decreased in the elderly. The work by Chen and co-workers suggests a negative correlation between COVID-19 mortality and tissue ACE-2 levels, at both a population and molecular level [8]. Circulating ACE-2, however, has been described to increase in pathological states such as hypertension, diabetes and heart failure and perhaps differences in circulating, shed ACE-2 and tissue-bound ACE-2 are key in virus susceptibility and subsequent disease severity.
Gender Differences in ACE-2
ACE-2 is on the X chromosome, hence men have only one allele and women have two [6,31]. Further to this, oestrogen is believed to upregulate ACE-2 expression [32], giving pre-menopausal women the advantage of two alleles and oestrogen upregulation, making a deficiency of ACE-2 and its ability to rally less likely in the event of a viral attack. In support of this hypothesis, the Chinese CDCC reported overall female mortality of 1.7% including suspected cases as well as serologically confirmed cases versus 2.8% in males. This difference was more marked in serologically confirmed cases, 2.8% female versus 4.7% male mortality. The overall ratio was 1.06 males to 1.0 females believed infected [2]. Hence the men were not significantly less likely to become infected, just more likely to have a more severe pathophysiological expression of the disease. Whilst the WHO suggested [9] that these gender differences may be driven by substantially greater rates of smoking in the Chinese male population, the rates of smoking in the COVID-19 cases were not provided in the epidemiological study. The X-linked nature of the ACE2 gene, with females having a greater range of phenotypes, may have a greater role than has been yet been fully defined in coronavirus pathogenesis gender differences. The range of ACE-2 phenotypes and their ability to upregulate compensatory mechanisms in the face of viral ACE-2 downregulation may play a role. Marked gender differences in disease have been confirmed in other large observational studies with Marcia et al. reporting 37% women in 6,232 patients with COVID and Mehra et al. reported 40% female patients in 8,910 COVID-19 patients requiring hospital admission and furthermore reported improved survival in female patients, independent of older age [10].
Serum ACE-2 levels are reported to be significantly lower in females [23] and there are fundamental differences in immune responses to viral infections based on gender with stronger humoral and cellular immune responses described in females [33].
Smoking and COVID-19
Smoking has been linked to upregulation of ACE and downregulation of ACE-2 [34], which could be hypothesised to make smokers less likely than the general population to become infected by virtue of having less ACE-2 required for viral entry. However, if a smoker becomes infected, a pre-existing ACE:ACE-2 imbalance may result in more severe disease due to greater inflammation, higher risk of ARDS and multi-factorial issues including poor baseline lung function and bacterial superinfection. Evidence supporting this picture is seen in data from Wuhan. Although smokers are said to comprise 52.1% of the male population in China [9], the rate of current smokers reported in COVID-19 series seems well below this: 7% by Huang et al. [35], 12.6% in Guan et al. [36], Zhou et al. reported 6% [1] and Zhang et al. [37] 6.4%. However, once infected, current smokers have a significantly greater mortality (9.4% versus 5.6% OR 2.96 CI 2.0–4.4) in the observational database of 8,910 COVID-19 patients [10].
Due to the extreme complexity of the RAS system, another component may be relevant in causing greater mortality in smokers with COVID-19. Neprilysin is a metalloprotease that has a number of functions but can act to breakdown Ang II to Ang(1-7), the role usually performed by ACE-2. It is highly expressed in airways, pulmonary interstitium and alveolar cells. A study examining circulating neprilysin levels in 1,536 community-based subjects ≥45 years, found that the lowest tertile group had the highest rates of smokers (p<0.001) and higher rates of hypertension (p=0.04) [38]. If smokers have low lung neprilysin activity, they may lack an important safety mechanism that could overcome virally mediated loss of the ACE-2. This might be relevant in patients taking Entresto (sacubitril/valsartan), a medication with proven benefit in the treatment of patients with heart failure. Neprilysin inhibition by the sacubitril component of Entresto may block the alternate method of generating the anti-inflammatory mediator (1-7) when ACE-2, under viral attack, is less able to do so. Clearly, this is a complex question, impossible to answer without more data and even recently reported observational studies did not have sufficient patients taking Entresto to report on the safety of this drug in COVID-19 [10,14,22].
Data Supporting RAS Activation in Severe COVID-19
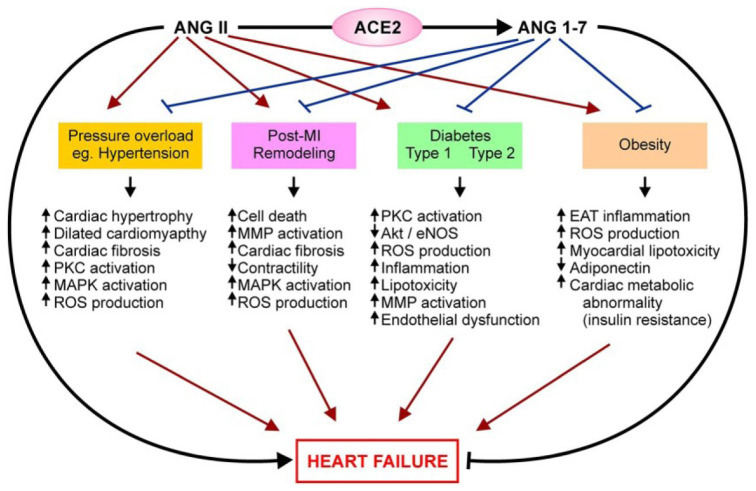
Reports from China showed that patients with severe disease, leading to intensive care unit (ICU) admission and death, had features consistent with unopposed RAS activity, such as higher blood pressure (BP) on admission to hospital and higher BP on admission to ICU in non-survivors [1,35], with a mean systolic BP of 145 mmHg in those requiring ICU admission versus 122 mmHg in milder cases (p=0.018) [35]. Lower serum potassium levels, combined with high urinary potassium has also been reported in more severe patients [39], suggesting Ang II-mediated activation of aldosterone. The presence of significant hypertension, instead of hypotension, in a group of patients admitted to ICU versus those not requiring ICU, is a particularly interesting clinical finding with implications for the pathogenesis of COVID-19. Excess RAS activity without ACE-2 balance to break down Ang II and block adverse effects, such as cellular damage and fibrosis, may play a key role in determining disease severity, similar to the RAS pro-inflammatory effects well known to contribute to heart failure (Figure 2 ).
Figure 2.
ACE2 favourable role in cardiovascular disease, mediated by Ang1-7.
Diagram from Patel et al. Circ Res 2016 [21].
Autopsy data published for four COVID-19 patients [40] has described platelet rich clot formation occluding small vessels and a microangiopathic picture, consistent with virally mediated vascular damage.
The ACE:ACE-2 Imbalance Caused by Viral ACE-2 Downregulation
Understanding the ACE:ACE-2 imbalance in COVID-19, its role in age, gender and racial differences in disease severity, and the difference between tissue bound and circulating ACE-2, could all prove key in treating this disease. In support of the fundamental ACE:ACE-2 imbalance having clinical relevance, it has been reported that serum Ang II levels are indeed significantly elevated in COVID-19 and correlate with both viral load and lung injury [41,42]. Whilst ACE formation of Ang II can be blocked by ACE inhibitors, up to 40% of Ang II is formed via non-ACE pathways such as chymase [4], making ACE inhibitors potentially less effective than ARB blockers in diminishing the problem of the excess Ang II, since the ACEI may only block 60% formation of the Ang II. On the other hand, the ARBs are highly selective blockers of the main receptor for the Ang II, the angiotensin receptor type 1 (AT1) receptor. ARBs do not decrease the amount of Ang II produced in the first place, but by blocking the AT1 receptors they activate a key counter regulatory anti-inflammatory cascade to restore the ACE:ACE-2 balance. The excessive circulating Ang II, unable to bind blocked AT1 receptors, binds AT2 receptors which trigger counter-regulatory anti-inflammatory actions and up-regulates ACE-2 expression [15] to remove excessive circulating Ang II. A protective role of increased tissue ACE-2 expression seems plausible since groups with higher levels such as younger people, premenopausal women and possibly Asian populations [8] do seem to have lower disease severity and mortality [2,9] compared to European populations with an older population and high rates of co-morbidities such as diabetes, hypertension and cardiovascular disease, all of which have been described as having higher circulating ACE-2 levels, due to increased ACE-2 shedding. It has been pointed out that in another RNA virus, human immunodeficiency virus (HIV), higher expression of binding sites such as CD4 actually protected from, rather than increased, virulence [15].
Males have only one X-linked ACE-2 allele and could be more vulnerable to phenotypes causing impaired ACE-2 regulation. Patients with pre-existing hypertension may have a greater frequency of the ACE polymorphisms that result in excessive Ang II levels, exacerbated by viral impairment of Ang II clearance. COVID-19 is a disease where a major battlefront is at the endothelium, fought by the tissue RAS. There have already been cases reported in the media of families tragically affected by very high rates of severe disease and mortality, in line with genetic factors playing a significant role in COVID-19 pathophysiology [43].
Lipid Metabolic Pathways and Links With Coronavirus Infection
Coronaviruses directly impact cellular systems, other than the RAS, which are important in inflammatory pathways. RNA viruses remodel host membranes and lipid metabolism creating a suitable environment for their replication [44]. Lipid metabolism pathways are impacted in corona virus infection, with glycerophospholipids and fatty acids significantly elevated in SARS CoV-229E infected cells. Up-regulated phosphatidylinositol (PI) may promote coronavirus entry [45]. COVID-19 is associated with cardiac events and significant serum troponin level elevation in a clinical setting [36] and elevated lysophospholipids, including LP1, have been reported in acute coronary syndromes from other causes, undergoing coronary angiography [46].
HCoV-229E infection up-regulates fatty acids, believed to promote efficient coronavirus replication. However, Yan and co-workers [45] reported that exogenous addition of fatty acids may interfere with viral replication by upsetting the delicate balance of fatty acids, causing reversion of lysophospholipids into phospholipids, limiting viral replication. It is possible that the manipulation of fatty acids in a clinical setting may upset the balance needed for viral replication. Use of drugs such as statins may also impact viral ability to harness cellular lipid pathways. Clearly more data is needed to investigate the role of fatty acid and cholesterol manipulation. The finding that statins decrease in-hospital mortality, even in a non-randomised study [10], is of interest.
Possible Long-Term Sequelae of Coronavirus Infection
Long-term sequelae of SARS, caused by a related coronavirus (SARS Co-V), have been reported in follow-up studies in survivors out to 15 years. These include sleep disturbance, characterised by increased stage 2 sleep percentage, diffuse myalgia, chronic fatigue, depression, lung damage and avascular femoral head necrosis [[47], [48], [49]].
Deranged lipid metabolism has also been reported in SARS survivors. Lipid metabolites, including phosphatidylinositol (PI) and lysophosphatidylinositol (LPI), are associated with cellular entry and/or egress of respiratory viruses. LPIs and PIs were markedly upregulated in recovered SARS patients. LPIs are thought to have a critical role in glucose homeostasis. A large proportion of the recovered SARS patients reported glucose metabolic disorders, including hyperinsulinaemia, insulin resistance, hyperglycaemia, and type 1 or 2 diabetes [48]. Patients who died of SARS were found to have extensive lung damage as well as features of systemic vasculitis. Autoantibodies against human epithelial and endothelial cells can develop after SARS-CoV infection and this could explain the severe deterioration in some patients in phase II of the disease and may lead to post-infectious cellular injury and SARS-induced immunopathology in survivors [50]. This long-term immunopathology could also be a risk in COVID-19, a related virus which also acts to inflame the endothelium and, due to gender differences in immune function, female survivors may be at greater risk to autoimmune mediated sequelae [33].
Immune System Role of Vitamin D and ACE
Vitamin D deficiency can be related to immune system dysfunction [18] and inflammation, and can cause a pro-thrombotic state; it is common in Europe in winter. Vitamin D is a potent negative endocrine regulator of the RAS and works predominantly by suppressing renin synthesis [51]. Vitamin D deficiency and genetic and geographical variation in its function may be another factor contributing to greater imbalance of the ACE:ACE-2 system leading to differences in disease severity in COVID-19. It has been suggested that vitamin D supplementation could reduce the risk of COVID-19 infection and death [52]. Lau et al. [17] reported a small study of vitamin D levels in 20 patients which is yet to be peer reviewed. They described vitamin D deficiency in 84.6% of COVID-19 patients in ICU and 57.1% of patients admitted to a ward bed. They found that 100% of patients under age 75 admitted to ICU had vitamin D deficiency (n=11).
ACE is best known for its role in blood pressure regulation by converting angiotensin I to Ang II, but in fact it cleaves many peptides and has a role in innate and adaptive immune responses, with ACE expressed on both neutrophils and macrophages. The role of ACE in immune responses and inflammation is complex and includes defence against intracellular pathogens, mediated via actions that are not dependent on Ang II, as reviewed by Bernstein and co-workers [18]. These complex interactions mean that ACEI and ARBs may not have the same impacts in COVID-19, a disease impacting both haemodynamic and inflammatory pathways.
Targets for COVID-19 Treatment
Many agents are under investigation or in clinical trial for the treatment of COVID-19 but so far no anti-viral drugs or vaccine have been officially approved for COVID-19 treatment. Hundreds of trials are listed in the WHO COVID-19 Trial data base (www.who.int International Clinical Trials Registry). A small trial using hydroxychloroquine and azithromycin showed some promise in decreasing viral carriage to only 3 to 6 days [53], an improvement on 20 days reported from China [1]. This combination could, however, carry a risk of arrhythmia due to long QT, in a group of patients where abnormal troponins and endothelial dysfunction can be present, with some arrythmias reported in China [1]. Longer trials will be needed.
Preliminary clinical data for the investigational RNA antiviral agent, remdesivir, did not show a survival benefit in a study of 237 patients in China but did show a trend to earlier recovery [54], and the Adaptive COVID-19 Treatment Trial (ACTT), a study of 1,063 patients with lung involvement in the USA, has not yet been peer reviewed but a press release from the National Institutes of Health (NIH) [55] reports a 31% faster recovery time (p<0.001) of 11 versus 15 days and possibly a trend to a survival benefit with 8% versus 11.6% mortality (p=0.059).
A variety of therapeutic approaches, in addition to a vaccine, may contribute to COVID-19 treatment and prevention in the medium and long term. However, in the current more urgent situation there are 2,075,668 active cases and 51,332 (2%) are serious or critical, with many countries still in the exponential rise phase of new cases. Treatment that can be distributed in large quantities is needed if the economic impact of this pandemic is to be addressed.
A meta-analysis of cardiac troponin results in COVID patients reported that higher levels correlated with more severe disease [20]. This is consistent with either myocarditis or an acute coronary syndrome, conditions for which manipulation of the RAS with commonly available drugs, already have an indication, based on treating endothelial and myocardial inflammation. Use of these drugs in COVID-19 patients meeting the definition for an acute coronary syndrome or for another valid cardiovascular indication can now be given with more confidence in light of recent studies showing no detriment for these drugs in COVID-19 [10,14,22].This approach may be one that is directed at fundamental viral vascular pathogenesis.
A broader therapeutic role for RAS inhibition in COVID-19 is being investigated in two randomised trials examining the effects of the ARB losartan on the severity and prognosis in COVID-19, in hospitalised COVID-19 patients (NCT 04312009) and in non-hospitalised patients (NCT04311177).
Conclusion
In the current global COVID-19 pandemic, many countries are in lockdown with social and economic paralysis. The impact of COVID-19 has been described as a warzone with many patients dying a lonely death, isolated from loved ones in overcrowded and hastily expanded hospitals. Currently, only supportive care is available. Whilst many therapeutic agents are under investigation [56,57], none have yet been approved for use in COVID-19, nor demonstrated a significant survival benefit. Even if some agents are proven to be effective, it will take time for trials and for production on a large scale.
Thinking of COVID-19 as a fundamentally cardiovascular disease that attacks the endothelium could provide momentum to use safe, established and widely available medications acting on the RAS, where they are already indicated for acute coronary syndrome and cardiac dysfunction, present in many patients with COVID-19. Whilst more data on the role of vitamin D in COVID pathogenesis is needed, replacing an essential vitamin when it is deficient, seems a safe, cost effective and easily achieved therapeutic strategy.
Any successful shift to milder disease severity will ease the burden on health care systems. Switching on endogenous anti-inflammatory pathways may also play a key role in decreasing the risk of long-term vascular and autoimmune sequelae in COVID-19 survivors, which could pose a further economic burden once the pandemic is over.
Although there may be more questions than answers and hot debate in the medical literature about the role of the RAS and drugs acting on this system in COVID-19, the consensus opinion is they are safe to use in COVID-19 [11,12], a view now supported by retrospective clinical data [10,14,22,[28], [29], [30]]. In managing a global pandemic with a high death rate, treatments aimed at the fundamental pathology, that can meet the scale of the problem, are an appealing option. Data from randomised clinical trials examining a broader role for RAS agents in COVID-19, beyond existing indications, is awaited and will further define the role of these medications.
Funding Sources
None.
Conflicts of Interest
None.
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Xiang J. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19), ChinaZhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145–151. [Article in Chinese] [Google Scholar]
- 3.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46:586–590. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wevers B.A., Van der Hoek L. Renin-angiotensin system in human coronavirus pathogenesis. Future Virol. 2010;5:145–161. doi: 10.2217/fvl.10.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dijkman R., Jebbink M.F., Deijs M., Milewska A., Pyrc K., Buelow E. Replication dependent downregulation of cellular angiotensin-converting enzyme 2 protein expression by human coronavirus NL63. J Gen Virol. 2012;93:1924–1929. doi: 10.1099/vir.0.043919-0. [DOI] [PubMed] [Google Scholar]
- 6.Luo Y., Liu C., Guan T., Li Y., Lai Y., Li F. Association of ACE2 genetic polymorphisms with hypertension-related target organ damages in south Xinjiang. Hypertens Res. 2019;42:681–689. doi: 10.1038/s41440-018-0166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayed-Tabatabaei F.A., Oostra B.A., Isaacs C.M., van Duijan C.M., Witteman J.C.M. ACE polymorphisms. Circ Res. 2006;98:1123–1133. doi: 10.1161/01.RES.0000223145.74217.e7. [DOI] [PubMed] [Google Scholar]
- 8.Chen J., Jiang Q., Xia X., Liu K., Yu Z., Tao W. Individual variation of the SARS-CoV2 receptor ACE2 gene expression and regulation. Preprints. 2020:202003019. doi: 10.1111/acel.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO data as presented on Worldometer website. www.worldometers.info Available at: [Accessed 14.6.2020]
- 10.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular disease, Drug therapy, and mortality in Covid-19. N Engl J Med. 2020;382(25):e102. doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. 2020. Escardio.org 13th March. Available at: [Accessed 14.6.2020]
- 12.Zaman S., MacIsaac A.I., Jennings G.L., Schlaich M., Inglis S.C., Arnold R. Cardiovascular disease and COVID-19: Australian/New Zealand consensus statement. Med J Aust. 2020 doi: 10.5694/mja2.50714. https://www.mja.com.au/journal/2020/cardiovascular-disease-and-covid-19-australiannew-zealand-consensus-statement Published Online First: 4 April. Available at: [Accessed 14.6.2020] [DOI] [PubMed] [Google Scholar]
- 13.Reynolds H.R., Adhikari S., Pulgarin C., Troxel A.B., Iturrate E., Johnson S.B. Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020;382(25):2441–2448. doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mancia G., Rea F.R., Ludergnani M., Apolone G., Corrao G. Renin-angiotensin-aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020;382(25):2431–2440. doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gurwitz D. Angiotensin receptor blockers as tentative SARS-CoV-2 therapeutics. Drug Dev Res. 2020 Mar 4 doi: 10.1002/ddr.21656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brojakowska A., Narula J., Shimony R., Bander J. Clinical implications of SARS-Cov2 interaction with renin angiotensin system: JACC review topic of the week. J Am Coll Cardiol. 2020;75(24):3085–3095. doi: 10.1016/j.jacc.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lau FH, Majumder R, Torabi R, Saeg F, Hoffman R, Cirillo JD, et al. Vitamin D insufficiency is prevalent in severe COVID-19. MedRxiv preprint. 10.1101/2020.04.24.20075838. [DOI]
- 18.Bernstein K.E., Khan Z., Giani J.F., Cao D.Y., Bernstein E.A., Shen X.Z. Angiotensin-converting enzyme in innate and adaptive immunity. Nat Rev Nephrol. 2018;14(5):325–336. doi: 10.1038/nrneph.2018.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aranow C. Vitamin D and the immune system. J Investig Med. 2011;59(6):881–886. doi: 10.231/JIM.0b013e31821b8755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lippi G., Lavie C.J., Sanchis-Gomar F. Meta-analysis on troponin I in patients with Coronavirus disease 2019 (COVID-10): evidence from a meta-analysis. Prog Cardiovasc Dis Mar. 2020;10 doi: 10.1016/j.pcad.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel V.B., Zhong J.C., Grant M.B., Oudit G.Y. Role of the ACE2/Angiotensin 1-7 axis of the renin-angiotensin system in heart failure. Circ Res. 2016;118(8):1313–1326. doi: 10.1161/CIRCRESAHA.116.307708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Epelman S., Tang W., Chen S., van Lente F., Francis G.S., Sen S. Detection of soluble angiotensin-converting enzyme 2 in heart failure. J Am Coll Cardiol. 2008;52(9):750–754. doi: 10.1016/j.jacc.2008.02.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uri K., Fagyas M., Kertesz A., Borbely A., Jenei C., Bene O. Circulating ACE-2 activity correlated with cardiovascular disease development. J Renin Angiotensin Aldosterone Syst. 2016;17(4) doi: 10.1177/1470320316668435. 1470320316668435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Soloman S.D. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020;382:17. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel A.B., Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA. 2020 Mar 24 doi: 10.1001/jama.2020.4812. [DOI] [PubMed] [Google Scholar]
- 26.Sommerstein R., Kochen M.M., Messerli F.H., Gräni C. Coronavirus disease 2019 (COVID-19): do angiotensin-converting enzyme inhibitors/angiotensin receptor blockers have a biphasic effect? J Am Heart Assoc. 2020;9(7):e016509. doi: 10.1161/JAHA.120.016509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang K., Gheblawi M., Oudit G.Y. Angiotensin converting enzyme 2: a double-edged sword. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047049. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Zhang P., Zhu L., Cai J., Lei F., Qin J.J., Xie J. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin ii receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;126(12):1671–1681. doi: 10.1161/CIRCRESAHA.120.317134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li J., Wang X., Chen J., Zhang H., Deng A. Association of renin-angiotensin system inhibitorswith severity or risk of death in patients with hypertension hospitalised for coronavirus disease 19 (COVID-19) infection in Wuhan, China. JAMA Cardiol. 2020:e201624. doi: 10.1001/jamacardio.2020.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bean D.M., Kraljevic Z., Searle T., Bendayan R., Pickles A., Folarin A. Treatment with ACE-inhibitors is associated with less severe disease with SARS-Covid-19 infection in a multi-site UK acute hospital trust. MedRxiv. 2020 Apr 11 doi: 10.1101/2020.04.07.20056788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Patel S.K., Wai B., Ord M., MacIsaac R.J., Grant S., Velkoska E. Association of ACE2 Genetic variants with blood pressure, left ventricular mass and cardiac function in Caucasians with type 2 diabetes. Am J Hypertens. 2012;25(2):216–222. doi: 10.1038/ajh.2011.188. [DOI] [PubMed] [Google Scholar]
- 32.Bukowska A., Spiller L., Wolke C., Lendeckel U., Weinert S., Hoffmann J. Protective regulation of the ACE2/ACE gene expression by estrogen in human atrial tissue from elderly men. Exp Biol Med (Maywood) 2017;242(14):1412–1423. doi: 10.1177/1535370217718808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ghosh S., Klein R.S. Sex drives dimorphic immune responses to viral infections. J Immunol. 2017;198:178–1790. doi: 10.4049/jimmunol.1601166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oakes J.M., Fuchs R.M., Gardener J.D., Lazartigues E., Xinping Y. Nicotine and the renin angiotensin system. Am J Physiol Regul Integr Comp Physiol. 2018;315(5):R895–R906. doi: 10.1152/ajpregu.00099.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical Features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.H., Ou C.Q., He J.-X. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of Coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang J.-J., Dong X., Cao Y.-Y., Yuan Y.D., Yang Y.B., Yan Y.Q. Clinical characteristics of 140 patients infected with SARS-CoV in Wuhan, China. Allergy. 2020 Feb 19 doi: 10.1111/all.14238. [DOI] [PubMed] [Google Scholar]
- 38.Reddy Y.N., Iyer S.R., Scott C.G., Rodeheffer R.J., Bailey K., Jenkins G. Soluble neprilysin in the general population: clinical determinants and its relationship to cardiovascular disease. J Am Heart Assoc. 2019;8:e012943. doi: 10.1161/JAHA.119.012943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen D, Li X, Song Q, Hu C, Su F, Dai J. Hypokalemia and clinical implications in patients with Coronavirus Disease 2019 (COVID-19), MedRxiv, 10.1101/2020.02.27.20028530 [DOI]
- 40.Fox SE, Akmatbekov A, Harbert JL, Li Q, Brown Q, Vender Heide RS. Pulmonary and cardiac pathology in COVID-19: the first autopsy series from New Orleans. MedRxiv, 10.1101/2020.04.06.20050575 [DOI] [PMC free article] [PubMed]
- 41.Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guo J., Huang Z., Lin L., Lv J. Coronavirus disease 2019 (COVID-19) and cardiovascular Disease: a viewpoint on the potential influence of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome Coronavirus 2 infection. J Am Heart Assoc. 2020;9(7):e016219. doi: 10.1161/JAHA.120.016219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.New York Times . March 18, 2020. Coronavirus ravages 7 members of a single family, killing 4. [Google Scholar]
- 44.Zhang Z., He G., Filipowicz N.A., Randall G., Belov G.A., Kopek B.G. Host lipids in positive-strand RNA virus genome replication. Front Microbiol. 2019;10:286. doi: 10.3389/fmicb.2019.00286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yan B., Chu H., Yuen K.-Y., Sze K.H., Lai P.M., Yuan S. Characterization of lipidomic profile of human coronavirus-infected cells: Implications for lipid metabolism remodelling upon coronavirus replication. Viruses. 2019;11(1):73. doi: 10.3390/v11010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arifin S.A., Falasca M. Lysophosphatidylinositol signalling and metabolic diseases. Metabolites. 2016;6(1):6. doi: 10.3390/metabo6010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moldofsky H., Patcai J. Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study. BMC Neurol. 2011;11:37. doi: 10.1186/1471-2377-11-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu Q., Zhou L., Sun X., Yan Z., Hu C. Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep. 2017;7:9110. doi: 10.1038/s41598-017-09536-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang P., Li J., Liu H., Han N., Jiabao J., Kou Y. Long term bone and lung consequences associated with hospital -acquired severe acute respiratory syndrome: a 15 year follow-up from a prospective cohort study. Bone Res. 2020;8:8. doi: 10.1038/s41413-020-0084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang Y.-H., Huang Y.-H., Chuang Y.-H., Peng C.-M., Wang L.-C., Lin Y.-T., Chiang B.-L. Autoantibodies against human epithelial cells and endothelial cells after severe acute respiratory syndrome (SARS)-associated coronavirus infection. J Med Virol. 2005;77:1–7. doi: 10.1002/jmv.20407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Argarwal R. Are vitamin D receptor agonists like angiotensin-converting enzyme inhibitors without side effects? Kidney Int. 2010;77(11):943–945. doi: 10.1038/ki.2010.77. [DOI] [PubMed] [Google Scholar]
- 52.Grant W.B., Lahore H., McDonnell S.L., Baggerly C.A., French C.B., Aliano J.L. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. 2020;12(4):E988. doi: 10.3390/nu12040988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gauret, Lagier J.C., Parola P., Hoang V.T., Meddeb L., Mailhe M. Hydroxychloroquine and azithromycin as a treatment of COVID-19; results of an open label non-randomised trial. Int J Antimicrob Agents. 17 March 2020 doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 54.Wang Y., Zhang D., Du G., Du R., Zhao J., Jin Y. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020;395(10236):1569–1578. doi: 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.NIH clinical Trial shows Remdesivir accelerates recovery from advanced COVID-19. 2020. www.NIH.gov Press release April 29. Available at: [Accessed 14.6.2020]
- 56.Li H., Zhou Y., Zhang M., Wang H., Zhao Q., Liu J. Updated approaches against SARS-CoV-2. Antimicrob Agents Chemother. 2020;64(6) doi: 10.1128/AAC.00483-20. e00483-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.World Health Organization Overview of the types/classes of candidate therapeutics 2020. https://www.who.int/blueprint/priority-diseases/key-action/Table of therapeutics Available at: [Accessed 14.6.2020]