Abstract
Median raphe cyst (MRC) is an uncommon, asymptomatic benign lesion, that may present anywhere on the midline ridge between the external urethral meatus and the anus. Although they are developmental in origin, they often present in the postpubertal age, aggravated by trauma, and are frequently infected secondarily. MRCs are often misdiagnosed as epidermal cysts, steatocystoma multiplex, and eccrine cystadenomas. They are underrecognized and less than ten case reports exist from the Indian subcontinent. We, herein report a male with an immunohistochemically proven parameatal MRC.
Keywords: Immunohistochemistry, median raphe cyst, steatocystoma multiplex, transitional epithelium, urogenital epithelium
Introduction
Historically, the median raphe was a Biblical euphemism for a developmental scar on the mammalian 'Baculum' or os penis. By definition, any cavity lined by urogenital epithelium, presenting over this raphe is termed as a median raphe cyst (MRC). MRC is an uncommon, asymptomatic benign lesion. When present near the external urethral meatus, it is termed as 'parameatal'.[1] Parameatal cysts often show a stratified squamous epithelium. Morphological types described in literature include classic, nodular, canalicular, linear, pigmented, and multicystic types. Amaranathan et al., in their study have inferred that there are only ten case reports of penile localization from India and less than 200 globally.[2] Histopathological types of MRCs include urethral, epidermoid, glandular, mucoid, melanized, and mixed types.[3] This patient presented to our outpatient department with an asymptomatic, parameatal median raphe cyst, showing mixed epithelial lining on Tzanck cytology and histopathology, and classic immunostaining for cytokeratin 7 (CK7) and cytokeratin 13 (CK13).
Case Report
A 33-year-old unmarried male patient, presented to the dermatology outpatient department, with a single, asymptomatic, skin colored swelling present on the glans penis, of 5 years duration. He had no history of trauma, application of local medicament, or high-risk sexual behavior. Clinical examination revealed a solitary 7 × 5 mm, flesh colored, nontender, smooth swelling, proximal to the meatus, over the ventral penile surface [Figure 1]. The lesion was not compressible and showed no transillumination. Aspiration with a 20 G needle was done and a Tzanck smear was made, from the viscous, nonmalodorous aspirate. Tzanck smear showed multiple flat epithelial cells similar to that of transitional epithelium and squamous cell epithelium [Figure 2]. The aspirate was found to be sterile on microbiological examination.
Figure 1.

A flesh-colored swelling, 7 × 5 mm in size, on ventral aspect of parameatal glans
Figure 2.

Tzanck smear shows flat, polygonal cells similar to that of squamous epithelium
Local high frequency sonography showed a well-defined, hypoechoic lesion measuring 6 × 5 × 3 mm, spanning the epidermis and dermis of the glans, with no other cystic or solid lesion in any part of the penis. A narrow punch biopsy was performed, and the section showed three distinct layers, the outermost being normal stratified squamous epithelium. Beneath that, fibrocollagenous stroma was appreciated [Figure 3]. The cyst showed variable lining i.e., stratified squamous and transitional type of epithelium. No adnexal structures or atypical cells were noted in cyst wall [Figure 4]. On immunohistochemistry, the cells were positive for cytokeratin 7 and cytokeratin 20 and negative for human milk fat globulin. On clinicopathological correlation, a final diagnosis of MRC of mixed epithelium type was made. Complete surgical excision was performed under local, infiltrative anesthesia.
Figure 3.

Three layers, outermost being stratified squamous epithelium. Fibrocollagenous connective tissue can be seen between epidermis and cyst epithelium. (H and E, 10 ×)
Figure 4.
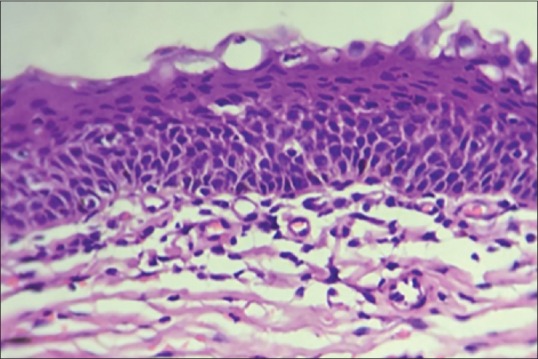
Cyst lining showing columnar cells at the base, flattening as they move upward - transitional epithelium. (H and E, 40 ×)
Discussion
MRC is an uncommon, benign midline lesion localized along the raphe anywhere between the external urethral meatus and the anus. They are synonymous with mucus cyst of the penile shaft and genitoperineal cysts of the medium raphe.[1]
Most cases are asymptomatic during childhood and become symptomatic during adolescence or adulthood. Patients may, rarely, present with pain (due to infection or trauma), dysuria, hematuria, hematospermia, and dyspareunia.[3] Commonly presenting as solitary cysts, the rare variants of MRC include canaliform, cord-like, and multicystic indurations on the median raphe.[4]
Differential diagnoses include steatocystomas, epidermal or dermoid cysts, glomus tumor, pilonidal cyst, urethral diverticulum, eccrine cystadenomas, and steatocystomas[5] which can be differentiated on the basis of histology and, wherever indicated, immunohistochemistry.[6]
Various pathogenetic hypotheses exist regarding the evolution of MRC. The first theory is 'tissue trapping' during embryonic fusion of urethral folds for development of urethral groove.[1,5,7] Another theory is that MRCs could be caused by the anomalous developmental of the periurethral glands of Littre[8] and by aberrant blockage of the paraurethral duct.[9]
Median raphe cysts show some characteristic morphological pointers, such as:
The most common presentation is a globular, nodular swelling
The most common site is over the median raphe
It can be median or paramedian in position
It is a translucent swelling and transillumination test is usually positive
On needling, the lesion oozes a viscid fluid.
They also demonstrate classic histopathological findings. They are derived from urogenital epithelium, 'transitioning' from columnar to squamous epithelium - the epithelium flattens to be able to accommodate the stretch levied by the enclosed mucosae. Shao et al.[3] have described various histopathological types. They are[1] pseudostratified columnar epithelium (if the proximal urethral cells are trapped),[2] squamous cell epithelium (if the distal urethral cells are trapped),[3] glandular epithelium (if the periurethral glands are trapped), and[4] the mixed type. Ciliated epithelium is rarely noticed and considered as a metaplastic change secondary to local irritation or trauma. Our case is a mixed type of MRC, showcasing the triple histological epithelial lining, as described above.
In the case reported by Persec et al.,[10] immunohistological typing of epithelial cells showed positivity for CK7, CK13 and negativity for HMFG-1. Our case has CK7 and CK13 positivity and was negative for CK10 and HMFG-1. The authors have tabulated immunohistochemical findings of MRC, pitted against epidermal cysts and steatocystoma multiplex, its close differentials [Table 1]. In most cases, clinicopathological correlation is sufficient to reach a diagnosis. Our case had an atypical parameatal distribution, and hence, immunohistochemical confirmation was done.
Table 1.
Immunohistochemical markers of median raphe cysts, pitted against its close clinicopathological differentials - epidermal cysts and steatocystoma multiplex
| Immunohistochemistry | Median raphe cyst (MRC) | Steatocystoma multiplex (SM) | Epidermal cyst |
|---|---|---|---|
| Cytokeratin 7 (CK7) | + | + | - |
| Cytokeratin 10 (CK10) | - | + | + |
| Cytokeratin 13 (CK13) | + | - | - |
| Human milk fat globulin - 1 (HMFG-1) | - | + | - |
Complete local excision of the cyst, including its wall, is the preferred treatment of choice. Simple needle aspiration leads to recurrence of the cyst. Marsupialization or deroofing are performed in deeply located large cysts, or multicystic lesions, which can result in gaping sinuses and cord-like tracts, which are cosmetically unsatisfactory, and hence, should be avoided. Other surgical complications include formation of a urethrocutaneous fistula.[3,9]
Conclusion
Median raphe cyst is a rare entity, reported infrequently from the Indian subcontinent, and is often unrecognized. MRCs are an uncommon type of disembryoplasia that can occur in any location of the median raphe, from the balanic meatus to the anal edges. These cysts are generally asymptomatic and their treatment of choice is surgical extirpation. A diagnosis of MRC should be kept as a possibility when a patient presents with a cystic or nodular lesion on the genitals, which must then be confirmed by histopathology and immunohistochemistry, wherever needed.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Otsuka T, Ueda Y, Terauchi M, Kinoshita Y. Median raphe (parameatal) cysts of the penis. J Urol. 1998;159:1918–20. doi: 10.1016/S0022-5347(01)63196-3. [DOI] [PubMed] [Google Scholar]
- 2.Amaranathan A, Sinhasan SP, Dasiah SD. Median raphe cysts of the prepucial skin, with triple histological linings: A case report and review of the literature. J Clin Diagn Res. 2013;7:1466–8. doi: 10.7860/JCDR/2013/6168.3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shao HI, Chen TD, Shao HT, Chen HW. Male median raphe cysts: Serial retrospective analysis and histopathological classification. Diagn Pathol. 2012;7:121. doi: 10.1186/1746-1596-7-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Verma SB. Canal-like median raphe cysts: An unusual presentation of an unusual condition. J Clin Exp Dermatol. 2009;34:857–8. doi: 10.1111/j.1365-2230.2009.03604.x. [DOI] [PubMed] [Google Scholar]
- 5.Nagore E, Sánchez-Motilla JM, Febrer MI, Aliaga A. Median raphe cysts of the penis: A report of five cases. Pediatr Dermatol. 1998;15:191–3. doi: 10.1046/j.1525-1470.1998.1998015191.x. [DOI] [PubMed] [Google Scholar]
- 6.Kirkham N, Elder D, Elenitsas R, Jasorsky C, Johnson B. 42 Tumors and cysts of the epidermis. Lever's Histopathology. 1997;8:685–746. [Google Scholar]
- 7.Krauel L, Tarrado X, Garcia-Aparicio L, Lerena J, Sunol M, Rodo J, et al. Median raphe cysts of the perineum in children. Urology. 2008;71:830–1. doi: 10.1016/j.urology.2007.11.131. [DOI] [PubMed] [Google Scholar]
- 8.Dini M, Baroni G, Colafranceschi M. Median raphe cyst of the penis: A report of two cases with immunohistochemical investigation. Am J Dermatopathol. 2001;23:320–4. doi: 10.1097/00000372-200108000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Shiraki IW. Parametal cysts of the glans penis: A report of 9 cases. J Urol. 1975;114:544–8. doi: 10.1016/s0022-5347(17)67079-4. [DOI] [PubMed] [Google Scholar]
- 10.Persec Z, Persec J, Sovic T, Rako D, Bacalja J, et al. Median Raphe Cyst–Clinical Report and Immunohistochemical Analysis? J Clin Exp Dermatol Res. 2013;S6:011. doi:10.4172/2155-9554.S6- [Google Scholar]


