Abstract
Objective
Bedside chest ultrasonography, when integrated with clinical data, is an accurate tool for improving the diagnostic process of many respiratory diseases. This study aims to evaluate the feasibility of a chest ultrasonographic screening program in nursing homes for detecting coronavirus disease-19 (COVID-19)–related pneumonia and improving the appropriateness of hospital referral of residents.
Design
Pragmatic, descriptive, feasibility study from April 2 to April 9, 2020.
Setting and Participants
A total of 83 older residents (age 85 ± 8) presenting mild to moderate respiratory symptoms and not previously tested for COVID-19, residing in 5 nursing homes in Northern Italy.
Methods
Chest ultrasonography was performed at the bedside by a team of hospital specialists with certified expertise in thoracic ultrasonography, following a systematic approach exploring 4 different areas for each hemithorax, from the anterior and posterior side. Presence of ultrasonographic signs of interstitial pneumonia, including comet-tail artifacts (B-lines) with focal or diffuse distribution, subpleural consolidations, and pleural line indentation, was detected. The specialist team integrated ultrasonography data with clinical and anamnestic information, and gave personalized therapeutic advice for each patient, including hospital referral when needed.
Results
The most frequent reasons for ultrasonographic evaluation were fever (63% of participants) and mild dyspnea (40%). Fifty-six patients (67%) had abnormal ultrasonographic findings. The most common patterns were presence of multiple subpleural consolidations (32 patients) and diffuse B-lines (24 patients), with bilateral involvement. A diagnosis of suspect COVID-19 pneumonia was made in 44 patients, and 6 of them required hospitalization. Twelve patients had ultrasonographic patterns suggesting other respiratory diseases, and 2 patients with normal ultrasonographic findings were diagnosed with COPD exacerbation.
Conclusions and Implications
In nursing home residents, screening of COVID-19 pneumonia with bedside chest ultrasonography is feasible and may represent a valid diagnostic aid for an early detection of COVID-19 outbreaks and adequate patient management.
Keywords: Lung ultrasonography, long-term care, coronavirus, viral pneumonia, interstitial pneumonia
Coronavirus disease 2019 (COVID-19) represents a big challenge for geriatric medicine.1 , 2 Frail older people are particularly at risk for developing severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection,3 , 4 and their clinical course is often characterized by severe respiratory failure and adverse outcomes.5 In Italy, the COVID-19 pandemic has been associated with high mortality rates, particularly in subjects older than 65 years with multimorbidity.6
Nursing home residents represent a category of subjects particularly vulnerable to the spread of respiratory viruses, including coronaviruses.7, 8, 9 COVID-19 outbreaks are being increasingly described in nursing homes and long-term care facilities,10 and health systems need to put up rapid and effective responses to prevent or detect such outbreaks at an early stage.11 , 12
Reverse transcriptase polymerase chain reaction for SARS-CoV-2 and high-resolution chest computed tomography (CT) are the reference standard tests for diagnosing SARS-CoV-2 infection and COVID-19–related pneumonia, respectively.13 However, the limited accessibility to these diagnostic resources in nursing homes could lead to delayed diagnosis or increased rates of hospital admission. Alternative diagnostic tests are thus needed in these healthcare settings to effectively screen residents who should primarily undergo reverse transcriptase polymerase chain reaction and chest CT testing.
Point-of-care chest ultrasonography is a rapid, inexpensive, and reliable diagnostic tool, available directly at the patient's bedside, that assists the diagnostic process of several respiratory diseases.14 , 15 This technique is particularly useful in older patients with mobility limitations and multimorbidity when integrated with clinical, epidemiologic, and anamnestic data.15 , 16 COVID-19 pneumonia can be visualized at chest ultrasonography as presence of indented or broken pleural line, bilateral areas of interstitial syndrome with B-lines alternating with spared areas of normal A-pattern, subpleural consolidations, and, in most severe cases, white lung pattern.17 , 18 Although not fully specific of COVID-19 pneumonia, in the epidemiologic context of a pandemic, the detection of 1 or more of these signs is highly suggestive of the disease.19 Thus, in older multimorbid nursing home residents with mild or moderate respiratory symptoms or fever, chest ultrasonography could help clinicians to gain important diagnostic information, prioritize the access to SARS-CoV-2 testing, and avoid many hospital admissions.
The objective of this study was to evaluate the feasibility of a chest ultrasonography program for the screening of COVID-19 in a group of Italian nursing homes located in the same district in Northern Italy, and to describe its impact on patient management.
Methods
A group of older subjects residing in 5 different nursing homes of the Emilia-Romagna region, Italy, was included in this pragmatic descriptive feasibility study conducted from April 2 to April 9, 2020. The nursing homes were chosen among those of the district where some cases of COVID-19, requiring hospital admission, were detected among residents in March 2020. All participants were isolated in compliance with recommendations of local health authorities. Included in the study were residents with respiratory symptoms, including cough and mild dyspnea with oxygen saturation in room air between 90% and 95% and respiratory rate >18, or fever, for which the nursing home physician was considering hospital referral for specialist evaluation and CT testing. Excluded were subjects with severe symptoms requiring urgent hospital admission and subjects who had already undergone testing for COVID-19.
Participating subjects were evaluated by a specialized hospital team belonging to the medical staff of a specialized geriatric unit of a large teaching hospital. The evaluation was performed within the Multidisciplinary Mobile Unit (MMU) project, which has been described in detail elsewhere.20 Briefly, the MMU consists of a hospital team, composed of a skilled internist with geriatric expertise and more than 5 years of chest ultrasonography experience and a resident in emergency-urgency medicine, delivering diagnostic examinations, including chest ultrasonography, and therapeutic advice to nursing home residents directly at their bedside, in order to avoid hospital admission.20 The team is equipped with a portable ultrasound device (Esaote MyLab Alpha, Esaote, Genova, Italy). After each visit, the team can either prescribe therapeutic advice or dispose admission to hospital.
Ultrasonographic examinations were performed by systematically scanning the front and the back side of each hemithorax, using both a convex probe for panoramic exploration and a linear probe for detailing pleural line and subpleural alterations, as recommended by chest ultrasonography guidelines.14 Each hemithorax was split into anterior-lateral sectors and posterior sectors, and each sector was then divided into upper and lower halves using the third intercostal space as reference, so as to obtain 4 areas for each hemithorax, according to our previously published research.16 The patient was kept in sitting position during examination whenever possible, with the aid of a second operator in case of severe mobility limitation. Images were saved on the ultrasonography software for review.
The presence, site, and distribution of abnormalities possibly associated with COVID-19 pneumonia,19 such as B-lines, either diffuse or with irregular distributions in different lung regions, pleural line thickening or break, consolidations, and air bronchograms, were detected. Each of these abnormalities can assume a diagnostic value for COVID-19 in the context of a nursing home outbreak during a pandemic.19 Ultrasonographic sign severity was graded according to the scoring system proposed by Soldati and colleagues (0 = regular pleural line, A-lines present; 1 = indented pleural line, focal B-lines; 2 = broken pleural line, subpleural consolidations; 3 = white lung with or without consolidations).17
Differential diagnosis between COVID-19 and other possible causes of respiratory symptoms and fever was made by integrating the clinical history and physical examination findings with ultrasonographic images.19 For example, the presence of a normal ultrasonographic pattern associated with dyspnea, cough, and smoking history was suggestive of exacerbation of chronic obstructive pulmonary disease. A history of heart disease associated with pleural effusion and homogeneous bilateral increase of B-lines without spared regions was suggestive of congestive heart failure. COVID-19–associated lung B-lines have in fact a typical focal distribution, with spared areas of normally ventilated lung nearby, whereas diffuse B-lines or white lung pattern indicate severe disease.19
Essential clinical information of each patient, including age, symptom type, severity, and timing, was collected from the nursing home clinical record. The outcome of the MMU consultation and subsequent patient disposition (therapeutic advice with or without activation of usual diagnostic routes for COVID-19, admission to hospital) was also recorded.
Data were expressed as mean ± standard deviation or percentages, as appropriate. Comparisons between subjects with normal ultrasonography and subjects with ultrasonographic abnormalities were made using t test and chi-square test. Data were analyzed with SPSS software (IBM, Armonk, NY).
The study protocol was approved by the Ethics Committee of Area Vasta Emilia Nord, Emilia-Romagna Region, under the ID 235/2020/OSS/AOUPR.
Results
We evaluated 83 older patients (60 females, 23 males, mean age 85 ± 8 years) residing in 5 different nursing homes. Symptom distribution and duration prior to the MMU consultation are summarized in Table 1 . Fever (63% of patients), cough (40%), and dyspnea or oxygen desaturation of mild severity (40%) were the most frequent reasons for consultation.
Table 1.
Overview of Demographic, Clinical, and Ultrasonographic Data of the 83 Nursing Home Residents That Were Screened for COVID-19 by Chest Ultrasonography
| Entire Sample (n = 83) | Patients With Normal Chest Ultrasonography (n = 27) | Patients With Ultrasonographic Abnormalities (n = 56) | P∗ | |
|---|---|---|---|---|
| General Characteristics | ||||
| Males | 23 (28) | 12 (44) | 11 (20) | .018 |
| Age, y, mean ± SD | 85 ± 8 | 83 ± 8 | 86 ± 7 | .04 |
| Symptoms before evaluation | ||||
| Cough | 33 (40) | 16 (59) | 17 (30) | .012 |
| Fever | 52 (63) | 11 (41) | 41 (72) | .004 |
| Dyspnea | 33 (40) | 3 (11) | 30 (54) | <.001 |
| Other symptoms | 2 (2) | 2 (7) | 0 (0) | .039 |
| Duration of symptoms, days, mean ± SD | 9 ± 5 | 8 ± 6 | 9 ± 5 | .47 |
| Ultrasonographic findings | ||||
| Ultrasonographic abnormalities | 56 (67) | 0 (0) | 56 (100) | — |
| Focal B-lines | 17 (20) | 0 (0) | 17 (30) | — |
| Diffuse B-lines | 24 (30) | 0 (0) | 24 (43) | — |
| Subpleural consolidations | 32 (39) | 0 (0) | 32 (57) | — |
| Isolated pleural line abnormalities | 3 (4) | 0 (0) | 3 (5) | — |
| Pleural effusion | 3 (4) | 0 (0) | 3 (5) | — |
| Lung ultrasonography score, mean ± SD | 1.5 ± 1.2 | 0 | 2.2 ± 0.8 | — |
| Diagnosis after consultation | ||||
| COVID-19 diagnosis | 44 (53) | 0 (0) | 44 (79) | — |
| Other pneumonia | 7 (8) | 0 (0) | 7 (13) | — |
| Congestive heart failure | 5 (6) | 0 (0) | 5 (8) | — |
| COPD exacerbation | 2 (2) | 2 (7) | 0 (0) | — |
| Outcome of the consultation | ||||
| No specific treatment | 27 (32) | 22 (82) | 5 (9) | <.001 |
| Therapy prescription | 50 (60) | 5 (19) | 45 (80) | <.001 |
| Hospital admission | 6 (7) | 0 (0) | 6 (11) | <.001 |
COPD, chronic obstructive pulmonary disease; SD, standard deviation.
Unless otherwise noted, values are n (%).
P values were calculated with t test and chi-square test, as appropriate. Significant P values (<.05) are indicated in bold.
Twenty-seven patients (33%) had a normal lung ultrasonographic pattern (Table 1), with regular pleural line and bilateral horizontal artifacts (A-lines) reflecting normally aerated lung surface. These findings allowed the exclusion of the presence of COVID-19–related interstitial pneumonia. In 2 cases, the integration of normal ultrasonographic findings with physical examination and patient history allowed the diagnosis of exacerbation of chronic obstructive pulmonary disease, and appropriate treatment was administered.
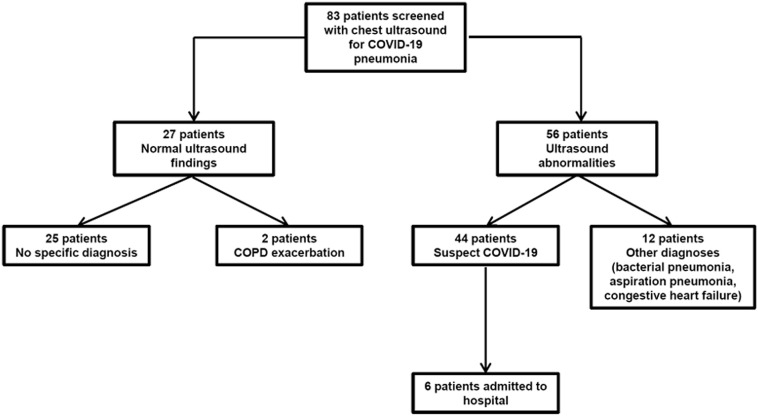
Fifty-six patients (67%) had abnormal ultrasonographic findings (Figure 1 ). The most frequent signs were multiple bilateral subpleural consolidations (32 patients), diffuse bilateral B-lines or white lung pattern (24 patients), and focal B-lines (17 patients). Pleural effusion and isolated pleural line abnormalities were detected in only 3 patients each. A diagnosis of COVID-19 interstitial pneumonia was considered probable in 44 cases (53% of the entire sample) after integration of ultrasonography with clinical data and personal history. In all of them, health surveillance system was activated for SARS-CoV-2 testing, and empiric pharmacologic treatment (antibiotics, hydroxychloroquine, or steroids) was prescribed. Hospital admission was disposed in only 6 patients.
Fig. 1.
Ultrasonographic appearance of suspect COVID-19 pneumonia in older patients residing in nursing homes. (A) Transversal scan in intercostal space, with demonstration of subpleural consolidations and diffuse comet-tail artifacts (B-lines). (B) Trasversal scan, with demonstration of indented pleural line associated with diffuse B-lines. (C) Longitudinal scan showing diffuse B-lines in intercostal spaces.
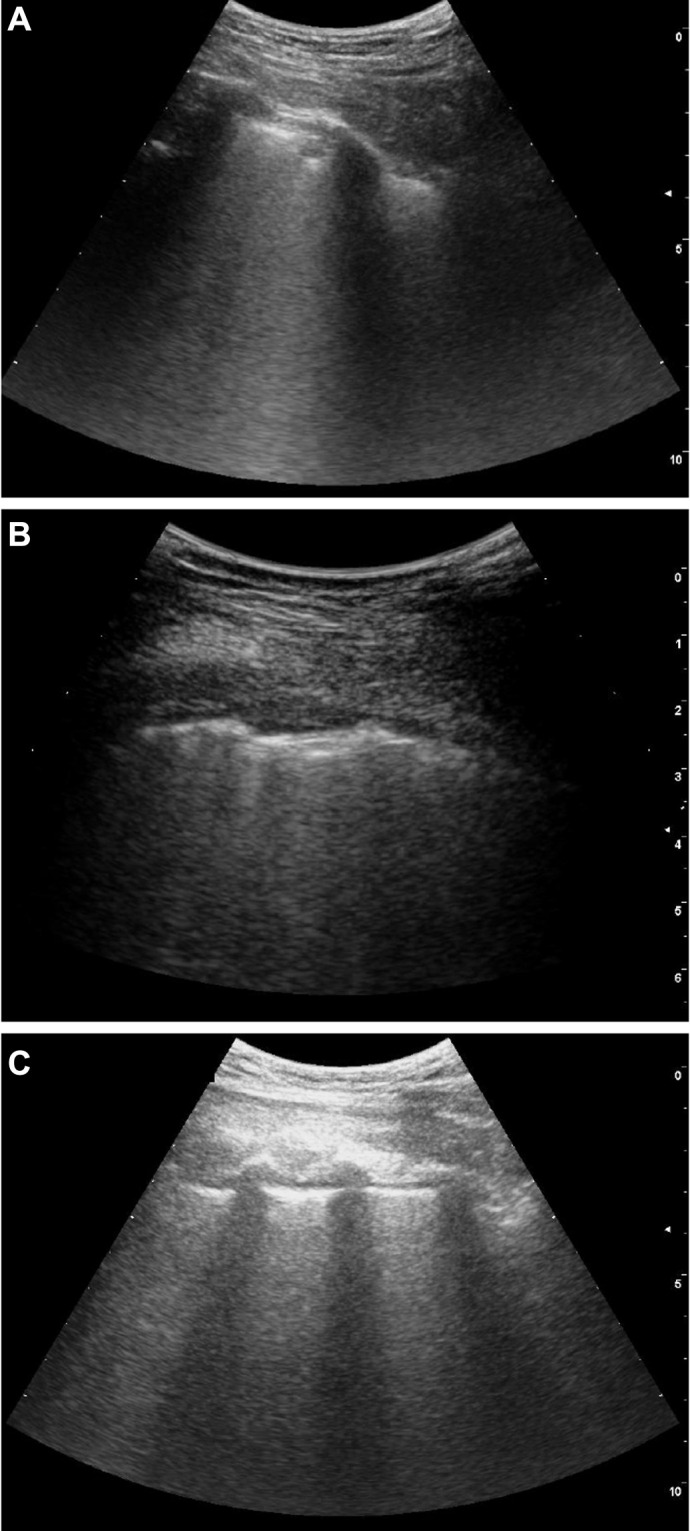
In the remaining 12 patients with abnormal ultrasonographic findings, the clinical picture and characteristics of images, with signs that are not generally associated with interstitial pneumonia (presence of pleural effusion, large consolidations with dynamic air bronchogram) suggested alternative diagnoses. Mild decompensated heart failure was diagnosed in 5 cases, aspiration pneumonia in 5 cases, and bacterial pneumonia in 2 cases. Appropriate treatment was then prescribed. An overview of the study findings is depicted in Figure 2 .
Fig. 2.
Overview of the study findings and classification of chest ultrasonographic examinations according to ultrasonographic appearance and clinical data. COPD, chronic obstructive pulmonary disease.
Discussion
We sought to explore the possible role of performing chest ultrasonography at the patient's bedside in nursing home residents with signs and symptoms compatible with SARS-CoV-2 infection. Our study shows that this approach is feasible, practical, and comfortable for patients and operators, supporting the role of point-of-care chest ultrasonography as a valid diagnostic aid in nursing homes during COVID-19 outbreak.
The integration of ultrasonographic imaging with clinical and anamnestic data allows for the refinement of the diagnostic process, not only for COVID-19, but also for other respiratory diseases that can be commonly found in the older frail population.15 Moreover, ultrasonographic evaluation could prevent hospital admission for diagnostic testing that is not available in a nursing home setting.15 , 20 In fact, all patients included in the present investigation were being strictly monitored by nursing home physicians as candidates for hospital admission. From this perspective, the use of chest ultrasonography in nursing homes could help to prevent avoidable hospitalizations.
The role of chest ultrasonography should, however, not be overestimated. Like traditional radiologic imaging (radiography and CT), chest ultrasonography only shows pulmonary involvement in SARS-CoV-2 infection. A negative chest imaging does not allow the ruling out of SARS-CoV-2 infection, and it should not be considered as a substitute for a thorough clinical examination and reverse transcriptase polymerase chain reaction testing, especially in high-risk subjects.21 In the early phases of COVID-19–related pneumonia, even chest CT can show normal results, and this concept may also apply to ultrasonography.22, 23, 24
Moreover, the correlation between ultrasonographic and CT findings in COVID-19 pneumonia has not been demonstrated yet, apart from small case series.18 However, in many other respiratory diseases, chest ultrasonography has showed a consistent agreement with CT findings in the hands of skilled operators and when integrated with clinical information.15 , 25 Differential diagnosis between COVID-19 pneumonia and other pulmonary diseases associated with interstitial syndrome, including pulmonary fibrosis and chronic heart failure, may also be challenging when no clinical or anamnestic data help to solve the diagnostic dilemma.17 The reliability and accuracy of ultrasonography in the diagnosis of COVID-19–associated pneumonia should thus be confirmed in future studies with prospective design.
Geriatric patients residing in nursing homes are probably those who can benefit the most from the implementation of chest ultrasonography in the diagnostic route of COVID-19 pneumonia.15 Multimorbidity, frailty, and mobility limitations may in fact represent important barriers to accessing traditional imaging resources.15 Pulmonary ultrasonographic screening, especially when symptoms are mild and contact with subjects tested positive for SARS-CoV-2 is uncertain, could provide important information for guiding diagnostic routes in nursing homes.
Unfortunately, point-of-care ultrasonography is not widespread in geriatric practice, and training programs are urgently needed to fill this gap.26 In older nursing home residents, timing of COVID-19 diagnosis may be crucial for reducing adverse outcomes. From this perspective, the use of point-of-care ultrasonography could provide a relevant diagnostic aid for improving patient care and outcomes.
Conclusions and Implications
The use of bedside chest ultrasonography in nursing home residents for screening of possible cases of COVID-19 pneumonia is practical and feasible, and has the potential to improve the management of outbreaks and patient care. Larger studies are needed to compare the effects of this approach with the usual care in terms of patient outcomes and control of outbreaks in nursing homes. Implementation of ultrasonography services in nursing home care should be carefully considered in the near future.
Acknowledgments
The authors thank the management, the doctors, and personnel of the 5 nursing homes of Parma province that participated to this study, and the management of Azienda Unità Sanitaria Locale di Parma for the support in the UMM project. The authors also thank Dr Angela Guerra for assistance in data collection and analysis and Dr Nicoletta Cerundolo for advice in manuscript revision.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Cesari M., Proietti M. Geriatric medicine in Italy in the time of COVID-19. J Nutr Health Aging. 2020;24:459–460. doi: 10.1007/s12603-020-1354-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landi F., Barillaro C., Bellieni A. The new challenge of geriatrics: Saving frail older people from the SARS-CoV-2 pandemic infection. J Nutr Health Aging. 2020;24:466–470. doi: 10.1007/s12603-020-1356-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abbatecola A.M., Antonelli Incalzi R. Editorial: COVID-19 spiraling of frailty in older Italian patients. J Nutr Health Aging. 2020;24:453–455. doi: 10.1007/s12603-020-1357-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lloyd-Sherlock P.G., Kalache A., McKee M. WHO must prioritise the needs of older people in its response to the covid-19 pandemic. BMJ. 2020;368:m1164. doi: 10.1136/bmj.m1164. [DOI] [PubMed] [Google Scholar]
- 5.Liu K., Chen Y., Lin R. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80:e14–e18. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 Mar 23 doi: 10.1001/jama.2020.4683. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Falsey A.R., Dallal G.E., Formica M.A. Long-term care facilities: A cornucopia of viral pathogens. J Am Geriatr Soc. 2008;56:1281–1285. doi: 10.1111/j.1532-5415.2008.01775.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chasqueira M.J., Paixão P., Rodrigues M.L. Respiratory infections in elderly people: Viral role in a resident population of elderly care centers in Lisbon, winter 2013-2014. Int J Infect Dis. 2018;69:1–7. doi: 10.1016/j.ijid.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Birch C.J., Clothier H.J., Seccull A. Human coronavirus OC43 causes influenza-like illness in residents and staff of aged-care facilities in Melbourne, Australia. Epidemiol Infect. 2005;133:273–277. doi: 10.1017/s0950268804003346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McMichael T.M., Currie D.W., Clark S. Epidemiology of COVID-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382:2005–2011. doi: 10.1056/NEJMoa2005412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan L.F., Seetharaman S. Preventing the spread of COVID-19 to nursing homes: Experience from a Singapore geriatric centre. J Am Geriatr Soc. 2020;68:942. doi: 10.1111/jgs.16447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roland K., Markus M. COVID-19 pandemic: Palliative care for elderly and frail patients at home and in residential and nursing homes. Swiss Med Wkly. 2020;150:w20235. doi: 10.4414/smw.2020.20235. [DOI] [PubMed] [Google Scholar]
- 13.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpicelli G., Elbarbary M., Blavais M. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 15.Ticinesi A., Scarlata S., Nouvenne A. The geriatric patient: The ideal one for chest ultrasonography? A review from the Chest Ultrasound in the Elderly Study Group (GRETA) of the Italian Society of Gerontology and Geriatrics (SIGG) J Am Med Dir Assoc. 2020;21:447–454.e6. doi: 10.1016/j.jamda.2019.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Ticinesi A., Lauretani F., Nouvenne A. Lung ultrasound and chest x-ray for detecting pneumonia in an acute geriatric ward. Medicine. 2016;95:e4153. doi: 10.1097/MD.0000000000004153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soldati G., Smargiassi A., Inchingolo M. Proposal for international standardization of the use of lung ultrasound for COVID-19 patients; a simple, quantitative, reproducible method. J Ultrasound Med. 2020;39:1413–1419. doi: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poggiali E., Dacrema A., Bastoni D. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID-19) pneumonia? Radiology. 2020;295:E6. doi: 10.1148/radiol.2020200847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piscaglia F., Stefanini F., Cantisani V. Benefits, open questions and challenges of the use of ultrasound in the COVID-19 pandemic era. The views of a panel of worldwide international experts. Ultraschall Med. 2020;41:228–236. doi: 10.1055/a-1149-9872. [DOI] [PubMed] [Google Scholar]
- 20.Nouvenne A., Caminiti C., Diodati F. Implementation of a strategy involving a multidisciplinary mobile unit team to prevent hospital admission in nursing home residents: Protocol of a quasi-experimental study (MMU-1) study. BMJ Open. 2020;10:e034742. doi: 10.1136/bmjopen-2019-034742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sverzellati N., Milone F., Balbi M. How imaging should properly be used in COVID-19 outbreak: An Italian experience. Diagn Interv Radiol. 2020;26:204–206. doi: 10.5152/dir.2020.30320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ai T., Yang Z., Hou H. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 Feb 26 doi: 10.1148/radiol.2020200642. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Long C., Xu H., Shen Q. Diagnosis of coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020;126:108961. doi: 10.1016/j.ejrad.2020.108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bernheim A., Mei X., Huang M. Chest CT findings in coronavirus disease-19 (COVID-19): Relationship to duration of infection. Radiology. 2020;295:200463. doi: 10.1148/radiol.2020200463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Staub L.J., Mazzali Biscaro R.R., Kaszubowski E. Lung ultrasound for the emergency diagnosis of pneumonia, acute heart failure, and exacerbations of chronic obstructive pulmonary disease/asthma in adults: A systematic review and meta-analysis. J Emerg Med. 2019;56:53–69. doi: 10.1016/j.jemermed.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Ticinesi A., Lauretani F., Nouvenne A. Chest ultrasound in Italian geriatric wards: Use, applications and clinicians' attitudes. J Gerontol Geriatr. 2020;68:1–10. [Google Scholar]